Abstract
Background/Aims
Patients with chronic constipation (CC) exhibit symptoms and functional abnormalities upon testing, but their relationship to age and gender is unclear. We assessed age- and gender-related differences in symptoms, colon transit time, and anorectal motility, sensation, and expulsion.
Patients and Methods
Retrospective, post hoc data analysis of patients with CC, who underwent Wireless Motility Capsule (WMC), High-Resolution Anorectal Manometry (HR-ARM), Balloon Expulsion Test (BET) and Rectal Sensory Testing (RST). Clinical assessment was made by questionnaires. Standard WMC criteria for colonic transit time (CTT) and the London classification was used for HR‐ARM analyses, and regression plots between age, gender, CTT, HR-HRM, RST and BET were calculated.
Results
We studied 75 women and 91 men. Abdominal pain, infrequent defecation, incomplete evacuation, defecatory straining, and multiple motility and anorectal function abnormalities were common. Abdominal pain was least frequently, and straining was most frequently associated with a motility abnormality. For each symptom, the highest prevalence was associated with failed BET. There was a significant increase in CTT with age only in men (p = 0.0006). In men, for each year of age there was a CTT increase of 1.02 h. The prevalence of abdominal pain and incomplete evacuation for females was significantly higher than that for males (both P < 0.05). The prevalence of low anal squeeze pressure for females was significantly higher than that for males, and the prevalence of poor rectal sensation for males was significantly higher than that for females (both P < 0.05). A significant decrease in basal anal and squeeze pressures with age occurred in women (p < 0.0001); an increase in age of one year was associated with a decrease in anal base pressure of 1.2 mmHg. Abnormal CTT and HR-ARM tests were associated with increased symptom frequency, but not severity.
Conclusions
There are significant age- and gender-related differences in symptoms, CTT, and HR-HRM parameters, rectal sensation, and expulsion, that may influence the multifaceted management of constipation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Constipation implies unsatisfactory defecation resulting from infrequent and difficult stool passage, or both [1]. Chronic constipation (CC), associated with excessive straining, incomplete evacuation, infrequent bowel movements, bloating, and abdominal pain, can affect quality of life (QoL) in up to 5% of the population [2]. Recurrent CC resulting from poor colonic propulsion at times together with poorly coordinated stool expulsion and altered gastrointestinal sensitivity may lead to significant morbidity and mortality due to fecal impaction, pseudo-obstruction, volvulus, and colonic perforation [3].
The Rome IV criteria classify CC into 4 types: (a) Functional Constipation (FC), (b) Irritable Bowel Syndrome, with Constipation (IBS-C), (c) Opioid-Induced Constipation (OIC), and (d) Functional Defecation Disorders (FDDs), such as inadequate and dyssynergic defecation [4]. Based on the detected physiological abnormalities upon testing, 3 subtypes of CC -at times overlapping- may be encountered: slow-transit constipation (STC), evacuation disorder (ED), and normal transit constipation (NTC). Such subtyping could improve the management of constipation, using a multifaceted approach [5].
Frequently, CC remains clinically undifferentiated, and tests of colon transit, such as the Wireless Motility Capsule (WMC), and tests of evacuation, such as High-Resolution Anorectal Manometry (HR-ARM), the Balloon Expulsion Test (BET), Rectal Sensory Test (RST), and MR defecography, may be used [6]. Recently, an International Anorectal Physiology Working Group (IAPWG) presented a consensus—the “London classification”- on the assessment of anorectal function, using HR‐ARM, aiming at prioritization in decision making for patients with symptoms of anorectal dysfunction [7]. However, motility test results can vary with age and gender in normal subjects as well as in subjects with constipation [8,9,10].
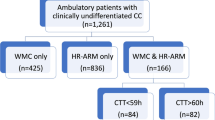
In this study, we conducted post hoc analyses of data from a recent study of colonic and anorectal motility in 166 community-based patients with clinically undifferentiated CC which reported a high prevalence of anorectal dysfunction, regardless of colon transit time (CTT) [11]. In this cohort, who were studied by both wireless motility capsule (WMC), high-resolution anorectal manometry (HR‐ARM), BET, and RST, we aimed to explore the possible relationships of age and gender to CTT, anorectal function and sensation parameters, and symptoms. Such relationships might influence the assessments proposed by the London Classification.
Patients and Methods
This is a post hoc analysis of prospectively collected data of patients with clinically undifferentiated CC. This database was created from de-identified motility test results and symptoms that were collected systematically as part of a retrospective, IRB-approved study (El Camino Hospital IRB, Mountain View, CA). Clinical details of the study cohort have been previously reported [11]. Briefly, the cohort included patients with infrequent bowels (STC) and disordered rectal evacuation (ED). No patients had evidence of colonic obstruction by colonoscopy. Symptoms (lower abdominal pain, infrequent defecation of hard stools, sense of incomplete evacuation of stools, and straining during defecation) were collected using a standard questionnaire that asked each patient to report “yes” or “no” for each symptom. A patient who reported a symptom was asked to also rate its severity as “mild”, “moderate” or “severe” (absent = 0, mild = 1, moderate = 2, and severe = 3) [12].
HR-ARM technique, RST, and BET Details of our HR-ARM technique, RST, and BET have been provided elsewhere following the sequence described by the London IAPWG Classification [7, 11]. HR-ARM involved measurements of resting (basal) anal tone and maximal anal sphincter (squeeze) pressure and anorectal coordination. The RST assessed rectal sensitivity, utilizing a rectal balloon placed proximal to the anal canal, recording the volume (in ml) to first sensation that provokes the desire to defecate, and the maximum tolerated volume upon gradual balloon inflation. Finally, the BET measured the ability to expel a 60 ml balloon from the rectum within 60 s. Normal values for our laboratory used over the study period and in this analysis are: anal sphincter basal pressure: 67-82 mmHg, maximal anal sphincter squeeze pressure: 191-247 mmHg, rectal sensation to balloon distention: 10–50 ml (volumes for each sensory level); rectal hypersensitivity, perception with < 10ml balloon distention; rectal hyposensitivity perception with > 40ml balloon distention; recto-anal inhibitory reflex (RAIR) threshold present and elicited with < 60 ml of balloon distention [6]. Abnormal motility test values were low anal base pressure < 67 mm Hg; low anal squeeze pressure < 191 mm Hg; low rectal sensation > 40 ml; failed balloon expulsion test (BET) balloon filled with 60 ml liquid expelled > 60 s.
WMC protocol The WMC (Smartpill®) is an ambulatory, non-invasive sensor that continuously samples intraluminal pH, temperature, and pressure, as it moves through the gastrointestinal tract; normative data have been previously published. Downloaded data were analyzed using the display software (Medtronic, Sunnyvale, California, USA). All medications were discontinued for 5 days before and during the 5-day conduct of WMC. Normal CTT was a priori defined as < or = 59 h, while prolonged CTT was > 59 h [13].
Analyses We used the London classification that examines for (a) the presence or absence of areflexia, (b) any disorders of anal tone (maximal anal sphincter basal pressure) and contractility (maximal anal sphincter squeeze pressure, (c) disorders of anorectal coordination and (d) disorders of rectal sensation to balloon distention (RST), specifically hypo- and hypersensitivity. BET was also analyzed and reported separately as positive (60 ml balloon expelled in a timely fashion, < 60 s) or negative. Statistical analyses, regression analyses, and calculation of cumulative distributions were performed using GraphPad Prism 10.0.2. Because the present analyses were exploratory, P-values were not adjusted for multiple comparisons [14].
Results
Our analyzed study cohort consisted of 166 patients, 75 women and 91 men, 142 Caucasians, 6 Hispanic and 18 Asians, with a median age of 65 years (range 22–86). Their median reported disease duration was 2.5 years. This cohort represents a heterogeneous collection of patients with undifferentiated chronic constipation that represent a typical clinical practice population. The median symptom scores for each interrogated variables were: Lower abdominal pain 0.67; infrequent bowel movements 1.49, incomplete evacuation 1.2, and straining 1.63), representing various degrees of frequency and severity (0 = none; 1 = Mild; 2 = Moderate; 3 = Severe) for each symptom. When HR-ARM abnormalities using the London classification and including the results of BET in the 166 patients were analyzed, there was only 1 patient exhibiting entirely normal CTT and HR-ARM. All others showed some abnormalities [11].
Motility Tests
Figure 1 illustrates our initial approach in examining possible relationships between age or gender and motility test results. We first examined the prevalence of abnormal test results in males compared to females. In the top left panel of Fig. 1 the prevalence of five different abnormal motility test results varied from 45 to 82%. When two values for prevalence are compared, if one value is outside the boundaries of the 95% confidence interval for the other value, the values are significantly different at P < 0.05.
Top panels. Prevalence of abnormal motility test results in males and females (left panel) and mean ages of subjects with or without an abnormal test result (right panel). Vertical bars give 95% confidence interval. Middle panels Values for CTT plotted versus the corresponding value for age. The solid line is the linear, least-squares regression line. The slope of the regression line is significantly different from zero by an F-test for males (P = 0.0006), but not for females (p = 0.441). Bottom panels. Cumulative distributions of ages for subjects with or without prolonged CTT. Results are from 91 males and 75 females
The prevalence of low anal squeeze pressure for females was significantly higher than that for males and the prevalence of low rectal sensation for males was significantly higher than that for females (both P < 0.05). The prevalence of prolonged CTT, low anal basal pressure and failed BET for males was not significantly different from corresponding values for females. Thus, there is wide variation in the prevalence of different abnormal motility test results, and there is no consistent difference between males and females for the prevalence of abnormal motility test results.
Since the mean age of male subjects 66 years (95% CI 64 to 68) was significantly higher than that for females 60 years (95% CI: 56 to 63), we considered that this age difference might mask a gender-related difference for at least some of the prevalence values illustrated in Fig. 1 top-left. To begin to explore this possibility, we calculated mean values for ages of subjects with and without an abnormal motility test result.
Figure 1 top right panel illustrates that the mean age of subjects stratified for the presence or absence of an abnormal motility test result ranged from 57 to 66 years. Except for the BET, the mean age of subjects with an abnormal motility test result was significantly higher than the mean age of those without the corresponding motility test abnormality. Even with the BET, the mean age of patients with a failed BET was higher than the mean age of those with a successful BET, but the difference was not significantly different. Thus, there was a clear association of older subjects with abnormal results for four of the five motility tests that we analyzed even though the range of mean ages of subjects for different motility tests was relatively narrow.
Colonic Transit Time (CTT)
Table 1 and Fig. 1 top panels show that the prevalence of prolonged CTT in males was not significantly different from that in females, but that the mean age of patients with prolonged CTT was significantly higher than that for those without. These data indicate that prolonged CTT tends to occur more frequently in older patients.
Since the prevalence of a prolonged CTT did not differ between males and females, but was associated with older patients, we examined the relationship between values of CTT and the corresponding ages for both males and females. Our thinking was that perhaps different relationships between values for CTT versus age between males and females might explain how the prevalence of a prolonged CTT can be similar for males and females with the mean age being higher with a prolonged CTT.
In Fig. 1 middle panels, the least-squares regression line for CTT versus age was significantly different from zero for males, but not for females. Thus, in males, age provides important information regarding CTT in that an increase in age of one year was associated with an increase in CTT of one hour. The panels in Fig. 1 middle also indicate how the prevalence of a prolonged CTT can be similar for males and females, with the mean age of patients being higher in those with a prolonged CTT. For males, values of CTT above 59 h tend to be concentrated above age 55 years and particularly above age 70 years, whereas for females, values above 59 h tend to be more widely distributed over values for age. These results are consistent with those in the bottom panels of Fig. 1.
Since a major objective of the present analyses was to examine the relationships of age to the prevalence of abnormal motility test results in males as compared to females, we calculated the cumulative distributions of age for patients with or without an abnormal motility test result, stratified by gender, as illustrated in the bottom panels of Fig. 1. These analyses can also quantify the distribution of age for prolonged CTT, referred to in our comments above, regarding regression plots of values of CTT versus age in the middle panels of Fig. 1.
In addition to the bottom panels in Fig. 1, Supplemental Figure S1 displays the cumulative distributions of age for males and females stratified for the presence or absence of an abnormal motility test result. Table 1 gives the number of patients, means and 95% confidence intervals for the cumulative distributions in Figs. 1 and S1.
A major advantage of cumulative distributions is that they provide a comprehensive visual analysis of the data that does not depend on a P-value. They also make it possible to understand the distribution of the data and easily identify patterns. In a figure displaying a cumulative distribution, the value on the Y-axis gives the probability of obtaining a value equal to or less than the corresponding value on the X-axis [14]. For example, in Fig. 1-bottom panels, the probability of a male with normal CTT being equal to or younger than 60 years of age is 42%. This is also the probability that the age of the next subject will be less than or equal to 60 years. The probability of a male with prolonged CTT being equal to or younger than 60 years of age is 20%. Again, this is also the probability that the age of the next subject will be less than or equal to 60 years The probabilities of being older than 60 years of age are 100 minus 42% or 20%, respectively.
The mean of the cumulative distribution is the expected value for the distribution. In Table 1, the mean (95% confidence interval) for males with prolonged CTT is 69.5 years (67.2 to 71.7) and for males without prolonged CTT is 62.6 years (58.6 to 66.6). If as pointed out above, one mean value is outside the boundaries of the 95% confidence interval for another mean value, the values are significantly different at P < 0.05.
Figure 1 top left panel and Table 1 show that the prevalence of prolonged CTT in males was not significantly different from that in females. Figure 1 bottom, however, illustrates that for both males and females, the mean for the cumulative distribution of age for subjects with prolonged CTT was significantly higher than that for subjects without prolonged CTT, indicating that prolonged CTT tended to occur in both older males and females. Also, for subjects with prolonged CTT as well as without prolonged CTT, the mean of the distribution of age for males was significantly higher than that for females (Table 1, Supplemental Figure S1).
Another advantage of displaying values for cumulative distributions is that they can identify a particular range of the distribution that includes the important differences. For example, Fig. 1 bottom left, illustrates two curves where the mean age for the curve for males with prolonged CTT is significantly higher than that for males without a prolonged CTT (Table 1). The curves show that the major differences are for males aged 45 to 65 years, even though the majority of values for prolonged CTT for males are above age 65 (Fig. 1 middle left. That is, the probabilities for males in this age range with prolonged CTT are lower than the corresponding probabilities for males without prolonged CTT indicating that males with a prolonged CTT have a lower probability of being younger (and a higher probability of being older) than males without a prolonged CTT.
Thus, cumulative distributions of age stratified for a normal or abnormal motility test result and for gender make it possible to identify the impact of both age and gender on the prevalence of abnormal test result for CTT when this impact is not apparent from values for prevalence and mean age of subjects with or without an abnormal test result.
Anal Basal Pressure
Table 1 and Fig. 1 top panels show that results with anal base pressure were similar to those for CTT. That is, the prevalence of low anal basal pressure in males was not significantly different from that in females, but that the mean age of patients with low anal base pressure was significantly higher than that for subjects without. These data indicate that low anal base pressure tends to occur more frequently in older subjects.
In the top panels in Fig. 2, the least-squares regression line for the relationship between anal base pressure and age was significantly different from zero for females but not for males. In females, but not males, age provided important information regarding values for anal base pressure, and an increase in age of one year was associated with a decrease in anal base pressure of 1.2 mmHg. These results are consistent with those in the bottom panels of Fig. 2.
Relationship of anal basal pressure to age in males and females with constipation. Top panels plot values for anal basal pressure versus the corresponding value for age. The solid line is the linear, least-squares regression line. The slope of the regression line is significantly different from zero by an F-test for females (P < 0.0001), but not for males (p = 0.387). Bottom panels give the cumulative distributions of ages for subjects with or without low basal pressure. Results are from 91 males and 75 females
Figure 2 bottom illustrates that for females, but not males, the mean of the cumulative distribution of age for low anal base pressure was significantly higher than that for no low anal base pressure (Table 1). The mean of the distribution of age for low anal base pressure for males did not differ from that for females, but the mean of the distribution of age for no low anal base pressure was significantly higher for males than for females (Supplemental Fig. 1, Table 1).
Thus, for anal base pressure, as was the case with CTT, cumulative distributions of age stratified for a normal or abnormal motility test result and for gender make it possible to identify the impact of both age and gender on the prevalence of abnormal test result for anal base pressure when this impact is not apparent from values for prevalence and mean age of subjects with or without an abnormal test result.
On the other hand, increasing age was associated with increasing values for CTT in males, but decreasing values for anal base pressure in females. Furthermore, for CTT, increasing age was associated with a higher probability of an abnormal motility test result in males, but for anal base pressure, increasing age was associated with a higher probability of an abnormal motility test result in females.`
Anal Squeeze Pressure
Table 1 and Fig. 1 top panels show that the prevalence of low anal squeeze pressure in females was significantly higher than that in males, and that the mean age of patients with low anal squeeze pressure was significantly higher than that for those without. These data indicate that low anal squeeze pressure tends to occur more frequently in older females.
In the top panels in Fig. 3, the least-squares regression line for the relationship between anal squeeze pressure and age was significantly different from zero for females, but not for males. In females, but not males, age provided important information regarding values for anal squeeze pressure, and an increase in age of one year was associated with a decrease in anal base pressure of 2.6 mmHg. These results are consistent with those in the bottom panels of Fig. 3.
Relationship of anal squeeze pressure to age in males and females with constipation. Top panels plot values for anal squeeze pressure versus the corresponding value for age. The solid line is the linear, least-squares regression line. The slope of the regression line is significantly different from zero by an F-test for females (P < 0.0001), but not for males (p = 0.223). Bottom panels give the cumulative distributions of ages for subjects with or without low squeeze pressure. Results are from 91 males and 75 females
Figure 3 bottom illustrates that for females, but not males, the mean of the cumulative distribution of age for low anal squeeze pressure was significantly higher than that for no low anal squeeze pressure (Table 1). On the other hand, the mean of the cumulative distribution of age for both low anal squeeze pressure and for no low anal squeeze pressure was significantly higher for males than for females (Supplemental Figure S1, Table 1).
Thus, in contrast to results with CTT and anal base pressure, both age and gender interact to influence the presence of an abnormal motility test result in ways that are consistent with values for the prevalence of low anal squeeze pressure in males and females, as well as the mean age of subjects with or without low anal squeeze pressure.
Rectal Sensation Test (RST)
Table 1 and Fig. 1 show that the prevalence of decreased rectal sensation in males was significantly higher than that in females, and that the mean age of subjects with decreased rectal sensation was significantly higher than that for subjects without, indicating that low rectal sensation tends to occur more frequently in older males.
In the top panels of Fig. 4, the least-squares regression line for the relationship between rectal sensation and age was not significantly different from zero for males or females, indicating that age does not provide any important information regarding rectal sensation per se in patients with CC. Figure 4 top does, however, provide important information in males regarding the probability of decreased rectal sensation. The top panels of Fig. 4 illustrate that for males there are 72 values (79%) above 40 mL, indicating low rectal sensation in contrast to 46 values (61%) for females. These different proportions for low rectal sensation are consistent with the results in Fig. 4 bottom.
Relationship of rectal sensation to age in males and females with constipation. Top panels plot values for rectal sensation versus the corresponding value for age. The solid line is the linear, least-squares regression line. The slope of the regression line was not significantly different from zero by an F-test for males (p = 0.479) or females (P = 0.318). Bottom panels give the cumulative distributions of ages for subjects with or without low rectal sensation. Results are from 91 males and 75 females
Figure 4 bottom illustrates that for males, but not females, the mean of the cumulative distribution of age for low rectal sensation was significantly higher than that for no low rectal sensation (Table 1). Further, the mean of the distribution of age for low rectal sensation but not that for no low rectal sensation was significantly higher for males than for females (Supplemental Figure S2, Table 1).
Thus, except for the slopes of the regression lines for rectal sensation not being significantly different from zero, results with rectal sensation agreed with those for anal squeeze pressure in that both age and gender interact to influence the presence of an abnormal motility test result in ways that are consistent with values for the prevalence of low rectal sensation in males and females, as well as the mean age of subjects with or without low rectal sensation.
Balloon Expulsion Test (BET)
Table 1 and Fig. 1 show that the prevalence of failed BET in males was not significantly different from that in females. The mean age of patients with a failed BET was higher than that of those with a successful BET; however, this difference was not statistically significant, probably because the smaller number of subjects in the successful BET group (n = 34) compared to the number of subjects in the failed BET group (n = 132) resulted in a much larger 95% confidence interval in the successful BET group. Since the BET was measured as success or failure, a linear regression analysis was not performed.
Figure 5 illustrates that for both males and females, the mean of the cumulative distribution for a failed BET was not significantly different from that for a successful BET (Table 1). The mean of the distribution for a failed BET, but not for a successful BET, was significantly higher for males than for females (Supplemental Figure S2, Table 1). Thus, cumulative distributions of age stratified for a normal or abnormal motility test result and for gender make it possible to identify the impact of both age and gender on the prevalence of abnormal test result for BET, when this impact is not apparent from values for prevalence and mean age of subjects with or without a failed BET.
The previous analyses of results in Figs. 1, 2, 3, 4 and 5 compared cumulative distributions of age between normal and abnormal results for a particular motility test and compared cumulative distributions of age between males and females for a particular motility test result. The data in Table 1 also illustrate that it is possible to compare distributions of age among different normal or abnormal motility test results for a particular gender.
A major finding when cumulative distributions are compared among different motility test results is that there are no consistent differences among the means for the cumulative distribution of age among different motility test results for gender or the presence or absence of an abnormal motility test result (Table 1). For example, in males, there were no significant differences for the means of the cumulative distribution of age among any abnormal or normal motility test results. For females, the means of the cumulative distribution of age for no decreased rectal sensation and for no failed BET were significantly higher than the means of the cumulative distribution of age for no low anal base pressure and for no low anal squeeze pressure. There were no significant differences between the mean cumulative distributions for other comparisons in females.
Symptoms
Although each subject rated symptom severity as “mild”, “moderate”, or “severe”, for the present analyses we rated symptoms as “present” or “absent”. As a result, a linear regression analysis was not possible for symptoms. Figure 6 left illustrates that the prevalence of four different symptoms varied from 21 to 91%. The prevalence of abdominal pain and incomplete evacuation for females was significantly higher than that for males. The prevalence of infrequent defecation and strain for females was not significantly different from corresponding values for males. Figure 6 right illustrates that the mean age of subjects stratified for the presence or absence of a symptom ranged from 57 to 66 years, the same range of ages as that for ages for motility test results in Fig. 1. The mean ages for abdominal pain and incomplete evacuation were significantly lower than corresponding mean values for no abdominal pain and no incomplete evacuation, respectively. The mean age for infrequent defecation was significantly higher than that for no infrequent defecation. The mean age for strain was not significantly different from that for no strain.
Abdominal Pain
Figure 6 left and Table 2 show that the prevalence of abdominal pain in females was significantly higher than that in males, and that the mean value for age for abdominal pain was significantly lower than the corresponding value for no abdominal pain. These data indicate that the abdominal pain tends to occur more frequently in younger females. Figure 7 illustrates that the mean for the cumulative distribution of age for males with abdominal pain was significantly higher than that for males without. In contrast, the mean for the cumulative distribution of age for females with abdominal pain was significantly lower than that for females without abdominal pain. In agreement with these findings, for subjects with abdominal pain, the mean of the cumulative distribution of age for males was significantly higher than that for females (Supplemental Figure S3, Table 2). Thus, with abdominal pain, in contrast to several analyses of motility test results, cumulative distributions of age stratified by gender or the presence or absence of abdominal pain were consistent with values for the prevalence of abdominal pain in males and females plus the mean age of subjects with or without abdominal pain.
Infrequent Defecation
Figure 6 and Table 2 show that the prevalence of infrequent defecation in males was significantly higher than that in females, and that the mean age of subjects with infrequent defecation was significantly higher than that for subjects without infrequent defecation. These data indicate that the infrequent defecation tends to occur more frequently in older males.
Figure 7 illustrates that the mean for the cumulative distribution of age for males with infrequent defecation was significantly higher than that for males without. Also, the mean for the cumulative distribution of age for females with infrequent defecation was not significantly different from that for females without. For subjects with, but not without infrequent defecation, the mean of the cumulative distribution of age for males was significantly higher than that for females (Supplemental Figure S3, Table 2). Thus, results for cumulative distributions of age stratified by gender or the presence or absence of infrequent defecation were consistent with values for the prevalence of a symptom in males and females plus the mean age of subjects with or without infrequent defecation.
One advantage of displaying values for cumulative distributions is illustrated in Fig. 7, where the mean age for the curve for males with infrequent defecation is significantly higher than that for males without. The curves, however, show that the major differences are for males aged 45 to 65 years. That is, the probabilities for males in this age range with infrequent defecation are lower than the corresponding probabilities for males without infrequent defecation, indicating that males with a infrequent defecation have a lower probability of being younger (and a higher probability of being older) than males without infrequent defecation.
Incomplete Evacuation
Figure 6 and Table 2 show that the prevalence of incomplete evacuation in females was significantly higher than that in males and that the mean value for age for incomplete evacuation was significantly lower than the corresponding value for no. These data indicate that incomplete evacuation tends to occur more frequently in younger females. Figure 7 illustrates that the mean for the cumulative distribution of age for females with incomplete evacuation was significantly lower than that for females without. In contrast, the mean for the cumulative distribution of age for males with incomplete evacuation was not significantly different from that for males without. In agreement with these findings, for subjects with incomplete evacuation, the mean of the cumulative distribution of age for males was significantly higher than that for females (Supplemental Figure S3, Table 2). Thus, results with incomplete evacuation agreed with those for abdominal pain, in that cumulative distributions of age stratified by gender or the presence or absence of incomplete evacuation were consistent with values for the prevalence of incomplete evacuation in males and females plus the mean age of subjects with or without incomplete evacuation.
Strain
Figure 6 and Table 2 show that the prevalence of strain in males was not significantly different from that in females and that the mean age of subjects with strain was significantly higher than that for subjects without. These data indicate that the infrequent defecation tends to occur more frequently in both older males and older females. Figure 7 illustrates that the mean for the cumulative distribution of age for males with strain was significantly higher than that for males without. In contrast, the mean for the cumulative distribution of age for females with strain was not significantly different from that for females without. Furthermore, for subjects with, but not without strain, the mean of the cumulative distribution of age for males was significantly higher than that for females (Supplemental Figure S3. Table 2). Thus, cumulative distributions of age stratified for age and for gender make it possible to identify the impact of both age and gender on the prevalence of abnormal test result when this impact is not apparent from values for prevalence of strain and mean age of subjects with or without strain.
The previous analyses of results in Fig. 7 compared cumulative distributions of age for the presence and absence of a particular symptom and compared cumulative distributions of age for males and females for the presence or absence of a particular symptom. The data in Table 2 also illustrate that it is possible to compare distributions of age among different symptoms for a particular gender. A major finding when cumulative distributions are compared among different symptoms is that there are no consistent differences among the different means for the cumulative distribution of age among different symptoms for gender or the presence or absence of a symptom (Table 2). For example, in males, the mean of the cumulative distribution of age for abdominal pain was significantly higher than that for the distribution of age for incomplete evacuation and for strain, but not for infrequent defection. For males with no symptoms, the mean of the cumulative distribution of age for incomplete evacuation was significantly higher than that for infrequent defecation, but was not significantly different from that for abdominal pain or strain. Also, for males with no symptoms, the mean of the cumulative distribution of age for abdominal pain was significantly higher than that for infrequent defecation.
For females, the mean of the cumulative distribution of age for abdominal pain was significantly lower than that for infrequent defecation and for strain, but was not significantly different from that for incomplete evacuation. For females with no symptoms, the mean of the cumulative distribution of age for infrequent defecation was significantly lower than that for abdominal pain and for incomplete evacuation, but was not significantly different from that for strain.
Discussion
This post hoc data analysis of a community-based cohort of subjects suffering from CC, examined the relationship among symptoms, age and gender, and various parameters measured in clinical practice, such as CTT, HR-HRM, RST, and BET. The study is unique, since it combines a sizeable set of data on CTT and HR-ARM and validates further the relationships (if any) among the variables assessed in such frequently used studies and symptoms. We found that there are significant age- and gender-related differences in symptoms, CTT, and various HR-HRM and other anorectal function and sensation measures that could guide the overall constipation management, using a multifaceted approach (i.e., laxatives, enemas, biofeedback, and pelvic floor physical therapy). This dataset enhances our previous findings revealing high prevalence of anorectal dysfunction in ambulatory patients with clinically undifferentiated CC, exhibiting areflexia, elevated basal anal sphincter pressure, decreased rectal sensation and failed balloon expulsion [11].
Several groups have observed an association of age and gender with values for anorectal and colonic motility tests in healthy subjects. Similarly, age and gender have been associated with values for anorectal and colonic motility tests, as well as symptoms in subjects with constipation and other disorders [8,9,10]. An important issue with nearly all published studies is that they have been based on subjects from a single study site. No matter how extensive the descriptions of the subjects, important questions will still arise regarding the extent to which subjects in one study are exchangeable with those in another. A major reason for studies occurring from single study sites may be that compared to funds available for clinical development of drugs, funds available for device studies are more limited. This, in turn, may result from the more extensive requirements for approval of drugs by the US Food and Drug Administration (FDA) compared to those for approval of medical devices [15]. An example of the difference in funding available for drug studies compared to device studies may be reflected in clinical trials listed on Clinicaltrials.gov. Entering search terms, “constipation” and”anorectal” returned 5 studies, while entering “constipation” and”lubiprostone”, a newer drug approved to treat constipation, returned 31 studies [16].
One objective of the present analyses was to compare (1) values for the prevalence of an abnormal motility test result or a symptom stratified by gender plus the mean age of subjects associated with the prevalence to (2) regression analyses of values for a motility test versus the corresponding age of the subject to (3) the cumulative distributions of age for normal and abnormal results for the same motility test. An important difference between the regression analyses and the cumulative distributions is that regression analyses examine values for the motility test per se, while cumulative distributions examine the same motility test values stratified for being normal or abnormal. Such comparisons might be important in helping to decide whether the range for normal values for a particular motility test result should vary with age and/or gender. Cumulative distributions for age stratified for gender and for a motility test result or symptom provide a comprehensive visual analysis of the data. The distributions give the probability that the stratified variable will be associated with an age equal to or less than a particular value and can also identify a particular range of the distribution that includes the important differences. As a result, the extent of the overlap of two distributions makes it possible for the reader to compare probabilities for a particular age stratified by age or gender to decide whether the differences are clinically important, regardless of any statistical comparisons of the data.
At times we found that cumulative distributions confirmed results from values for prevalence of an abnormal motility test result or a symptom and the mean age of subjects associated with the prevalence. This was the case for analyses of data for low anal squeeze pressure, decreased rectal sensitivity, abdominal pain, infrequent defecation and incomplete evacuation. At other times, we found that cumulative distributions could identify the impact of age and gender on the prevalence of a motility test result or symptom that was not apparent from values for prevalence and mean age of subjects associated with the prevalence. This was the case for prolonged CTT, low anal base pressure, failed BET, and strain.
We also performed regression analyses for motility test values versus age to explore possible changes in a particular motility test value with a change in age. In general, these analyses confirmed results from cumulative distributions of age stratified for motility results or gender. These results were not as helpful as those from cumulative distributions because they did not distinguish between normal and abnormal motility test results. Cumulative distributions, however, can show clear associations of abnormal as well as normal motility test results with age for both males and females for all motility test results analyzed.
Some [17] have reported correlation coefficients for plots of motility test results versus age; however, these coefficients only indicate how close the paired values are to a straight line. Correlation coefficients do not indicate the magnitude of a change in one variable that is associated with the magnitude of the change in the paired variable, and the same value for a correlation coefficient can be associated with lines having very different slopes. One striking feature of the present analyses as well as of a number of published reports, is the extensive variation in the relationships between gender or prevalence of a motility test result or symptom and age. Some of this variation may be attributable to a lack of reproducibility of motility test results. In one study of constipated subjects that considered test results defined as normal or abnormal, 79 percent of tests were not reproducible on a single repeat test [18]. Another source of variation may be related to the number of abnormal motility test results or symptoms experienced by a single individual. In the present study, 94% of subjects had more than one abnormal motility test result and 16% had abnormal results for all five motility tests. In addition, 95% of subjects reported more than one symptom and 22% reported all four symptoms.
It seems likely that a constipated subject with a single abnormal motility test result or a single symptom will have a different pathophysiology than a subject with multiple abnormal motility test results or symptoms. This phenomenon is not considered by the Rome IV consensus for functional constipation, or functional bowel disorders [4]. The same seems likely for the London Classification, which appears to focus on a single abnormal motility test result [7]. Finally, it seems possible that variation in the number of abnormal motility test results or symptoms in constipated subjects might account for the findings that a majority of subjects remained constipated after treatment with one of the newer treatments for constipation [19]. On the other hand, the variation in constipated subjects in the number of abnormal motility test results or symptoms might indicate important pathophysiological differences that respond to different therapeutic measures. The occurrence of different combinations of motility abnormalities with different symptom frequencies represent important challenges to investigators who conduct clinical trials of therapeutic agents for chronic constipation and seek to enroll a homogeneous population of study subjects. The variation in relatively small age-related and gender-related changes in values for abnormal motility test results indicates that it will not be necessary in clinical trials to stratify subjects with chronic constipation for age or gender.
The IAPWG has stressed that an abnormal HR-ARM is not necessarily a complete reflection of disease and a comprehensive pelvic floor evaluation to assess structure and function, such as endoanal ultrasound, MR defecography, rectal Barostat, or Functional Lumen Imagine Probe (FLIP) would provide a broader perspective [7]. Further, the IAPWG has not recommended specific, quantitative reference limits, but they describe findings in accordance with the upper and lower limits of “normal”, as we did in our study. The IAPWG also acknowledged that gender, multiparity and advanced age may have exerted a deleterious effect on anorectal motor and sensory dysfunction. For example, we do not consider the low anal pressures seen in our female cohort as solely contributing to the evacuation disorder, since they might simply represent a weakened pelvic floor and anal tone in the general context of sarcopenia. Although we have no data on pregnancy and vaginal delivery in the females of our study, advanced age and female gender significantly altered several measures of sensation and motor dysfunction, possibly related to the ubiquitous prevalence of many concurrent abnormalities in our cohort [11]. Further, many other details are not available in our female cohort. Specifically, we do not have data on duration of pregnancy, number of pregnancies and Cesarian section deliveries, times of vaginal deliveries, rates of episiotomies, etc. We also do not have anal ultrasound data to concurrently correlate with HR-ARM values of anal tone.
Our results also identify the occurrence of non-unique motility abnormalities in individual subjects. For example, the London Classification assigns abnormalities of anal pressure to a different phenotype from the phenotype that includes the balloon expulsion test. We found, however, that as many as 31.9% of subjects have abnormal values for both tests (data not shown). The prevalence of multiple abnormalities of colonic and anorectal motility and sensation in the same subject with constipation would be a limiting confounder. We therefore considered the possibility that it might be useful to examine any relationships between symptoms and anorectal motility and sensation abnormalities in our cohort.
Anorectal function testing has been used for many years as a guide in clinical decision making [20]. The hierarchical separation of the London classification into major abnormalities only seen in disease, minor and potentially of significance in symptomatic patients, or inconclusive, would objectively facilitate characterization and individualize treatment of CC, and lead to improved outcomes. We think that the present study provides another dimension, that of the relationship of the anorectal function and colonic transit findings to symptoms, age and gender, and its usefulness in decision making [10, 21].
The patients in our cohort represented a challenging group since they could not be clinically differentiated, exhibiting variable degrees of abdominal pain suggestive of IBS-C, infrequent urge to evacuate, suggestive of CIC, and straining and incomplete evacuation, suggestive of ED. Given the high prevalence of HR-ARM, RST and BET abnormalities, our cohort was ultimately managed by local means (gut-directed behavioral and pelvic floor therapy, enemas, and suppositories) when ED dominated, reassurance, antispasmodics, and fiber supplementation when CTT was normal, and combination strategies (oral osmotic and/or stimulant laxatives, behavioral and pelvic floor therapy, enemas, and suppositories, and/or surgery) when CTT delay was dominant. Unfortunately, the retrospective nature of this study could not provide reliable outcome data on the efficacy or comparative effectiveness of such approaches, based on our testing and findings, or even symptoms [22, 23]. Nevertheless, our subjects represent a unique group that was studied very carefully and with a high degree of granularity using state-of-the-art testing (WMC, HR-ARM, BET, and RST) to examine for slow-transit constipation and evacuation disorder. Other than the knowledge of the reported co-existing conditions affecting the enteric nervous system (ENS), we have no other way to quantify any neurologic dysfunction. No subjects had spinal cord injury or acute colonic dysmotility. All subjects were ambulatory and were studied electively because of their leading symptom, that of chronic constipation, to rule out slow-transit constipation. As noted in our previous report [11], 50% of the cohort did not have prolonged CTT. We did not measure luminal resistance due to left colonic hypermotility or myochosis since that would require colonic (not anorectal) manometry, which is generally a complex research tool.
Hormonal influences may play a role in post-menopausal women but, again, we have no hormonal measurements or details of prior obstetrical or gynecologic data in our cohort to provide additional insights. We postulate that the noted differences in anal sphincter competence reflect remote obstetrical trauma or sarcopenia, typically predominating in females. For example, we have found that patients with fecal incontinence have lower vitamin-D levels. Such patients are more likely to be females, Caucasian, older, and exhibiting increased numbers of chronic comorbidities, including GI functional and structural pathologies and, overall, significantly higher Carlson Comorbidity Index (CCI) (unpublished data). Prior compelling evidence supports a role for vitamin-D supplementation as an intervention to mitigate this chronic inflammatory process, in turn involved in frailty and muscle loss [24].
Of note, abdominal pain was least frequently, and straining was most frequently associated with a motility abnormality. Since abdominal pain has a very complex underlying pathophysiology, one could argue about the confidence level of this relationship. This indeed is an important point. We believe that our cohort was enriched by patients with chronic idiopathic constipation and evacuation disorder since both these conditions are associated with less abdominal pain (classically a feature of IBS-C). Only 59/166 patients in our cohort were deemed as fulfilling IBS criteria [11].
We have previously shown, that in most clinical therapeutic trials, a majority of patients treated with a newer agent remained constipated and that clinicians should anticipate a high probability that, with one of the newer treatments for constipation (such as with lubiprostone, methylnaltrexone, prucalopride, linaclotide, and naloxegol), a patient will remain constipated with persistent abdominal symptoms, and our current data revealing high proportion for ED, support this notion [20]. The key strength of our study is its community-based and pragmatic nature, derived from a stable cohort of patients followed by one clinician, allowing us to obtain high degree of granularity in their diagnosis, management, and follow-up, based on formal testing. Yet, several key weaknesses need to be brought forth: (a) Retrospective in nature, and small in sample size. As such, our data will require further and confirmation prospectively, on more patients undergoing WMC, HR-ARM with RST and BET, possibly combined with MR defecography, as part of a standardized protocol. (b) The select nature of our cohort. Our patients reported herein had more severe and refractory constipation that had not responded to medical therapy, implemented at the primary care setting, mostly comprising various osmotic and stimulant laxatives, sometimes combined with enemas and/or suppositories. (c) Patient preselection. The patients in the cohort represented a fraction of patients (approximately 10%) who underwent both WMC and HR-ARM in less than 1 month from each other and < 3 months from the request time. Mostly due to insurance non-authorization, 90% of our patients with undifferentiated CC did not have both studies performed. In other instances, positive findings in one or another study were considered adequate for decision making and further management and the other study was not pursued. (d) Lack of well-validated clinical questionnaires for both CC and ED that would link the frequency and severity of the clinical presentation to the test findings. A multi-institutional study involving patients with a wider spectrum of indications (i.e., recurrent pseudo-obstructions, fecal impactions, overflow diarrhea), underlying etiologies (neuropathic or myopathic, post-operative) and symptom intensity and frequency, and taking into consideration the effects of various concomitant drug therapies (carbidopa/levodopa, tricyclics, opioids, etc.) in a precise fashion would be needed to address these deficiencies. Finally, (e) Lack of information on the durability and reproducibility of WMC, HR-ARM, RST, and BET findings in such patients. A previous study had shown that only a minority of patients who underwent repeat anorectal manometry as analyzed by the London Classification had stable manometric findings, raising questions regarding the validity of a single manometric, motor or sensory measurement [18].
Critics could question ready application of our findings in clinical practice without data on how the findings predicted outcome or response to a given treatment modality. Although we agree with such a noble goal, we started by trying to understand the relative utilities of the tests, and the interrelationships of their respective findings to clinical and demographic data. The ability of our findings in predicting outcomes will depend on how outcomes are defined and quantified. Unfortunately. the currently used treatment modalities (such as laxatives, biofeedback, and pelvic floor physical therapy) are not easily accessible, practical, or affordable enough. We hope that our observations herein would serve as an early step for validation of future prospective trials.
In summary, this post hoc analysis of prospectively collected data in a carefully studied population of ambulatory subjects with CC raises some provocative questions about the interrelationship between age, gender, symptoms, and WMC, HR-ARM parameters, RST, and BET that will need to be addressed in larger prospective trials. More work will also be needed to demonstrate the value of such measurements as surrogate markers of clinical response, or as a response to gut behavioral and pelvic physical therapy, or a particular pharmacologic or surgical intervention as suggested in recent guidelines [25].
Key Messages
-
Various functional abnormalities are noted upon colonic transit and anorectal manometry testing (London classification) in patients with chronic constipation, but their relationship to age and gender is unclear.
-
Subjects suffering from chronic constipation exhibit significant age- and gender-related differences in symptoms, colon transit times, various high-resolution anorectal manometry and other anorectal function and sensation measures.
-
Full functional assessment could guide the overall constipation management, using a multifaceted approach (i.e., laxatives, enemas, biofeedback, and pelvic floor physical therapy), while posing opportunities and challenges in therapeutic clinical research trials.
References
Mearin F, Lacy BE, Chang L et al. Bowel disorders. Gastroenterology. 2016. https://doi.org/10.1053/j.gastro.2016.02.031.
Whitehead WE, Wald A, Diamant NE et al. Functional disorders of the anus and rectum. Gut 1999;45:Ii55–Ii59.
Sommers T, Petersen T, Singh P et al. Significant morbidity and mortality associated with fecal impaction in patients who present to the emergency department. Dig Dis Sci. 2019;64:1320–1327. https://doi.org/10.1007/s10620-018-5394-8.
Aziz I, Whitehead WE, Palsson OS et al. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev Gastroenterol Hepatol. 2020;14:39–46. https://doi.org/10.1080/17474124.2020.1708718.
Camilleri M, Ford AC, Mawe GM et al. Chronic constipation. Nat Rev Dis Primers. 2017;3:17095. https://doi.org/10.1038/nrdp.2017.95.
Rao S, Hatfield R, Soffer E et al. Manometric tests of anorectal function in healthy adults. Am J Gastroenterol. 1999;94:773–783.
Carrington EV, Heinrich H, Knowles CH et al. The international anorectal physiology working group (IAPWG) recommendations: Standardized testing protocol and the London classification for disorders of anorectal function. Neurogastroenterol Motil. 2020;32:e13679. https://doi.org/10.1111/nmo.13679.
Lucak S, Lunsford TN, Harris LA. Evaluation and treatment of constipation in the geriatric population. Clin Geriatr Med. 2021;37:85–102. https://doi.org/10.1016/j.cger.2020.08.007.
Nojkov B, Baker JR, Chey WD et al. Age- and gender-based differences in anorectal function, gastrointestinal symptoms, and constipation-specific quality of life in patients with chronic constipation. Dig Dis Sci. 2023;68:1403–1410. https://doi.org/10.1007/s10620-022-07709-z.
Jameson JS, Chia YW, Kamm MA et al. Effect of age, sex and parity on anorectal function. Br J Surg. 1994;81:1689–1692.
Triadafilopoulos G, Lee M, Neshatian L. High prevalence of anorectal dysfunction in ambulatory patients with chronic constipation, regardless of colon transit time. Dig Dis Sci. 2023. https://doi.org/10.1007/s10620-023-08072-3.
Rosa-E-Silva L, Gerson L, Davila M et al. Clinical, radiologic, and manometric characteristics of chronic intestinal dysmotility: the Stanford experience. Clin Gastroenterol Hepatol. 2006;4:866–873.
Saad RJ. The wireless motility capsule: a one-stop shop for the evaluation of GI motility disorders. Curr Gastroenterol Rep. 2016;18:14.
Sheskin DJ. The cumulative frequency distribution. p35. Handbook of Parametric and Nonparametric Statistical Procedures, 4th edn. Boca Raton: Chapman & Hall/CRC; 2007.
Gelijns AC. Comparing the Development of Drugs, Devices and Clinical Procedures. P147–201. Modern Methods of Clinical Investigation. http://www.nap.edu/catalog/1550.html.
https://clinicaltrials.gov. Accessed 10-6-2023
Cali RL, Blachford GJ, Perry RE et al. Christensen MA. Normal variation in anorectal manometry. Dis Colon Rectum. 1992;35:1161–1164.
Triadafilopoulos G, Clarke JO, Kamal A et al. Intra-subject variability in high resolution anorectal manometry using the London classification: diagnostic and therapeutic implications. Dig Dis Sci. 2022;67:5014–5018.
Sonu I, Triadafilopoulos G, Gardner JD. Persistent constipation and abdominal adverse events with newer treatments for constipation. BMJ Open Gastroenterol. 2016;3:e000094. https://doi.org/10.1136/bmjgast-2016-000094).
Camilleri M, Brandler J. Refractory constipation: how to evaluate and treat. Gastroenterol Clin North Am. 2020;49:623–642.
Barnett JL, Hasler WL, Camilleri M. American Gastroenterological Association medical position statement on anorectal testing techniques. Gastroenterology 1999;116:732–7600.
Rao SS, Benninga MA, Bharucha AE et al. ANMS-ESNM position paper and consensus guidelines on biofeedback therapy for anorectal disorders. Neurogastroenterol Motil. 2015;27:594–609.
Chiarioni G, Whitehead WE, Pezza V et al. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology 2006;130:657–664.
Girgis CM. Vitamin D and skeletal muscle: emerging roles in development, anabolism and repair. Calcif Tissue Int. 2020;106:47–55.
Chang L, Chey WD, Imdad A et al. American Gastroenterological Association-American College of Gastroenterology Clinical Practice Guideline: Pharmacological Management of Chronic Idiopathic Constipation. Gastroenterology 2023;164:1086–1106.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no Conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Triadafilopoulos, G., Gardner, J.D. Relationship of Age and Gender to Motility Test Results and Symptoms in Patients with Chronic Constipation. Dig Dis Sci 69, 1302–1317 (2024). https://doi.org/10.1007/s10620-024-08314-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-024-08314-y