Abstract
Background and Aims
There is a paucity of research on the use of the electronic health record (EHR) by gastroenterology and hepatology providers and its effect on work–life balance. Our aim was to study the after-hour EHR work completed among providers within a multispecialty academic practice.
Methods
Time spent completing EHR tasks during evening hours (7p-7a) and days off was prospectively recorded for 35 providers over six consecutive months at a single center. Type and time of EHR tasks completed were compared based on subspecialty, academic degree, academic track category, identified gender, and number of weekly assigned clinical days worked. Prior to the data collection, providers filled out a survey regarding EHR use, work hours, and work–life balance.
Results
All providers used EHR during evening hours and during days off. The total mean after-hours time spent completing EHR tasks was 18.4 m (± 13.0) per day and 45.0 m (± 25.8) during days off. There was significant variation in the daily mean after-hours time spent completing EHR tasks among subspecialties, range 45.3 m (± 27.1) (advanced endoscopy)-28.7 m (± 22.7) (hepatology), and among providers who work clinically > 7.5 days per week versus those who do not, 42.1 m (± 25.7) vs 30.0 m (± 14.0). The most common after-hours EHR task was note completion. 83% providers reported being unable to complete EHR tasks during allotted workday time and 87% report that EHR tasks interfered with family life; 74% with social life.
Conclusion
Gastroenterology and hepatology providers spend a significant amount of after-hour time completing EHR tasks which is perceived to interfere with family/social life.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decade, there has been a rapid adoption of Electronic Health Record (EHR) systems by US hospitals [1]. EHRs have the potential to improve patient care but, with this adoption, there has been a contemporaneous increase in healthcare provider burnout [2,3,4]. Burnout, a syndrome which involves feelings of work-related exhaustion, stress, depersonalization, and dissatisfaction, can lead to a decrease in patient care quality and provider productivity [5,6,7,8]. Providers who report feelings of burnout have a decreased sense of job satisfaction, higher rate of substance abuse, higher rates of medical errors, and more malpractice claims [6, 9, 10]. Greater than 50% of US physicians report feelings of burnout [11, 12]. EHR-related work demands are a significant contributor toward healthcare provider burnout and attrition [13, 14]. Providers report spending up to two hours daily completing EHR-related tasks outside of normal allotted office hours [15].
The rate of provider burnout varies significantly among subspecialties [2, 4, 6, 16]. The field of gastroenterology and hepatology encompasses the care of a broad array of diseases and has physicians and non-physician providers with markedly disparate areas of expertise leading to significantly different practice workflows. Similar to other medical subspecialties, gastroenterology and hepatology providers spend up to one hour of EHR-related work associated with each hour of face-to-face patient contact [17]. There are no large studies, however, evaluating after-hour EHR-related work demands among the various subspecialties within gastroenterology and hepatology and the perceived impact on work–life balance.
Given the known contribution of EHR work demands on provider burnout as well as the known variation in the rates of burnout among different subspecialties, the aim of our study was to evaluate the usage patterns of EHR work among providers within a large tertiary care academic gastroenterology and hepatology division and to assess the perceived influence of after-hour EHR work on work–life balance. The subsequent goal of this study is to identify potential workflow interventions to help mitigate gastroenterology and hepatology provider burnout and lead to improved patient care and provider work-related satisfaction.
Methods
Electronic health record use and tasks completed by 35 providers within a multispecialty academic gastroenterology and hepatology division between 9/1/19 and 2/29/20 using audit log data from Epic (Epic Systems Corporation) were prospectively collected and analyzed from a single center in Madison, Wisconsin. The multispecialty academic group includes providers who specialize in inflammatory bowel disease, hepatology, interventional/advanced endoscopy, genetics, esophagology, and general gastroenterology. The program has an accredited fellowship as well as fourth-year fellowships in inflammatory bowel disease, hepatology, and interventional/advanced endoscopy. The practice completes approximately 26,000 endoscopic procedures and sees approximately 25,000 patients in the outpatient/inpatient setting annually. EHR time spent on specific tasks as well as types of tasks completed per provider was tabulated by a previously validated Epic event logging system [18]. Quantitative logged data included the time of day, day of the week, provider-specific clinical work day assignment, and daily duration of EHR for each provider. After-hours work was defined as work-related tasks completed between 7 pm and 7 am, Monday–Friday. Work-related tasks completed during Saturday, Sunday, or a federal holiday was classified as work completed during days off. Qualitative EHR-specific task data included note completion, patient correspondence, patient-related message response, pre-chart analysis, pathology follow-up, and order placement for each provider. The quantitative and qualitative data were compared based on the following variables: provider subspecialty, specific career track, physician vs non-physician provider, half days spent doing clinical work, and identified gender. Physician providers within the group are segregated into three different career paths: academic (completing between 2- and 7.5-day sessions of clinical work per week), clinical (completing 9.5-day sessions per week), and blended (completing 8.5-day sessions per week). The faculty did not use medical scribes. Providers did not receive additional compensation for working after-hours or from home. Faculty newly starting within our practice during the study period, gastroenterology and hepatology fellows, contracted physicians and pediatric gastroenterology, and hepatology providers were excluded from the study analysis.
Prior to the study onset, all providers within the division were asked to complete a questionnaire which incorporated questions from a previously validated survey designed to assess impact of health information technology on provider job satisfaction [19, 20]. Providers indicated their answers on a 4-point scale in addition to responding to specific questions regarding their individual EHR use. Lastly, providers were asked to indicate their demographics and academic career path.
Statistical analysis was performed using a Student’s t test with a two-sided P value to compare means and a chi-square test to assess categorical values. Statistical significance was consider for P values < 0.05. The study was considered exempt by the University Institution Review Board.
Results
EHR use and practices for 35 gastroenterology and hepatology providers were examined over a 6-month period. The providers’ characteristics and demographic information are summarized in Table 1. The total mean after-hours daily time spent on completing EHR tasks was 33.6 min (m) (± 19.0) per day with a range of 7–91 m. Approximately 14% (5/35) of providers spent > 1 h per day on average after work hours completing EHR-related tasks. The mean daily time working on EHR during evening hours was 18.4 m (± 13.0). 23% (8/35) of providers spent greater than 30 min working on the EHR from 7PM-7AM with the highest provider working 53 min nightly on EHR tasks. The mean time spent during days off was 45.0 m (± 25.8). 23% (8/35) of providers spent greater than 60 min of working on EHR task on off-days with the highest provider working a mean 141 min on each off-day.
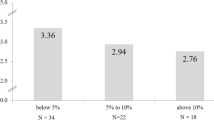
There was a significant variation in the daily mean after-hours total time spent completing EHR tasks among subspecialties: advanced endoscopy 45.3 m (± 27.1), GI genetics 43.8 (± 20.6), inflammatory bowel disease 33.0 m (± 12.7), general gastroenterology 31.8 m (± 20.2), esophagology 29.2 m (± 9.7), and hepatology 28.7 m (± 22.7), P < 0.01 (Fig. 1). Providers who work clinically > 7.5 days of sessions per week spent significantly more total after-hours daily time on EHR tasks compared to those who work clinically \(\le \)7.5 days per week, 42.1 m (± 25.7) vs 30.0 m (± 14.0), P < 0.01. There was no significant variation in the daily mean after-hours time spent completing EHR tasks between non-physician providers 36.1 m (± 26.6) vs physicians 32.6 m (± 19.3) P = 0.28, and male 35.6 m (± 20.2) vs female 31.8 m (± 23.4) P = 0.21 providers.
The most common after-hour EHR tasks were completing notes 31.8 m (± 26.7), pre-visit chart review 23.1 m (± 12.4), managing patient EHR messages 16.9 m (± 7.0), and placing orders 5.6 m (± 3.7). The mean number of daily patient messages received was 30.5 (± 11.5). There was a significant difference in the mean number of patient messages received per day by subspecialty: inflammatory bowel disease 43.2 (14.9), hepatology 31.2 (9.2), advanced endoscopy 30.2 (7.9), esophagology 28.0 (5.4), general GI 26.8 (7.1), GI genetics 21.7 (6.5), (Range 12.9–62.6) P < 0.01 (Fig. 2).
All gastroenterology and hepatology providers were electronically sent the questionnaire on EHR use. 65% (23/35) of the providers completed the survey. The administrated survey results revealed that 100% of the respondents use remote EHR access from home with 83% (19/23) reporting the reason for remote access being unable to complete EHR tasks during allotted workday time. 87% (20/23) of the providers agreed or strongly agreed the EHR added to daily workflow frustration. 43% (10/23) of the providers reported the time spent on EHR use at home was excessive. No providers reported that there was optimal time for EHR documentation during the time allotted during the workday, 22% (5/23) reported it was satisfactory, and 78% (18/23) noted the time allotted was poor or marginal. 52% (12/23) of the providers agreed or strongly agreed the EHR improved clinical workflow and 61% (14/23) reported the EHR improved patient care. 17% (4/23) of providers agreed the EHR improved job satisfaction, while 83% (19/23) disagreed or strongly disagreed. 83% (19/23) reported the EHR improved communication among healthcare providers. 87% (20/23) responded that the EHR interferes with personal/family time and 74% (17/23) with social time/life (Table 2).
Discussion
Our study indicated a significant amount of gastroenterology and hepatology provider time spent after-hours completing EHR tasks. This finding is similar to the previous studies for other subspecialties [14,15,16,17,18]. Electronic Health Records have clear benefits and have improved aspects of patient care since their rapid adoption over the past two decades [1]. Unfortunately, physicians have identified EHR as a significant contributor to provider burn out [3, 21]. This after-hour workload likely contributes to work–life imbalance and career dissatisfaction. Similar to other studies, our findings revealed a perceived influence of after-hour work on work–life balance [3, 4]. It is therefore of paramount importance to understand the complexities of after-hours EHR provider tasks to implement organizational strategies for workload support.
Our study revealed a significant variation in after-hours EHR use among our providers. Previous studies have shown a significant variation in EHR usage among medical and surgical subspecialties [22]. As a specialty, gastroenterology and hepatology is unique as it involves truly disparate subspecialties including hepatology, motility, inflammatory bowel disease, general gastroenterology, and advanced endoscopy. Each of these subspecialties has unique workflows and practice patterns. Our study, first and foremost demonstrated that all gastroenterology and hepatology providers completed after-hours EHR tasks and the vast majority perceived EHR tasks as interfering with family and social time. Notably, our study revealed a variation among the daily after-hours work completed among our providers with advanced endoscopy providers completing the most and hepatology providers the least. It is likely this difference is secondary to the influence of gastroenterology procedures leading to differences in daily practice workflows. In addition, the patient populations cared for within these subspecialties have different levels of clinical needs. This difference in practice patterns even within a single multispecialty practice is significant and should be recognized in order to implement tailored strategies to decrease provider EHR use and potential provider burn out.
Within our group, 16% of our faculty are within the academic track, 10% are within the clinical tract, and a majority, 74%, are within the blended career track. There was not a significant difference in the amount of EHR after-hours work between career tracks. Not surprisingly, gastroenterology providers who work clinically with patients > 7.5 days per week, clinical or blended career track, spent approximately 40% more total after-hours daily time on EHR tasks compared to those who work clinically ≤ 7 per week, academic track. This is likely due to the weekly workflow demands of more clinically active providers leading to after-hour work requirements for the completion of all the requested tasks. In addition, more clinically active providers have a larger volume of EHR tasks, i.e., note completion, order entry, patient messages, and result notifications, compared to less clinically active providers. Factors known to play a role in provider burnout include increasing work demands of the electronic health record and production pressure [23]. This increase in after-hours EHR work associated with increasing clinical demands should be taken into consideration when developing providers’ schedules.
There was a significant variation in the mean daily number of patient messages received during working and non-working hours among the subspecialties with IBD providers and hepatologists receiving the most and general GI and GI genetics receiving the least (range 12.9–62.6). Approximately 46% of providers received > 30 patient messages per day and 9% of the providers received > 50 patient messages per day. This significant variation and range observed is likely due to the inherent differences in the patient populations cared for by these providers. In addition, there are subtle differences in the clinic workflows for these subspecialty practices. The number of patient messages received per day did not appear to correlate with after-hours EHR time. However, a recent study revealed that healthcare providers with high volumes of patient-related messages had approximately four times the odds of burnout compared to those with the least [24].
The survey results revealed that all responding providers use remote EHR access. The most common reason, 83% of providers gave for using remote EHR access was to enable the provider to complete tasks which were unable to be completed during the allotted time during the workday. This is higher than previously reported in other studies [19]. It is possible that the procedural demands associated with gastroenterology and hepatology practice limit the allotted daytime work to complete alternate tasks, as minimal time is saved during the work day for EHR completion. Almost 90% of responding providers reported that interactions with the EHR led to frustration and time spent completing EHR tasks were modest or excessive. This is similar to previous studies which showed approximately 70% of providers experience EHR-related stress [19]. In addition, only 17% reported the EHR improved job satisfaction. Although, most, 83% of providers felt the EHR improved communication, 87% reported the EHR interfered with time with family or personal time. Lastly, for the academic tenure track faculty, 84% spent more time after-hours or during days off completing EHR tasks relative to research-related activities. Patients now often expect rapid responses to messages including explanations for radiologic, laboratory, and pathology results; medication renewal or change requests; and referrals and direct electronic provider clinical communications. In addition, health institutions often require rapid completion of all medical documentation. This increasing provider EHR workload contributes to after-hours work and therefore to provider burnout.
It has been recommended that healthcare organizations assess for EHR-related stress among their providers and implement targeted interventions to prevent provider burnout and excess EHR use [19, 22, 25]. Similar to other studies, the most common after-hours EHR task for our providers was note completion [18]. Insufficient time to complete documentation has been shown to be the leading predictor of provider burn out [19]. Scribes have been shown to decrease the burden of provider documentation, improve provider productivity, and improve provider satisfaction [26,27,28]. Another potential organizational tool to decrease provider burn out includes using a team-based care approach, which entails delegating some EHR clinical tasks to members of the healthcare team [29]. In addition, provider-specific workflows can be changed to allow for increased time to complete documentation during the work day [30]. Lastly, creating and adopting an efficient, optimized, user-friendly provider EHR interface can improve provider as well as patient satisfaction and decrease provider burn out [13, 14, 31,32,33,34].
A significant limitation of our study was that it was conducted at a single center with a limited sample size. While our findings are similar to other studies on EHR use, the workflows used at one center are unique. In addition, our study was completed at an academic center and might not apply to a private practice setting. Larger multi-center studies are needed to more accurately evaluate after-hour EHR use among gastroenterology and hepatology providers. In addition, future studies are needed to further identify specific factors contributing to after-hour provider work.
In conclusion, our study revealed that gastroenterology and hepatology providers, similar to other medical and surgical subspecialties, spend a significant amount of after-hours time completing EHR tasks. In addition, completing EHR tasks led to provider frustration and after-hour EHR time was felt to interfere significantly with home and family time, contributing to provider burn out. There was a significant variation in the amount of after-hours EHR work completed among subspecialties within a single practice. For future studies, this information will be used to identify potential workflow interventions to help mitigate gastroenterology and hepatology provider burnout and lead to improved patient care and provider work-related satisfaction. It is of paramount importance that all healthcare organizations regularly assess for EHR-related stress among their providers and implement effective changes to improve both provider satisfaction and patient care.
References
Henry J, Pylypchuk Y, Searcy T, et al. Adoption of Electronic Health Record Systems among U.S. Non-Federal Acute Care Hospitals: 2008–2015. ONC Data Brief 35; 2016.
Shanafelt TD, Boone S, Tan L et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1322–1385.
Friedberg MW, Chen PG, Van Busum KR et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q. 2014;3:1.
Shanafelt TD, Hasan O, Dyrbye LN et al. Changes in burnout and satisfaction with work-life balance in physicians and the general UW working population between 2011 and 2014. Mayo Clin Proc. 2015;90:1600–1613.
West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283:516–529.
Shanafelt TD, Balch CM, Bechamps G et al. Burnout and medical errors among American surgeons. Ann Surg 2010;251:995–1000.
Williams ES, Manwell LB, Konrad TR et al. The relationship of organizational culture, stress, satisfaction, and burnout with physician-reported error and suboptimal patient care: results from the MEMO study. Health Care Manage Rev 2007;32:203–212.
Salyers MP, Bonfils KA, Luther L et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med 2017;32:475–482.
McCain RS, McKinley N, Dempster M et al. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad Med J 2018;94:43–47.
Chen KY, Yang CM, Lien CH et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci 2013;10:1471–1478.
Linzer M, Visser MR, Oort FJ et al. Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med 2001;111:170–175.
Allegra CJ, Hall R, Yothers G, Prevalence of burnout in the U.S. oncology community: results of a,. survey. J Oncol Pharm Pract/Am Soc Clin Oncol 2003;2005:140–147.
Melnick E, Dyrbye L, Sinsky C et al. The Association Between Perceived Electronic Health Record Usability and Professional Burnout Among US Physicians. Mayo Clin Proc. 2020;95:476–487.
Shanafelt TD, Dyrbye LN, Sinsky C et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016;91:836–848.
Sinsky C, Colligan L, Li L et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165:753–760.
Shanafelt TD, West CP, Sloan JA et al. Career fit and burnout among academic faculty. Arch Intern Med 2009;169:990–995.
Ramrakhiani N, Morikawa C, Shetler K. Gastroenterology Providers Spend an Additional 45–50 Minutes of Electronic Health Records Per Hour of Scheduled Time. Clin Gastroenterol Hepatol. 2021;19:1489–1490.
Arndt BG, Beasley JW, Watkinson MD et al. Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Ann Fam Med. 2017;15:419–426.
Gardner RL, Cooper E, Haskell J et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc. 2019;26:106–114.
Baier RR, Gardner RL, Buechner JS et al. Creating a survey to assess physicians’ adoption of health information technology. Med Care Res Rev 2012;69:231–234.
Linzer M, Poplau S, Babbott S et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med 2016;31:1004–1010.
Redd TK, Doberne JW, Lattin D, et al. Variability in Electronic Health Record Usage and Perceptions among Specialty vs. Primary Care Physicians. AMIA Annu Symp Proc. 2015 Nov 5;2015:2053–62.
Kuhn CM, Flanagan EM. Self-care as a professional imperative: physician burnout, depression, and suicide. Can J Anaesth. 2017;64:158–168.
Hilliard RW, Haskell J, Gardner RL. Are specific elements of electronic health record use associated with clinician burnout more than others? J Am Med Inform Assoc. 2020;27:1401–1410.
Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet 2009;374:1714–1721.
Martel ML, Imdieke BH, Holm KM et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center Experience. Jt Comm J Qual Patient Saf 2018;44:238–249.
Bank AJ, Obetz C, Konrardy A et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res 2013;5:399–406.
Koshy S, Feustel PJ, Hong M, Kogan BA. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urology 2010;184:258–262.
Hopkins K, Sinsky CA. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014 Nov-Dec;21:23–9
Shanafelt TD, Noseworthy JH. Executive leadership and physician wellbeing: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc 2017;92:129–146.
Krist AH, Beasley JW, Crosson JC et al. Electronic health record functionality needed to better support primary care. J Am Med Inform Assoc 2014;21:764–767.
Collier R. Rethinking EHR interfaces to reduce click fatigue and physician burnout. CMAJ. 2018;190:E994–E995.
Marmor RA, Clay B, Millen M et al. The Impact of Physician EHR Usage on Patient Satisfaction. Appl Clin Inform. 2018;9:11–14.
Downing NL, Bates DW, Longhurst CA. Physician Burnout in the Electronic Health Record Era: Are We Ignoring the Real Cause? Ann Intern Med. 2018;169:50–51.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benson, M., Gopal, D. & Pfau, P. Electronic Health Record Work Demands for Gastroenterology and Hepatology Providers: A Prospective Use Analysis and Survey Study. Dig Dis Sci 68, 1218–1225 (2023). https://doi.org/10.1007/s10620-022-07691-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07691-6