Abstract
Background
Peroral cholangioscopy (POC)-guided lithotripsy is an effective treatment for difficult biliary stones. A clear definition of factors associated with the efficacy of POC-guided lithotripsy in one session and the performance of electrohydraulic lithotripsy (EHL) and laser lithotripsy (LL) have not clearly emerged.
Methods
This was a non-randomized prospective multicenter study of all consecutive patients who underwent POC lithotripsy (using EHL and/or LL) for difficult biliary stones. The primary endpoint of the study was the number of sessions needed to achieve complete ductal clearance and the factors associated with this outcome. Secondary endpoints included the evaluated efficacies of LL and EHL.
Results
Ninety-four patients underwent 113 procedures of EHL or LL. Complete ductal clearance was obtained in 93/94 patients (98.94%). In total, 80/94 patients (85.11%) achieved stone clearance in a single session. In the multivariate analysis, stone size was independently associated with the need for multiple sessions to achieve complete ductal clearance (odds ratio = 1.146, 95% confidence interval: 1.055–1.244; p = 0.001). Using ROC curves and the Youden index, 22 mm was found to be the optimal cutoff for stone size (95% confidence interval: 15.71–28.28; p < 0.001). The majority of the patients (62.8%) underwent LL in the first session. Six patients failed the first session with EHL after using two probes and therefore were crossed over to LL, obtaining ductal clearance in a single additional session with a single LL fiber. EHL was significantly associated with a larger number of probes (2.0 vs. 1.02) to achieve ductal clearance (p < 0.01). The mean procedural time was significantly longer for EHL than for LL [72.1 (SD 16.3 min) versus 51.1 (SD 10.5 min)] (p < 0.01).
Conclusions
POC is highly effective for difficult biliary stones. Most patients achieved complete ductal clearance in one session, which was significantly more likely for stones < 22 mm. EHL was significantly associated with the need for more probes and a longer procedural time to achieve ductal clearance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic retrograde cholangiopancreatography (ERCP) is the standard method for the management of biliary stones [1,2,3,4]. More than 50% of ERCPs are performed for biliary diseases, with such cases predominantly involving common bile duct stones. Conventional techniques, including endoscopic sphincterotomy (EST) with balloon or basket-assisted stone removal, endoscopic papillary large balloon dilation (EPLBD), and mechanical lithotripsy (ML), have success rates up to 95%. However, in 10–15% of cases, these methods may fail [1,2,3]. Biliary stones that are unable to be extracted by such methods can be considered “difficult biliary stones” [1,2,3]. In the past, these difficult-to-remove stones needed multiple procedures, namely extracorporeal shock wave lithotripsy (ESWL), or even more invasive methods for complete ductal clearance [1, 2, 5].
Peroral cholangioscopy-guided electrohydraulic lithotripsy (EHL) and Holmium laser lithotripsy (LL) were first introduced in the 1980s for difficult stones [6, 7]. Although these procedures were shown to be effective in these clinical scenarios, such methods produce high energy levels; consequently, there is the requirement for a clear vision of the bile duct to avoid serious lesions. Traditionally, peroral cholangioscopy (POC) with the “mother–baby” system, where the cholangioscope is inserted through the therapeutic channel of the duodenoscope, has been utilized [8]. However, this process has several limitations, since the equipment is fragile and complex, requires the coordination of two experienced endoscopists, and allows limited steerability and maneuverability of the cholangioscope, leading to limited field visualization [1, 2, 9].
In the past few years, a single-operator cholangioscopy (SOC) system has been introduced, allowing for a more routine use of these technologies [10]. Furthermore, this device has been recently improved, with the second-generation digital system now allowing for superior visualization of the biliary system when compared with the original one [2, 9].
With the emergence and availability of EHL and LL guided by SOC in the management of difficult biliary stones, conventional techniques have become less popular. EHL and LL are useful tools to fragment large stones inside the bile duct, thus facilitating their extraction [2, 11]. Recent reports have suggested that SOC-guided EHL and LL are safe and effective techniques for the treatment of difficult biliary stones, with success rates ranging between 77–100 and 64–97%, respectively, and adverse-event rates of 2.9% to 13% [2, 9, 11,12,13,14,15,16]. Two recent studies have suggested that although EHL and LL are associated with similar overall fragmentation rates and adverse events, LL is associated with shorter procedural times and a higher single-session fragmentation rate [17, 18]. Furthermore, EHL employs a probe with limited life, which has the same price (350–400 euros per probe) as a LL fiber, and it is unclear how the limited duration of the EHL probe affects ductal clearance, the use of more probes or more sessions (raising the costs), or the need for conversion from the EHL technique to an LL technique. Furthermore, it is unclear how different localizations of difficult stones may affect ductal clearance in a single session, and finally, there is scarce information about factors affecting ductal clearance in a single session [16,17,18].
Therefore, we conducted a prospective national multicenter study to evaluate the efficacy and safety of SOC-guided lithotripsy using LL or EHL in patients with difficult biliary stones, aiming to evaluate the number of sessions needed to achieve complete ductal clearance and the factors associated with the outcome, as well as to assess the efficacy of LL and EHL.
Methods
Patients and Setting
This was a prospective, national, multicenter study of all consecutive patients who underwent single-operator cholangioscopy-guided lithotripsy for the management of difficult biliary stones between January 2017 and September 2020.
The following inclusion criteria were used in this study: (1) patients with 1 or more biliary stones that failed treatment by mechanical lithotripsy and/or balloon sphincteroplasty in a previous session or during the first ERCP session; (2) impacted stones; and (3) stones in difficult locations—cystic stump or intrahepatic bile ducts (IHBDs).
Patients with distorted anatomies, malignant strictures, and bleeding diatheses were excluded from the study.
This study was conducted at 5 Portuguese University-affiliated hospitals and one large district hospital. This study was conducted in compliance with the International Conference on Harmonization guidelines for Good Clinical Practice (E6) and the 2013 Declaration of Helsinki. All of the patients provided informed written consent before their procedures. The ethics committee at each institution approved this observational study (see below).
End Points and Definitions
The primary endpoint of the study comprised the number of sessions needed to achieve clinical success, which was defined as complete ductal clearance confirmed by POC associated with an occlusion cholangiogram, and the factors associated with clinical success. Secondary endpoints considered were safety and adverse events, the role of the number and location of stones in achieving clinical success, and the efficacy of the two techniques used for cholangioscopy-guided lithotripsy, namely LL technology or the bipolar EHL system.
Difficult stones were defined by their size (larger than 15 mm), shape (barrel or square-shaped stones), location (cystic, intrahepatic, or stones located above a stricture) and whether they were impacted in the bile duct. Stone impaction was defined as an immobile stone that precluded guidewire and/or basket/mechanical lithotripter passage [1, 2, 6]. Failure after the use of two probes was defined as failure in ductal stone clearance after 2-probe lithotripsy. The stone size was determined using a comparative measurement method (using the scope tip as the reference standard). After data acquisition, image analysis was performed in an Osirix workstation (Osirix, software version 9.0) by a study investigator after proper training. In all patients, the cystic stump was accessed by direct visualization, namely by cholangioscopy. The median duration reported for EHL and LL was defined as the median duration of the procedure namely the duration of the entire treatment for each patient (one or more sessions) to obtain complete stone ductal clearance using EHL or LL. The decision to discontinue the procedure at any session was at the discretion of the endoscopist and was depending on several factors namely the evolution of the procedure, the duration, the number and size of stones, and the performance-status of the patient.
Adverse events were defined as any complications related to SOC-guided lithotripsy and were carefully assessed using previously specified definitions [2, 19].
Technique and Endoscopists
All procedures were performed with the patients in the prone position under sedation with propofol administration by an anesthesiologist. All patients received intraprocedural intravenous prophylactic antibiotics (fluoroquinolone or third-generation cephalosporin). Every patient included had previously undergone biliary sphincterotomy. When considered necessary, an extension of the preexisting sphincterotomy or balloon sphincteroplasty was performed to facilitate the passage of the cholangioscope. From 2017 to 2019, SOC was performed with the second-generation “SpyGlass” Direct Visualization System using a single-operator four-way deflected 10-Fr Spy-Scope (Boston Scientific, Natick, MA, USA) inserted through the working channel of a therapeutic duodenoscope. From March 2019, SOC was undertaken with the new improved second-generation system (DSII). The choice of the SOC-guided lithotripsy system in each patient depended on the availability and endoscopist preference (see discussion). The cholangioscope was inserted through the papilla and advanced to the common bile duct or cystic stump toward the target stone, with direct endoscopic vision and intermittent fluoroscopy. When deemed necessary, the cholangioscope was advanced over a stiff 0.025-inch guidewire. After direct visualization of the stone, the guidewire was changed by the 1.9-Fr EHL probe. When using LL technology, the fiber was preloaded into the cholangioscope’s 1.2-mm working channel, which allows the simultaneous presence of the laser fiber and the 0.025-inch guidewire. For lithotripsy, two techniques were used: LL and the bipolar EHL system. After SOC-guided lithotripsy, when ductal clearance could not be achieved in one session, a biliary plastic stent was inserted until the next session. Details of the fibers and techniques used in lithotripsy have been described elsewhere. All procedures were performed or supervised by experienced endoscopists with a personal load of more than 4000 ERCPs and more than 20 cholangioscopy-guided lithotripsy procedures in their careers.
The patients were kept in the hospital for at least one night to evaluate possible complications. Follow-up continued for at least 2 months, with subsequent visits and blood tests.
Statistical Analysis
Categorical variables are shown as absolute and relative frequencies, and quantitative variables are summarized as the mean and standard deviation or as the median and range according to the normality of the distribution. Differences between quantitative variables were tested using the Wilcoxon–Mann–Whitney test, and differences between categorical variables were tested using a chi-square test and Fisher´s exact test. To explain one versus multiple lithotripsy sessions and one versus multiple probes in EHL, binary logistic regression models were performed after evaluating potential predictors through univariate analysis. Positive factors resulting from multivariate analysis to explain one versus multiple lithotripsy sessions were tested for their ability to discriminate between positive and negative results with receiver operating characteristic curves (ROCs). The overall performance of the ROC analysis was quantified by computing the area under the curve (AUC) and 95% confidence intervals (CI). The optimal cutoffs of the ROC analysis were assessed using the Youden index. The null hypothesis was rejected when the test statistic p values were less than < 0.05. Statistical analyses were performed with the Stata software package version 14 (Stata- Corp 2015, Stata Statistical Software, Release 14; StataCorp, College Station, TX, USA).
Results
Patients, Stone Location and Interventions
In total, during the study period, 94 patients were enrolled, accounting for a total of 113 procedures. Of all patients enrolled, the majority were female (n = 55, 58.51%). The mean age was 71.06 (range 32–97 years). Forty-one patients (43.61%) had a prior cholecystectomy before the stone removal attempt. In total, 88 patients (93.6%) had failed at least 1 prior ERCP with stone removal attempts (median 1; range 0–7) using conventional stone extraction techniques. In such cases, biliary plastic stents were placed until definitive resolution of the complex bile duct stones. In the remaining 6 patients (6.4%), cholangioscopy-guided lithotripsy was performed in the index session after failure of conventional methods for stone extraction. Patient demographics and prior interventions are described in Table 1.
The majority of patients had stones in the common bile duct/common hepatic duct (n = 74, 78.72%). Twelve patients (12.77%) had stones in the cystic duct/cystic stump, and 8 patients (8.52%) had stones in the intrahepatic biliary tree. In total, 24 patients (25.53%) had impacted stones not removable by conventional techniques. The mean stone diameter was 20.35 mm (range 8–50 mm). The mean number of stones was 1.9 (range 1–15). The cholangiographic findings are summarized in Table 2.
Ductal Clearance and Predictive Factors for the Need for Multiple Sessions
Complete ductal clearance was achieved in 93/94 patients (98.9%) after a median number of 1 session (range 1–3). In total, 80/94 patients (85.11%) achieved complete stone removal in 1 session. In the remaining patients, ductal clearance was obtained after 2 sessions (8/94, 8.51%) or 3 sessions (5/94, 5.32%) (Table 3). In one patient, complete ductal clearance was not achieved after 2 sessions of cholangioscopy-guided lithotripsy. This last patient had multiple intrahepatic bile duct stones, which required multiple sessions to achieve complete ductal stone clearance. However, the patient died due to complications of cirrhosis secondary to low phospholipid-associated cholelithiasis syndrome.
The characteristics of patients who required only one session were compared to those who required more than one session to achieve complete ductal clearance (Tables 4, 5). Patients who required more than one session had larger stones (26.79 vs. 19.26, p = 0.068) and a higher number of stones (3.00 vs. 1.74, p = 0.063). Regarding stone location, 86.49% (64/74) of patients with common bile duct/common hepatic duct stones and 91.67% (11/12) of patients with cystic stump stones required only one session. On the other hand, a much lower proportion of patients with IHBD stones required only one session (62.50%, 5/8). Although not statistically significant (p = 0.153), IHBD stones were associated with a higher number of sessions to achieve complete ductal clearance. When EHL was used in the first session, 28/35 (80.0%) patients required only one session, while when LL was used, a slightly higher proportion of 52/59 (86.54%) patients required only one session (Table 4). In the multivariate analysis, stone size was independently associated with the need for multiple sessions to achieve complete ductal clearance (odds ratio = 1.146, 95% confidence interval: 1.055–1.244; p = 0.001)—Table 5.
Analysis of Receiver Operating Characteristic (ROC) Curves for Stone Size
ROC analysis (Fig. 1) yielded an AUC value of 0.6414 (95% confidence interval: 0.4388–0.8439) for stone size as a discriminator of accuracy for the need for multiple sessions for lithotripsy. On the basis of the Youden index, 22 mm was found to be the optimal cutoff for stone size (95% confidence interval: 15.71–28.28; p < 0.001). Therefore, the probability of complete ductal clearance in a single session was 17/20 (95.00%) for stones 0–15 mm, 55/60 (91.66%) for stones 15–30 mm, 8/13 (61,53%) for stones 30–45 mm, and almost 0 for stones larger than 45 mm.
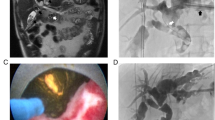
Performance of EHL and LL and of Factors Associated with the Outcomes
The median procedural time of cholangioscopy-guided lithotripsy was 69.48 min (range 20–210 min)—Table 3. In the first session, 59 patients (62.8%) underwent LL, and 29 patients (30.8%) were submitted to EHL. The mean procedural time was significantly longer for EHL than for LL [72.1 (SD 16.3 min) versus 51.1 (SD 10.5 min)] (p < 0.01). Six patients (6.4%) failed the first session with EHL after using two probes and therefore were crossed over to LL to obtain ductal clearance in a single additional session with a single LL fiber (Fig. 1).
Eighty patients (85,11%) required only one probe to achieve complete ductal clearance, while in 14 patients (14.89%), there was the need to use more than one probe to achieve complete ductal clearance (range 1–5)—Table 3. Regarding the patients treated with LL (n = 59), only one patient required 2 probes to achieve complete ductal clearance (1/59, 1.69%), while all the others required only one probe to achieve the same result (58/59, 98,31%). Considering the patients who started treatment with EHL (n = 35), 23 (65.71%) needed only one probe (Fig. 2), and the remaining 12 need more than one EHL probe (range 2–5). Therefore, EHL was significantly associated with a larger number of probes (2.0 vs. 1.02, p < 0.01) to achieve ductal clearance when compared to LL.
Considering EHL patients, stone size was associated with the need for more than one probe (p = 0.0061). Although not statistically significant, the number of stones was different between the two groups (1.43 vs. 3.16)—Table 6. On multivariate analysis (Table 7), stone size was the only predictor for more than one EHL probe or the need for crossing over to the LL probe.
Adverse Events
Adverse events were encountered in 29/94 patients (30.85%). Twenty-one patients (22.34%) experienced a transient fever between 37.7 and 39.3 °C for 24 h (16 patients) to 48 h (5 patients). Fever was managed conservatively, with fever clearance in all cases after 48 h. Five patients (5.32%) had mild post-ERCP pancreatitis, which was successfully managed conservatively, and 3 patients (3.19%) had postprocedural cholangitis, successfully treated with intravenous antibiotics (Table 3). No differences were found regarding complications in the EHL and LL groups.
Discussion
In this multicenter study of 94 patients who underwent 113 procedures of EHL or LL, complete ductal clearance was obtained in 93/94 patients (98.94%). In total, 80/94 patients (85.11%) achieved stone clearance in a single session. On multivariate analysis, stone size was independently associated with the need for multiple sessions to achieve complete ductal clearance, and it was significantly more likely for stones smaller than 22 mm than for stones larger than 22 mm. EHL was significantly associated with a larger number of probes to achieve ductal clearance, and the mean procedural time was significantly longer for EHL than for LL.
Cholangioscopy was first reported in Japan in 1978 using a prototype and was made possible by the combined use of a master duodenoscope and a thin cholangiopancreatoscope that can be passed through the instrument channel of the master duodenoscope; therefore, this technique has become known as peroral cholangiopancreatoscopy using the “mother-baby” technique [8]. More than one decade after this initial report, two different techniques for large stone fragmentation became available using the direct visualization of the stones via POC. From the University of Erlangen-Nuremberg, in 1986, we found the first report of the use of a Neodymium-YAG laser under direct vision for the fragmentation of a large stone in a 74-year-old man [7]. Three years later, in 1989, a group from Hong Kong reported the success of EHL lithotripsy with POC in a group of five patients [6]. After the initial enthusiasm for other reports [6, 20,21,22], this excitement waned by the beginning of the twenty-first century, and reports became scarce about POC-guided lithotripsy [23]. The main reason was that the technique of POC using the mother-daughter approach was delicate, was expensive (due to frequent repairs), was sometimes difficult with respect to insertion into the bile duct, required two experienced endoscopists, and had only two-way tip deflection. However, in 2007, single-operator cholangioscopy was introduced, which allows a more routine use of these technologies [24]. Furthermore, this device has been being improved twice, and the new digital system permits superior visualization of the biliary and pancreatic systems when compared with the original device [25]. Therefore, the success of stone fragmentation using EHL or HL has increased.
Therefore, during the last 13 years, much work has been done concerning POC-guided lithotripsy for difficult bile duct stones [2, 13, 15, 26,27,28]. Several case series have evaluated the fragmentation success of POC-guided lithotripsy with good results ranging from 77.3%-99.2% [18]. In the largest published series, a retrospective multicenter analysis of 407 patients, complete clearance of the ducts was obtained in 97.3 of the patients with a median session of 1 (range 1–4). Complete stone removal in a single session was obtained in 77.4% of the cases [17]. In a recent systematic review and meta-analysis including 35 studies with 1762 participants, overall fragmentation success was obtained in 91.2% of the patients, and complete single-session fragmentation success was obtained in 76.9% of the cases. However, for studies limited to the second-generation system, the overall stone fragmentation success rate was 95%, and the rate of bile duct clearance after a single session was 82% [18]. In a large multinational registry, Maydeo et al. reported that stone clearance in a single session was obtained in 80% of patients, and overall fragmentation success was achieved in 87.2% [16]. In a recent study from Germany, complete stone removal at the initial procedure was obtained in 75% of the patients, and overall success was achieved in 95% of the patients [25]. Our current study results are in good agreement with the literature, with complete stone removal obtained in 98.94% of the patients and complete single-session fragmentation success obtained in 85.11% of the cases.
Few studies have analyzed factors associated with the success of POC-guided lithotripsy. In one dedicated study, stone clearance in a single procedure was significantly more likely when the largest stone was less than 30 mm in size. Furthermore, in a multivariate analysis, other predictors of success in a single session included a smaller number of stones and a particular type of POC-guided lithotripsy, namely HL technology [16]. In the abovementioned study including 407 patients, difficult anatomy/cannulation was the only significant predictor associated with technical failure. On multivariate analysis, after adjusting for confounders, only the duration of the index procedure was a significant predictor of the need for more than one session. Furthermore, although technical success and adverse events were not significantly different between the EHL and HL groups, the procedure time was significantly longer in the EHL group than in the LL group [17]. In the current study, after multivariate analysis, stone size was independently associated with success in a single session, as suggested in the work of Maydeo et al. [16]. However, using ROC analysis, our cutoff was 22 mm, which may be related to the technique for measuring stone size, the number of stones in difficult locations (e.g., intrahepatic), or even the duration of the procedure. Taken together, it appears that stone size is clearly a predictive factor for a single-session procedure. In the current study, although not statistically significant, there was a trend in favor of an intrahepatic stone location and multiple stones as predictive factors for more than one lithotripsy session, and intuitively, these factors can limit the performance of a single session.
Another important issue is the performance of EHL and LL. In a large multicenter series of 407 patients, there were no differences in ductal clearance when using EHL or LL, but the mean procedure time was significantly longer in the EHL group than in the LL group [17]. In another study of 156 patients analyzing bile duct stone clearance in a single session of lithotripsy, although not statistically significant (p = 0.35), there was a trend in favor of LL (82%) versus EHL (74%) for ductal clearance in a single session [16]. In a recent systematic review including 1762 participants, the overall stone fragmentation success rate was not significantly different for EHL compared with LL [18]. In the abovementioned systematic review, there was a trend in favor of LL versus EHL (82.9% vs. 70.9%) for the rate of single-session lithotripsy success, and the mean procedure time was significantly longer for EHL than for LL, although the mean size of stones treated with EHL was smaller than that with LL. In the current study, there was also a trend in favor of LL versus EHL (86.54% vs. 80.0%) for complete stone removal in a single session, and the mean procedural time was significantly longer for patients submitted to EHL than for patients submitted to previous literature. In our study and similar to the existing literature [16,17,18], the overall stone fragmentation success rate and adverse events were not significantly different between EHL and LL. However, one topic that has been poorly assessed is the number of probes that are needed to achieve ductal clearance in a single session or overall. The issue is that the price of an EHL probe is similar to that of an LL probe. However, an EHL probe has a limited duration (somewhere between 1200 and 1300 pulses); therefore, the procedure is long, and more probes will be needed, which would incur higher costs [16,17,18]. In the current study, 34.28% of the patients submitted to EHL needed 2 or more probes to achieve complete ductal clearance, whereas when using LL, only one patient needed more than one LL probe because they were crossed over to an additional session of LL. Furthermore, six EHL patients failed complete ductal clearance after using two probes, and they were crossed over to another session with LL. In our multivariate analysis, the presence of larger stones were independent factors associated with the need for more than one probe. Taken together, there is a clear suggestion that if a patient has a large stone (larger than 22 mm), LL is the procedure to choose; otherwise, there is a risk of a prolonged procedure involving more than one EHL probe (increasing the costs) or posing a risk of an additional POC lithotripsy session.
The present study has several limitations. First, in the study protocol, there were no objective criteria for when to stop a procedure prior to complete ductal clearance and schedule another procedure. Furthermore, there were no criteria, nor was the selection between EHL and LL randomized, for stone clearance. Moreover, there were no comparative data with other techniques for stone fragmentation/removal, namely EPLBD and ML. Another potential limitation is that although the prices for EHL and LL probes are similar, no clear cost data were provided in our study.
The strengths of our study include the large number of patients and procedures included and the fact that this was the first prospective multinational study in our country. Furthermore, a large amount of data was extensively evaluated to determine factors associated with complete ductal clearance, including details on the number of probes used to achieve ductal clearance.
In conclusion, peroral cholangioscopy-guided lithotripsy is highly effective for difficult biliary stones, and most patients will achieve complete ductal clearance in one session, which is significantly more likely for stones < 22 mm. EHL is significantly associated with the need for more probes, increasing costs, and a longer procedural time to achieve ductal clearance.
Availability of data and material
The datasets generated and/or analyzed in the present study are available from the corresponding author on reasonable request.
Abbreviations
- POC:
-
Peroral cholangioscopy
- EHL:
-
Electrohydraulic lithotripsy
- LL:
-
Laser lithotripsy
- EST:
-
Endoscopic sphincterotomy
- EPLBD:
-
Endoscopic papillary large balloon dilation
- SOC:
-
Single-operator cholangioscopy
References
Aburajab M, Dua K. Endoscopic management of difficult bile duct stones. Curr Gastroenterol Rep 2018;20:8.
Canena J, Lopes L, Fernandes J, Alexandrino G, Lourenço L, Libânio D et al. Outcomes of single-operator cholangioscopy-guided lithotripsy in patients with difficult biliary and pancreatic stones. GE Port J Gastroenterol 2019;26:105–113.
Yasuda I, Itoi T. Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc 2013;25:376–385.https://doi.org/10.1111/den.12118.
Canena J. Once upon a time a guideline was used for the evaluation of suspected choledocholithiasis: A fairy tale or a nightmare? GE Portug J Gastroenterol 2018;25:6–9.
Misra SP, Dwivedi M. Large-diameter balloon dilation after endoscopic sphincterotomy for removal of difficult bile duct stones. Endoscopy 2008;40:209–213.
Leung JW, Chung SS. Electrohydraulic lithotripsy with peroral choledochoscopy. BMJ (Clin Res Ed) 1989;299:595–598.
Lux G, Ell C, Hochberger J, Müller D, Demling L. The first successful endoscopic retrograde laser lithotripsy of common bile duct stones in man using a pulsed neodymium-YAG laser. Endoscopy 1986;18:144–145.
Nakajima M, Akasaka Y, Yamaguchi K, Fujimoto S, Kawai K. Direct endoscopic visualization of the bile and pancreatic duct systems by peroral cholangiopancreatoscopy (PCPS). Gastrointest Endosc 1978;24:141–145.
Wong JC, Tang RS, Teoh AY, Sung JJ, Lau JY. Efficacy and safety of novel digital single-operator peroral cholangioscopy-guided laser lithotripsy for complicated biliary stones. Endosc Int Open 2017;5:E54–E58.
Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: A clinical feasibility study (with video). Gastrointest Endosc 2007;65:832–841.
Bang JY, Sutton B, Navaneethan U, Hawes R, Varadarajulu S. Efficacy of single-operator cholangioscopy-guided lithotripsy compared with large balloon sphincteroplasty in management of difficult bile duct stones in a randomized trial. Clin Gastroenterol Hepatol 2020;18:2349-2356.e3.
Laleman W, Verraes K, van Steenbergen W, Cassiman D, Nevens F, van der Merwe S et al. Usefulness of the single-operator cholangioscopy system SpyGlass in biliary disease: A single-center prospective cohort study and aggregated review. Surg Endosc 2017;31:2223–2232.
Tsuyuguchi T, Sakai Y, Sugiyama H, Ishihara T, Yokosuka O. Long-term follow-up after peroral cholangioscopy-directed lithotripsy in patients with difficult bile duct stones, including Mirizzi syndrome: An analysis of risk factors predicting stone recurrence. Surg Endosc 2011;25:2179–2185.
Navaneethan U, Hasan MK, Kommaraju K, Zhu X, Hebert-Magee S, Hawes RH et al. Digital, single-operator cholangiopancreatoscopy in the diagnosis and management of pancreatobiliary disorders: a multicenter clinical experience (with video). Gastrointest Endosc [Internet] 2016;84:649–55. https://doi.org/10.1016/j.gie.2016.03.789.
Franzini T, Moura R, Bonifácio P, Luz G, de Souza T, dos Santos M et al. Complex biliary stones management: Cholangioscopy versus papillary large balloon dilation—A randomized controlled trial. Endoscopy International Open 2018;06:E131–E138.
Maydeo AP, Rerknimitr R, Lau JY, Aljebreen A, Niaz SK, Itoi T et al. Cholangioscopy-guided lithotripsy for difficult bile duct stone clearance in a single session of ERCP: Results from a large multinational registry demonstrate high success rates. Endoscopy 2019;51:922–929.
Brewer Gutierrez OI, Bekkali NLH, Raijman I, Sturgess R, Sejpal DV, Aridi HD et al. Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Clin Gastroenterol Hepatol 2018;16:918–926.e1. https://doi.org/10.1016/j.cgh.2017.10.01718.
McCarty TR, Gulati R, Rustagi T. Efficacy and safety of peroral cholangioscopy with intraductal lithotripsy for difficult biliary stones: A systematic review and meta-analysis. Endoscopy 2021;53:110–122. https://doi.org/10.1055/a-1200-8064.
Kedia P, Tarnasky PR. Endoscopic management of complex biliary stone disease. Gastrointest Endosc Clin N Am 2019;29:257–275.
Binmoeller KF, Brückner M, Thonke F, Soehendra N. Treatment of difficult bile duct stones using mechanical, electrohydraulic and extracorporeal shock wave lithotripsy. Endoscopy 1993;25:201–206.
Das AK, Chiura A, Conlin MJ, Eschelman D, Bagley DH. Treatment of biliary calculi using holmium: Yttrium aluminum garnet laser. Gastrointest Endosc 1998;48:207–209.
Adamek HE, Buttmann A, Wessbecher R, Kohler B, Riemann JF. Clinical comparison of extracorporeal piezoelectric lithotripsy (EPL) and intracorporeal electrohydraulic lithotripsy (EHL) in difficult bile duct stones. A prospective randomized trial. Dig Dis Sci 1995;40:1185–92.
Hui C-K, Lai K-C, Ng M, Wong W-M, Yuen M-F, Lam S-K et al. Retained common bile duct stones: A comparison between biliary stenting and complete clearance of stones by electrohydraulic lithotripsy. Aliment Pharmacol Ther 2003;17:289–296.
Chen YK, Pleskow DK. SpyGlass single-operator peroral cholangiopancreatoscopy system for the diagnosis and therapy of bile-duct disorders: a clinical feasibility study (with video){A figure is presented}. Gastrointest Endosc 2007;65:832–841.
Bokemeyer A, Gerges C, Lang D, Bettenworth D, Kabar I, Schmidt H et al. Digital single-operator video cholangioscopy in treating refractory biliary stones: A multicenter observational study. Surg Endosc [Internet] 2020;34:1914–22. https://doi.org/10.1007/s00464-019-06962-0.
Wong JC, Tang RS, Teoh AY, Sung JJ, Lau JY, Bhandari S et al. Efficacy and safety of novel digital single-operator peroral cholangioscopy-guided laser lithotripsy for complicated biliary stones. Endosc Int Open 2017;5:E54–E58.
Patel MS, Davis MM, Lypson ML, Gilman W, Matthew DSL, Bosanquet N, Oppong R et al. Health economics education in undergraduate medical training: Introducing the health economics education (HEe) website. BMC Med Educ [Internet] 2013;15:126.
Patel SN, Rosenkranz L, Hooks B, Tarnasky PR, Raijman I, Fishman DS et al. Holmium-yttrium aluminum garnet laser lithotripsy in the treatment of biliary calculi using single-operator cholangioscopy: A multicenter experience (with video). Gastrointest Endoscop 2014;79:344–348.
Funding
There was no funding for this research.
Author information
Authors and Affiliations
Contributions
Gonçalo Alexandrino contributed to performing procedures, collection of data, analysis and interpretation of data, and drafting the manuscript; Luis Lopes contributed to conception and design of the study, performing procedures, collection of data, analysis and interpretation of data, and drafting the manuscript; João Fernandes contributed to conception and design of the study, collection of data, critical revision of the manuscript, and approval of the final draft submitted; Marta Moreira contributed to collection of data, critical revision of the manuscript, and approval of the final draft submitted; Tarcísio Araújo contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; Sara Campos contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; Rui Loureiro contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; Luísa Figueiredo contributed to collection of data, critical revision of the manuscript, and approval of the final draft submitted; Luís Carvalho Lourenço contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; David Horta contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; Tiago Bana e Costa contributed to collection of data, preforming procedures, critical revision of the manuscript, and approval of the final draft submitted; Patricio Costa contributed to statistical analysis, critical revision of the manuscript, and approval of the final draft submitted; and Jorge Canena contributed to conception and design of the study, collection of data, analysis and interpretation of data, performing procedures and drafting the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Jorge Canena is an International Consultant for Boston Scientific but did not receive any financial arrangements for this research, or any assistance with manuscript preparation. The remaining authors declare that they have no competing interests.
Ethics approval
This study was conducted in compliance with the International Conference on Harmonization guidelines for Good Clinical Practice (E6) and the 2013 Declaration of Helsinki. All patients provided written informed consent before inclusion in the study. This observational study was approved by local Ethics Committees of 6 hospitals (ULSAM 44/2018, EDOC/ULSBA/15191, EC/56-2018, HGO 23/18, HEM-CHLO 060618 and HBA 2121/18).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Video showing bursts of an electrohydraulic probe for fragmentation of a stone. (MPG 14432 kb)
video showing complete setting of Cholangioscopy-guided laser lithotripsy for multiples stones of the bile duct. (MPG 20756 kb)
Rights and permissions
About this article
Cite this article
Alexandrino, G., Lopes, L., Fernandes, J. et al. Factors Influencing Performance of Cholangioscopy-Guided Lithotripsy Including Available Different Technologies: A Prospective Multicenter Study with 94 Patients. Dig Dis Sci 67, 4195–4203 (2022). https://doi.org/10.1007/s10620-021-07305-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-021-07305-7