Abstract
Background/Aim
The prognosis of patients with hepatocellular carcinoma (HCC) undergoing transarterial chemoembolization (TACE) is highly heterogeneous because of variable characteristics of tumor burden and liver dysfunction. We aimed to propose and validate an albumin–bilirubin (ALBI) grade-based prognostic nomogram for HCC patients undergoing TACE.
Methods
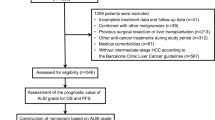
A total of 1051 patients with HCC undergoing TACE were randomly assigned to derivation (n = 525) and validation (n = 526) set in this retrospective study based on prospective data. The multivariate Cox proportional hazards model in derivation set was used to generate the nomogram. The predictive accuracy of the nomogram was evaluated by discrimination and calibration tests.
Results
In multivariate analysis, presence of ascites, ALBI grade 2–3, serum ɑ-fetoprotein level ≥ 400 ng/mL, total tumor volume ≥ 396 cm3, presence of vascular invasion, and poor performance status were independently associated with decreased survival of patients in the derivation set. Each patient had an individualized score from 0 to 41 by adding up the points from these six prognostic predictors. The nomogram generated from the derivation set had a concordance index of 0.72 (95% confidence interval [CI] 0.63–0.82). Discrimination test in the validation set provided a good concordance index 0.72 (95% CI 0.62–0.81), and the calibration plots consistently matched the ideal 45-degree reference line for 3- and 5-year survival prediction.
Conclusions
The ALBI grade-based prognostic model can well discriminate the survival in HCC patients undergoing TACE. The proposed easy-to-use nomogram may accurately predict the survival at 3 and 5 years for individual HCC patient in the precision medicine era.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the most common primary liver cancer and the fourth leading cause of cancer mortality globally [1]. Chronic hepatitis B and C, alcoholism and nonalcoholic fatty liver disease (NAFLD) are the main etiologies of HCC [2, 3]. The prognosis of HCC remains poor despite improved diagnosis and therapy because most patients are identified at an advanced stage [4, 5]. For early-stage HCC, curative treatments such as surgical resection, tumor ablation, and transplantation are suggested. Transarterial chemoembolization (TACE) is usually indicated for unresectable HCC with good liver functions aiming to improve survival [6,7,8]. However, patients undergoing TACE appear to experience variable clinical outcomes because of highly heterogeneous characteristics of tumor burden and underlying liver functional reserve.
The prognosis of HCC depends on tumoral extent, performance status, and liver functional reserve. Many HCC staging systems used Child–Turcotte–Pugh (CTP) classification to evaluate the severity of liver dysfunction [2, 3]. However, CTP classification has its shortcoming including subjective variables and their cutoff values are arbitrary [9]. The model for end-stage liver disease (MELD) score is an alternative tool to measure liver functional reserve [10]. Recently, the albumin–bilirubin (ALBI) grade incorporates only two subjective variables (serum albumin and bilirubin level) to assess liver function. Notably, the ALBI grade has been validated in several studies for HCC as a marker of hepatic reserve [11,12,13,14].
Nomogram derived from hazard functions is a straightforward tool to estimate the survival in human cancers [15]. Importantly, nomogram may improve prognostic accuracy from group level to individual level. In addition, medical providers can use this simple tool to calculate approximate survival for each patient at the time of diagnosis and treatment planning. Several reports have used nomogram to predict the prognosis of HCC patients undergoing different treatments [16,17,18,19]; however, very few studies have specifically evaluated the feasibility of ALBI grade-based nomogram in the setting of TACE. We aimed to propose and validate an ALBI-based prognostic nomogram for prognostic prediction in patients with HCC undergoing TACE.
Methods
Patients
From 2002 to 2017 in Taipei Veterans General Hospital, a total of 1051 HCC patients undergoing TACE as the primary therapy were prospectively collected and retrospectively analyzed. Patients were randomly assigned to derivation and validation set. The baseline demographic data, etiology of HCC, tumor burden, liver functional reserve, performance status, and laboratory data were comprehensively collected at the time of diagnosis. These patients were followed up every 3–4 months after initial treatment. This study was approved by the Institutional Review Broad of Taipei Veterans General Hospital and complies with the standards of the Declaration of Helsinki and current ethical guidelines. Waiver of consent was obtained, and patient records/information was anonymized and de-identified prior to analysis.
Diagnosis and Definitions
HCC was diagnosed by contrast-enhanced dynamic computed tomography (CT) and magnetic resonance imaging (MRI) showing early hyperenhancement in arterial phase and delayed washout in venous phase [2, 3, 20]. Hepatitis B virus (HBV)-related HCC was classified as patients who were seropositive for HBV surface antigen (HBsAg). Patients who were anti-hepatitis C virus (HCV)-positive were considered as HCV-related HCC. Patients with daily alcohol consumption of at least 40 g for 5 years or more were diagnosed as alcoholism [21]. The presence of ascites was diagnosed by abdominal ultrasound or CT, and the severity was defined according to the European Association for the Study of the Liver (EASL) criteria [22]. The performance status of each patient was evaluated by Eastern Cooperative Oncology Group (ECOG) [23]. The calculation of total tumor volume (TTV) was based on individual tumor diameter as previously described [24]. The presence of thrombus adjacent to the tumor in portal system with blurring boundary by CT or MRI was defined as vascular invasion [25]. The ALBI score was calculated by the following equation = 0.66 × log10bilirubin − 0.085 × albumin, and ALBI grade was defined as ALBI grade 1 (score ≤ − 2.60), ALBI grade 2 (score > − 2.60 and ≤ − 1.39), and ALBI grade 3 (score > − 1.39) as originally proposed [11, 12].
Treatment
The treatments of HCC patients were discussed by multidisciplinary HCC broad at our hospital. Written informed consent and shared decisions were performed after patient consultation. The indications for patients undergoing TACE were: unresectable HCC with adequate liver functional reserve, no main portal vein trunk invasion or distant metastasis, and serum creatinine concentration less than 1.5 mg/dL [26, 27]. The procedure of TACE was done according to the Seldinger’s method [26].
Statistical Analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA). The comparison of continuous variables was analyzed by the Mann–Whitney test. The chi-square test was used to compare the categorical data. The survival of HCC patients was examined by the Kaplan–Meier method with the log-rank test. The BETAs coefficient and hazard ratios of independent prognosis predictors were evaluated by the multivariate Cox model. The performance of the nomogram was analyzed by the concordance index and the calibration plot [28,29,30,31]. A p value < 0.05 was considered statistically significant.
Results
Baseline Demographics
After randomization, the derivation and validation set contained 525 patients and 526 patients, respectively. Baseline demographics are summarized in Table 1. The mean and median follow-up duration in the derivation set and validation set were 31 ± 18 months and 30 ± 19 months, respectively. The majority of patients were male (76%) with a mean age of 67 years. HBV and HCV were the only underlying etiology of liver disease in 43% and 29%, respectively. About 54% patients had single tumors and 49% patients had maximal tumor diameter larger than 5 cm. Diabetes mellitus was found in 27% patients, and 20% of patients had ascites (grade 1 in 15%, grade 2 in 3%, and grade 3 in 2%). Seventy-seven percent of patients were classified as CTP class A, and 59% of patients had performance status 0. There was no significant difference between the two sets in tumor burden, liver functional reserve, serum laboratory data, and Barcelona Clinic of Liver Cancer (BCLC) staging (all p > 0.05) except in vascular invasion.
A higher ALBI score was associated with an increased CTP score (p < 0.001 for trend; Fig. 1a). However, a poor correlation between ALBI score and model for end-stage liver disease (MELD) score was observed (p = 0.303 for trend; Fig. 1b).
Survival Analysis in the Derivation Set
There was a significant survival difference between ALBI grade 1 and grade 2–3 in the derivation set (p < 0.001, Fig. 2). Factors that were possibly linked with survival were investigated among patients in the derivation set (Table 2). In the univariate analysis, factors associated with increased risk of mortality included serum platelet ≤ 150,000/μL, serum creatinine > 1.2 mg/dL, presence of ascites, ALBI grade 2–3, tumor size equal or larger than 5 cm, serum AFP ≥ 400 ng/mL, TTV ≥ 396 cm3, presence of vascular invasion, and performance status 2 or worse (all p < 0.05). In the multivariate Cox proportional analysis, presence of ascites (BETA 0.278, p = 0.004), ALBI grade 2–3 (BETA 0.470, p < 0.001), serum AFP ≥ 400 ng/mL (BETA 0.741, p < 0.001), TTV ≥ 396 cm3 (BETA 0.631, p < 0.001), presence of vascular invasion (BETA 0.506, p < 0.001), performance status 2 (BETA 0.315, p = 0.004), and performance status 3–4 (BETA 0.439, p = 0.008) were independently associated with a decreased survival.
Construction of the Nomogram
Six variables selected in the multivariate Cox model from the derivation set were included to build a nomogram. The ratios of calculated BETAs were used to determine the proportional prognostic effect of these variables. Serum AFP ≥ 400 ng/ml was defined as 10 points because of the highest BETA value (Fig. 3). The nomogram points of other five variables were TTV ≥ 396 cm3 (8.5), vascular invasion (6.7), ALBI grade 2–3 (6.3), presence of ascites (3.7), performance status 2 (4.2), and status 3–4 (5.8). The total score of this nomogram ranges from 0 to 41. By adding up the score of six variables in each patient, the survival probability can be estimated for individual HCC patient at 3 and 5 years (Fig. 3).
Discrimination and Calibration of the Nomogram in the Derivation Set
The 525 patients in the derivation set were categorized into four groups (Q) according to the nomogram points (Q1: ≤ 6, Q2: 6.1 to 9.9, Q3: 10 to16.4, Q4: > 16.4) for the calibration plots. The concordance index of nomogram in the derivation set was 0.72 (95% confidence interval [CI] 0.63–0.82). The calibration plots for both 3- and 5-year survival fell along the 45-degree line for patients across Q1 to Q4 (Fig. 4a, b).
The calibration of nomogram for 3- and 5-year survival prediction in the derivation set. The X-axis presents the nomogram-predicted overall survival, and the Y-axis shows the mean survival and 95% confidence interval calculated by Kaplan–Meier method. Patients were divided into quantiles (Q) to evaluate the accuracy of nomogram (Q1: ≤ 6, Q2: 6.1–9.9, Q3: 10 to 16.4, Q4: > 16.4). The calibration lines fit along with the 45-degree reference for 3- and 5-year survival in the derivation set
Discrimination and Calibration of the Nomogram in the Validation Set
In the validation set, the concordance index of established nomogram to predict survival was 0.72 (95% CI 0.62–0.81). The calibration plots for 3- and 5-year survival showed good correlation with the ideal 45-degree reference line for the four groups of patients (Fig. 5a, b).
The calibration of nomogram for 3- and 5-year survival prediction in the validation set. Patients were divided into quantiles (Q) to evaluate the accuracy of nomogram (Q1: ≤ 6, Q2: 6.1–9.9, Q3: 10 to 16.4, Q4: > 16.4). The calibration lines fit along with the 45-degree reference for 3- and 5-year survival in the validation set
Discussion
HCC patients undergoing TACE comprise a very heterogeneous population regarding liver functional reserve and tumor burden. In this large cohort study with adequate follow-up duration, an ALBI-based nomogram was developed and used to estimate individual survival of HCC patients undergoing TACE. There are two major implications of this approach. First, the ALBI grade may exhibit reliable discriminative ability in assessing the survival of this special patient population. Second, our results demonstrate internally validated ALBI grade-based nomogram to predict the prognosis of HCC patients undergoing TACE. This nomogram was easy-to-apply tool and provide clinicians who can readily calculate the predicted survival straightforwardly on an individual basis.
The underlying liver functional reserve plays an important role in prognostic evaluation for HCC [2, 32]. Several HCC staging systems adopted the CTP classification to assess the severity of liver function reserve. However, CTP classification has several drawbacks including subjective assessment of the severity of ascites and hepatic encephalopathy, and some variables are closely interrelated [9]. Although the MELD score was applied for the same purpose, it is mainly used to prioritize end-stage cirrhotic patients awaiting liver transplantation [10]. The ALBI grade has been proposed as a simple and objective method in assessing liver reserve for HCC and validated in the multicenter study [11]. Consistent with most previous studies [11, 12], our results show that the ALBI grade can discriminate overall survival in HCC patients undergoing TACE. In multivariate Cox model, ALBI grade 2–3 was associated with 50% increased risk of mortality compared with ALBI grade 1. Therefore, the ALBI grade is considered a powerful tool to predict the outcome in these patients.
In addition to the ALBI grade, consistent with previous studies [33, 34], our study also shows that patients with higher TTV tend to have decreased survival. Moreover, in accordance with published series [25, 32], the presence of vascular invasion and poor performance status were independent risk factors associated with poor survival in our study. Taken together, the extent of tumoral involvement, the severity of liver dysfunction, and performance status are considered major prognostic predictors for HCC patients undergoing TACE.
Serum AFP level is a widely used biomarker both in diagnosis and in outcome prediction for HCC. Patients with higher AFP level are often associated with more aggressive cancer phenotype [35, 36]. Consistently [37], our results demonstrate that patients with higher serum AFP level had decreased overall survival. Alternatively, ascites is a typical hallmark of portal hypertension and was identified as an independent poor prognostic predictor [38]. In this study, the presence of ascites increased the risk of mortality by 40%, further indicating its pivotal role in prognostic prediction for HCC patients undergoing TACE.
We have constructed an assessable ALBI grade-based nomogram to predict survival of individual patients undergoing TACE. The advantage of the nomogram is that all variables are ordinary clinical characteristics and no complex mathematical calculation is required. This easy-to-use nomogram may improve patient–physicians communication, decision making, and selection of patients for prospective clinical trials. Notably, in comparison with a previous study which adopted CTP classification as a prognostic component, instead we used ALBI grade, a more objective and evidence-based method to assess liver dysfunction for outcome prediction in patients undergoing TACE [39].
The concordance index of the derivation set was 0.72 in this study. This means that patients with higher nomogram points had 72% increased risk of mortality. In the validation set, the nomogram also shows an excellent concordance index of 0.72. These results confirm that this ALBI grade-based nomogram is a fairly good prediction model for HCC characterized by highly heterogeneous clinical behavior. The calibration plots were used to evaluate the accuracy of nomogram by comparing the nomogram-predicted survival and actual survival by Kaplan–Meier method. In the derivation set, the calibration plots for overall survival at 3 and 5 years well matched the idealized 45-degree line, confirming the predictive accuracy of nomogram. Similar distributions were observed in 3-year and 5-year survival in the validation set, suggesting that the ALBI grade-based nomogram is a simple and feasible prognostic tool to predict survival for these patients.
Our ALBI-based prognostic nomogram has several advantages compared with another study from Taiwan [40]. Firstly, the proposed predictive nomogram comprehensively included six important variables including total tumor volume, vascular invasion, AFP, ALBI grade, ascites, and performance status. A major feature is that we have incorporated TTV to describe tumor burden and performance status in the nomogram. Secondly, our nomogram is a graphic presentation and straightforward tool to predict individual patient survival. Medical providers can use this simple tool to calculate approximate survival for each patient at the time of diagnosis and treatment planning. For example, for patients with nomogram point 0, the 3- and 5-year survival rates were 65% and 49%, respectively. Thirdly, our proposed ALBI-based prognostic nomogram had a concordance index 0.72 in the derivation and validation cohort. However, the area under the receiver operating characteristics curve for the other ALBI-based prognostic model was 0.68–0.72 [40]. Therefore, our ALBI-based nomogram is a better and more feasible model.
This study has a few limitations. First, our nomogram was generated from a cohort where hepatitis B is the major etiology of chronic liver disease, and external validation is required before this model can be applied in western countries. Second, the nomogram was generated from TACE patients; therefore, it may not be suitable for patients undergoing other therapies. Third, in order to minimize the effect of multi-collinearity in this nomogram, all six variables in the model need to be used to generate estimate survival; missing of any of these variables might decrease the predictive accuracy.
Conclusions
The ALBI grade-based nomogram, generated from a large patient cohort, may provide quantitative evidence to support the prognostic feasibility in HCC patients undergoing TACE. This easy-to-apply nomogram may accurately predict the survival for individual HCC patient counseling for TACE and should be considered in treatment planning for HCC patients undergoing TACE.
Key Messages
-
The prognosis of hepatocellular carcinoma (HCC) patients undergoing transarterial chemoembolization (TACE) is highly heterogeneous.
-
Albumin–bilirubin (ALBI)-based nomogram was developed in the derivation set. Each patient had an individualized score from 0 to 41 by adding up the points from the six prognostic predictors. This nomogram had a good concordance index (0.72) in the validation set.
-
The proposed ALBI grade-based nomogram is an easy-to-use prognostic tool that may accurately predict the survival at 3 and 5 years for individual HCC patient in the precision medicine era.
Abbreviations
- ALBI:
-
Albumin–bilirubin
- AFP:
-
Alpha-fetoprotein
- BCLC:
-
Barcelona Clinic Liver Cancer
- CTP:
-
Child–Turcotte–Pugh score
- CT:
-
Computed tomography
- ECOG:
-
Eastern Cooperative Oncology Group
- HCC:
-
Hepatocellular carcinoma
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- MELD:
-
Model for end-stage liver disease
- MRI:
-
Magnetic resonance imaging
- TACE:
-
Transarterial chemoembolization
- TTV:
-
Total tumor volume
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
EASL Clinical Practice Guidelines. Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236.
Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the american association for the study of liver diseases. Hepatology. 2018;68:723–750.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53:1020–1022.
Barman PM, Sharma P, Krishnamurthy V, et al. Predictors of mortality in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. Dig Dis Sci. 2014;59:2821–2825.
Sieghart W, Hucke F, Peck-Radosavljevic M. Transarterial chemoembolization: modalities, indication, and patient selection. J Hepatol. 2015;62:1187–1195.
Lo CM, Ngan H, Tso WK, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002;35:1164–1171.
Kim DS, Lim TS, Jeon MY, et al. Transarterial chemoembolization in treatment-naive and recurrent hepatocellular carcinoma: a propensity-matched outcome analysis. Dig Dis Sci. 2019;64:3660–3668.
Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis. 2008;28:110–122.
Huo TI, Lee PC, Huang YH, et al. The sequential changes of the model for end-stage liver disease score correlate with the severity of liver cirrhosis in patients with hepatocellular carcinoma undergoing locoregional therapy. J Clin Gastroenterol. 2006;40:543–550.
Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33:550–558.
Liu PH, Hsu CY, Hsia CY, et al. ALBI and PALBI grade predict survival for HCC across treatment modalities and BCLC stages in the MELD era. J Gastroenterol Hepatol. 2016;32:879–886.
Kim JH, Sinn DH, Lee JH, et al. Novel albumin–bilirubin grade-based risk prediction model for patients with hepatocellular carcinoma undergoing chemoembolization. Dig Dis Sci. 2018;63:1062–1071.
Ho SY, Liu PH, Hsu CY, et al. A new prognostic model based on albumin-bilirubin grade for hepatocellular carcinoma beyond the milan criteria. Dig Dis Sci. 2020;65:658–667.
Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26:1364–1370.
Hsu CY, Liu PH, Hsia CY, et al. Surgical resection is better than transarterial chemoembolization for patients with hepatocellular carcinoma beyond the milan criteria: a prognostic nomogram study. Ann Surg Oncol. 2016;23:994–1002.
Kao WY, Su CW, Chiou YY, Chiu NC, Liu CA, Fang KC, Huo TI, Huang YH, Chang CC, Hou MC, Lin HC, Wu JC. Hepatocellular carcinoma: nomograms based on the albumin–bilirubin grade to assess the outcomes of radiofrequency Ablation. Radiology. 2017; 162382.
Xu L, Peng ZW, Chen MS, et al. Prognostic nomogram for patients with unresectable hepatocellular carcinoma after transcatheter arterial chemoembolization. J Hepatol. 2015;63:122–130.
Hsu CY, Liu PH, Ho SY, et al. Using nomogram of the Barcelona Clinic Liver Cancer system for treatment selection in patients with stage C hepatocellular carcinoma. BMC Cancer. 2018;18:289.
Ronot M, Purcell Y, Vilgrain V. Hepatocellular carcinoma: current imaging modalities for diagnosis and prognosis. Dig Dis Sci. 2019;64:934–950.
Grant BF, Dufour MC, Harford TC. Epidemiology of alcoholic liver disease. Semin Liver Dis. 1988;8:12–25.
EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010; 53:397–417.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982; 5:649–655.
Toso C, Asthana S, Bigam DL, Shapiro AM, Kneteman NM. Reassessing selection criteria prior to liver transplantation for hepatocellular carcinoma utilizing the Scientific Registry of Transplant Recipients database. Hepatology. 2009;49:832–838.
Lee YH, Hsu CY, Huang YH, et al. Vascular invasion in hepatocellular carcinoma: prevalence, determinants and prognostic impact. J Clin Gastroenterol. 2014;48:734–741.
Huo TI, Wu JC, Huang YH, et al. Acute renal failure after transarterial chemoembolization for hepatocellular carcinoma: a retrospective study of the incidence, risk factors, clinical course and long-term outcome. Aliment Pharmacol Ther. 2004;19:999–1007.
Bargellini I, Sacco R, Bozzi E, et al. Transarterial chemoembolization in very early and early-stage hepatocellular carcinoma patients excluded from curative treatment: a prospective cohort study. Eur J Radiol. 2012;81:1173–1178.
Pencina MJ, D’Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23:2109–2123.
Harrell FE Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387.
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16:965–980.
Forster MR. Key concepts in model selection: performance and generalizability. J Math Psychol. 2000;44:205–231.
Waked I, Berhane S, Toyoda H, et al. Transarterial chemo-embolisation of hepatocellular carcinoma: impact of liver function and vascular invasion. Br J Cancer. 2017;116:448–454.
Hsu CY, Huang YH, Hsia CY, et al. A new prognostic model for hepatocellular carcinoma based on total tumor volume: the Taipei Integrated Scoring System. J Hepatol. 2010;53:108–117.
Huo TI, Hsu CY, Huang YH, et al. Prognostic prediction across a gradient of total tumor volume in patients with hepatocellular carcinoma undergoing locoregional therapy. BMC Gastroenterol. 2010;10:146.
Tangkijvanich P, Anukulkarnkusol N, Suwangool P, et al. Clinical characteristics and prognosis of hepatocellular carcinoma: analysis based on serum alpha-fetoprotein levels. J Clin Gastroenterol. 2000;31:302–308.
Yamashita T, Ji J, Budhu A, et al. EpCAM-positive hepatocellular carcinoma cells are tumor-initiating cells with stem/progenitor cell features. Gastroenterology. 2009;136:1012–1024.
Hsu CY, Liu PH, Lee YH, et al. Using serum alpha-fetoprotein for prognostic prediction in patients with hepatocellular carcinoma: what is the most optimal cutoff? PLoS One. 2015;10:e0118825.
Hsu CY, Lee YH, Huang YH, et al. Ascites in patients with hepatocellular carcinoma: prevalence, associated factors, prognostic impact, and staging strategy. Hepatol Int. 2013;7:188–198.
Huo TI. ALBI grade as a new player in hepatocellular carcinoma. J Chin Med Assoc. 2019;82:1.
Lee IC, Hung YW, Liu CA, et al. A new ALBI-based model to predict survival after transarterial chemoembolization for BCLC stage B hepatocellular carcinoma. Liver Int. 2019;39:1704–1712.
Acknowledgments
This study was supported by the grants from Taipei Veterans General Hospital (V107A-008, VN109-06, V108A-002, VN108-05), Taipei, Taiwan, that helped data collection, analysis, interpretation, and manuscript preparation.
Author information
Authors and Affiliations
Contributions
T.-I. Huo is the guarantor of the article. Specific author contributions: S.-Y. Ho, C.-Y. Hsu, and T.-I. Huo performed the research and wrote the paper. P.-H. Liu and C.-W. Su collected and analyzed the data. C.-C. Ko, Y.-H. Huang, R.-C. Lee, and M.-C. Hou contributed to study design and data collection. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ho, SY., Hsu, CY., Liu, PH. et al. Albumin–Bilirubin (ALBI) Grade-Based Nomogram for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization. Dig Dis Sci 66, 1730–1738 (2021). https://doi.org/10.1007/s10620-020-06384-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06384-2