Abstract
Background
An altered gastrointestinal barrier function is reportedly associated with the pathogenesis of functional dyspepsia (FD); however, the pathogenesis of FD has not yet been fully elucidated.
Aims
The objective of the present study was to determine whether the mucosal barrier function is impaired in patients with FD and to investigate the mechanisms underlying FD.
Methods
The present study included patients with FD (FD group, n = 24), non-FD patients with abdominal symptoms (symptomatic control group, n = 14), and patients with no abdominal symptoms (asymptomatic control group, n = 20). The groups were compared regarding the mucosal electrical impedance (MI) values of the stomach and duodenum, which were measured using a tissue conductance meter during esophagogastroduodenoscopy.
Results
There were no significant differences between the three groups in the MI of the stomach. In contrast, the duodenal MI of the FD group (17.8 ± 4.3 Ω) was significantly lower than those of the symptomatic control group (27.2 ± 6.4 Ω, p < 0.0001) and asymptomatic control group (23.0 ± 7.4 Ω, p = 0.016). The expression of zonula occludens-1 (ZO-1) was significantly lower in the FD group than in the symptomatic control group (p = 0.011), where ZO-1 was positively correlated with the duodenal MI (β = 0.513, p = 0.017). The interleukin (IL)-1β expression was significantly higher in the FD group than in the symptomatic control group (p = 0.041), where IL-1β was inversely correlated with the duodenal MI (β = − 0.600, p = 0.004).
Conclusions
The mucosal barrier function of the duodenum was altered in patients with FD. Both a decreased ZO-1 and increased IL-1β may play a role in the pathogenesis of FD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional dyspepsia (FD) is a functional gastrointestinal disorder characterized by heterogeneous symptoms thought to originate from the gastroduodenal region, including postprandial fullness, early satiety, epigastric pain, and epigastric burning [1]; this condition affects 12–15% of the general population in developed countries [2]. FD is currently defined based on the Rome IV criteria [3]. Although FD is not a life-threatening disease per se, a high prevalence of FD has a substantial social impact, as FD impairs quality of life and reduces labor productivity [4]. The pathogenesis of FD remains unclear.
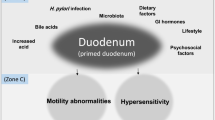
Several potential mechanisms and etiologies of FD have been proposed, particularly concerning the stomach. Factors that may play a role in the pathogenesis and development of FD include altered gastric motility [5], impairment of gastric emptying [6, 7] and gastric accommodation [5], and hypersensitivity to gastric distension [6, 8, 9].
Several studies have focused on the role of the duodenal function in the pathogenesis of FD. Some reports have shown that duodenal hypersensitivity is involved in FD, with symptoms potentially mediated by acids [10], lipids [11], and capsaicin [12]. It has also been suggested that the pathogenesis of FD involves low-grade duodenal inflammation, especially in post-infectious conditions [13] and some allergic conditions [14]. More recently, it has been shown that low-grade inflammation in patients with FD is associated with increased duodenal mucosal permeability [15].
Although previous studies have suggested that an impaired duodenal mucosal barrier function might be involved in the pathophysiology of FD, no study has yet examined this in detail or determined which factors influence the mucosal barrier function. Furthermore, it remains unclear whether the mucosal barrier function of the stomach is also altered in patients with FD.
The recently developed tissue conductance meter enables the evaluation of the gastrointestinal mucosal barrier function based on the calculated mucosal electrical impedance (MI) in real time in the clinical setting. The objective of the present study was to measure the gastrointestinal MI to assess whether the mucosal barrier function was impaired in patients with FD and to investigate the mechanisms underlying FD.
Patients and Methods
Study Patients
This case–control study was conducted between August 2016 and December 2017. The following three groups of patients were recruited: patients with FD (FD group), patients who had FD-like symptoms but were not diagnosed with FD (symptomatic control group), and patients who had no FD-like symptoms (asymptomatic control group). FD was diagnosed based on the Rome III criteria when no organic disorders were detected by esophagogastroduodenoscopy (EGD). The FD group included 24 patients with FD (11 females, 13 males) consisting of postprandial distress syndrome (PDS, n = 16) and epigastric pain syndrome (EPS, n = 8). The symptomatic control group included 14 patients (6 females, 8 males) without FD but with FD-like symptoms, including epigastric pain and/or abdominal distention. Based on EGD findings, pathological analysis of biopsy samples, high-resolution manometry, and multichannel intraluminal impedance/pH monitoring, the symptomatic control group was diagnosed with achalasia (n = 2), esophagogastric junction outflow obstruction (n = 5), distal esophageal spasm (n = 1), GERD (n = 4), and early gastric cancer associated with GERD (n = 2). The main symptoms were chest oppression in the cases of achalasia and esophagogastric junction outflow obstruction, epigastric pain in the cases of GERD and distal esophageal spasm, and early satiety, postprandial fullness, and epigastric pain in the cases of early gastric cancer associated with GERD. The asymptomatic control group included 20 patients (7 females, 13 males) who required EGD for the evaluation of gastric lesions, including early gastric cancer and submucosal tumor.
The study protocol was approved by the ethics committee of Kyushu University Hospital, and written informed consent was obtained from all patients before enrollment. This study was registered with the University Hospital Medical Information Network (UMIN000023397).
Mucosal Electrical Impedance Measurement
During EGD, the MI values in the duodenum and stomach were measured using a tissue conductance meter (TCM AS-TC100; Asch Japan Co., Ltd., Tokyo, Japan); this comprised a 1.9-mm-diameter catheter with a stick-shaped electrode sensor at the tip, similar to that used in a previous report, but with some modifications [16]. The MI measurement was taken as previously described, with some minor modifications [17]. In brief, the reference electrodes were placed on the flexor sides of the bilateral forearms. Another electrode was inserted through the working channel of the endoscope. The mucosa of the greater curvature of the gastric body, gastric antrum, and duodenal bulb was gently touched with the tip of the electrode for 3 s. Alternating currents of 320 Hz and 30.7 kHz were then loaded in turn at a constant voltage of 12.5 mV [17]. The MI of the duodenum and stomach was measured three times in each patient, and the impedance value was accepted whenever the contact between the electrode and the mucosa was stable enough to obtain a constant value. The electrical impedance reflects the resistance in biological tissue [17], wherein biological tissue is considered to be an analogue of a parallel circuit of a resistor and capacitor [18]; the resistor and capacitor of the biological tissue correspond to the barrier integrity and water content, respectively [19, 20]. In this model, the absolute value of electrical impedance (|Z|) is theoretically calculated by the following equation [17]:
where R is the resistance, C is the capacitance, and ω is the angular frequency of the loaded alternating current. As |Z| approximates to R when ω is negligibly small, the optimum low frequency (320 Hz) was determined from the test data so that R was well approximated by |Z| [21]. The MI value obtained at this low frequency (320 Hz) was then used to indicate the mucosal barrier function. The mean duodenal and gastric MI values of the three groups (FD, symptomatic control, and asymptomatic control) were compared. Within the FD group, we also compared the duodenal MI between patients with PDS (n = 16) versus those with EPS (n = 8).
One of the gold standards of MI measurement is the baseline impedance as measured by the multichannel intraluminal pH/impedance test (MII-pH; Sandhill Scientific, Highland Ranch, CO, USA) [22]. Fourteen of the included patients underwent MII-pH, and their lower esophageal MI was also measured. We therefore compared the MI recorded by the tissue conductance meter with the MI recorded by the MII-pH and found that the two values were significantly positively correlated (r = 0.6005, p = 0.023) (Supplementary Figure 1). This finding indicated that the MI measured using the tissue conductance meter in the present study was sufficiently reliable for analysis.
Histological Evaluation of Duodenal Eosinophilic Infiltration
During EGD, we obtained biopsy specimens from the duodenal bulb in 21 patients (12 in the FD group and nine in the symptomatic control group). The extent of eosinophilic infiltration was evaluated by counting the number of eosinophils in five high-powered fields (HPFs). Specimens were evaluated in a blinded manner by two experienced pathologists (T.S. and M.F.).
Extraction of RNA and Quantitative Real-Time Reverse-Transcription Polymerase Chain Reaction
The preparation of total RNA and quantitative real-time reverse-transcription polymerase chain reaction for the assessment of the gene expression in biopsy samples of the duodenal mucosa was performed as described previously [23]. The target mRNA expression levels were examined by reverse-transcription polymerase chain reaction using FAM-labeled TaqMan Gene Expression Assay reagents (Applied Biosystems, Foster City, CA, USA) for primer–probe sets of target genes (Applied Biosystems) for zonula occludens (ZO)-1 (Hs01551861_m1), occludin (Hs00170162_m1), claudin-1 (Hs00221623_m1), claudin-2 (Hs00252666_s1), claudin-3 (Hs00265816_s1), claudin-4 (Hs00976831_s1), protease-activated receptor (PAR)-1 (Hs00169258_m1), PAR-2 (Hs00608346_m1), tumor necrosis factor (TNF)-α (Hs00174128_m1), and interleukin (IL)-1β (Hs01555410_m1). Each well was filled with the cDNA equivalent of 40 ng of RNA plus the volume of TaqMan Universal PCR Master Mix. No AmpErase UNG was required to achieve a final volume of 20 μl; this mixture was then allowed to react using an ABI 7500 fast Real-Time PCR System (Applied Biosystems). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) (Hs03929097_g1) was used as an internal control. The measured threshold cycle (CT) was normalized by subtracting the CT for GAPDH of each sample from that for ZO-1, occludin, claudin-1, claudin-2, claudin-3, claudin-4, PAR-1, PAR-2, TNF-α, and IL-1β. Based on the obtained ΔCT, the ratios of ZO-1, occludin, claudin-1, claudin-2, claudin-3, claudin-4, PAR-1, PAR-2, TNF-α, and IL-1β mRNA to GAPDH mRNA were calculated using the following formula [17]: target mRNA/GAPDH mRNA ratio = 2−ΔCT.
Evaluation of the Association Between Helicobacter pylori Infection and the Duodenal and Gastric Mucosal Electrical Impedance
We examined whether the H. pylori infection status affected the MI in the whole group of 58 patients. The 58 patients were divided in accordance with their H. pylori status into the no infection group (n = 25), eradicated group (n = 18), and current infection group (n = 15); the duodenal and gastric MI values of the three groups were then compared.
Evaluation of the Association Between Proton Pump Inhibitor Usage and the Duodenal and Gastric Mucosal Electrical Impedance
We examined whether PPI usage affected the MI in the whole group of 58 patients. The 58 patients were divided in accordance with their PPI usage into the PPI group (n = 21) and the non-PPI group (n = 37); the duodenal and gastric MI values of the two groups were then compared.
Data and Statistical Analyses
Continuous data were presented as the mean ± standard deviation if appropriate. Data were evaluated by one-way analysis of variance followed by a post hoc Tukey–Kramer significant difference test. A linear regression analysis was used to assess whether dependent variables (ZO-1, occludin, PAR-1, PAR-2, claudin-1, claudin-2, claudin-3, claudin-4, TNF-α, or IL-1β) were related to independent variables (duodenal MI) in order to determine the correlation between the MI and the target mRNA/GAPDH mRNA ratio. After conducting a univariate linear regression analysis, a multivariate linear regression analysis was performed using the stepwise method for all variables. Variables for inclusion in the multivariate linear regression analysis were selected by the stepwise method, by inputting all values of ZO-1, occludin, PAR-1, PAR-2, claudin-1, claudin-2 claudin-3, claudin-4, TNF-α, and IL-1β. Spearman’s correlation coefficient was used to analyze the correlation between ZO-1 and IL-1β. To adjust for the potential effects of age, sex, body mass index (BMI), history of bacterial eradication, proton pump inhibitor (PPI) use, NSAID use, and smoking history, an analysis of covariance (ANCOVA) was carried out to identify differences in the MI between the FD, symptomatic control, and asymptomatic control groups. For the ANVOCA, the values were presented as the mean ± standard error with 95% confidence interval. Bonferroni’s post hoc test was used to detect significant differences between the groups. A two-sided p value of less than 0.05 was considered statistically significant. All statistical analyses were performed with the SPSS software program, version 22.0 for Windows (IBM Japan, Tokyo, Japan).
Results
Clinical Characteristics of the Patients
The clinical characteristics of the patients are shown in Table 1. There were no significant differences between the three groups regarding sex or age. The BMI of the symptomatic control group was significantly lower than that of the asymptomatic control group (p = 0.046); however, there was no significant difference in the BMI between the FD group and the symptomatic control group. The incidence of PPI usage was significantly higher in both the FD group (50.0%) and the symptomatic control group (57.1%) than in the asymptomatic control group (5.0%, p = 0.0015). There were no significant differences between the three groups in the smoking history, drinking history, comorbid disease conditions (hypertension, dyslipidemia, diabetes mellitus, constipation), or H. pylori status.
Mucosal Electrical Impedance in Patients with Functional Dyspepsia
The respective MI values of the gastric antrum and body were 21.4 ± 5.3 Ω and 20.3 ± 5.3 Ω in the FD group, 26.9 ± 7.5 Ω and 24.6 ± 8.2 Ω in the symptomatic control group, and 23.5 ± 8.4 Ω and 24.3 ± 7.7 Ω in the asymptomatic control group (Fig. 1a, b). There was no significant difference between the three groups in the MI values of the gastric antrum (p = 0.11) and gastric body (p = 0.13). In contrast, the MI of the duodenum in the FD group (17.8 ± 4.3 Ω) was significantly lower than that in the symptomatic control group (27.2 ± 6.4 Ω, p < 0.0001) and the asymptomatic control group (23.0 ± 7.4 Ω, p = 0.016) (Fig. 1c). In addition, the MI in the duodenum tended to be lower than that in the gastric antrum in the FD group, although no such difference was observed in the asymptomatic control group. Within the FD group, there was no significant difference in the duodenal MI of the PDS group (18.1 ± 4.7 Ω, n = 16) versus the EPS group (17.1 ± 3.5 Ω, n = 8, p = 0.60).
The mucosal electrical impedance (MI) of the gastrointestinal mucosa in the functional dyspepsia (FD), symptomatic control, and asymptomatic control groups. A tissue conductance meter was used to measure the MI of the gastrointestinal mucosa during esophagogastroduodenoscopy in the gastric antrum (a), gastric body (b), and duodenum (c). The data are shown as the median (interquartile range). *p < 0.05 between the two indicated groups
The ANCOVA adjusted for age, sex, BMI, PPI usage, oral NSAID usage, and smoking history showed that the duodenal MI value of the FD group (17.7 ± 1.3 Ω) was significantly lower than that of the symptomatic control group (27.8 ± 1.7 Ω, p < 0.001) and tended to be lower than that of the asymptomatic control group (22.8 ± 1.6 Ω, p = 0.073); there was no significant difference in the duodenal MI of the symptomatic control group versus the asymptomatic control group (p = 0.17).
mRNA Expression of Tight Junction Proteins or Protease-Activated Receptors in the Functional Dyspepsia and Symptomatic Control Groups
The expression of ZO-1 was significantly lower in the FD group than in the symptomatic control group (p = 0.011). However, there were no significant differences between the FD and symptomatic control groups in the mRNA expressions of the other tight junction proteins (occludin, claudin-1, claudin-2, claudin-3, and claudin-4; Fig. 2a–f), PAR-1, or PAR-2 (Fig. 2g, h). In addition, a subanalysis revealed no significant difference in the expression of ZO-1 between the PDS group (n = 7) and EPS group (n = 5) (p = 0.37).
Duodenally expressed tight junction and protease-activated receptor (PAR) in the functional dyspepsia (FD) and symptomatic control groups. The duodenal mRNA expressions in the FD group and symptomatic control group of tight junction proteins, including zonula occludens (ZO)-1 (a), occludin (b), claudin-1 (c), claudin-2 (d), claudin-3 (e), and claudin-4 (f), and of PAR-1 (g) and PAR-2 (h). The data are shown as the median (interquartile range). *p < 0.05 between the two indicated groups
Univariate Linear Regression Analysis of the Relationship Between the Zonula Occludens-1 Expression and the Duodenal Mucosal Electrical Impedance
A univariate linear regression analysis of the duodenal MI and the tight junction proteins/indicated cytokines revealed that the duodenal MI was positively associated with the expression of ZO-1 (β = 0.513, p = 0.017) (Fig. 3) and negatively associated with the expression of IL-1β (β = − 0.600, p = 0.004). A multiple linear regression analysis revealed that ZO-1 was a significantly positive predictor of duodenal MI (β = 0.424, p = 0.049), while IL-1β was a significantly negative predictor of duodenal MI (β = − 0.486, p = 0.027) (Tables 2, 3).
The results of a linear regression analysis between the duodenal mucosal electrical impedance (MI) and the mRNA expression of zonula occludens (ZO)-1. The relationship between the duodenal MI and the ZO-1 expression as calculated by a linear regression analysis in 21 patients, including those in the functional dyspepsia (FD) group and the symptomatic control group
Associations Between Duodenal Mucosal Electrical Impedance and the Expressions of Interleukin-1β and Tumor Necrosis Factor-α
The IL-1β expression was significantly higher in the FD group than in the symptomatic control (p = 0.041), while there was no significant difference in TNF-α expression between the FD and symptomatic control groups (p = 0.94) (Fig. 4a, b). We then performed a linear regression analysis for 21 patients (12 from the FD group and nine from the symptomatic control group) to determine how IL-1β was related to the duodenal MI. IL-1β was inversely related to the duodenal MI (β = − 0.600, p = 0.004) (Fig. 4c), while the expression of IL-1β was not significantly correlated with that of ZO-1 (ρ = − 0.158, p = 0.49) (Fig. 4d). In addition, a subanalysis revealed no significant difference in the expression of IL-1β between the PDS group (n = 7) and EPS group (n = 5) (p = 0.48).
The expressions of interleukin (IL)-1β and tumor necrosis factor (TNF)-α, the relationship between IL-1β and duodenal mucosal electrical impedance (MI), and the correlation between IL-1β and zonula occludens (ZO)-1. The duodenally expressed cytokines IL-1β (a) and TNF-α (b) in the FD group and symptomatic control group. The data are shown as the median (interquartile range). *p < 0.05 between the two indicated groups. The relationship between the duodenal MI and the IL-1β expression as determined by a linear regression analysis (c), and the correlation between IL-1β and ZO-1 (d) as determined by a Spearman’s correlation coefficient analysis in 21 subjects, including those in the FD group and the symptomatic control group
Eosinophil Count of the Duodenal Mucosa
The eosinophil count of the FD group (19.8 ± 20.0 per five HPFs) tended to be greater than that of the symptomatic control group (11.3 ± 6.9 per five HPFs), although this intergroup difference did not reach statistical significance (p = 0.24). A linear regression analysis found no significant association between the eosinophil count and duodenal MI (β = − 0.116, p = 0.62).
The duodenal eosinophil count of the PDS group (27.1 ± 23.5 per five HPFs) tended to be higher than that of the EPS group (9.4 ± 6.7 per five HPFs) and that of the symptomatic control group; however, this difference was not significant (p = 0.076).
Effects of H. pylori Status on the Duodenal and Gastric Mucosal Electrical Impedance Values
There were no significant differences in duodenal MI between the no infection group (20.8 ± 6.4 Ω), eradicated group (22.6 ± 8.5 Ω), and current infection group (22.8 ± 6.3 Ω) (p = 0.62). Similarly, there were no significant differences in gastric body MI between the no infection group (21.7 ± 5.7 Ω), eradicated group (23.7 ± 8.7 Ω), and current infection group (23.5 ± 7.6 Ω, p = 0.66). The MI of the antrum of the no infection group (20.3 ± 6.0 Ω) was significantly lower than that of the eradicated group (26.2 ± 7.7 Ω, p = 0.026); however, there was no significant difference between the no infection group and the current infection group (25.2 ± 6.9 Ω, p = 0.11).
In a subanalysis performed exclusively for the FD group, there were no significant differences in the duodenal MI between the no infection group (18.2 ± 5.3 Ω, n = 14), eradicated group (17.0 ± 2.6 Ω, n = 7), and current infection group (17.9 ± 1.8 Ω, n = 3) (p = 0.86); in the MI of the antrum between the no infection group (19.5 ± 5.9 Ω), eradicated group (23.6 ± 3.0 Ω), and current infection group (24.6 ± 3.0 Ω) (p = 0.15); or in the MI of the gastric body between the no infection group (21.6 ± 7.0 Ω), eradicated group (17.9 ± 1.9 Ω), and current infection group (20.6 ± 2.3 Ω) (p = 0.45).
Taken together, these findings indicate that the H. pylori infection status affected the MI of the gastric antrum in the total group of enrolled patients. However, the H. pylori infection status did not affect the MI of the duodenum or gastric body in either the FD group or the total group of enrolled patients.
Effects of Proton Pump Inhibitor Usage on the Duodenal and Gastric Mucosal Electrical Impedance
There was no significant difference between the PPI group and the non-PPI group in the MI of the duodenum (21.8 ± 5.8 Ω versus 21.9 ± 7.7 Ω, p = 0.94), gastric antrum (25.1 ± 7.0 Ω versus 22.5 ± 7.3 Ω, p = 0.20), or gastric body (24.5 ± 7.4 Ω versus 21.9 ± 7.0 Ω, p = 0.23).
In a subanalysis performed exclusively for the FD group, there was no significant difference between the PPI group and the non-PPI group in the MI of the duodenum (18.6 ± 4.6 Ω versus 17.0 ± 4.0 Ω, p = 0.37), gastric antrum (22.6 ± 4.6 Ω versus 20.1 ± 5.9 Ω, p = 0.28), or gastric body (22.4 ± 5.8 Ω versus 18.2 ± 4.5 Ω, p = 0.086).
Taken together, these findings indicate that taking PPIs did not affect the duodenal MI or the gastric MI in either the FD group or the total group of enrolled patients.
Discussion
The main findings of the present study were: (1) patients with FD had a relatively decreased MI in the duodenum, but not in the stomach; (2) patients with FD had a decreased expression of ZO-1 and an increased expression of IL-1β compared with the symptomatic control patients; and (3) ZO-1 and IL-1β were positively and negatively associated, respectively, with the duodenal MI in patients with FD.
An increase in the duodenal mucosal permeability occurs with low-grade inflammation [15], and subsequent duodenal hypersensitivity to some mediators, including acids [10], lipids [11], and capsaicin [12], might play an important role in the pathogenesis of FD. Indeed, an increased duodenal mucosal permeability has been directly demonstrated in patients with FD [15, 16]. Furthermore, an ex vivo study using biopsy samples showed that patients with FD have a decreased transepithelial electric resistance and increased paracellular passage compared with healthy volunteers [15]. More recently, a study used a tissue conductance meter to show that the duodenal mucosal permeability is increased in patients with FD [16]. Consistent with these previous findings, the present study showed that the duodenal mucosal barrier function was impaired in patients with FD, although changes in the gastric mucosal barrier function were not involved in the pathogenesis of FD.
One major mechanism of the regulation of the duodenal mucosal barrier function is the involvement of tight junction proteins. The tight junction complex functions as a barrier by controlling the paracellular permeability of endothelial and epithelial cells [24]. Tight junction proteins are composed of several transmembrane molecules, including the ZO, occludin, and claudin families. One study showed that the increased mucosal permeability in patients with FD is likely caused by a decreased expression of tight junction proteins [15]; quantification of the expression of the indicated molecules by measuring the average fluorescence intensity showed lower expressions of ZO-1, occludin, β-catenin, desmocollin-2, and desmoglein-2 in patients with FD compared with control subjects [15]. We therefore examined the expressions of ZO-1, occludin, claudin-1, claudin-2, claudin-3, and claudin-4 and explored their potential association with the impaired duodenal mucosal barrier function. In the present study, the expression of ZO-1 in the FD group was significantly lower than that in the symptomatic control group, while there was no significant difference in the expression of claudin-1–4 between the FD and symptomatic control groups; these results are consistent with those of Vanheel et al. [15]. However, Vanheel et al. [15] also showed that FD was associated with a decreased expression of occludin, which was not seen in our series. The reason for this discrepancy may be that MI is affected by diverse factors, including metabolic conditions (such as type 2 diabetes and obesity) and race [25, 26]. Further studies are required to clarify this point.
The significant positive relationship between the duodenal MI and the ZO-1 expression (Fig. 3) supports the notion that ZO-1 plays an important role in the duodenal MI not only in patients with FD, but also in patients with abdominal symptoms without FD. ZO-1 was the first protein to be identified as a constituent of tight junctions [27]. Both ZO-1 and ZO-2 are essential for the maintenance of the barrier function in epithelial cells [28], and ZO-1 is downregulated in some inflammatory conditions, such as celiac disease [29, 30].
Another mechanism involved in the regulation of the gut mucosal barrier function involves the PAR signaling pathways. Trypsin/PAR-2 receptors play a pivotal role in altering the intestinal permeability [31, 32]. In contrast, thrombin induces barrier disruption mainly through its effect on PAR-1 in endothelial cells [33]. The stimulation of both PAR-1 and PAR-2 induces the reorganization of actin filaments through the phosphorylation of the 20-kD myosin regulatory light chain, which affects tight junction proteins and the barrier function via paracellular pathways [33]. However, no study has yet examined whether PAR is related to changes in the duodenal mucosal barrier function in FD. Therefore, we compared the expressions of PAR-1 and PAR-2 in patients with FD with those in symptomatic control patients, but found no significant difference in their expression between these two groups. In addition, neither the expression of PAR-1 nor PAR-2 was associated with the duodenal MI (Tables 2, 3). These findings suggest that PARs do not affect the duodenal mucosal barrier function in the clinical setting.
Previous studies have shown that low-grade inflammation is associated with the pathogenesis of FD. A study evaluating peripheral blood mononuclear cells found that patients with FD had increased cytokine levels of TNF-α, IL-1β, and IL-10 compared with healthy subjects [34]. IL-1β disrupts the barrier function of epithelial cells, including retinal pigment epithelial cells, intestinal epithelial cells, and human corneal epithelial cells [35,36,37]. Furthermore, IL-1β induces disruption of the barrier function of simian virus 40-immortalized human corneal epithelial cells, which is accompanied by the disappearance of ZO-1 and occludin from the interfaces of neighboring cells through the NF-κB signaling pathway [37]. TNF-α also disrupts the corneal epithelial barrier function by changing the localization of ZO-1 [38]. Therefore, the cytokines IL-1β and/or TNF-α expressed in the duodenum might be associated with its mucosal barrier function, although this has yet to be confirmed. In the present study, the expression of IL-1β was significantly higher in the FD group than in the symptomatic control group, and duodenally expressed IL-1β (but not TNF-α) was significantly inversely correlated with the duodenal mucosal barrier function in all patients, including the patients with FD and the symptomatic control patients (Fig. 4a–c).
The present study found no correlation between the expressions of IL-1β and ZO-1 (Fig. 4d), although the IL-1β expression was significantly higher in the FD group than in the symptomatic control group, suggesting that the IL-1β expressed in the duodenal mucosa may play a role in the pathogenesis of FD. The serum levels of both IL-1β and TNF-α are reportedly increased in patients with FD [34]. However, in our study, only IL-1β mRNA was upregulated in biopsied duodenal mucosa. As IL-1β is released by eosinophils [39], the tendency toward a greater eosinophil count in the FD group than in the symptomatic control group might have affected our findings. Furthermore, macrophages are involved in the production of TNF-α, and macrophage infiltration of the duodenal mucosa is reportedly characteristic of post-infectious FD, with macrophages/TNF-α potentially functioning as mediators of low-grade inflammation [40]. The present study did not include patients with post-infectious FD, which might further explain the discrepancy between the previous findings and our own.
The duodenal eosinophil count is reportedly significantly higher in subjects with non-ulcer dyspepsia based on the Rome II criteria than in controls [14]. The number of duodenal eosinophils in patients with post-infectious FD is reportedly significantly higher than that in healthy volunteers [40]. We therefore examined whether duodenal eosinophilic infiltration was associated with the pathogenesis of FD, and we found that the eosinophil count tended to be higher in the FD group than in the symptomatic control group; however, the difference did not reach statistical significance. In addition, the extent of duodenal eosinophilic infiltration was not significantly associated with the duodenal mucosal barrier function. Patients with PDS with early satiety reportedly have relatively increased duodenal eosinophilic infiltration [41]. The extent of duodenal eosinophilic infiltration tended to be higher in patients with PDS than in both patients with EPS and symptomatic controls in the present study, although this intergroup difference did not reach statistical significance. The lack of an association between PDS and eosinophilia may have been due to a type II (power) error.
The tissue conductance meter used in the present study was originally used to evaluate the electrical impedance of the postauricular skin, nasal turbinates, and nasal polyps in patients with chronic rhinosinusitis [21]. It was then applied to the gastrointestinal area. The MI measured in vivo by a similar method to that used in the present study is generally accepted to be an indicator of the mucosal barrier function [22, 42, 43]. More recently, it has been shown that the duodenal mucosal permeability measured using this tissue conductance meter is increased in patients with FD compared with healthy subjects [16]. Therefore, the present study aimed to clarify how the mucosal barrier function was associated with the pathogenesis of FD and its underlying mechanisms. We showed that the barrier function was not altered in the gastric mucosa, but was altered in the duodenal mucosa, where both increased IL-1β and decreased ZO-1 levels were detected. As we were unable to rule out the possible influence of multiple background factors on the present results, we performed an ANCOVA adjusted for age, sex, BMI, PPI usage, oral NSAID usage, and smoking history; this analysis showed that the mucosal barrier function was altered in patients with FD compared with the two control groups, which suggests that the duodenal MI may be a useful index for differentiating FD from other symptomatic disorders, like GERD, in the clinical setting.
One of the strengths of the present study was the inclusion of a symptomatic control group. There is no objective index to support a diagnosis of FD in clinical practice. Thus, we sometimes encounter patients with FD-like symptoms whose condition is difficult to differentiate from other gastrointestinal disorders, especially from GERD. The present findings suggest that a real-time duodenal MI evaluation during EGD may be useful for differentiating FD from other disorders with abdominal symptoms. Measuring the duodenal mucosally expressed IL-1β may also be useful for confirming a diagnosis of FD in the clinical setting. Although patients with post-infectious FD were not included in the present study, low-grade inflammation is reportedly observed even in non-post-infectious FD [44]. Accordingly, IL-1β may be a target for the novel treatment of FD in the future.
The present study also had several limitations that warrant mention. First, no biopsy samples were obtained from the asymptomatic control group due to ethical issues. To account for this, the biopsy samples from the symptomatic control group were used as a reference. In the symptomatic control group, such biopsy samples were required for the diagnosis of the organic disease. We consider that it was acceptable to use these samples as a reference, as there were no significant differences between the symptomatic control and asymptomatic control groups in the MI values of the duodenum or stomach. Second, our examination of the factors associated with duodenal MI included data from a total of 21 subjects, including 12 patients with FD and nine symptomatic control patients. As the symptomatic control patients had several underlying diseases, we cannot exclude the possibility that this might have affected the results. Third, we showed a significant inverse/positive relationship between the IL-1β/ZO-1 expression and the duodenal barrier function in patients with FD; however, we were unable to determine whether the increased IL-1β and decreased ZO-1 were the cause or the result of FD, and whether IL-1β downregulated the expression of ZO-1 in the clinical setting, as these questions were beyond the scope of the present study. Further studies are necessary to clarify these points.
In conclusion, we used a newly developed method involving the real-time measurement of the MI during EGD to show that the mucosal barrier function of the duodenum, but not of the stomach, is altered in patients with FD. The duodenal MI is significantly positively correlated with ZO-1 and inversely correlated with IL-1β. Both ZO-1 and IL-1β may play a role in the pathogenesis of FD, and IL-1β might be a novel target for the treatment of FD.
References
Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology. 2006;130:1466–1479.
El-Serag HB, Talley NJ. The prevalence and clinical course of functional dyspepsia. Aliment Pharmacol Ther. 2004;19:643–654.
Suzuki H. The application of the Rome IV criteria to functional esophagogastroduodenal disorders in Asia. J Neurogastroenterol Motil. 2017;23:325–333.
Halling K, Kulich K, Carlsson J, Wiklund I. An international comparison of the burden of illness in patients with dyspepsia. Dig Dis. 2008;26:264–273.
Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352.
Lunding JA, Tefera S, Gilja OH, et al. Rapid initial gastric emptying and hypersensitivity to gastric filling in functional dyspepsia: effects of duodenal lipids. Scand J Gastroenterol. 2006;41:1028–1036.
Shindo T, Futagami S, Hiratsuka T, et al. Comparison of gastric emptying and plasma ghrelin levels in patients with functional dyspepsia and non-erosive reflux disease. Digestion. 2009;79:65–72.
Boeckxstaens GE, Hirsch DP, Kuiken SD, Heisterkamp SH, Tytgat GN. The proximal stomach and postprandial symptoms in functional dyspeptics. Am J Gastroenterol. 2002;97:40–48.
Tack J, Caenepeel P, Fischler B, Piessevaux H, Janssens J. Symptoms associated with hypersensitivity to gastric distention in functional dyspepsia. Gastroenterology. 2001;121:526–535.
Bratten J, Jones MP. Prolonged recording of duodenal acid exposure in patients with functional dyspepsia and controls using a radiotelemetry pH monitoring system. J Clin Gastroenterol. 2009;43:527–533.
Feinle C, Meier O, Otto B, D’Amato M, Fried M. Role of duodenal lipid and cholecystokinin A receptors in the pathophysiology of functional dyspepsia. Gut. 2001;48:347–355.
Hammer J, Fuhrer M. Clinical characteristics of functional dyspepsia depending on chemosensitivity to capsaicin. Neurogastroenterol Motil. 2017;29:1–12.
Kindt S, Tertychnyy A, de Hertogh G, Geboes K, Tack J. Intestinal immune activation in presumed post-infectious functional dyspepsia. Neurogastroenterol Motil. 2009;21:832–856.
Talley NJ, Walker MM, Aro P, et al. Non-ulcer dyspepsia and duodenal eosinophilia: an adult endoscopic population-based case–control study. Clin Gastroenterol Hepatol. 2007;5:1175–1183.
Vanheel H, Vicario M, Vanuytsel T, et al. Impaired duodenal mucosal integrity and low-grade inflammation in functional dyspepsia. Gut. 2014;63:262–271.
Ishigami H, Matsumura T, Kasamatsu S, et al. Endoscopy-guided evaluation of duodenal mucosal permeability in functional dyspepsia. Clin Transl Gastroenterol. 2017;8:e83.
Koizumi H, Suzuki H, Ohbuchi T, Kitamura T, Hashida K, Nakamura M. Increased permeability of the epithelium of middle ear cholesteatoma. Clin Otolaryngol. 2015;40:106–114.
Yamamoto T, Yamamoto Y. Electrical properties of the epidermal stratum corneum. Med Biol Eng. 1976;14:151–158.
Lawrence JN. Electrical resistance and tritiated water permeability as indicators of barrier integrity of in vitro human skin. Toxicol In Vitro. 1997;11:241–249.
Martinsen OG, Grimnes S, Nilsen SH. Water sorption and electrical properties of a human nail. Skin Res Technol. 2008;14:142–146.
Suzuki H, Koizumi H, Ikezaki S, et al. Electrical impedance and expression of tight junction components of the nasal turbinate and polyp. ORL J Otorhinolaryngol Relat Spec. 2016;78:16–25.
Farre R, Blondeau K, Clement D, et al. Evaluation of oesophageal mucosa integrity by the intraluminal impedance technique. Gut. 2011;60:885–892.
Iboshi Y, Nakamura K, Ihara E, et al. Multigene analysis unveils distinctive expression profiles of helper T-cell-related genes in the intestinal mucosa that discriminate between ulcerative colitis and Crohn’s disease. Inflamm Bowel Dis. 2014;20:967–977.
Zihni C, Mills C, Matter K, Balda MS. Tight junctions: from simple barriers to multifunctional molecular gates. Nat Rev Mol Cell Biol. 2016;17:564–580.
Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60.
Thaiss CA, Levy M, Grosheva I, et al. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science. 2018;359:1376–1383.
Stevenson BR, Siliciano JD, Mooseker MS, Goodenough DA. Identification of ZO-1: a high molecular weight polypeptide associated with the tight junction (zonula occludens) in a variety of epithelia. J Cell Biol. 1986;103:755–766.
Umeda K, Ikenouchi J, Katahira-Tayama S, et al. ZO-1 and ZO-2 independently determine where claudins are polymerized in tight-junction strand formation. Cell. 2006;126:741–754.
Montalto M, Cuoco L, Ricci R, Maggiano N, Vecchio FM, Gasbarrini G. Immunohistochemical analysis of ZO-1 in the duodenal mucosa of patients with untreated and treated celiac disease. Digestion. 2002;65:227–233.
Pizzuti D, Bortolami M, Mazzon E, et al. Transcriptional downregulation of tight junction protein ZO-1 in active coeliac disease is reversed after a gluten-free diet. Dig Liver Dis. 2004;36:337–341.
Bueno L, Fioramonti J. Protease-activated receptor 2 and gut permeability: a review. Neurogastroenterol Motil. 2008;20:580–587.
Jacob C, Yang PC, Darmoul D, et al. Mast cell tryptase controls paracellular permeability of the intestine. Role of protease-activated receptor 2 and beta-arrestins. J Biol Chem. 2005;280:31936–31948.
Hirano M, Hirano K. Myosin di-phosphorylation and peripheral actin bundle formation as initial events during endothelial barrier disruption. Sci Rep. 2016;6:20989.
Liebregts T, Adam B, Bredack C, et al. Small bowel homing T cells are associated with symptoms and delayed gastric emptying in functional dyspepsia. Am J Gastroenterol. 2011;106:1089–1098.
Al-Sadi RM, Ma TY. IL-1β causes an increase in intestinal epithelial tight junction permeability. J Immunol. 2007;178:4641–4649.
Cui HS, Hayasaka S, Zhang XY, Hayasaka Y, Chi ZL, Zheng LS. Effect of berberine on barrier function in a human retinal pigment epithelial cell line. Jpn J Ophthalmol. 2007;51:64–67.
Kimura K, Teranishi S, Nishida T. Interleukin-1β-induced disruption of barrier function in cultured human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2009;50:597–603.
Tanaka H, Fukuda K, Ishida W, Harada Y, Sumi T, Fukushima A. Rebamipide increases barrier function and attenuates TNFα-induced barrier disruption and cytokine expression in human corneal epithelial cells. Br J Ophthalmol. 2013;97:912–916.
Esnault S, Kelly EA, Nettenstrom LM, Cook EB, Seroogy CM, Jarjour NN. Human eosinophils release IL-1β and increase expression of IL-17A in activated CD4+ T lymphocytes. Clin Exp Allergy. 2012;42:1756–1764.
Futagami S, Shindo T, Kawagoe T, et al. Migration of eosinophils and CCR2-/CD68-double positive cells into the duodenal mucosa of patients with postinfectious functional dyspepsia. Am J Gastroenterol. 2010;105:1835–1842.
Walker MM, Salehian SS, Murray CE, et al. Implications of eosinophilia in the normal duodenal biopsy—an association with allergy and functional dyspepsia. Aliment Pharmacol Ther. 2010;31:1229–1236.
Saritas Yuksel E, Higginbotham T, Slaughter JC, et al. Use of direct, endoscopic-guided measurements of mucosal impedance in diagnosis of gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10:1110–1116.
van Rhijn BD, Weijenborg PW, Verheij J, et al. Proton pump inhibitors partially restore mucosal integrity in patients with proton pump inhibitor-responsive esophageal eosinophilia but not eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2014;12:1815–1823.
Li X, Chen H, Lu H, et al. The study on the role of inflammatory cells and mediators in post-infectious functional dyspepsia. Scand J Gastroenterol. 2010;45:573–581.
Acknowledgment
We appreciate the technical assistance we received from the Research Support Center, Research Center for Human Disease Modeling, Kyushu University Graduate School of Medical Sciences. We thank Kelly Zammit, BVSc, from Edanz Editing (www.edanzediting.com/ac), for editing a draft of this manuscript.
Author information
Authors and Affiliations
Contributions
KK and HO proposed the study. KK, EI, and YM performed the research. KK and YM collected and analyzed the data. TS, MF, and YO performed the histological diagnosis. KK and EI wrote the manuscript. YO supervised the study. All authors contributed to the interpretation of the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.

10620_2019_5470_MOESM1_ESM.jpg
Supplemental Figure 1. Correlation between the esophageal mucosal electrical impedance (MI) measured using the 24-h multichannel intraluminal pH/impedance test (MII-pH) versus the tissue conductance meter. The esophageal MI was measured in 14 patients (from either the functional dyspepsia group or the symptomatic control group) using both the MII-pH and the tissue conductance meter. The correlation between the MI values obtained using the different devices was calculated by performing Pearson’s correlation analysis. (JPEG 173 kb)
Rights and permissions
About this article
Cite this article
Komori, K., Ihara, E., Minoda, Y. et al. The Altered Mucosal Barrier Function in the Duodenum Plays a Role in the Pathogenesis of Functional Dyspepsia. Dig Dis Sci 64, 3228–3239 (2019). https://doi.org/10.1007/s10620-019-5470-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-5470-8