Abstract
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-known procedure with both diagnostic and therapeutic utilities in managing pancreaticobiliary conditions. With the advancements of endoscopic techniques, ERCP has become a relatively safe and effective procedure. However, as ERCP is increasingly being utilized for different advanced techniques, newer complications have been noticed. Post-ERCP complications are known, and mostly include pancreatitis, infection, hemorrhage, and perforation. The risks of these complications vary depending on several factors, such as patient selection, endoscopist’s skills, and the difficulties involved during the procedure. This review discusses post-ERCP complications and management strategies with new and evolving concepts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Endoscopic retrograde cholangiopancreatography (ERCP) remains the standard procedure for evaluation and management of pancreaticobiliary conditions. Over time, the utility of ERCP has increased dramatically, and the role of ERCP in medical management has expanded from a diagnostic procedure to one that is mostly therapeutic. While this expansion has improved treatment modalities for biliary pathology, complications and adverse events following ERCP continue to persist and may have a significant impact on patients’ morbidity and rarely mortality [1]. Generally, ERCP is considered to be safe and effective. Several retrospective studies have demonstrated that ERCP is safe and efficacious, even in high-risk populations such as the elderly, who often have chronic diseases that are aggravated by medical procedures [2, 3]. Though it is a safe, ERCP carries the highest risk of procedure-related complications among endoscopic procedures. Despite advances in endoscopic technology, operator skills, and research-driven safety protocols, the incidence of ERCP-related complications and mortality remains relatively constant. Several distinct studies reported consistent ERCP complications and mortality rates over a decade between 10–12% and 0.4–1.4%, respectively [4,5,6].
Common post-ERCP complications include pancreatitis, hemorrhage, cholecystitis, infection, and intestinal perforation (Fig. 1). Post-ERCP pancreatitis (PEP) is the most frequent adverse event following the procedure. The epidemiologic description of PEP is challenging depending on the presence of the patient, procedural and cumulative risk factors, and the clinical criteria used to define PEP and method of data collection/study design [7, 8]. In addition to morbidity and mortality, ERCP-related complications have important healthcare-associated cost implications, with annual costs surpassing 150 million dollars in the USA. Furthermore, a minority (5%) of complications are advanced, requiring the use of additional resources to treat them and extended hospital stay [9,10,11]. Beyond healthcare expenditures, ERCP-related complications are taxing and may impose significant psychosocial effects on endoscopists [12]. Given the burden on patients and clinicians, understanding and reducing post-ERCP complications are paramount. In this study, after a review of several articles, we present ERCP-related complications, patient and procedural risk factors for post-ERCP complications, strategies to prevent adverse complications, and potential strategies for management.
Complications of ERCP
Post-ERCP Pancreatitis (PEP)
Post-ERCP pancreatitis (PEP) is the most frequent complication following ERCP, with an incidence ranging between 1.6 and 15%, with an average of 3–5% as reported in most studies [11, 13,14,15,16,17,18,19,20,21,22,23,24,25,26]. The discrepancy in incidence rates is mainly due to varying definitions of PEP and its classification system. In most cases, PEP is mild or moderate and follows a severe course in only a minority of cases. A systematic review of 108 placebo or no-stent arms of RCTs with 13,296 patients showed a global PEP incidence of 9.7% with a mortality of 0.7%. The PEP severity information was available only for 8857 patients, which were mild in 5.7%, moderate in 2.6%, and severe in only 0.5% of cases [11].
Two widely used definitions of PEP have been described in the literature (Table 1). The original consensus definition and classification of PEP were first described in 1991 by Cotton et al. The diagnosis of PEP is based on (1) the presence of new or worsening abdominal pain clinically consistent with acute pancreatitis, (2) serum lipase and/or amylase activity at least three times the upper limit of normal (ULN) at 24 h following the procedure and (3) hospitalization or prolongation of existing hospitalization of at least two nights [27]. The second definition is the revised Atlanta international consensus (RAC) definition and classification of acute pancreatitis (AP) (Table 1). The RAC defines AP as the presence of ≥ 2 of the following: characteristic acute abdominal pain, post-ERCP, serum amylase and/or lipase ≥ 3 times the upper limit of normal (ULN) after 24 h of ERCP, and/or an abdominal computed tomography (CT) scan with findings consistent with AP [28].
Mechanisms of PEP
The exact pathogenesis of PEP is not clear, but several mechanisms have been suggested in the literature (Fig. 2). One proposed mechanism of injury is direct mechanical trauma, whereby prolonged or difficult instrument manipulation, such as guidewire manipulation, causes ductal edema leading to obstruction to the outflow of pancreatic secretions. Another proposed mechanism is chemical injury due to injected contrast. Hydrostatic injury may also occur from increased pressure in the pancreatic duct from manometry without aspiration or contrast injection. Infection resulting from the introduction and ascension of intestinal flora and/or bacteria from endoscope or contrast media into the pancreatic duct may also represent another mechanism of injury. Additionally, a thermal injury may also result from the use of electrocautery during sphincterotomy [29, 30].
Risk Factors for PEP
Understanding the risk factors for PEP is essential to reduce its risk and improve procedural safety. It is also vital to identify high-risk cases before the procedure so that the procedure can be avoided altogether if possible or the procedure time can be minimized. Risk factors for non-ERCP pancreatitis are vastly different from those involved in ERCP-induced pancreatitis. Unlike PEP, gallstones, alcohol abuse, and infection are the key risk factors for non-ERCP pancreatitis [31]. However, several other risk factors for PEP have been identified and have previously been categorized as the patient, procedure, and operator-related factors.
Most importantly, cumulative risk has been recognized as a significant factor as more than one risk factor exists. Established risk factors for PEP include suspected sphincter of Oddi dysfunction (SOD), female gender, medical history of acute pancreatitis, prior history of PEP, normal serum bilirubin levels, and nondilated extrahepatic bile ducts [17, 23, 32,33,34,35]. Earlier literature suggests that chronic pancreatitis serves as a protective factor against PEP, possibly because of decreased enzymatic exocrine function and pancreatic atrophy. However, a recent retrospective study by Phillip et al. identified chronic pancreatitis as an independent risk factor for PEP [odds ratio (OR) 3.7]. The reason for this phenomenon is not entirely apparent, but the extent of existing chronic pancreatitis may influence the risk for PEP [36].
Younger patient age (< 60 years) is also a well-known risk factor for the development of PEP. Studies have confirmed that the prevalence of PEP in patients younger than 60 years (14.14%) is significantly higher than the patients > 60 years old (5.03%) [37]. The decreased risk may reflect the functional decline of the pancreas associated with age or the degrading pancreatic parenchyma, resulting in a weaker response to mechanical insults by ERCP [23]. However, another proposed theory is that in younger patients, pancreatic function and sensitivity are more robust and elicit a greater response to injury compared to older patients [37]. Other less explored risk factors for PEP have been implicated including intraductal papillary mucinous neoplasms (IPMNs), the absence of common bile duct (CBD) stones, periampullary diverticula, pregnancy and obesity [37,38,39,40,41]. Initially, early feeding was thought to increase the risk of PEP, but an RCT by Park et al. [42] on asymptomatic patients with serum amylase < 1.5 fold the ULN at 4 h revealed that early feeding does not increase the incidence of PEP and associated with reduced costs. Similarly, underlying diseases, such as hypertension, diabetes, cirrhosis, have also been shown to have little to no effect on the occurrence of PEP [37].
Cumulative Effect
It is essential to understand that risk factors for PEP have a cumulative effect, and the risk of PEP is increased for each additional patient risk factor. In patients with multiple risk factors, the rate of PEP has been reported to be as high as 40%. This phenomenon also explains the different reports of the incidence of PEP [24, 28]. For example, a female patient, with a suspected SOD, normal bilirubin, and difficult cannulation, is theoretically at a much more increased risk for PEP and also more likely to follow a severe course of PEP.
Procedural Factors
In addition to patient characteristics, the risk of PEP is also determined as much by procedural factors. Understanding the risk associated with procedural techniques can help clinicians choose the best approach for each patient. Several procedure-related risk factors have been identified in the literature: difficult cannulation, pancreatic duct wire passages, pancreatic sphincterotomy, ampullectomy, pancreatic duct development, repeated or aggressive pancreatography, failed clearance of bile duct stones, and short-duration balloon dilation of an intact biliary sphincter. Multiple studies have confirmed these as independent risk factors [34, 43]. Importantly, as it pertains to electrocautery, the use of pure or blended current does not influence the risk of PEP [44].
Operator Factors
ERCP is a technical procedure and can be challenging to perform. Therefore, operator-related risk factors, including case volume and trainee participation, have been suggested to influence the risk of PEP. One study demonstrated an independent increase in the risk of PEP with trainee involvement, but other studies have not demonstrated increased rates of PEP with trainee participation [17, 18, 20]. Iida et al. [45] investigated the efficacy and safety of endoscopic treatments for CBD stones by trainees in a single-center retrospective study and found that bile duct catheter insertion success rates and complete stone removal rates were similar for trainees and experts. Case volume has also been suggested as a risk factor. Little evidence exists that ERCP case volume influences the rate of post-ERCP pancreatitis. Two studies, Williams et al. and Testoni et al. [22, 46] demonstrated that the risk of pancreatitis was not associated with the case volume.
Prevention of PEP
Given the health implications of post-ERCP complications, understanding which endoscopic technique most effectively reduce PEP is essential (Fig. 3).
Endoscopic Techniques
Pancreatic Duct Stenting
Pancreatic duct stenting, which allows appropriate outflow of the pancreatic fluids and relief of pancreatic ductal hypertension, is effective in preventing PEP. It is recommended in high-risk (difficult biliary cannulation, SOD manometry, ampullectomy, etc.) cases for prevention of PEP. Several studies have demonstrated a remarkable decrease in the incidence and severity of PEP with prophylactic pancreatic duct stenting [47, 48]. The use of stents in patients with low risk of PEP is not apparent, nor is the proper timing of stent placement (i.e., preceding or the following sphincterotomy) or location of stent placement. However, given that difficulty with pancreatic duct drainage can lead to proteinase activation and worsening pancreatitis, Sugimoto et al. [49] showed pancreatic stent placement up to the pancreatic body or tail specifically may allow better duct drainage than stent placement in the pancreatic head. The ideal period of stent retention is not precise. Some authors have proposed that prolonged retention of stents causes ductal changes similar to those in chronic pancreatitis [13]. Other studies have shown that allowing stents to remain in place for 7–10 days results in a decreased incidence of PEP compared to the immediate removal of stents following the procedure [50].
Guidewire-Assisted Cannulation
Guidewire-assisted cannulation improves the efficiency and limits the injection of contrast into the pancreas during cannulation. A meta-analysis (n = 3450) demonstrated that the wire-guided method significantly decreased the incidence of PEP by half, increased initial cannulation success, reducing the need to use precut sphincterotomy, and limited other ERCP-related complications [51]. However, multiple pancreatic guidewire passages may increase PEP risk due to damage to the orifice of the Wirsung’s duct. Therefore, if the unintended insertion of a guidewire into the pancreatic duct occurs, endoscopists should consider protective stent placement [8].
Papillary Fistulotomy
Papillary fistulotomy (PF) is another alternative to overcoming complicated biliary tract cannulation. A recent prospective study (n = 102) by Furuya et al. [52] found that PF was more effective than guidewire cannulation in maintaining lower amylase/lipase levels. Advanced cannulation techniques, such as transpancreatic sphincterotomy (TPS) and needle-knife precut papillotomy (NKPP) have also been utilized to gain biliary access to reduce ERCP complications further. While NKPP helps to improve the ERCP success rate under challenging cannulations, it also increases the risk of bleeding and perforation. In a meta-analysis, Pecsi et al. [53] compared the efficacy and complication rates of TPS to NKPP and found that TPS superior in achieving difficult biliary access and causes less bleeding than NKPP, but there were no differences in rates of PEP, perforation, or total complication.
Others
As reported earlier, assistance with cannulation may help reduce PEP. Intraduodenal acetic acid infusion is a method of catalyzing secretin release which has been shown to facilitate pancreatic duct cannulation and possibly reduce complications. In an RCT by Fang et al., the intraduodenal acetic acid infusion was found to significantly decrease difficult pancreatic cannulation rate, facilitate pancreatic duct cannulation, and reduce radiation exposure [54]. Patients with altered anatomy may also present challenges in endoscopic evaluations and predispose them to additional risks of complications. Thus, a knowledge of the right choice of endoscopic devices limits complications can be helpful. A recent retrospective study by Mbatashi et al. [55] showed that in Billroth II patients, use of conventional duodenoscope produced the lowest rate of adverse events (6.1%), followed by 10.7% with the use of single-balloon enteroscopy and 33.3% with a pediatric colonoscope. In patients with periampullary diverticula (PAD), cannulation can be extremely difficult. Karaahmet et al. found that needle-knife fistulotomy might be a feasible option to help facilitate successful biliary cannulation in these patients [38].
Pharmacological Prevention of PEP
Several types of medical therapies have been proposed in the prevention of PEP (Fig. 3). Nonsteroidal anti-inflammatory drugs (NSAIDs) inhibit key mediators (prostaglandins and phospholipase A2) involved in PEP. Due to their rapid onset and higher bioavailability, rectal administration of NSAIDs has proven superior to the oral administration in preventing PEP [56]. The preferred NSAIDs are indomethacin and diclofenac as they are superior to naproxen in the prevention of PEP. In a double-blind, randomized trial, patients with rectal administration of diclofenac and indomethacin had a much lower incidence (4% and 5.8%, respectively) of PEP than those who received naproxen (15.9%) [57]. Another meta-analysis of RCTs showed that 100 mg diclofenac or indomethacin immediately before or after ERCP decreases PEP risk from 12.5 to 4.4% [58]. However, some conflicting studies about the role of rectal NSAIDs do exist which could be due to the types of NSAIDs used. Martinez L et al. investigated the use of prophylactic diclofenac in a mixed cohort of patients undergoing ERCP and found that PEP was noted in 3.4% of patients who received prophylactic rectal diclofenac and 2.8% in patients who did not receive diclofenac (p = 0.554) [59].
The timing (i.e., pre-ERCP, post-ERCP) administration of NSAIDs may also affect the PEP incidence. A meta-analysis of 21 RCTs showed that post-ERCP administration of indomethacin (RR, 0.47; 95% CI 0.31–0.70; p = 0.0002) was more effective in preventing PEP than pre-ERCP administration (RR, 0.59; 95% CI 0.45–0.79; p = 0.0003). However, pre-ERCP administration of diclofenac (RR, 0.32; 95% CI 0.16–0.63; p = 0.001) was more effective than that in post-ERCP (RR, 0.65; 95% CI 0.27–1.599; p = 0.35). [60]. Another meta-analysis of six RCTs inclusive of 2229 patients showed that pre-ERCP administration of rectal indomethacin reduced the risk of PEP as compared to placebo (RR 0.60, 95% CI 0.45–0.80; p < 0.0001) [61]. However, another meta-analysis by Yang et al. showed that a single dose of rectal NSAIDs (both diclofenac and indomethacin) is effective in the prevention of PEP regardless of the timing of administration [62].
The recommended NSAIDs dose for PEP varies regionally, and safety and efficacy have contended with varying doses. While many Western countries utilize a 50–100 mg rectal dose of NSAIDs to prevent PEP, a 25 mg dose is recommended in Japan. A retrospective study found that a 25 mg rectal dose of diclofenac was effective in the prevention of PEP [63].
When NSAIDs are contraindicated, somatostatin may provide some benefit in patients with PEP risk. Wang et al. conducted a meta-analysis of the placebo-controlled RCTs and found that prophylactic use of long-term somatostatin injection can significantly reduce the incidence of PEP in high-risk patients PEP (8.4% in the placebo vs. 5.8% in somatostatin group). However, short-term or bolus injection of somatostatin was not found to be useful [64].
Nitric oxide (NO) use may also help prevent PEP by reducing the amplitude and baseline pressure produced by the sphincter of Oddi and inhibit resting SO activity, thereby allowing easier CBD cannulation [65,66,67]. Additionally, IV glucagon has been used during ERCP to inhibit duodenal motility and relax the SO for similar reasons [68]. In a double-blind randomized study (n = 455), Katsinelos et al. demonstrated that the rate of PEP was significantly lower in the group who received 2.4 mg sublingual nitroglycerin and glucagon 1 mg IV versus the group of patients who received 6 puffs of sterile water and 20 mg hyoscine-n-butyl bromide IV (3.08% vs. 7.46%, p = 0.037) [69]. IV hydration therapy also helps prevent continuous injury to the pancreas from hypoperfusion. Current ASGE guidelines recommend administration of periprocedural lactated Ringer (LR) solution administration to reduce PEP [9]. In addition to preventing hypoperfusion, LR solution is thought to be useful in preventing acidosis that exacerbates pancreatitis. In a randomized study on first time ERCP patients, aggressive hydration with LR (3 mL/kg/h periprocedure, a post-procedure 20-mL/kg bolus followed by 3 mL/kg/h for 8 h, n = 39) was found to be superior than standard LR hydration (periprocedural 1.5 mL/kg/h and for 8 h after procedure, n = 23) (p = 0.016) [70]. A recent systematic review and meta-analysis of RCTs (n = 722) showed that the aggressive hydration with LR solution is associated with a lower incidence of PEP (OR = 0.29; 95% CI 0.16–0.53) and moderate-to-severe PEP (OR = 0.16; 95% CI 0.03–0.96) and shorter duration of length of stay [71].
Given that oxidative stress also plays a role in the pathogenesis of pancreatitis, antioxidative agents should theoretically improve outcomes. However, a meta-analysis by Goosh et al. found that antioxidant therapy had no significant effect on the incidence of PEP [72]. Other studies have shown that allopurinol, glucocorticoids, ceftazidime, glyceryl trinitrate, interleukin-10, and gabexate are not consistently effective therapies for prevention of PEP, and thus are not routinely recommended [73, 74].
Appropriate Patient Selection
Appropriate patient selection is an integral part of reducing the incidence of PEP. Endoscopists should thoroughly review the patient risk factors to determine if alternatives to therapeutic ERCP can be used, especially in patients with multiple risk factors (such as SOD, female gender, age < 60, etc.). As mentioned earlier, ERCP is now mostly therapeutic and should be primarily utilized in patients whose clinical condition requires therapeutic intervention. Therefore, a better understanding of the clinical conditions is required, which may allow choosing safer, less invasive, and accurate diagnostic modalities. For example, MRCP or EUS may be used instead of ERCP to diagnose choledocholithiasis, without the associated risk of PEP complications [9, 73].
Bleeding
Bleeding is another significant complication associated with ERCP (Table 1). The rate of post-sphincterotomy bleeding after ERCP is estimated to be 0.3–2% [13, 24, 25, 75]. Bleeding can be further classified as insignificant or clinically significant based on a change in hemoglobin and the absence/presence of overt GI bleeding. In a multicenter study on 2347 patients undergoing endoscopic biliary sphincterotomy showed that about 48 (2%) patients developed hemorrhage. Another study from Italy showed the rate of hemorrhage to be about 1.13% [13, 16]. The most common reported causes of the ERCP bleeding were endoscopic biliary and pancreatic sphincterotomy. Other less common causes of post-ERCP bleeding include hemobilia, pseudoaneurysm, and splenic, hepatic, and/or vascular injury [9].
Risk Factors for Post-ERCP Bleeding
Patient-Related
Patient-related risk factors for post-sphincterotomy bleeding include coagulopathy, use of anticoagulants within 3 days of ERCP, and active cholangitis [76]. The role of anticoagulants and antiplatelets in post-ERCP bleeding has been a topic of interest as the use of antithrombotic therapy, as well as dual antiplatelet agents (APA) and acetylsalicylic acid (ASA) increases the risk of bleeding. ASGE guidelines suggest withholding APAs when undergoing ERCP, whether urgently or emergently. However, in some cases, emergent ERCP interventions are indicated [9]. The precise risk of performing ERCP interventions in patients taking APAs within a few days or even on the ERCP day has been unclear in the literature. A multicenter retrospective study did not find a statistically significant association of the type and combination of APAs and the number of days the APAs were held with post-ERCP bleeding on multivariate analysis [75]. On the other hand, several factors which were thought to increase the risk of post-ERCP hemorrhage but have been discredited including the use of aspirin or NSAIDs within 3 days of ERCP, ampullary tumor, prolonged sphincterotomy, periampullary diverticulum, and extension of prior sphincterotomy [75].
Procedure-Related
Endoscopic biliary and pancreatic sphincterotomy are some of the most common procedure-related cause of post-ERCP bleeding [77, 78]. On multivariable analysis, Masci et al. [16] found that percutaneous sphincterotomy and papilla orifice stenosis were significantly associated with bleeding. Additionally, the occurrence of any bleeding observed during the procedure is a risk factor [13]. However, endoscopist case volume can also be another risk factor as one study found that case volume per week was an operator-related risk factor for post-ERCP bleeding [13].
Prevention of Post-ERCP Bleeding
Prevention of post-ERCP bleeding can be divided into appropriate patient selection and endoscopists-related measures. Several strategies, mainly related to modifying procedural techniques, have been proposed to reduce post-endoscopic sphincterotomy (post-EST) bleeding. One method to reduce the risk of bleeding is to avoid unnecessary sphincterotomy in high-risk patients [9]. Additionally, EST alternatives such as endoscopic papillary large balloon dilatation (EPLBD) can be employed in patients with coagulopathy. One study found that EPLBD without endoscopic sphincterotomy is best to use in patients with coagulopathy and increased risk for post-sphincterotomy bleeding [79]. Other strategies include using blended rather than pure-cutting current and the use of a microprocessor-controlled generator to decrease the risk of post-sphincterotomy bleeding [80].
Pharmacotherapeutic Prevention of Bleeding
Few studies have evaluated the role of pharmacological intervention in preventing post-EST bleeding. Limited evidence has indicated that acid suppression by proton pump inhibitors (PPIs) might decrease the risk of immediate and delayed bleeding. In an open-label randomized study (n = 125) by Leung, PPIs did not reduce post-EST bleeding, decrease in hemoglobin (Hb), need for blood transfusion, and length of stay. Immediate bleeding was noted in 15% of patients who received PPIs and 6.2% who did not (p = 0.14), and delayed bleeding was seen in 3.3% of patients receiving PPI and 7.7% receiving standard care (p = 0.44) [81].
Basic management of post-EST bleeding includes fluid resuscitation, the reversal of coagulopathy, and blood transfusion. Injection of dilute epinephrine into and around the sphincterotomy site, in addition to argon plasma coagulation and/or multipolar electrocautery, may be used to treat significant hemorrhage [76, 82]. Other tools for managing intraprocedural bleeds include balloon tamponade of the sphincterotomy site and fully covered self-expandable metal stents (FCSEMSs) in refractory bleeding may also be used [83]. Lastly, angiographic embolization can be used for hemobilia originating from above the hilum [84].
Infection
Endoscopy-related bacteremia does carry a risk of spread to distant tissues and organs. The most common infections following ERCP include cholangitis and duodenoscope-related infection and to a lesser degree, infective endocarditis [9]. The most common bacteria involved in biliary tract infection include mostly gram-negative organisms (such as E. coli., Klebsiella spp., Pseudomonas aeruginosa, Enterococcus spp.) and less commonly gram-positive bacteria (such as Staph. epidermidis, Streptococcus spp., E. faecium) [74, 85]. Generally, the most often recognized risk factors for post-ERCP infection include the use of combined percutaneous and endoscopic procedures, stent placement in malignant strictures, jaundice, low case volume, and incomplete biliary drainage [74].
Cholangitis
Cholangitis and sepsis are well-known complications of ERCP, with an incidence of 0.5% to 3%. Clinical presentation includes fever, jaundice, and abdominal pain, and occasionally hypotension and altered mental status in severe cases [9]. Risk factors include old age, previous ERCP history, and hilar obstruction. Patients with incomplete biliary drainage or prior history of liver transplantation have the highest risk of post-ERCP cholangitis [85]. The risk of cholangitis can be up to 10% in patients who have retained stone fragments following mechanical lithotripsy. Consequently, bile stone extraction serves as a protective factor [85]. Specific techniques are used to decompress an obstructed bile duct-like endoscopic sphincterotomy, stent insertion, and/or balloon dilatation, though therapeutic and necessary but also increase risks of cholangitis [86].
The mechanism of infection involves colonization by bacteria or endotoxins that penetrate the bile crosses the blood barrier in the setting of biliary stasis or during a prolonged ERCP operation [85]. Another mechanism is by damage to the epithelium during contrast injection or other procedures that allow a conduit for bacteria to enter. Previously placed stents may also become obstructed (due to stone fragments, bacterial biofilm, sludge, tumor or tissue growth) and block the lumen of the stent, resulting in delayed infection. Furthermore, in patients with an obstructed bile duct, stent migration may occur and result in cholangitis. Of note, metal stents are associated with fewer risks [9].
Prevention of Cholangitis
Several strategies are recommended to reduce the risk of post-ERCP cholangitis. Pharmacologic prophylaxis (coverage for enteric gram-negative organisms and enterococci) before ERCP is recommended for any patient with a history of liver transplantation or has known or suspected biliary obstruction that may be incompletely drained. However, routine use of antibiotics before ERCP is not recommended in the absence of suspected biliary obstruction, anticipated difficulty with complete biliary drainage, sclerosing cholangitis, pancreatic pseudocysts, and immunocompromised status [9]. In a small (n = 86) randomized open-label noninferiority trial for the prevention of post-procedural septicemia and cholangitis, IV moxifloxacin was not found to be inferior to IV ceftriaxone for prophylactic treatment of post-ERCP cholangitis and associated morbidity [86]. Other suggested methods to reduce post-ERCP cholangitis include the use of CO2 cholangiography, contrast-free method, MRCP and/or CT-guided drainage and air cholangiography. Of note, in patients with a need of endoscopic bilateral stent-in-stent (SIS) placement of self-expandable metallic stents (SEMS) for unresectable malignant hilar biliary obstruction, use of air assisted cholangiography (compared to contrast-assisted cholangiography) was significantly associated with reduced rates of post-ERCP cholangitis (4.8% in the air group vs. 29.2% in the contrast group, p = 0.048) [87].
In patients presenting with an obstructed bile duct, other therapeutic techniques (endoscopic sphincterotomy, stone extraction, stent insertion, and balloon dilatation) can be used to reestablish free biliary drainage, but these procedures are not entirely risk-free as compared to diagnostic ERCP. As mentioned, one major cause of cholangitis includes incomplete biliary drainage, which can also occur in the setting of choledocholithiasis and incomplete stone clearance. EPLBD may also be performed to avoid retained stone fragments and reduce the risk of cholangitis in case of larger stones. An RCT (N = 90) showed that both EST with EPLBD or EST with mechanical lithotripsy are similarly effective in removal of large (> 12 mm) stones, but the rate of cholangitis was higher in the lithotripsy group (13.3%) compared with the EPLBD group (0.00%) (p = 0.026) [88]. In a meta-analysis of 4 RCTs, SEMSs were found to have lesser stent occlusion at four months with significantly reduced risk of recurrent biliary obstruction as compared to plastic stents [89]. However, both SEMSs and plastic stents are useful, and given the inherent adverse effects of stenting, placing multiple plastic stents may help prevent early stent occlusion and subsequent cholangitis [90].
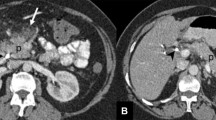
Cholecystitis
Post-ERCP cholecystitis (PEC) is not nearly as common as PEP but has been reported with an incidence of 0.5% [13]. Though not common, early recognition of PEC is vital as it can lead to significant morbidity such as purulent cholecystitis requiring emergent cholecystectomy. The pathogenesis is unclear but may involve contamination of the gallbladder by nonsterile contrast [91]. The risk factors for PEC occurrence within 2 weeks of ERCP were evaluated in a retrospective study comprising of 2672 patients which included a history of acute pancreatitis, history of chronic cholecystitis, gallbladder opacification, biliary duct metallic stent placement, and high leukocyte counts before ERCP. Additional risk factors include the presence of stones in the gallbladder, and having contrast fill the gallbladder during the procedure [91]. An important finding of this study was that metallic stenting of the biliary duct, but not plastic stenting during ERCP significantly increased duodenal biliary reflux and risk of PEC. The mechanism may include cystic duct obstruction secondary to stenting (OR = 3.66; 95% CI 1.78–7.54; p < 0.001). Lastly, unlike PEP, the study showed that the risk of PEC increased with age, so elderly patients should be thoroughly evaluated before the procedure [91].
Prevention of PEC
When patients with these risk factors undergo ERCP, prophylactic measures should be taken to prevent PEC. The most crucial measure is endoscopic gallbladder drainage, which has proven to be effective and safe. Therefore, in high-risk patients, temporary gallbladder decompression with a plastic stent or endoscopically placed nasocholecystic tube should be considered. Use of prophylactic antibiotics to prevent cholecystitis is an avenue that has not yet been explored. However, treatment of PEC typically involves surgery or percutaneous cholecystostomy, and in nonsurgical candidates, transpapillary and EUS-guided gallbladder drainage may additionally be considered as treatment options [92, 93].
Duodenoscope-Related Transmission of Infection
The duodenoscope is very useful in treating pancreatobiliary conditions, but it is a sophisticated instrument that is amenable to infection. These particular devices have a unique elevator mechanism that helps orient accessories (guidewires, catheters, etc.) into the endoscopic field of view [94]. However, the intricate design of the elevator mechanism makes it difficult to adequately clean, which lends itself to bacterial contamination. Currently, the most common organism responsible for duodenoscope-related infection is Pseudomonas aeruginosa [95]. However, other organisms involved in exogenous contamination include Mycobacteria, Salmonella, Helicobacter pylori, Clostridia difficile, and more recently, multidrug-resistant organisms (carbapenem-resistant Enterobacteriaceae) [95,96,97,98]. To a lesser degree, viral causes implicated may include hepatitis B and C viruses [95, 99]. Some of the common patient-related risk factors for infection include bile or pancreatic duct obstruction, tissue damage, and compromised/deficient immune status. Procedure- or device-related factors include inadequate disinfection, complex duodenoscope design, damaged components, and contaminated automated endoscope reprocessor (AER) [95].
Prevention of Duodenoscope-Related Transmission of Infection
Several strategies exist to reduce the occurrence of duodenoscope-associated infections. One of the essential strategies includes regular servicing of duodenoscopes to reduce transmission of pathogens. Additionally, strict adherence to the CDC, FDA, and manufacturer disinfection guidelines can help prevent duodenoscope infection [95]. The AER is a newer automatic cleaning technique that was thought to improve duodenoscope cleaning by eliminating human error in cleaning and improving particle removal. However, even this method is also not without risks of contamination. Currently, the FDA recommends the use of AER only after manual cleaning. Other possible strategies involve periodic assessment of cleaning staff to ensure competency and implementing quality control measures (i.e., monthly microbiologic surveillance). Further development of newer, less complex duodenoscope designs is needed to improve ease of cleaning for long-term use, in addition to better sterilization methods [9, 95]. New FDA recommendation may obviate the need for duodenoscope reprocessing and reuse completely. Given the complex design and difficulty associated with cleaning and reprocessing duodenoscopes to be reused, the FDA is now recommending use of either duodenoscopes with disposable components (e.g., endcaps) or completely disposable duodenoscopes to eliminate the possibility of instrument contamination and reduce the risk of infection in patients [100].
Other less reported infectious events following ERCP include disseminated Candida albicans, of which one rare case was reported in an immunocompetent and noncritically ill patient [101]. Additionally, endoscopy-related bacteremia may rarely lead to remote bacterial seeding and infective endocarditis. As such, guidelines do not recommend the use of antibiotics to prevent endocarditis for patients who undergo a gastrointestinal tract procedure [9].
Intestinal Perforation
ERCP carries an approximate 1% risk of perforation, with an 8–23% mortality [102, 103]. The most common clinical finding is severe abdominal pain along with leukocytosis, fever, tachycardia, and occasionally back pain [9]. The Stapfer classification is a scheme used to describe four types of perforations. Type I perforations, produced by the metal guide, are located on the medial or lateral duodenal wall and may result in intraperitoneal perforation. These perforations commonly cause contrast leaks in the retroperitoneum. Type II perforations include periampullary perforations derived from a biliary or pancreatic sphincterotomy or precut papillotomy. Type III perforations occur far from the ductal papilla perforation and are related to the instrumentation, like guidewires or stents. Type IV perforations are associated with retropneumoperitoneum post-ERCP and may not represent true perforations [9, 102, 103].
The most common type of duodenal perforation is type II occurring in 46% of cases. Type I and III perforations occur, albeit to a lesser degree, in 25 and 22% of cases, respectively [104]. Patient-related risk factors for perforation include suspected SOD, older patient age, female sex, and surgical or altered anatomy, such as situs inversus or Billroth II gastrectomy [19, 105,106,107,108,109,110,111]. Procedure-related factors include difficult cannulation, biliary stricture dilation, intramural injection of contrast material, prolonged procedure, sphincterotomy, and precut papillotomy EPLBD and ERCP by lesser experienced endoscopists [14, 19, 105,106,107,108,109,110,111].
Management of Intestinal Perforations
Perforations require rapid diagnosis and treatment to avoid severe complications like sepsis and multiple organ failure. However, management of ERCP-related perforations is controversial as the management has slowly shifted to conservative management and challenging identification of patient requiring surgery. Initial management of suspected perforation includes nil per os, IV fluids, and broad-spectrum antibiotics [105, 106]. Indications for surgery are based on the type, size, and location of the perforation. Surgery may be indicated in type I perforations, cases with a significant contrast leak, retroperitoneal collections, persistent biliary obstruction, unsuccessful conservative treatment, and peritoneal signs of sepsis [102, 105]. A retrospective study of all post-ERCP perforations over 15 years found that type I perforations require immediate surgery, type II and III perforations can be managed conservatively assuming no significant complications (abdominal collections, peritoneal irritation and/or sepsis), and type IV perforations respond to conservative treatment [102].
Traditionally, the standard medical treatment approach with an oral contrast study to confirm no further leakage are done as a part of conservative management [9, 112]. In efforts to expand conservative treatment, some studies have suggested that endoscopically placed fully covered self-expandable metal stents (FC-SEMS) could potentially be effective in types II and III perforations [104, 113]. In a 2018 retrospective analysis of patients with type II perforation, treatment with the placement of FC-SEMS was shown to be adequate and effective, and none of the patients required surgery or experienced death. This may indicate that FC-SEMS placement is safe and effective in treating type II perforations and represent an added layer to conservative treatment [113]. Additionally, Odemis et al. [114] found that in addition to using as conservative treatment, FC-SEMS helps reduce pain, lower WBC, and decrease the length of hospital stay. In addition to antibiotics and nasogastric/nasoduodenal aspiration, European Society of Gastrointestinal Endoscopy (ESGE) guidelines recommend stent placement only as a means of rescue treatment in certain cases [112]. This recommendation was drawn based upon two previous cases in which stenting was shown to be effective as a rescue treatment [83, 115]. As such, it may not reflect the potential of the FC-SEMS as a first-line treatment for type II and III perforations. However, ASGE highlighted the use of FC-SEMS as a direct treatment in cases of noted intraoperative periampullary perforations to seal the defect [9, 116, 117]. Other less explored endoscopic therapeutic options with reported success include through-the-scope clips [118], endoscopic purse-string suture [119], over-the-scope clip [120], fibrin glue [121], band ligation [122], and endoscopic vacuum therapy [123].
Other Miscellaneous Complications
Indirect complications may also occur as a result of ERCP. Several cardiopulmonary adverse events such as hypoxia, hypotension, cardiac dysrhythmia, and aspiration have been reported and accounted for 4–16% of ERCP-related adverse events [124, 125]. Air embolism is another adverse event that may occur [126, 127]. Other rare complications include ileus, pneumothorax and/or pneumoperitoneum, hepatic subcapsular hematoma, hepatic abscess formation, pseudocyst infection, splenic injury, and biliary or pancreatic duct fistulae [125, 128, 129]. Lastly, adverse reaction to contrast material has been described with ERCP [130, 131].
Limitations
Some of the data reported in the epidemiological profile of various post-ERCP complications were established in retrospective studies. Larger, prospective multicenter studies are needed to further clarify the accurate epidemiological description of post-ERCP complications and general effectiveness and safety of ERCP. Additionally, further attempts could be made to reach a consensus regarding the clinical definition and criteria for post-ERCP complications to promote consistency in reporting complications. Lastly, further studies are needed to confirm risk factors for less common post-ERCP complications (cholecystitis, cholangitis, and perforation), as well as the optimal timing (pre-ERCP, post-ERCP) of rectal Diclofenac administration to prevent PEP.
Conclusion
In conclusion, ERCP remains the standard treatment modality for several disorders of the pancreaticobiliary system. Post-ERCP complications, although mostly mild, remain an important source of concern. Identification of risk factors can help clinicians appropriately selecting patients for ERCP intervention and anticipate potential adverse events. Strategies to reduce and manage ERCP-related complications do exist, but large-scale studies are needed to determine the true extent of each risk factor and preventative measure. Review of current knowledge of ERCP complications, risk factors, prevention strategies, and management algorithms may help improve the clinical utility of ERCP and can reduce the ERCP-related adverse events.
References
Talukdar R. Complications of ERCP. Best Pract Res Clin Gastroenterol. 2016;30:793–805. https://doi.org/10.1016/j.bpg.2016.10.007.
Galeazzi M, Mazzola P, Valcarcel B, et al. Endoscopic retrograde cholangiopancreatography in the elderly: results of a retrospective study and a geriatricians’ point of view. BMC Gastroenterol. 2018;18:38. https://doi.org/10.1186/s12876-018-0764-4.
Ukkonen M, Siiki A, Antila A, Tyrvainen T, Sand J, Laukkarinen J. Safety and efficacy of acute endoscopic retrograde cholangiopancreatography in the elderly. Dig Dis Sci. 2016;61:3302–3308. https://doi.org/10.1007/s10620-016-4283-2.
Siiki A, Tamminen A, Tomminen T, Kuusanmaki P. ERCP procedures in a Finnish community hospital: a retrospective analysis of 1207 cases. SJS Off Organ Finn Surg Soc Scand Surg Soc. 2012;101:45–50. https://doi.org/10.1177/145749691210100109.
Kapral C, Muhlberger A, Wewalka F, Duller C, Knoflach P, Schreiber F. Quality assessment of endoscopic retrograde cholangiopancreatography: results of a running nationwide Austrian benchmarking project after 5 years of implementation. Eur J Gastroenterol Hepatol. 2012;24:1447–1454. https://doi.org/10.1097/meg.0b013e3283583c6f.
Glomsaker T, Hoff G, Kvaloy JT, Soreide K, Aabakken L, Soreide JA. Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg. 2013;100:373–380. https://doi.org/10.1002/bjs.8992.
Rustagi T, Jamidar PA. Endoscopic retrograde cholangiopancreatography-related adverse events: general overview. Gastrointest Endosc Clin N Am. 2015;25:97–106. https://doi.org/10.1016/j.giec.2014.09.005.
Jamry A. Risk factors of pancreatitis after endoscopic sphincterotomy. Review of literature and practical remarks based on approximately 10,000 ERCPs. Polski Przeglad Chirurgiczny. 2017;89:29–33. https://doi.org/10.5604/01.3001.0010.5409.
Chandrasekhara V, Khashab MA, Muthusamy VR, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32–47. https://doi.org/10.1016/j.gie.2016.06.051.
Elmunzer BJ. Reducing the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis. Dig Endosc Off J Jpn Gastroenterol Endosc Soc. 2017;29:749–757. https://doi.org/10.1111/den.12908.
Kochar B, Akshintala VS, Afghani E, et al. Incidence, severity, and mortality of post-ERCP pancreatitis: a systematic review by using randomized, controlled trials. Gastrointest Endosc. 2015;81:143–149. https://doi.org/10.1016/j.gie.2014.06.045.
Keswani RN, Taft TH, Cote GA, Keefer L. Increased levels of stress and burnout are related to decreased physician experience and to interventional gastroenterology career choice: findings from a US survey of endoscopists. Am J Gastroenterol. 2011;106:1734–1740. https://doi.org/10.1038/ajg.2011.148.
Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909–918. https://doi.org/10.1056/nejm199609263351301.
Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1–10.
Rabenstein T, Schneider HT, Bulling D, et al. Analysis of the risk factors associated with endoscopic sphincterotomy techniques: preliminary results of a prospective study, with emphasis on the reduced risk of acute pancreatitis with low-dose anticoagulation treatment. Endoscopy. 2000;32:10–19. https://doi.org/10.1055/s-2000-138.
Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417–423. https://doi.org/10.1111/j.1572-0241.2001.03594.x.
Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425–434.
Vandervoort J, Soetikno RM, Tham TC, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652–656. https://doi.org/10.1067/mge.2002.129086.
Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721–731.
Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139–147. https://doi.org/10.1111/j.1572-0241.2006.00380.x.
Cheon YK, Cho KB, Watkins JL, et al. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc. 2007;65:385–393. https://doi.org/10.1016/j.gie.2006.10.021.
Williams EJ, Taylor S, Fairclough P, et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39:793–801. https://doi.org/10.1055/s-2007-966723.
Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31–40. https://doi.org/10.1038/ajg.2008.5.
Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc. 2009;70:80–88. https://doi.org/10.1016/j.gie.2008.10.039.
Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781–1788. https://doi.org/10.1111/j.1572-0241.2007.01279.x.
Enochsson L, Swahn F, Arnelo U, Nilsson M, Lohr M, Persson G. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc. 2010;72:1175–1184. https://doi.org/10.1016/j.gie.2010.07.047.
Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393.
Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. https://doi.org/10.1136/gutjnl-2012-302779.
Zouhairi ME, Swartz D, Shah T. Post-ERCP pancreatitis: mechanisms, risk factors, and prevention. Pancreat Disord Ther. 2013;. https://doi.org/10.4172/2165-7092.1000116.
Pezzilli R, Romboli E, Campana D, Corinaldesi R. Mechanisms involved in the onset of post-ERCP pancreatitis. J Pancreas. 2002;3:162–168.
Zitinic I, Plavsic I, Poropat G, Hauser G. ERCP induced and non-ERCP-induced acute pancreatitis: two distinct clinical entities? Med Hypotheses. 2018;113:42–44. https://doi.org/10.1016/j.mehy.2018.02.017.
Yaghoobi M, Pauls Q, Durkalski V, et al. Incidence and predictors of post-ERCP pancreatitis in patients with suspected sphincter of Oddi dysfunction undergoing biliary or dual sphincterotomy: results from the EPISOD prospective multicenter randomized sham-controlled study. Endoscopy. 2015;47:884–890. https://doi.org/10.1055/s-0034-1392418.
Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy. 2003;35:830–834. https://doi.org/10.1055/s-2003-42614.
Ding X, Zhang F, Wang Y. Risk factors for post-ERCP pancreatitis: a systematic review and meta-analysis. Surgeon J R Coll Surgeon Edinb Irel. 2015;13:218–229. https://doi.org/10.1016/j.surge.2014.11.005.
Miyatani H, Matsumoto S, Mashima H. Risk factors of post-endoscopic retrograde cholangiopancreatography pancreatitis in biliary type sphincter of Oddi dysfunction in Japanese patients. J Dig Dis. 2017;18:591–597. https://doi.org/10.1111/1751-2980.12541.
Phillip V, Schwab M, Haf D, Algul H. Identification of risk factors for post-endoscopic retrograde cholangiopancreatography pancreatitis in a high volume center. PLoS ONE. 2017;12:e0177874. https://doi.org/10.1371/journal.pone.0177874.
Lin Y, Liu X, Cao DQ, et al. Analysis of risk factors and prevention strategies of post-ERCP pancreatitis. Eur Rev Med Pharmacol Sci. 2017;21:5185–5190. https://doi.org/10.26355/eurrev_201711_13838.
Karaahmet F, Kekilli M. The presence of periampullary diverticulum increased the complications of endoscopic retrograde cholangiopancreatography. Eur J Gastroenterol Hepatol. 2018;30:1009–1012. https://doi.org/10.1097/meg.0000000000001172.
Mehta SN, Pavone E, Barkun JS, Bouchard S, Barkun AN. Predictors of post-ERCP complications in patients with suspected choledocholithiasis. Endoscopy. 1998;30:457–463. https://doi.org/10.1055/s-2007-1001308.
Martinez J, Johnson CD, Sanchez-Paya J, de Madaria E, Robles-Diaz G, Perez-Mateo M. Obesity is a definitive risk factor of severity and mortality in acute pancreatitis: an updated meta-analysis. Off J Int Assoc Pancreatol. 2006;6:206–209. https://doi.org/10.1159/000092104.
Inamdar S, Berzin TM, Sejpal DV, et al. Pregnancy is a risk factor for pancreatitis after endoscopic retrograde cholangiopancreatography in a national cohort study. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2016;14:107–114. https://doi.org/10.1016/j.cgh.2015.04.175.
Park CH, Jung JH, Hyun B, et al. Safety and efficacy of early feeding based on clinical assessment at 4 hours after ERCP: a prospective randomized controlled trial. Gastrointest Endosc. 2018;87:1040–1049. https://doi.org/10.1016/j.gie.2017.09.021.
Chen JJ, Wang XM, Liu XQ, et al. Risk factors for post-ERCP pancreatitis: a systematic review of clinical trials with a large sample size in the past 10 years. Eur J Med Res. 2014;19:26. https://doi.org/10.1186/2047-783x-19-26.
Maple JT, Keswani RN, Hovis RM, et al. Carbon dioxide insufflation during ERCP for reduction of postprocedure pain: a randomized, double-blind, controlled trial. Gastrointest Endosc. 2009;70:278–283. https://doi.org/10.1016/j.gie.2008.12.050.
Iida T, Kaneto H, Wagatsuma K, et al. Can trainees safely perform endoscopic treatments for common bile duct stones? A single-center retrospective study. Intern Med (Tokyo, Jpn). 2018;57:923–928. https://doi.org/10.2169/internalmedicine.9737-17.
Testoni PA, Mariani A, Giussani A, et al. Risk factors for post-ERCP pancreatitis in high- and low-volume centers and among expert and non-expert operators: a prospective multicenter study. Am J Gastroenterol. 2010;105:1753–1761. https://doi.org/10.1038/ajg.2010.136.
Choudhary A, Bechtold ML, Arif M, et al. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc. 2011;73:275–282. https://doi.org/10.1016/j.gie.2010.10.039.
Mazaki T, Mado K, Masuda H, Shiono M. Prophylactic pancreatic stent placement and post-ERCP pancreatitis: an updated meta-analysis. J Gastroenterol. 2014;49:343–355. https://doi.org/10.1007/s00535-013-0806-1.
Sugimoto M, Takagi T, Suzuki R, et al. Pancreatic stents for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis should be inserted up to the pancreatic body or tail. World J Gastroenterol. 2018;24:2392–2399. https://doi.org/10.3748/wjg.v24.i22.2392.
Cha SW, Leung WD, Lehman GA, et al. Does leaving a main pancreatic duct stent in place reduce the incidence of precut biliary sphincterotomy-associated pancreatitis? A randomized, prospective study. Gastrointest Endosc. 2013;77:209–216. https://doi.org/10.1016/j.gie.2012.08.022.
Tse F, Yuan Y, Moayyedi P, Leontiadis GI. Guidewire-assisted cannulation of the common bile duct for the prevention of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. Cochrane Database Syst Rev. 2012;12:Cd009662. https://doi.org/10.1002/14651858.cd009662.pub2.
Furuya CK, Sakai P, Marinho FRT, et al. Papillary fistulotomy vs conventional cannulation for endoscopic biliary access: a prospective randomized trial. World J Gastroenterol. 2018;24:1803–1811. https://doi.org/10.3748/wjg.v24.i16.1803.
Pecsi D, Farkas N, Hegyi P, et al. Transpancreatic sphincterotomy has a higher cannulation success rate than needle-knife precut papillotomy—a meta-analysis. Endoscopy. 2017;49:874–887. https://doi.org/10.1055/s-0043-111717.
Fang J, Wang SL, Zhao SB, et al. Impact of intraduodenal acetic acid infusion on pancreatic duct cannulation during endoscopic retrograde cholangiopancreatography: a double-blind, randomized controlled trial. J Gastroenterol Hepatol. 2018;33:1804–1810. https://doi.org/10.1111/jgh.14148.
Mbatshi G, Macken EJ, De Schepper HU, Piessevaux H, Deprez PH, Moreels TG. Comparison of side-viewing duodenoscope and single-balloon enteroscope to perform ERCP in patients with Billroth II gastrectomy. Acta Gastro-enterol Belg. 2017;80:493–497.
Elmunzer BJ, Scheiman JM, Lehman GA, et al. A randomized trial of rectal indomethacin to prevent post-ERCP pancreatitis. N Engl J Med. 2012;366:1414–1422. https://doi.org/10.1056/nejmoa1111103.
Mohammad Alizadeh AH, Abbasinazari M, Hatami B, et al. Comparison of rectal indomethacin, diclofenac, and naproxen for the prevention of post endoscopic retrograde cholangiopancreatography pancreatitis. Eur J Gastroenterol Hepatol. 2017;29:349–354. https://doi.org/10.1097/meg.0000000000000787.
Sethi S, Sethi N, Wadhwa V, Garud S, Brown A. A meta-analysis on the role of rectal diclofenac and indomethacin in the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Pancreas. 2014;43:190–197. https://doi.org/10.1097/mpa.0000000000000090.
Del Olmo Martinez L, Velayos Jimenez B, Almaraz Gomez A. Rectal diclofenac does not prevent post-ERCP pancreatitis in consecutive high-risk and low-risk patients. Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patologia Digestiva. 2018;110:505–509. https://doi.org/10.17235/reed.2018.5259/2017.
Lyu Y, Cheng Y, Wang B, Xu Y, Du W. What is impact of nonsteroidal anti-inflammatory drugs in the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis: a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2018;18:106. https://doi.org/10.1186/s12876-018-0837-4.
Garg R, Mohan BP, Krishnamoorthi R, Rustagi T. Pre-endoscopic retrograde cholangiopancreatography (ERCP) administration of rectal indomethacin in unselected patients to reduce post-ERCP pancreatitis: a systematic review and meta-analysis. Indian J Gastroenterol Off J Indian Soc Gastroenterol. 2018;37:120–126. https://doi.org/10.1007/s12664-018-0841-1.
Yang C, Zhao Y, Li W, et al. Rectal nonsteroidal anti-inflammatory drugs administration is effective for the prevention of post-ERCP pancreatitis: an updated meta-analysis of randomized controlled trials. Pancreatol Off J Int Assoc Pancreatol. 2017;17:681–688. https://doi.org/10.1016/j.pan.2017.07.008.
Okuno M, Shiroko J, Taguchi D, et al. The effectiveness of the rectal administration of low-dose diclofenac for the prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis. Intern Med (Tokyo, Jpn). 2018;57:2289–2294. https://doi.org/10.2169/internalmedicine.0554-17.
Wang G, Xiao G, Xu L, et al. Effect of somatostatin on prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis and hyperamylasemia: a systematic review and meta-analysis. Pancreatol Off J Int Assoc Pancreatol. 2018;18:370–378. https://doi.org/10.1016/j.pan.2018.03.002.
Staritz M, Poralla T, Ewe K, Meyer Zum Buschenfelde KH. Effect of glyceryl trinitrate on the sphincter of Oddi motility and baseline pressure. Gut. 1985;26:194–197.
Kaufman HS, Shermak MA, May CA, Pitt HA, Lillemoe KD. Nitric oxide inhibits resting sphincter of Oddi activity. Am J Surg. 1993;165:74–80.
Luman W, Pryde A, Heading RC, Palmer KR. Topical glyceryl trinitrate relaxes the sphincter of Oddi. Gut. 1997;40:541–543.
Carr-Locke DL, Gregg JA, Aoki TT. Effects of exogenous glucagon on pancreatic and biliary ductal and sphincteric pressures in man demonstrated by endoscopic manometry and correlation with plasma glucagon. Dig Dis Sci. 1983;28:312–320. https://doi.org/10.1007/BF01324947.
Katsinelos P, Lazaraki G, Chatzimavroudis G, et al. Impact of nitroglycerin and glucagon administration on selective common bile duct cannulation and prevention of post-ERCP pancreatitis. Scand J Gastroenterol. 2017;52:50–55. https://doi.org/10.1080/00365521.2016.1228117.
Buxbaum J, Yan A, Yeh K, Lane C, Nguyen N, Laine L. Aggressive hydration with lactated Ringer’s solution reduces pancreatitis after endoscopic retrograde cholangiopancreatography. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2014;12:303–307. https://doi.org/10.1016/j.cgh.2013.07.026.
Wu D, Wan J, Xia L, Chen J, Zhu Y, Lu N. The efficiency of aggressive hydration with lactated ringer solution for the prevention of post-ERCP pancreatitis: a systematic review and meta-analysis. J Clin Gastroenterol. 2017;51:e68–e76. https://doi.org/10.1097/mcg.0000000000000856.
Gooshe M, Abdolghaffari AH, Nikfar S, Mahdaviani P, Abdollahi M. Antioxidant therapy in acute, chronic and post-endoscopic retrograde cholangiopancreatography pancreatitis: an updated systematic review and meta-analysis. World J Gastroenterol. 2015;21:9189–9208. https://doi.org/10.3748/wjg.v21.i30.9189.
Parekh PJ, Majithia R, Sikka SK, Baron TH. The “Scope” of post-ERCP pancreatitis. Mayo Clin Proc. 2017;92:434–448. https://doi.org/10.1016/j.mayocp.2016.10.028.
Szary NM, Al-Kawas FH. Complications of endoscopic retrograde cholangiopancreatography: how to avoid and manage them. Gastroenterol Hepatol. 2013;9:496–504.
Oh HC, El H II, Easler JJ, et al. Post-ERCP bleeding in the era of multiple antiplatelet agents. Gut Liver. 2018;12:214–218. https://doi.org/10.5009/gnl17204.
Wilcox CM, Canakis J, Monkemuller KE, Bondora AW, Geels W. Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol. 2004;99:244–248.
Hamada T, Yasunaga H, Nakai Y, et al. Bleeding after endoscopic sphincterotomy or papillary balloon dilation among users of antithrombotic agents. Endoscopy. 2015;47:997–1004. https://doi.org/10.1055/s-0034-1392408.
Hussain N, Alsulaiman R, Burtin P, et al. The safety of endoscopic sphincterotomy in patients receiving antiplatelet agents: a case-control study. Aliment Pharmacol Ther. 2007;25:579–584. https://doi.org/10.1111/j.1365-2036.2006.03225.x.
Park DH, Kim MH, Lee SK, et al. Endoscopic sphincterotomy vs endoscopic papillary balloon dilation for choledocholithiasis in patients with liver cirrhosis and coagulopathy. Gastrointest Endosc. 2004;60:180–185.
Morris ML, Tucker RD, Baron TH, Song LM. Electrosurgery in gastrointestinal endoscopy: principles to practice. Am J Gastroenterol. 2009;104:1563–1574. https://doi.org/10.1038/ajg.2009.105.
Leung WK, But DY, Wong SY, et al. Prevention of post-sphincterotomy bleeding by proton pump inhibitor: a randomized controlled trial. J Dig Dis. 2018;19:369–376. https://doi.org/10.1111/1751-2980.12604.
Ferreira LE, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007;102:2850–2858. https://doi.org/10.1111/j.1572-0241.2007.01563.x.
Canena J, Liberato M, Horta D, Romao C, Coutinho A. Short-term stenting using fully covered self-expandable metal stents for treatment of refractory biliary leaks, postsphincterotomy bleeding, and perforations. Surg Endosc. 2013;27:313–324. https://doi.org/10.1007/s00464-012-2368-3.
Millward SF. ACR appropriateness criteria on treatment of acute nonvariceal gastrointestinal tract bleeding. J Am College Radiol. 2008;5:550–554. https://doi.org/10.1016/j.jacr.2008.01.010.
Chen M, Wang L, Wang Y, et al. Risk factor analysis of post-ERCP cholangitis: a single-center experience. Hepatobiliary Pancreat Dis Int HBPD INT. 2018;17:55–58. https://doi.org/10.1016/j.hbpd.2018.01.002.
Kim NH, Kim HJ, Bang KB. Prospective comparison of prophylactic antibiotic use between intravenous moxifloxacin and ceftriaxone for high-risk patients with post-ERCP cholangitis. Hepatobiliary Pancreat Dis Int HBPD INT. 2017;16:512–518. https://doi.org/10.1016/s1499-3872(17)60056-0.
Lee JM, Lee SH, Jang DK, et al. Air cholangiography in endoscopic bilateral stent-in-stent placement of metallic stents for malignant hilar biliary obstruction. Ther Adv Gastroenterol. 2016;9:189–198. https://doi.org/10.1177/1756283x15618132.
Stefanidis G, Viazis N, Pleskow D, et al. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278–285. https://doi.org/10.1038/ajg.2010.421.
Pfau PR, Pleskow DK, Banerjee S, et al. Pancreatic and biliary stents. Gastrointest Endosc. 2013;77:319–327. https://doi.org/10.1016/j.gie.2012.09.026.
Costamagna G, Boskoski I. Current treatment of benign biliary strictures. Ann Gastroenterol. 2013;26:37–40.
Cao J, Peng C, Ding X, et al. Risk factors for post-ERCP cholecystitis: a single-center retrospective study. BMC Gastroenterol. 2018;18:128. https://doi.org/10.1186/s12876-018-0854-3.
Irani S, Baron TH, Grimm IS, Khashab MA. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video). Gastrointest Endosc. 2015;82:1110–1115. https://doi.org/10.1016/j.gie.2015.05.045.
Kedia P, Sharaiha RZ, Kumta NA, et al. Endoscopic gallbladder drainage compared with percutaneous drainage. Gastrointest Endosc. 2015;82:1031–1036. https://doi.org/10.1016/j.gie.2015.03.1912.
Rutala WA, Weber DJ. ERCP scopes: what can we do to prevent infections? Infect Control Hosp Epidemiol. 2015;36:643–648. https://doi.org/10.1017/ice.2015.98.
Rahman MR, Perisetti A, Coman R, Bansal P, Chhabra R, Goyal H. Duodenoscope-associated infections: update on an emerging problem. Dig Dis Sci. 2018;. https://doi.org/10.1007/s10620-018-5431-7.
Spach DH, Silverstein FE, Stamm WE. Transmission of infection by gastrointestinal endoscopy and bronchoscopy. Ann Intern Med. 1993;118:117–128.
Epstein L, Hunter JC, Arwady MA, et al. New Delhi metallo-beta-lactamase-producing carbapenem-resistant Escherichia coli associated with exposure to duodenoscopes. JAMA. 2014;312:1447–1455. https://doi.org/10.1001/jama.2014.12720.
Rutala WA, Weber DJ. Outbreaks of carbapenem-resistant Enterobacteriaceae infections associated with duodenoscopes: What can we do to prevent infections? Am J Infect Control.. 2016;44:e47–e51. https://doi.org/10.1016/j.ajic.2015.10.037.
Kovaleva J, Peters FT, van der Mei HC, Degener JE. Transmission of infection by flexible gastrointestinal endoscopy and bronchoscopy. Clin Microbiol Rev. 2013;26:231–254. https://doi.org/10.1128/cmr.00085-12.
Administration USFaD. FDA recommends health care facilities and manufacturers begin transitioning to duodenoscopes with disposable components to reduce risk of patient infection. 2019.
Park TY, Yang YJ, Shin SP, et al. Candidemia after endoscopic retrograde cholangiopancreatography in an immunocompetent patient: a case report and literature review. Saudi J Gastroenterol Off J Saudi Gastroenterol Assoc. 2018;24:135–137. https://doi.org/10.4103/sjg.sjg_536_17.
Jimenez Cubedo E, Lopez Monclus J, Lucena de la Poza JL, et al. Review of duodenal perforations after endoscopic retrograde cholangiopancreatography in Hospital Puerta de Hierro from 1999 to 2014. Revista espanola de enfermedades digestivas: organo oficial de la Sociedad Espanola de Patologia Digestiva. 2018;110:515–519. https://doi.org/10.17235/reed.2018.5255/2017.
Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002;34:293–298. https://doi.org/10.1055/s-2002-23650.
Tringali A, Cintolo M, Hassan C, Adler DG, Mutignani M. Type II-III ERCP-related perforations treated with temporary fully covered self-expandable stents. Dig Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2017;49:1169–1170. https://doi.org/10.1016/j.dld.2017.06.005.
Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191–198.
Howard TJ, Tan T, Lehman GA, et al. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999;126:658–663. (discussion 64-5).
Lai CH, Lau WY. Management of endoscopic retrograde cholangiopancreatography-related perforation. Surgeon J R Coll Surgeon Edinb Irel. 2008;6:45–48.
Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM. Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc. 2009;23:833–838. https://doi.org/10.1007/s00464-008-0157-9.
Morgan KA, Fontenot BB, Ruddy JM, Mickey S, Adams DB. Endoscopic retrograde cholangiopancreatography gut perforations: when to wait! When to operate! Am Surgeon. 2009;75:477–483. (discussion 83-4).
Fatima J, Baron TH, Topazian MD, et al. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management (Chicago, IL: 1960). Arch Surg. 2007;142:448–454. https://doi.org/10.1001/archsurg.142.5.448. (discussion 54-5).
Preetha M, Chung YF, Chan WH, et al. Surgical management of endoscopic retrograde cholangiopancreatography-related perforations. ANZ J Surg. 2003;73:1011–1014.
Paspatis GA, Dumonceau JM, Barthet M, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) position statement. Endoscopy. 2014;46:693–711. https://doi.org/10.1055/s-0034-1377531.
Tringali A, Pizzicannella M, Andrisani G, et al. Temporary FC-SEMS for type II ERCP-related perforations: a case series from two referral centers and review of the literature < sup/>. Scand J Gastroenterol. 2018;53:760–767. https://doi.org/10.1080/00365521.2018.1458894.
Odemis B, Oztas E, Kuzu UB, et al. Can a fully covered self-expandable metallic stent be used temporarily for the management of duodenal retroperitoneal perforation during ERCP as a part of conservative therapy? Surg Laparosc Endosc Percutaneous Tech. 2016;26:e9–e17. https://doi.org/10.1097/sle.0000000000000240.
Jeon HJ, Han JH, Park S, Youn S, Chae H, Yoon S. Endoscopic sphincterotomy-related perforation in the common bile duct successfully treated by placement of a covered metal stent. Endoscopy. 2011;43:E295–E296. https://doi.org/10.1055/s-0030-1256464.
Vezakis A, Fragulidis G, Nastos C, Yiallourou A, Polydorou A, Voros D. Closure of a persistent sphincterotomy-related duodenal perforation by placement of a covered self-expandable metallic biliary stent. World J Gastroenterol. 2011;17:4539–4541. https://doi.org/10.3748/wjg.v17.i40.4539.
Park WY, Cho KB, Kim ES, Park KS. A case of ampullary perforation treated with a temporally covered metal stent. Clin Endosc. 2012;45:177–180. https://doi.org/10.5946/ce.2012.45.2.177.
Amodio PM, Faggiani R, Pastorelli A, et al. Selected treatments for duodenal perforation after ERCP. A report of three cases. Chir Ital. 2007;59:343–346.
Li Q, Ji J, Wang F, et al. ERCP-induced duodenal perforation successfully treated with endoscopic purse-string suture: a case report. Oncotarget. 2015;6:17847–17850. https://doi.org/10.18632/oncotarget.4079.
Buffoli F, Grassia R, Iiritano E, Bianchi G, Dizioli P, Staiano T. Endoscopic, “retroperitoneal fatpexy” of a large ERCP-related jejunal perforation by using a new over-the-scope clip device in Billroth II anatomy (with video). Gastrointest Endosc. 2012;75:1115–1117. https://doi.org/10.1016/j.gie.2011.05.029.
Mutignani M, Iacopini F, Dokas S, et al. Successful endoscopic closure of a lateral duodenal perforation at ERCP with fibrin glue. Gastrointest Endosc.. 2006;63:725–727. https://doi.org/10.1016/j.gie.2005.11.028.
Li Y, Han Z, Zhang W, et al. Successful closure of lateral duodenal perforation by endoscopic band ligation after endoscopic clipping failure. Am J Gastroenterol. 2014;109:293–295. https://doi.org/10.1038/ajg.2013.415.
Loske G, Rucktaschel F, Schorsch T, van Ackeren V, Stark B, Muller CT. Successful endoscopic vacuum therapy with new open-pore film drainage in a case of iatrogenic duodenal perforation during ERCP. Endoscopy. 2015;47:E577–E578. https://doi.org/10.1055/s-0034-1393388.
Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010;71:446–454. https://doi.org/10.1016/j.gie.2009.10.027.
Ji Young Bang GAC. Rare and underappreciated complications of endoscopic retrograde cholangiopancreatography. Tech Gastrointest Endosc. 2014;16:195–201. https://doi.org/10.1016/j.tgie.2014.07.007.
Efthymiou M, Raftopoulos S, Antonio Chirinos J, May GR. Air embolism complicated by left hemiparesis after direct cholangioscopy with an intraductal balloon anchoring system. Gastrointest Endosc. 2012;75:221–223. https://doi.org/10.1016/j.gie.2011.01.038.
Farnik H, Weigt J, Malfertheiner P, et al. A multicenter study on the role of direct retrograde cholangioscopy in patients with inconclusive endoscopic retrograde cholangiography. Endoscopy. 2014;46:16–21. https://doi.org/10.1055/s-0033-1359043.
Chavalitdhamrong D, Donepudi S, Pu L, Draganov PV. Uncommon and rarely reported adverse events of endoscopic retrograde cholangiopancreatography. Dig Endosc Off J Jpn Gastroenterol Endosc Soc. 2014;26:15–22. https://doi.org/10.1111/den.12178.
Chi KD, Waxman I. Subcapsular hepatic hematoma after guide wire injury during endoscopic retrograde cholangiopancreatography: management and review. Endoscopy. 2004;36:1019–1021. https://doi.org/10.1055/s-2004-825861.
Draganov P, Cotton PB. Iodinated contrast sensitivity in ERCP. Am J Gastroenterol. 2000;95:1398–1401. https://doi.org/10.1111/j.1572-0241.2000.02069.x.
Pan JJ, Draganov PV. Adverse reactions to iodinated contrast media administered at the time of endoscopic retrograde cholangiopancreatography (ERCP). Inflamm Allergy Drug Targets. 2009;8:17–20.
Acknowledgments
None.
Funding
None to report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Johnson, K.D., Perisetti, A., Tharian, B. et al. Endoscopic Retrograde Cholangiopancreatography-Related Complications and Their Management Strategies: A “Scoping” Literature Review. Dig Dis Sci 65, 361–375 (2020). https://doi.org/10.1007/s10620-019-05970-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05970-3