Abstract
Background
Several animal and human studies have reported that sphincter of Oddi (SO) motility shows cyclical changes during the fasting state. However, to date, the relationship between the SO motility and the migrating motor complex (MMC) of the small bowel (SB) remains unclear in humans.
Aims
We observed SO motility over a long study period and evaluated its relationship with the MMC of the SB in humans using percutaneous long-term manometry.
Methods
Our study included patients with hepatolithiasis who required percutaneous transhepatic catheter placement and subsequently underwent choledochoscopy and stone removal. Long-term percutaneous transhepatic SO manometry was performed after complete stone removal. SO and SB motility were simultaneously recorded.
Results
SO motility showed cyclical phasic changes with periodic high-frequency contractions similar to the MMC contractions of the SB. All high-frequency contractions of the SO coincided with phase III contractions of the MMC of the SB. The proportions of phase III contractions of SO and SB were similar, but the proportions of phase I (P = 0.001) and phase II (P = 0.002) contractions were significantly different. The mean basal SO pressure was observed to significantly increase in phase III compared to phase I (P = 0.001) and phase II (P = 0.001) contractions.
Conclusions
SO motility in humans showed cyclical phasic changes closely coordinated with the MMC of the SB in a fasting state; however, the proportion of phases differed between the SO and the SB. The basal pressure significantly increased during physiological high-frequency phase III contractions of the SO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several animal studies have reported that sphincter of Oddi (SO) motility shows clearly distinguishable cyclical changes in a fasting state [1,2,3,4], and these cyclical changes in SO motility show a close relationship with the migrating motor complexes (MMCs) of the small bowel (SB). Few studies in humans have described cyclical changes in SO motility because long-term SO manometry is not usually performed [5,6,7,8]; such cyclical changes of the SO remain neglected as a part of the normal criteria of SO motility and diagnosis of SO dysfunction, although periodic high-frequency contractions of the SO have been observed in human SO manometry studies.
SO manometry can be performed via the endoscopic transpapillary route or percutaneously. Conventional endoscopic SO manometry does not indicate overall SO motility because recordings are obtained over a relatively short period and could be affected by a number of factors including air inflation and medications used during endoscopy. Percutaneous SO manometry can be performed via the transhepatic or T-tube tract, allowing long-term recordings without associated discomfort and/or risk of complications and may reflect a more accurate physiological baseline than endoscopic SO manometry. We used a specially designed percutaneous long-term SO manometry catheter (3- or 8-lumen) to simultaneously evaluate the SO and SB motility. Therefore, here we performed long-term percutaneous SO manometry simultaneously with obtaining SB tracings to accurately evaluate the cyclical changes/patterns of SO motility and their relationship with the MMC of the SB in humans.
Methods
Patients
Our study included patients diagnosed with hepatolithiasis who underwent percutaneous transhepatic choledochoscopy between January 2006 and December 2014. Exclusion criteria were: prior upper gastrointestinal surgeries, history of sphincterotomy, or presence of a periampullary diverticulum or papillary stenosis indicated by fluoroscopic evidence of a slow/reduced flow through the papilla. Manometric studies were performed without any premedication after an overnight fasting period approximately 4–7 days after complete removal of the hepatolithiasis. Patients underwent minimum 3-year follow-up for the assessment of the development of symptoms related to apparent SO dysfunction. This study was approved by the Ethical Committee of the Ajou University Hospital.
Percutaneous Transhepatic SO Manometry
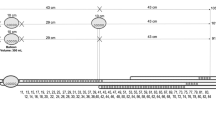
We used two types of specially designed percutaneous manometric catheters to simultaneously record SO and SB motility tracings. The first was a 3-lumen manometric catheter (Arndorfer Inc., Greendale, WI, USA) (Fig. 1a) that was 160 cm long with an outer diameter of 1.7 mm. The inner diameter of each lumen and the diameter of each luminal orifice was 0.5 mm. The two proximal orifices used to record the SO motility were set 2 mm apart, and the distal orifice used to record the SB motility was located 10 cm below the orifice above. The other catheter was an 8-lumen manometric catheter (Arndorfer Inc., Greendale, WI, USA) that was designed to record the propagation of duodenal motility to the proximal jejunum and simultaneously record SO motility (Fig. 1b). The 3-lumen manometry catheter has just only one side hole for duodenal motility. Therefore, we could not evaluate the propagation of MMC of SB using the 3-lumen manometry catheter. For that reason, we used a specially manufactured 8-lumen manometry catheter (increased the number of lumens for the small bowel) to further evaluate the propagation of MMC of the SB and the correlation between the SO and SB motility. It was 200 cm long with an outer diameter of 4.5 mm, and the inner diameter of each lumen and the diameter of each luminal orifice was 0.5 mm. The three proximal orifices used to record the SO motility tracing were set 2 mm apart, while the five distal orifices to record the SB motility tracing were 10 cm apart beginning from the third proximal orifice. The location of the side hole for SB motility was determined using a modification of the manometry catheter design used in the study of Kuo et al. [9], and the 10-cm spacing was used to compare and measure the SO motility and duodenal motility completely independent. Each lumen was infused with sterilized and distilled water at a rate of 0.25 mL/min using a low-compliance pneumohydraulic capillary infusion system (Arndorfer Inc., Greendale, WI, USA) (Fig. 2). Pressures were recorded using the PC polygraph HR (Synectic Medical Inc., Stockholm, Sweden) or Polygram Net (Medtronic, Skovlunde, Denmark).
a Schematic diagram showing percutaneous long-term sphincter of Oddi (SO) manometry using a 3-lumen catheter. The 3-lumen catheter was inserted into the mature percutaneous transhepatic tract and the common bile duct and advanced into the duodenum. b Fluoroscopic image showing percutaneous long-term SO manometry performed with an 8-lumen catheter. Using the 8-lumen catheter, the three proximal lumens recorded the SO motility (white arrow) and the five distal lumens (black arrows) recorded duodenal and jejunal small bowel motility
The manometry catheter was inserted via a percutaneous transhepatic biliary drainage tract and tightly anchored to the skin at the appropriate position under fluoroscopic and manometry monitoring guidance. During the manometry examination, one must remain next to the patient. SO and SB motility were simultaneously recorded over a duration > 1 MMC cycle of the SB in a fasting state only during the time period when high-frequency contractions of the SB were observed more than twice. SO motility was classified into phases I, II, and III based on the criteria used for classifying MMC of the SB [10]. The MMC phases were defined as follows: (1) phase I, a period of quiescence that always follows phase III and precedes phase II; (2) phase II, a period of irregular contractions that vary in amplitude and periodicity; and (3) phase III, a period of a distinct pattern of regular high-amplitude contractions that migrate to the distal segments of the bowel. The proportion of phases was defined as the percentages of phases I, II, and III in each cyclic phasic change of the SO and SB motility. Amplitudes of SO pressure were measured and expressed in mmHg using 0 duodenal pressure as a reference. SO phasic contractions were defined as SO waves measuring at least 16 mmHg in amplitude, while duodenal contractions were defined as duodenal waves measuring at least 6 mmHg in amplitude [6]. Basal SO pressure was defined as the mean value of the basal pressure obtained from the two proximal orifice recordings, which was only obtained using the 3-lumen SO manometry catheter. In this study, the basal pressure of the SO was measured using only the 3-lumen SO manometry catheter because the outer diameter of the 8-lumen manometry catheter (4.5 mm) was larger than the conventional 3-lumen SO manometry catheter. However, the 8-lumen catheter more accurately showed the propagation of duodenal contraction waves; therefore, it was easier to evaluate the relationship between the SO and SB contractions.
Statistical Analysis
The statistical analysis was performed using Student’s t test. Mean basal pressure was analyzed using the paired t test. Data were analyzed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA). The results are expressed as a mean ± standard deviation. Two-tailed P values < 0.05 were considered statistically significant.
Results
The baseline characteristics of each patient are noted in Table 1. We studied 31 patients (17 men and 14 women). The mean age of the patients was 55.6 (range 31–79) years. Percutaneous transhepatic manometry was performed using a 3-lumen catheter in 15 patients and the 8-lumen catheter in 16 patients. Patients were followed up for 4.8 ± 1.8 years, and no patient was observed to have developed any symptoms of apparent SO dysfunction.
Cyclic Changes in SO Motility
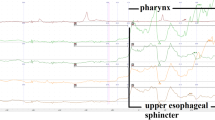
Cyclical phase changes in SO motility were noted in all patients who underwent percutaneous manometry with the 3-lumen (Fig. 3a) or 8-lumen (Fig. 3b) catheter. Cyclical SO motility was closely coordinated with the MMC of the SB other than the finding that the SO was not quiescent during phase I of the SB. Phase III (high-frequency contraction period) of the SO coincided with phase III of the MMC of the SB. The mean duration of one cycle of the SO and SB was 78.5 ± 43.5 min and 77.9 ± 40.1 min, respectively (P value of SO vs. SB = 0.75).
a Cyclical changes in the sphincter of Oddi motility observed using 3-channel percutaneous sphincter of Oddi manometry. b The cyclical changes in the sphincter of Oddi motility observed using 8-channel percutaneous sphincter of Oddi manometry. The SO showing cyclical phasic changes observed with use of 3- and 8-channel percutaneous manometry as noted in the small bowel
Phase I of the SO and SB Motility
In all 31 studied patients, phase I of the SO (9.3 ± 6 min) was significantly shorter than that of the SB (20.8 ± 18 min; P = 0.001) because the SO showed irregular contractions during phase I of the MMC of the SB even though the SB motility showed a period of quiescence. The proportion of phase I of one complete MMC cycle in the SO (14.3 ± 11.0%) was significantly smaller than that of the MMC of the SB (28.8 ± 19.0%; P = 0.001) (Table 2).
Phase II of the SO and SB Motility
In all 31 studied patients, phase II of the SO (61.2 ± 39 min) was significantly longer than that observed in the SB (50.9 ± 35 min; P = 0.008). The proportion of phase II in the SO (74.6 ± 15.0%) was significantly larger than that observed in the SB (62.3 ± 20.0%; P = 0.002). The mean frequency of phasic contractions of the SO in phase II was 4.5 ± 2/min (Table 3).
Phase III of the SO and SB Motility
In all 31 studied patients, regular high-frequency contractions that coincided with phase III of the MMC of the SB were noted. There was no significant difference in the proportion of phase III between SO (8.7 ± 5.0%) and SB (8.1 ± 4.0%; P = 0.340). The frequency of phasic contractions in phase III was 10.0 ± 1.0/min in SO and 10.1 ± 1.0/min in the SB (P = 0.820) (Table 4).
Basal Pressure of the SO
The basal pressure of the SO obtained in only the 15 patients who were examined using 3-lumen catheters was 18.5 ± 4 mmHg, 18.8 ± 4 mmHg, and 29.6 ± 8 mmHg in phases I, II, and III, respectively. The basal pressure significantly increased in phase III compared to phase I (P = 0.001) and phase II (P = 0.001). In two patients, the mean basal pressure of the SO in phase III (43 mmHg and 42 mmHg, respectively) increased above the defined normal range (< 40 mmHg) (Fig. 4).
a Incremental increase in basal pressure observed during phase III contractions of the sphincter of Oddi using 3-channel percutaneous sphincter of Oddi manometry. b The incremental increase in basal pressure during phase III contractions of the sphincter of Oddi using 8-channel percutaneous sphincter of Oddi manometry (black arrow, incremental increase in the basal pressure during phase III contractions of the sphincter of Oddi)
Discussion
Few studies performed in humans have reported on cyclical changes in SO motility [5,6,7,8]. Torsoli et al. [6] identified that the frequency of SO phasic contractions traced/recorded by performing long-lasting transductal manometry varied cyclically in close relation to the duodenal MMC in humans; however, a varying number of autonomous SO contractions were observed during duodenal phases I and II although rapid phasic contractions of the SO and duodenal phase III were similar. Worthley et al. [7] evaluated the SO motility in post-cholecystectomy patients with indwelling T-tubes during the fasting state and noted a close relationship between the phasic contraction patterns of the SO and the duodenum during the interdigestive cycle. In their study, however, the SO motility in humans was only classified into two phases: a prolonged phase in the SO corresponding to duodenal phases I and II, and the short phase in the SO that just preceded the onset of duodenal phase III.
We simultaneously recorded SO and SB motility using specially designed manometry catheters and classified SO motility into phases I, II, and III based on the criteria used for the MMC of the SB. We could then evaluate and compare the characteristics of each phase of the SO and SB. In this study, we observed that the SO motility in all patients showed definite cyclical changes closely coordinated with the MMC of the SB, as the duration of one cycle of MMC and the proportions of phase III in the SO and SB were almost identical and all high-frequency contractions of the SO coincided with phase III contractions of the MMC of the SB. However, the proportions of phases I and II were significantly different between SO and SB motility. The SB was observed to be quiescent despite contractile activity of the SO (phase II) being observed that resulted in a lack of sequential motility progression between the SO and the SB. This evidence indirectly supports the theory that SO contractility in humans is closely correlated with SB contractility and that the SO may possesses innate contractility.
High-frequency phasic contractions of the SO are referred to as “tachyrhythmia” or “tachyoddia” and have been considered motility abnormalities [11, 12]. Based on the Rome II and III criteria for functional SO disorders, high-frequency phasic contractions (> 7/min) are defined as abnormal [13, 14]. However, Torsoli et al. [6] reported that the phases demonstrating maximal frequency of phasic activity (9–12/min) were followed by a phase of 0 frequency using endoscopic or transductal manometry in patients with suspected SO dysfunction. Akita et al. [5] observed high-frequency contractions (9.49 ± 0.35/min) in 12 of 23 patients with biliary disease during percutaneous transhepatic SO manometry. In five of these patients, high-frequency contractions were observed twice at intervals of 85.4 ± 13.3 min. In our study, we observed high-frequency contractions (10.0 ± 1.0/min) of the SO that coincided with phase III of the SB in all patients without any apparent SO dysfunction over a long-term follow-up period. Isolated high-frequency contractions of the SO synchronous with phase III of the MMC of the SB were not noted. Therefore, we reckon that the synchronous occurrence of high-frequency contractions of the SO coinciding with phase III of duodenal contractions noted during endoscopic SO manometry should be considered physiological and not an abnormality. From the Rome IV criteria, the frequency and amplitude of phasic wave contractions were excluded from the diagnostic criteria, which matches our study result [15].
Here we observed the basal pressure based on the cyclical changes in SO motility. The basal pressure of the SO was observed to significantly increase in phase III compared to phases I and II. In two of our patients, it rose above the defined normal range (> 40 mmHg) despite their being asymptomatic with regard to apparent SO dysfunction. Therefore, an increase in basal pressure during high-frequency contractions of the SO, which is synchronous with duodenal MMC phase III, should perhaps be considered physiological rather than indicating SO dysfunction. An increment of basal pressure during high-frequency contractions of the SO that is asynchronous with duodenal MMC phase III could mean SOD; however, this should be carefully interpreted. If this finding is noted during an endoscopic SO manometry procedure, we suggest discontinuing the evaluation of the basal pressure during these high-frequency contractions of the SO and restarting the evaluation once they have ceased.
Limitations of this study include the fact that we studied only patients who were diagnosed with hepatolithiasis and considered to show normal SO function. Although percutaneous SO manometric studies performed in healthy controls would be of interest, this is unlikely to be achieved. Data with regard to SO manometric studies in patients with biliary stones are limited. One SO manometric study was conducted in Caucasians with extrahepatic biliary stones and resulted in normal SO manometric parameters [16]. SO motility is usually evaluated using 3-lumen manometry catheters. However, because the 3-lumens of these catheters are inadequate to precisely evaluate the relationship between SO and SB motility, a specially designed 8-lumen manometry catheter was used in this study to effectively record SO motility as well as assess the sequential progression of duodenal motility through to the proximal jejunum. However, the basal pressure of the SO could only be obtained using the 3-lumen catheter because the larger diameter of the manometry catheter could have altered the amplitude of the SO pressure wave [17]. Therefore, only data from 3-manometry catheter in 15 patients were obtained to analyze the basal pressure of the SO and we abandoned the pressure data from the 8-channel manometry catheter in 16 patients. However, when we compared the frequency and proportion of each phases of both catheters, there were no statistically significant differences between them. Therefore, we described not only individual results from the 3- and 8-channel manometry catheters, but also integrated results from both manometry catheters except for the basal pressure in Tables 2, 3 and 4.
In conclusion, the SO motility in humans showed cyclical phasic changes that were closely coordinated with the MMC of the SB in a fasting state. The proportion of phases I and II was different between the SO and the SB. Additionally, physiological high-frequency contractions, which significantly increased the basal pressure and coincided with phase III of the MMC of the SB, were noted in all patients without any apparent SO dysfunction. This evidence suggests that the SO contractility in humans is in close correlation with SB contractility but may possess innate contractility.
References
Honda R, Toouli J, Dodds WJ, Sarna S, Hogan WJ, Itoh Z. Relationship of sphincter of Oddi spike bursts to gastrointestinal myoelectric activity in conscious opossums. J Clin Invest. 1982;69:770–778.
Scott RB, Strasberg SM, El-Sharkawy TY, Diamant NE. Fasting canine biliary secretion and the sphincter of Oddi. Gastroenterology. 1984;87:793–804.
Coelho JC, Moody FG, Senninger N. A new method for correlating pancreatic and biliary duct pressures and sphincter of Oddi electromyography. Surgery. 1985;97:342–349.
Takahashi I, Dodds WJ, Itoh Z, Hogan WJ, Kern MK. Influence of transsphincteric fluid flow on spike burst rate of the opossum sphincter of Oddi. Gastroenterology. 1984;87:1292–1298.
Akita Y, Nimura Y, Yasui A. Percutaneous transhepatic manometry of sphincter of Oddi. Dig Dis Sci. 1991;36:1410–1417. https://doi.org/10.1007/BF01296808.
Torsoli A, Corazziari E, Habib FI, et al. Frequencies and cyclical pattern of the human sphincter of Oddi phasic activity. Gut. 1986;27:363–369.
Worthley CS, Baker RA, Iannos J, Saccone GT, Toouli J. Human fasting and postprandial sphincter of Oddi motility. Br J Surg. 1989;76:709–714.
Yuasa N, Nimura Y, Yasui A, Akita Y, Odani K. Sphincter of Oddi motility in patients with bile duct stones. A comparative study using percutaneous transhepatic manometry. Dig Dis Sci. 1994;39:257–267. https://doi.org/10.1007/BF02090195.
Kuo KK, Utsunomiya N, Nabae T, et al. Sphincter of Oddi motility in patients with hepatolithiasis and common bile duct stones. Dig Dis Sci. 2000;45:1714–1718. https://doi.org/10.1023/A:1005546631237.
Gorard DA, Vesselinova-Jenkins CK, Libby GW, Farthing MJ. Migrating motor complex and sleep in health and irritable bowel syndrome. Dig Dis Sci. 1995;40:2383–2389. https://doi.org/10.1007/BF02063242.
Gregg JA, Antal RD. Rhythm abnormalities of the biliary and pancreatic sphincters: diagnosis by endoscopic manometry. Am J Surg. 1984;148:602–606.
Hogan WJ, Geenen J, Venu R, Dodds WJ, Helm J, Toouli J. Abnormally rapid phasic contractions of the human sphincter of Oddi (tachyoddia). Gastroenterology. 1983;84:1189.
Corazziari E, Shaffer EA, Hogan WJ, Sherman S, Toouli J. Functional disorders of the biliary tract and pancreas. Gut.. 1999;45:Ii48–Ii54.
Behar J, Corazziari E, Guelrud M, Hogan W, Sherman S, Toouli J. Functional gallbladder and sphincter of oddi disorders. Gastroenterology. 2006;130:1498–1509.
Cotton PB, Elta GH, Carter CR, Pasricha PJ, Corazziari ES. Gallbladder and sphincter of Oddi disorders. Gastroenterology. 2016;150:1420–1429.
Guelrud M, Mendoza S, Vicent S, Gomez M, Villalta B. Pressures in the sphincter of Oddi in patients with gallstones, common duct stones, and recurrent pancreatitis. J Clin Gastroenterol. 1983;5:37–41.
Funch-Jensen P, Kraglund K, Djurhuus JC. The influence of measuring catheter diameter on direct manometry in the canine sphincter of Oddi. Scand J Gastroenterol. 1984;19:926–930.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Yoo, B.M., Kim, J.H., Yang, M.J. et al. Cyclic Change of Sphincter of Oddi Motility and Its Relationship with Small Bowel Migrating Motor Complex in Humans. Dig Dis Sci 63, 3425–3433 (2018). https://doi.org/10.1007/s10620-018-5276-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5276-0