Abstract
Background and Aims
To evaluate impact of ambulatory triglyceride levels on risk of recurrent pancreatitis in patients with hypertriglyceridemic pancreatitis.
Methods
We conducted a longitudinal retrospective cohort study of patients with serum triglyceride level ≥ 500 mg/dL during index hospitalization for acute pancreatitis within a regional integrated healthcare system between 2006 and 2013 (follow-up through 2015). Cases were identified based on combination of diagnosis codes and serum amylase/lipase. We used multivariable robust Poisson regression to determine independent effect of baseline (first outpatient) triglyceride measurement on risk of recurrent pancreatitis. Ambulatory triglyceride levels were categorized as normal (0–200 mg/dL), moderately elevated (201–500 mg/dL), and highly elevated (> 500 mg/dL). We further assessed factors related to likelihood of normalization of serum triglycerides (< 200 mg/dL) in the outpatient setting.
Results
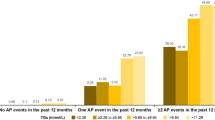
One hundred and fifty-one patients met study inclusion criteria with median follow-up of 3 years. Overall, 45 (29.8%) patients experienced at least 1 recurrent attack with 25 (16.6%) experiencing multiple episodes. In multivariable analysis, patients that continued to have moderately elevated ((adjusted rate ratio RR 5.47 (95% CL 1.80, 16.65)) as well as highly elevated (RR 8.45 (2.55, 27.96)) triglycerides were at increased risk of disease recurrence compared to patients that achieved normalization. Patients with triglyceride measurement performed within 30 days from discharge were more likely to achieve normalization, 40 versus 26%, p = 0.03.
Conclusions
For patients with hypertriglyceridemic pancreatitis, even modest elevation in subsequent triglyceride levels was associated with increased risk of recurrence. Future efforts should focus on ensuring timely care in the outpatient setting with a goal of normalizing triglycerides.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Elevated triglyceride levels are an uncommon but well-established etiology for acute pancreatitis. Hypertriglyceridemia has been estimated to account for 1–10% of all cases of acute pancreatitis [1, 2]. The incidence of acute pancreatitis has been shown to increase by the level of baseline hypertriglyceridemia [3, 4]. While several studies have indicated a relationship between hypertriglyceridemia and pancreatitis-associated complications [2, 5,6,7], limited data exist regarding the natural history of this form of acute pancreatitis.
Recidivism is of particular concern in acute pancreatitis with up to 10–30% of patients experiencing recurrent episodes [8,9,10]. Repeated episodes of acute pancreatitis contribute substantially to overall disease burden by prompting repeated hospitalization, adversely impacting quality of life as well as increasing the risk of progression to chronic pancreatitis. Because alcohol and gallstones are the most common causes of pancreatitis, extensive research has focused on methods to prevent disease recurrence in patients with these etiologies [11, 12]. To date, similar data on factors associated with disease recurrence in hypertriglyceridemic pancreatitis is lacking.
The objective of the present study was to characterize risk factors for disease recurrence in patients with hypertriglyceridemic acute pancreatitis. Specifically, we sought to quantify the impact of post-discharge triglyceride levels on risk of recurrent acute pancreatitis as well as identify factors associated with improved control of triglycerides in the ambulatory setting.
Methods
Study Design, Setting, and Patient Population
A retrospective cohort study was conducted on patients hospitalized at any of the Kaiser Foundation Southern California hospitals for acute pancreatitis between 2006 and 2013. Kaiser Permanente is an integrated healthcare system that comprises nine regions, of which Southern California is the largest comprising 13 acute care hospitals that serves a population of over 4.2 million active health plan enrollees. The health plan enrollees receive comprehensive services encompassing the full spectrum of care including ambulatory, inpatient, laboratory, and pharmacy services. This study was approved by the Kaiser Permanente Southern California Institutional Review Board.
Adult patients (≥ 18 years of age) were identified through a combination of discharge diagnosis codes for acute pancreatitis (International Classification of Disease (ICD-9) 577.1) and an elevated serum amylase/lipase (≥ 3 times upper limit of normal) during the first qualified (index) hospitalization between January 1, 2006, and December 31, 2013. This strategy has previously been shown to have a positive predictive value of > 95% when compared with manual chart validation based on clinical criteria [13]. Patients were then limited to those who had a triglyceride level ≥ 500 mg/dL (hypertriglyceridemia) at any point during the index hospitalization. To examine the impact of hypertriglyceridemia on recurrent acute pancreatitis, patients were further limited to those who had at least one outpatient triglyceride measure within 1 year following the index hospitalization.
Follow-up of each patient began on the date of outpatient triglyceride measure and ended with a readmission for acute pancreatitis (an event) or the earliest of the following dates: death, loss of health plan enrollment, or the study end date, December 31, 2015 (Fig. 1).
The same criteria that were used to define hospital admission with acute pancreatitis for the index hospitalization were applied to determine the study event (readmission with acute pancreatitis). Manual chart review was conducted to identify recurrent episodes of acute pancreatitis. During manual chart review, all episodes of acute pancreatitis were confirmed by two of the following three criteria: typical upper abdominal pain, amylase/lipase ≥ 3 times upper limit of normal, and/or confirmatory findings on cross-sectional imaging.
Study Variables
All variables were obtained from the Kaiser Permanente electronic health record, including other established etiologies of acute pancreatitis (alcohol abuse either self-reported from previous outpatient visits or any reported history of alcohol use in the year before index hospitalization, gallstone disease according to International Classification of Diseases, Ninth Revision code 574.x in the year before or year after index hospitalization; and [3] cholecystectomy [Current Procedural Terminology codes 47,562, 47,563, 47,600, 47,605] in the 180 days after index hospitalization)) and demographic variables including age and sex; as well as additional potential confounders: smoking (ever/never as obtained from the electronic record), obesity (body mass index > 30) and diabetes (defined by combination of diagnosis codes, medications and biochemical parameters). The Charlson’s comorbidity score was used as a measure of patient comorbidity [14]. Income and education levels were derived on the basis of members’ addresses using block-group-level estimates provided by Claritas, Inc. (http://www.claritas.com). For purposes of the present study, all patient demographic and clinical characteristics other than cholecystectomy were collected during or prior to the index hospitalization and they were referred to as baseline covariates.
Data Analysis
Descriptive analysis was performed to assess for differences in demographic and clinical characteristics relative to the index hospitalization of the acute pancreatitis patients with (> 500 mg/dL) and without (< 500 mg/dL) hypertriglyceridemia (Table 1). Among patients with hypertriglyceridemia who were qualified for the study, we examined the patient demographic and clinical characteristics by the baseline ambulatory triglyceride level, classified as low-normal (0–200 mg/dL), moderately elevated (200–500 mg/dL), and highly elevated (> 500 mg/dL). Patient characteristics are reported with number of patents and (%) for categorical variables, and with mean (SD) for normally distributed data or median (IQR) for non-normally distributed data. For group comparisons, we used Chi-square or Fisher’s exact test for categorical variables and t test or nonparametric Wilcoxon’s rank-sum test (for two groups), and analysis of variance (ANOVA) or Kruskal–Wallis test (for more than two groups), as appropriate. Shapiro–Wilk’s test of normality was used to determine whether the parametric assumption was appropriate.
Overall and risk factor-stratified crude event rates were calculated using the unadjusted log-linear (Poisson) regression models with a robust error variance and are reported as per 1000 person-days of follow-up. Rate ratios and the 95% confidence intervals were estimated using the low-normal triglyceride group as the reference group. We then performed a multivariable robust Poisson regression analysis to evaluate the effect of ambulatory triglyceride measurement on the risk of recurrent acute pancreatitis. Additional covariates included in the multivariable model included age, sex, alcohol etiology, Charlson’s comorbidity, and diabetes.
All analyses were performed in SAS statistical software version 9.3 (Cary, N.C). All reported p values are two-sided with alpha 0.05 level of significance.
Results
We identified a total of 5981 patients who were hospitalized for acute pancreatitis during the study period, of whom 2519 had a measured serum triglyceride during the index hospitalization. After applying study inclusion and exclusion criteria, 151 of the 237 patients with elevated triglycerides satisfied criteria for entry into the current study. Details of cohort assembly are presented in Fig. 2. In terms of ambulatory triglyceride levels, there were 47 (31.1%) patients with low-normal triglycerides, and 67 (44.4%) and 37 (24.5%) with moderately and high elevated triglycerides at baseline (Table 1), respectively. Median (interquartile range—IQR) time to the first outpatient triglyceride was 48 (16–101) days. Overall, 62.3% of patients had baseline ambulatory triglyceride measurement performed within 30 days of hospital discharge. Patients with normal baseline serum triglycerides (0–200 mg/dL) had significantly shorter time to baseline measurement (median 31 days) from index hospital discharge compared to patients with higher baseline levels (median 41 and 51 days for moderately elevated and highly elevated, respectively, p = 0.002). Patients with outpatient serum triglyceride measured within 30 days following discharge were more likely to have normalization of triglyceride levels (0–200 mg/dL) compared to patients with delayed triglyceride measurement, 40 versus 26%, p = 0.03).
Median duration of follow-up was 1,101 and 818 and 626 days for patients with low-normal, moderately elevated, and highly elevated outpatient triglyceride level, respectively (Table 2). A total of 29.8% (45/151) of patients experienced at least one recurrent acute pancreatitis requiring hospitalization during the study period. Among patients with recurrent acute pancreatitis, 25/45 (56%) experienced more than one recurrence during the study period with seven out of 45 patients (16%) experiencing five or more episodes.
Impact of Baseline Serum Triglyceride on Risk of Recurrent Acute Pancreatitis
The overall and covariate stratified event rates and rate ratios are presented in Table 2. Overall, elevated levels of baseline serum triglycerides were associated with a corresponding increase in risk of subsequent pancreatitis episodes. The overall event rates for recurrent acute pancreatitis were 0.21, 0.71, and 1.50 per 100-person-days, respectively, for patients with low-normal, moderately elevated, and highly elevated outpatient triglyceride level. The effect was significant primarily among patients aged 45 years or less as well as those without alcohol or diabetes history.
Using multivariable robust Poisson regression, elevation in baseline serum triglyceride level remained a significant independent risk factor for recurrent episodes of acute pancreatitis after adjusting for age, sex, Charlson comorbidity score, alcohol and diabetes (Table 3). Of note, even modest elevation (200–500 mg/dL) in baseline triglyceride was associated with a substantially increased risk with an adjusted rate ratio of 5.47 (95% confidence limit 1.80, 16.65). Higher levels of baseline triglyceride (> 500 mg/dL) were associated with a corresponding increase in risk of recurrent acute pancreatitis, adjusted risk ratio 8.45 (2.55, 27.96). There was also an inverse relationship between age and risk of recurrent pancreatitis such that older patients were at a reduced risk compared to patients aged < 45 years. A high Charlson score was also independently associated with increased risk of recurrent pancreatitis whereas alcohol and diabetes were not. There were no significant factors associated with delayed outpatient baseline measurement in multivariate analysis. In univariate analysis, for every point BMI increased, there was an 11.4% less likely chance of having > 30 days to baseline measurement. There was no evidence of interaction between variables included in the Poisson regression model.
Discussion
In this retrospective cohort study of patients with hypertriglyceridemic acute pancreatitis, we found that elevated triglycerides in the ambulatory setting were associated with increased risk of subsequent disease recurrence. In particular, even modest elevation of triglycerides (200–500 mg/dL) following discharge was associated with substantially increased risk of recurrent pancreatitis. Measurement of outpatient triglyceride within 30 days of discharge was significantly associated with improved baseline triglyceride control.
Although hypertriglyceridemia is a well-established risk factor for acute pancreatitis, relatively limited data are available regarding the natural history of this form of pancreatitis due to its rarity compared to other etiologies such as biliary or alcohol-related pancreatitis. Population-based data have helped to further define the risk of incident pancreatitis according to triglyceride levels [3]. Likewise, several recent studies have linked elevation in triglycerides in the hospital setting to increased risk of inpatient complications such as persistent organ failure [7]. The present study extends these previous findings by characterizing the impact of outpatient triglyceride levels on risk of recurrent acute pancreatitis in a well-defined cohort of patients with hypertriglyceridemic acute pancreatitis. Our finding of an increased risk of recurrent pancreatitis even at modest baseline triglyceride levels is consistent with previous studies that demonstrated a step-wise increase in risk of incident pancreatitis as well as pancreatitis-related complications at modestly increased triglyceride levels.
Hypertriglyceridemia is believed to trigger pancreatitis through downstream effects of liberated free fatty acids, which in turn can lead to direct mitochondrial injury with in the acinar cell. Specifically, in experimental animal models addition of free fatty acid exacerbated caerulin-induced pancreatitis through a cyclic GMP mediated pathway that promoted increased retention of intracellular calcium levels [1, 15]. It is unclear to what extent a previous pancreatic injury predisposes to augmented risk of pancreatitis for any given level of elevation in serum triglycerides. While findings from the present study were qualitatively similar to those reported from a recent population-based study from Denmark [16], the observed crude event rate appeared to be higher in the present study cohort potentially indicating an increased susceptibility to recurrent episodes following an incident attack of pancreatitis.
Besides the primary findings, there were several additional notable observations in the present study. First, it was interesting to note that younger patients were more likely to suffer disease recurrence. Second, the triglyceride effect appeared to be most pronounced among patients without history of chronic alcohol or diabetes. Taken together, these findings may indicate the underlying presence of a primary dyslipidemia in younger patients as opposed to elevation in triglycerides secondary to alcohol or diabetes among older patients. Another important observation from the present study was that over half (58%) of all the acute pancreatitis patients during the study period did not have a serum triglyceride measured at all during their hospitalization. In addition, among the patients with hypertriglyceridemic pancreatitis that was included in the present study, only 38% had a repeat triglyceride measurement obtained within 30 days of hospital discharge. These figures reflect current practice patterns and highlight opportunities for quality improvement initiatives.
There were several limitations to the present study. First, we used the first (baseline) outpatient triglyceride measurement following discharge as a proxy for overall triglyceride control. Triglyceride levels can fluctuate over time and the baseline measurement may not reflect subsequent levels. We were unable to pursue a more comprehensive approach to assess the impact of overall triglyceride control in the ambulatory setting due to a lack of available ambulatory measurements. However, the level of serum triglyceride when measured at the first outpatient setting was nevertheless significantly associated with risk of recurrent acute pancreatitis. That said, the time to first outpatient serum triglyceride measurement is likely a surrogate for additional factors including vigilance of physician follow-up as well as patient adherence to care recommendations. Another set of limitations for the present study was the lack of inpatient triglyceride measurement in over half the patients hospitalized for acute pancreatitis during the study period as well as delay in follow-up outpatient triglyceride measurement beyond 30-days for patients who were followed up. Given the retrospective nature of the study, it is possible that there were other mechanisms such as idiopathic recurrent pancreatitis that may have led to modestly elevated triglyceride measurements in these patients as well. Medications and medical comorbidities such as chronic kidney disease may also impact triglyceride measurements, but we were unable to adjust for those based on the limited sample size.
The present findings have several implications for clinical practice. First, we recommend that serum triglycerides should be routinely checked during hospitalization for acute pancreatitis. It is likely that we have underestimated the prevalence of HTG-related acute pancreatitis and recent literature indicates increased risk of pancreatitis-related complications with even modest elevation of triglycerides [7, 17]. Second, patients with elevated triglycerides during hospitalization should be scheduled for early follow-up in the ambulatory setting with a repeat measurement within 30 days of discharge. Finally, our data suggest that normalization of serum triglycerides below 200 mg/dL should be the goal of outpatient therapy to reduce risk of recurrent acute pancreatitis in this patient population.
In summary, in this study of patients with hypertriglyceridemic pancreatitis, we found that disease recurrence was common. There was substantial variation in the time to follow-up assessment of triglyceride levels after discharge. Patients with triglycerides measured within 30 days post-discharge were more likely to achieve triglyceride control at baseline. Even modest elevation in triglycerides (> 200 mg/dL) was associated with significant increase in risk of disease recurrence. These findings indicate that greater vigilance in monitoring patients with hypertriglyceridemic pancreatitis in the ambulatory setting with an emphasis on normalization of triglyceride levels may be an important opportunity to reduce risk of future episodes of pancreatitis in this population.
References
Ewald N, Hardt PD, Kloer H-U. Severe hypertriglyceridemia and pancreatitis: presentation and management. Curr Opin Lipidol. 2009;20:497–504. https://doi.org/10.1097/MOL.0b013e3283319a1d.
Tsuang W, Navaneethan U, Ruiz L, Palascak JB, Gelrud A. Hypertriglyceridemic pancreatitis: presentation and management. Am J Gastroenterol. 2009;104:984–991. https://doi.org/10.1038/ajg.2009.27.
Murphy MJ, Sheng X, MacDonald TM, Wei L. Hypertriglyceridemia and Acute Pancreatitis. JAMA Intern Med. 2013;173:162. https://doi.org/10.1001/2013.jamainternmed.477.
Scherer J, Singh VP, Pitchumoni CS, Yadav D. Issues in hypertriglyceridemic pancreatitis: an update. J Clin Gastroenterol. 2014;48:195–203. https://doi.org/10.1097/01.mcg.0000436438.60145.5a.
Anderson F, Thomson SR, Clarke DL, Buccimazza I. Dyslipidaemic pancreatitis clinical assessment and analysis of disease severity and outcomes. Pancreatology. 2009;9:252–257. https://doi.org/10.1159/000212091.
Deng L-H, Xue P, Xia Q, Yang X-N, Wan M-H. Effect of admission hypertriglyceridemia on the episodes of severe acute pancreatitis. World J Gastroenterol. 2008;14(28):4558–4561. http://www.ncbi.nlm.nih.gov/pubmed/18680239. Accessed June 21, 2017.
Nawaz H, Koutroumpakis E, Easler J, et al. Elevated serum triglycerides are independently associated with persistent organ failure in acute pancreatitis. Am J Gastroenterol. 2015;110:1497–1503. https://doi.org/10.1038/ajg.2015.261.
Lankisch PG, Breuer N, Bruns A, Weber-Dany B, Lowenfels AB, Maisonneuve P. Natural history of acute pancreatitis: a long-term population-based study. Am J Gastroenterol. 2009;104:2797–2805. https://doi.org/10.1038/ajg.2009.405.
Vipperla K, Papachristou GI, Easler J, et al. Risk of and factors associated with readmission after a sentinel attack of acute pancreatitis. Clin Gastroenterol Hepatol. 2014;12:1911–1919. https://doi.org/10.1016/j.cgh.2014.04.035.
Whitlock TL, Repas K, Tignor A, et al. Early readmission in acute pancreatitis: incidence and risk factors. Am J Gastroenterol. 2010;105:2492–2497. https://doi.org/10.1038/ajg.2010.234.
da Costa DW, Bouwense SA, Schepers NJ, et al. Same-admission versus interval cholecystectomy for mild gallstone pancreatitis (PONCHO): a multicentre randomised controlled trial. Lancet. 2015;386:1261–1268. https://doi.org/10.1016/S0140-6736(15)00274-3.
Nordback I, Pelli H, Lappalainen-Lehto R, Järvinen S, Räty S, Sand J. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology. 2009;136:848–855. https://doi.org/10.1053/j.gastro.2008.11.044.
Wu BU, Pandol SJ, Amy Liu I-L. Simvastatin is associated with reduced risk of acute pancreatitis: findings from a regional integrated healthcare system. Gut. 2014:1–6. https://doi.org/10.1136/gutjnl-2013-306564.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–1251. http://www.ncbi.nlm.nih.gov/pubmed/7722560. Accessed June 21, 2017.
Wang Y, Sternfeld L, Yang F, et al. Enhanced susceptibility to pancreatitis in severe hypertriglyceridaemic lipoprotein lipase-deficient mice and agonist-like function of pancreatic lipase in pancreatic cells. Gut. 2009;58:422–430. https://doi.org/10.1136/gut.2007.146258.
Pedersen SB, Langsted A, Nordestgaard BG. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis. JAMA Intern Med. 2016;176:1834–1842. https://doi.org/10.1001/jamainternmed.2016.6875.
Sue LY, Batech M, Yadav D, et al. Impact of serum triglycerides on clinical outcomes in acute pancreatitis: findings from a regional integrated healthcare system. Pancreas. 2017;46(7):874–879.
Acknowledgments
A portion of this study was funded through a research grant from Shire pharmaceuticals, Lexington MA. The sponsor did not have any role in data analysis, interpretation or manuscript preparation/review.
Author information
Authors and Affiliations
Contributions
Dr. Wu contributed to study concept, design, interpretation of data, manuscript preparation, and revision. Dr. Batech contributed to data collection, data analysis, data interpretation, and manuscript preparation. Dr. Dong contributed to data collection, data interpretation, and critical revision of manuscript. Dr. Yadav contributed to study concept, study design, interpretation of data, and manuscript revision. Dr. Chen contributed to study concept, data analysis, data interpretation, and revision of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors affirm they have no relevant financial conflicts to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix
Appendix
See Table 4.
Rights and permissions
About this article
Cite this article
Wu, B.U., Batech, M., Dong, E.Y. et al. Influence of Ambulatory Triglyceride Levels on Risk of Recurrence in Patients with Hypertriglyceridemic Pancreatitis. Dig Dis Sci 64, 890–897 (2019). https://doi.org/10.1007/s10620-018-5226-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-5226-x