Abstract
Background
Gastric per oral endoscopic myotomy (G-POEM) of the pylorus is a technique that is recently being used to treat gastroparesis. Our aim was to report our experience in performing G-POEM for refractory gastroparesis of different etiologies and determine symptom improvement.
Methods
Thirteen patients undergoing G-POEM are reported. Pre- and post-procedure gastric emptying study (GES) and PAGI-SYM for symptom severity were obtained. Patients underwent G-POEM by creating a submucosal tunnel starting in the greater curvature of the distal antrum and extending it to the beginning of the duodenal bulb, followed by a full thickness pyloromyotomy.
Results
All 13 gastroparesis patients successfully underwent G-POEM (one diabetic [DGp], four idiopathic [IGp], eight postsurgical [PSGp]). Postsurgical patients included 4 s/p esophagectomy for esophageal cancer, 3 s/p Nissen fundoplication, and 1 s/p esophagectomy for achalasia. There were no procedure-related side effects. Of 11 patients completing follow-up questionnaires, eight were improved subjectively (four patients reported considerably better, four patients somewhat better, one unchanged, and two worse). Individual symptom severity scores tended to improve, particularly vomiting, retching, and loss of appetite. Of six patients that had post-G-POEM GES; GES improved in four, unchanged in one, and worsened in one).
Conclusions
G-POEM for treatment of refractory gastroparesis appears to be a feasible and safe technique that can be successfully performed in patients with a variety of etiologies including different types of postsurgical gastroparesis. Our initial experience suggests that the majority of patients report some improvement in symptoms, particularly symptoms of vomiting, retching, and loss of appetite. Further experience is needed to determine the efficacy and safety of G-POEM and predict those who best respond to this treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroparesis is a disorder defined objectively by delayed gastric emptying in the absence of mechanical obstruction and subjectively by symptoms such as early satiety, nausea, vomiting, postprandial fullness, and upper abdominal pain [1]. Gastric emptying does not correlate well with symptoms in gastroparesis. Gastroparesis has three primary etiologies, diabetic gastroparesis (DGp), idiopathic gastroparesis (IGp), and postsurgical gastroparesis (PSGp). Patients with gastroparesis are often treated with prokinetic drugs such as metoclopramide, erythromycin, and domperidone as well as with antiemetic agents such as promethazine and ondansetron, but response may be limited and side effects may occur [2]. For refractory patients, treatment options are limited. Gastric electric stimulation has also been tried, but this is listed by the FDA as humanitarian device exemption.
The pyloric sphincter helps regulate gastric emptying. Prior studies using water perfused manometry and high-resolution manometry have characterized the pylorus muscle as a sphincter which is seen as an area of high pressure on manometry. Some patients with diabetic gastroparesis can have pylorospasm, which is prolonged periods of increased pyloric tone and phasic contractions [3,4,5]. Studies of the pylorus using the Endoscopic Functional Luminal Imaging Probe (EndoFLIP) showed that the pylorus in gastroparesis patients has higher pressure and lower compliance compared to normal subjects [6] with pyloric diameter and cross-sectional area (CSA) associated with symptoms of early satiety and postprandial fullness [7].
Therapies for gastroparesis have been directed toward the pylorus with partial success. Previous open label studies have shown some improvement in symptoms and gastric emptying after botulinum neurotoxin A (BoNT/A) [8]. BoNT/A injection to the pylorus inhibits release of acetylcholine and reduces pyloric smooth muscle pressure [9]. However, placebo-controlled studies showed similar responses in composite symptoms of gastroparesis when comparing BoNT/A and placebo [2, 10]. Another approach has been through surgical pyloroplasty, which has been in use for over 40 years. Hibbard et al. [11] showed that the use of surgical pyloromyotomy in patients with gastroparesis improved both symptom scores as well as gastric emptying. Later studies demonstrated adding a surgical pyloroplasty to use of gastric electric stimulator placement improved both symptoms of gastroparesis as well as gastric emptying, both in short-term and long-term follow-up [12, 13]. Transpyloric stenting of the pylorus has shown initial improvement in symptoms and gastric emptying, but there is concern for stent migration and long-term viability [14, 15].
Per oral endoscopic myotomy (POEM) is a newer technique that was initially used for the treatment of achalasia and was first described by Ortega et al. and first performed on a human by Inoue [16, 17]. With the development of this technique and the successful results of other pyloric therapies, an endoscopic pyloromyotomy was theorized, with its first application in pigs by Kawai et al. [18] and first human case performed by Khashab et al. which was published in 2013 [19]. Recently, a multicenter trial was published with data on 30 patients who received G-POEM for gastroparesis, showing 86% clinical response and only two adverse events (6.7%) [20].
Our aim in this study was to report our results in performing G-POEM performed by a single endoscopist in patients with refractory gastroparesis from a variety of etiologies of gastroparesis, including atypical forms of gastroparesis, and determine the symptom improvement as well as to use EndoFLIP to see if there were pyloric sphincter characteristics that could predict a successful procedure.
Methods
The first 13 patients undergoing G-POEM are reported in this study from October 2015 to October 2016. Patients were offered this procedure if they had ongoing severe refractory symptoms for which a pyloromyotomy was suggested for treatment of their refractory symptoms. Our center also provides treatment with domperidone and gastric electric stimulation; stimulator placement was generally offered to diabetic or idiopathic gastroparesis patients with refractory nausea and vomiting prior to considering pyloromyotomy, or at times, a pyloromyotomy was suggested to be done laparoscopically with placement of GES. The G-POEM procedures were performed by a single interventional endoscopist (SS), experienced in endoscopic submucosal dissection (ESD) and POEM, at either Winthrop University Hospital or Temple University Hospital. Pre-procedure gastric emptying study (GES) was done on all patients. Each patient filled out a questionnaire that included the Patient Assessment of GI Symptoms (PAGI-SYM). The PAGI-SYM, which includes the Gastroparesis Cardinal Symptom Index, assesses symptoms of gastroparesis asking about their primary symptom of gastroparesis as well as the severity of other symptoms including nausea, stomach fullness, loss of appetite, bloating, retching, vomiting, stomach visibly larger, not able to finish a normal size meal, feeling excessively full after meals, and upper abdominal pain. Patients graded their symptoms severity over the prior 2 weeks from 0 (none) to 5 (very severe) [21, 22].
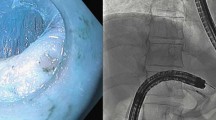
Patients underwent G-POEM during endoscopic gastroduodenoscopy (EGD) procedure under general anesthesia using a standard Olympus 190 upper endoscope. The technique used was adopted from Dr. Inoue described in the initial G-POEM procedure with some modifications [19]. After completing an initial diagnostic EGD, an Endoscopic Functional Luminal Imaging Probe (EndoFLIP) measurement of the pylorus was taken, if felt to be clinically feasible and safe. A gentamicin wash was then performed of the stomach, esophagus, and oral cavity. The G-POEM procedure was then started by creating a submucosal tunnel starting in the greater curvature of the distal antrum 5 cm proximal to the pylorus and extending it to the beginning of the duodenal bulb using an I-Type Hybrid Knife. This was followed by a full thickness pyloromyotomy using an I-Type Hybrid Knife or a Hook Knife. Post-pyloromyotomy EndoFLIP was then performed if it was felt to be clinically feasible and safe. The submucosal tunnel was then closed using an endoscopic suturing device. Any accidental mucosotomy was closed using clips. Patients were admitted to the hospital after the G-POEM. An upper GI series was performed on either day 1 or day 2 post-G-POEM based on the patients’ clinical symptoms to evaluate for perforation. If there was no leak seen on the upper GI series, patient was started on a liquid diet and when able to tolerate the diet without pain was discharged home.
Post-procedure GES and repeat questionnaire were performed approximately 3 months after treatment to assess treatment response to G-POEM. Patients filled out the CPGAS (Clinical Patient Grading Assessment Score) to assess their overall response to the treatment mainly if they had improved or not (as a dichotomized response) and the degree of their improvement from + 3 to − 3: + 3 (completely better); + 2 (considerably better); + 1 (somewhat better); 0 (unchanged); − 1 (somewhat worse); − 2 (considerably worse); − 3 (very considerably worse) [23]. This CPGAS is analogous to clinical global patient impression (CGPI), used in other treatment trials [24].
Statistical Analysis
Data and statistical analysis were performed using a de-identified Microsoft Excel database. Student’s t test was used to compare pretreatment and posttreatment values, responders and non-responders, as well as different subtypes of gastroparesis. Results are expressed as mean ± standard deviation (SD).
Results
Patients
Thirteen patients with refractory gastroparesis (persistent symptoms and gastric retention) successfully underwent G-POEM (mean age 45.7 ± 10.3 years; six male, seven females) (Table 1). One patient had diabetic gastroparesis (DGp), four had idiopathic gastroparesis (IGp), and eight were postsurgical gastroparesis (PSGp). Of the eight PSGp patients, three were post-Nissen fundoplication and five had atypical postsurgical gastroparesis (four post-esophagectomy for esophageal cancer, and one post-esophagectomy with gastric pull-up for achalasia). Eleven of the 13 patients had previously been treated with Botox injections of the pylorus (one DGp, four IGp, six PSGp), one PSGp had previously had pyloric surgery as well as balloon dilations, and one had no previous pyloric treatment (PSGp). Three of the patients had previous gastric stimulators placed (one DGp, two IGp).
G-POEM Procedure
The average time for G-POEM was 119 ± 23 min from scope insertion to removal. The average length of the submucosal tunnel was 6.8 ± 2.0 cm which took an average of 35 ± 13 min to complete. The average myotomy length was 3.5 ± 0.8 cm which took an average of 23.9 ± 9.3 min to complete. The average time for the submucosal tunnel to be closed with a running suture was 5.1 ± 2.8 min. The average time from incision to closure of the G-POEM was 64.4 ± 17.1 min. During the procedure, three patients had an accidental mucosotomy and all were closed with clips. The average length of hospital stay post-G-POEM was 2.5 ± 1.4 days. None of the patients had a leak on the upper GI series that was done post-procedurally. Post-procedurally, there was only one complication, a pulmonary embolism (PE) in a patient who had previously had a PE and there was suspicion of underlying hematologic abnormality.
EndoFLIP
EndoFLIP measurements of the pylorus were taken pre-procedurally in nine patients and post-procedurally in four patients. The EndoFLIP measurements were not performed in two patients: in two patients, the catheter could not be passed past the pylorus, whereas in two patients, it was not attempted due to the timing of the case. Measurements were taken with 30-, 40-, 50-ml balloon inflation. Prior to the procedure, with 30-ml inflation, the pylorus was characterized as average pressure of 15.7 ± 8.4 mm Hg, cross-sectional area (CSA) of 78.2 ± 34.8 mm2, diameter of 9.7 ± 2.2 mm, distensibility of 6.0 ± 3.3 mm2/mmHg, and compliance of 196 ± 99 mm3/mmHg. Immediately after the G-POEM procedure, there were trends to improvement with decrease in average pressure of 9.6 ± 10.8 mm Hg, increase in CSA of 83.6 ± 27.3 mm2 and diameter of 10.2 ± 1.6 mm, and improved distensibility to 6.6 ± 5.2 mm2/mmHg and compliance to 203 ± 178 mm3/mmHg. When comparing patients that clinically improved with those that did not, only one measurement showed significant difference—minimum diameter with 40 cc balloon volume; a larger CSA was present in those improving (14.7 vs. 12.3 mm2, p = 0.04). No other significant differences were seen between EndoFLIP and clinical response, symptom scores, or gastric emptying.
Symptom Response
Eleven of the 13 patients completed their follow-up questionnaires at approximately 3-month follow-up (108 ± 69 days). Of these 11 patients, eight were improved subjectively using the CGPAS (73%) (three IGp, five PSGp), two were worsened (IGp, PSGp), and one was unchanged (PSGp). Overall, the mean CGPAS score was 0.6 ± 1.6.
Of the 11 patients with follow-up information, four patients had a CGPAS score of 2 (considerably better). The response to the G-POEM tended to be better if patients had a prior clinical improvement to Botox injection into the pylorus. We had response information to eight of the eleven patients undergoing prior Botox injection of the pylorus before the G-POEM. Of five patients that responded to Botox injection of the pylorus, three (60%) responded to G-POEM, whereas of three patients not responding to Botox injection of the pylorus, only one (33%) responded to G-POEM.
No significant difference was seen between pre and post-GCSI scores when looking at all patients (2.1 ± 0.8 vs 1.9 ± 1.0) and patients that showed improvement (1.9 ± 0.6 vs 1.6 ± 1.0) or no improvement (2.8 ± 1.1 vs 2.7 ± 0.7). There was a trend toward a lower starting GCSI in patients who improved when compared to those who did not improve (1.9 ± 0.6 vs 2.8 ± 1.1; p = 0.14). Using the clinically meaningful change of the GCSI of 0.5 [22], five of the eleven patients with follow-up had a clinically meaningful improvement. The individual symptom scores, particularly vomiting, retching, and loss of appetite, tended to improve in patients with reduction of symptom severity of 29, 24, and 24%, respectively (Table 2). The GCSI score does not factor in symptoms of regurgitation or abdominal pain that some of our patients had.
Gastric Emptying
All patients had delayed gastric emptying before the procedure, averaging 78% retention at 2 h and 49% retention at 4 h. Post-G-POEM GES was obtained in six patients. Gastric emptying improved with the percent retention at 2 h decreasing from 79 to 60% (p = 0.06) and the percent retention at 4 h decreasing from 49 to 33% (p = 0.10) (Table 2). In the six patients with follow-up gastric emptying tests, four improved gastric emptying (three clinically improved, one unchanged), one had an unchanged gastric emptying (clinically improved), and one had a worsened gastric emptying (clinically improved). Of the four GES that improved, two studies were within normal limits after G-POEM, one was mildly abnormal (12% retention, normal < 10%) which was the patient who subjectively was unchanged, and one was markedly abnormal but improved from baseline (97% retention to 65% retention) (Table 1).
Discussion
This study demonstrates that G-POEM for treatment of refractory gastroparesis appears to be a feasible and safe procedure. Furthermore, our study shows that G-POEM can be performed in a variety of patients with different types of gastroparesis including different types of atypical postsurgical gastroparesis. This study had 100% procedural success with no procedural complications. The majority of patients reported being at least ‘somewhat’ better. Individual symptoms tended to improve particularly vomiting, retching, and loss of appetite which tended to have 20–30% decrease in symptom score. Only one adverse event was reported (pulmonary embolism). This patient had a previous history of pulmonary embolism.
Our single-center results are similar to other G-POEM studies that have been reported (see Table 3 for comparison of previous study results) as well as surgical pyloroplasty studies [10]. Three previous single-center trials were performed ranging from seven patients to 29 patients, mainly performed on DGp and IGp, had similar clinical efficacy as our study ranging from 81 to 86% improvement [25,26,27]. The Khashab et al. report was a retrospective multicenter study of five centers included 30 patients both of which had a 100% procedural success and 86% clinical response and 7% complication rate, which unfortunately did not use a validated gastroparesis symptom questionnaire [20]. Of interest, our study shows the procedure was able to be accomplished in a number of different forms of atypical and postsurgical gastroparesis.
The utility of the EndoFLIP in assessing pyloric dysfunction in patients with gastroparesis is being reported. Gourcerol et al. [27] showed fasting pyloric compliance in patients with gastroparesis was significantly lower than in healthy controls and correlated with symptom severity and gastric emptying time. Malik et al. [7] showed pyloric diameter and cross-sectional area were inversely correlated with symptom severity. Snape et al. [30] demonstrated significant correlation between pyloric distensibility and pressure and showed that reduced pyloric distensibility was associated with delayed gastric emptying. It was our hypothesis that EndoFLIP measurements taken prior to G-POEM may help to determine which patients will benefit from G-POEM and those who will not. Although no correlation was seen, our numbers are limited and further studies with the use of EndoFLIP are needed. Our post-procedure EndoFLIP measurements were taken right after the endoscopic pyloromyotomy; perhaps, there is swelling and inflammation affecting the measurements and performing this later after the pyloromyotomy would be better to assess the improvement in pyloric characteristics. We found the intubation of the pylorus with the EndoFLIP catheter could be difficult due to looping of the catheter in the stomach; better techniques to intubate the pylorus are being developed.
Many of our patients had prior botulinum toxin injections into the pylorus. BoNT/A injections into the LES have been reported to make Heller myotomy and POEM more difficult in achalasia due to scarring induced by the BoNT/A injection [31]. We did not find that this made the G-POEM procedure more difficult. The response to G-POEM tended to be greater in those that had a clinical response to Botox injection into the pylorus, compared those that Botox did not help symptoms. Pylorospasm appears to be relevant disease mechanism in a subset of gastroparesis patients. The response to BoNT/A injections into the pylorus may help predict those who might respond to G-POEM. Further studies are needed to help investigate if the response to pyloric botulinum toxin injection is a helpful test to see who might respond to G-POEM.
Each of the patients had refractory gastroparesis with persistent symptoms and delayed gastric emptying. Many of the postsurgical patients had low gastroparesis symptoms, as assessed by the GCSI. This might have been from their prior vagotomy as the vagus nerve mediates sensory transmission from the GI tract or due to atypical symptoms of gastroparesis as several patients had initially esophageal disorders such as achalasia and had post-esophagectomy gastroparesis. The lack of significant change in the GCSI might have been due to the lower GCSI values that were present at baseline. The symptoms that responded to G-POEM in our study included vomiting, retching, and loss of appetite. A larger number of patients undergoing this procedure would strengthen this statement statistically. Our study used the commonly used, validated questionnaire, PAGI-SYM that includes the Gastroparesis Cardinal Symptom Index (GCSI) and captures other symptoms such as upper abdominal pain. Interestingly, our study revealed a lower starting GCSI in patients who improved compared with those who did not respond. This suggests those with lower GCSI and less severe symptomatic disease had a better response whereas those with more severe symptoms who may have more severe gastroparesis with antral hypomotility that would not be improved with pyloromyotomy. Perhaps pyloromyotomy should be performed earlier in the disease course rather than in patients that are refractory to other treatments as was done in our study. No other predictive factors of response were seen in our small study. Gonzalez et al. [26] suggest that diabetes and female gender were associated with a poor response. Further larger-scale studies will be needed to determine the utility of pre-procedural testing including EndoFLIP as response to other treatments such as Botox injection of the pylorus.
Our study had the patients rate their response to treatment with G-POEM using the CGPAS. The CPGAS is analogous to clinical global patient impression (CGPI), used in other treatment trials. Using this assessment, 73% of patients rated an improvement with the G-PEOM procedure. Of our 11 patients with follow-up information, four had a score of 2 (considerably better). The more favorable response with the CPGAS assessment than the GCSI might stem from the CPGAS including other symptoms that patients deem important to their disorder, such as regurgitation and abdominal pain.
Gastric emptying improved with the G-POEM procedure and normalized in some patients. Patients had initially the 4-h gastric emptying scintigraphy test. We were unable to obtain post-procedure gastric emptying tests in all patients, in part, due to referral areas being some distance from our center.
There are several limitations in this study. This study was performed at an academic medical center, one with experience with gastroparesis, and the procedure was performed by an expert interventional endoscopist. We did not have follow-up on all the patients—symptoms and gastric emptying. Finally, the EndoFLIP data were not obtained on all patients pre- and post-procedure as the catheter could not be passed across the pylorus in all patients.
In conclusion, our single-center study involving 11 patients in whom follow-up data were available shows that G-POEM is a potential treatment option of refractory gastroparesis. G-POEM appears to be feasible, safe, and potentially useful technique. Furthermore, our study shows that G-POEM can be performed in a variety of patients with different types of gastroparesis including different types of atypical postsurgical gastroparesis. Of the gastroparesis symptoms, vomiting, retching, and loss of appetite tended to improve the most. Post-procedure gastric emptying scintigraphy was available in only six patients: four showed improvements, one unchanged, and one worse. Randomized sham-controlled studies are needed to further assess the efficacy of G-POEM and to predict those who respond best to this treatment.
References
Camilleri M, Parkman HP, Shafi MA, Abell TL, Gerson L, American College of Gastroenterology. Clinical guideline: management of gastroparesis. Am J Gastroenterol. 2013;108:18–37.
Arts J, Holvoet L, Caenepeel P, et al. Clinical trial: a randomized-controlled crossover study of intrapyloric injection of botulinum toxin in gastroparesis. Aliment Pharmacol Ther. 2007;26:1251–1258.
Fisher R, Cohen S. Physiological characteristics of the human pyloric sphincter. Gastroenterology. 1973;64:67–75.
Desipio J, Friedenberg FK, Korimilli A, Richter JE, Parkman HP, Fisher RS. High-resolution solid-state manometry of the antropyloroduodenal region. Neurogastroenterol Motil. 2007;19:188–195.
Mearin F, Camilleri M, Malagelada JR. Pyloric dysfunction in diabetics with recurrent nausea and vomiting. Gastroenterology. 1986;90:1919–1925.
Gourcerol G, Tissier F, Melchior C, et al. Impaired fasting pyloric compliance in gastroparesis and the therapeutic response to pyloric dilatation. Aliment Pharmacol Ther. 2015;41:360–367.
Malik Z, Sankineni A, Parkman HP. Assessing pyloric sphincter pathophysiology using EndoFLIP in patients with gastroparesis. Neurogastroenterol Motil. 2015;27:524–531.
Miller LS, Szych GA, Kantor SB, et al. Treatment of idiopathic gastroparesis with injection of botulinum toxin into the pyloric sphincter muscle. Am J Gastroenterol. 2002;97:1653–1660.
James AN, Ryan JP, Parkman HP. Inhibitory effects of botulinum toxin on pyloric and antral smooth muscle. Am J Physiol Gastrointest Liver Physiol. 2003;285:G291–G297.
Friedenberg FK, Palit A, Parkman HP, Hanlon A, Nelson DB. Botulinum toxin A for the treatment of delayed gastric emptying. Am J Gastroenterol.. 2008;103:416–423.
Hibbard ML, Dunst CM, Swanstrom LL. Laparoscopic and endoscopic pyloroplasty for gastroparesis results in sustained symptom improvement. J Gastrointest Surg. 2011;15:1513–1519.
Sarosiek I, Forster J, Lin Z, Cherry S, Sarosiek J, McCallum R. The addition of pyloroplasty as a new surgical approach to enhance effectiveness of gastric electrical stimulation therapy in patients with gastroparesis. Neurogastroenterol Motil. 2013;25:134-e80.
Davis BR, Sarosiek I, Bashashati M, Alvarado B, McCallum RW. The long-term efficacy and safety of pyloroplasty combined with gastric electrical stimulation therapy in gastroparesis. J Gastrointest Surg. 2017;21:222–227.
Clarke JO, Sharaiha RZ, Kord Valeshabad A, Lee LA, Kalloo AN, Khashab MA. Through-the-scope transpyloric stent placement improves symptoms and gastric emptying in patients with gastroparesis. Endoscopy. 2013;45:E189–E190.
Khashab MA, Besharati S, Ngamruengphong S, et al. Refractory gastroparesis can be successfully managed with endoscopic transpyloric stent placement and fixation (with video). Gastrointest Endosc. 2015;82:1106–1109.
Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8–10.
Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271.
Kawai M, Peretta S, Burckhardt O, Dallemagne B, Marescaux J, Tanigawa N. Endoscopic pyloromyotomy: a new concept of minimally invasive surgery for pyloric stenosis. Endoscopy. 2012;44:169–173.
Khashab MA, Stein E, Clarke JO, et al. Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2013;78:764–768.
Khashab MA, Ngamruengphong S, Carr-Locke D, et al. Gastric per-oral endoscopic myotomy for refractory gastroparesis: Results from the first multicenter study on endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2017;85:123–128.
Rentz AM, Kahrilas P, Stanghellini V, et al. Development and psychometric evaluation of the patient assessment of upper gastrointestinal symptom severity index (PAGI-SYM) in patients with upper gastrointestinal disorders. Qual Life Res. 2004;13:1737–1749.
Revicki DA, Rentz AM, Dubois D, et al. Development and validation of a patient-assessed gastroparesis symptom severity measure: the gastroparesis cardinal symptom index. Aliment Pharmacol Ther. 2003;18:141–150.
Maranki JL, Lytes V, Meilahn JE, et al. Predictive factors for clinical improvement with Enterra gastric electric stimulation treatment for refractory gastroparesis. Dig Dis Sci. 2008;53:2072–2078.
Parkman HP, Van Natta ML, Abell TL, et al. Effect of nortriptyline on symptoms of idiopathic gastroparesis: the NORIG randomized clinical trial. JAMA.. 2013;310:2640–2649.
Shlomovitz E, Pescarus R, Cassera MA, et al. Early human experience with per-oral endoscopic pyloromyotomy (POP). Surg Endosc. 2015;29:543–551.
Gonzalez JM, Benezech A, Vitton V, Barthet M. G-POEM with antro-pyloromyotomy for the treatment of refractory gastroparesis: mid-term follow-up and factors predicting outcome. Alim Pharm Ther. 2017;46:364–370.
Dacha S, Mekaroonkamol P, Li L, et al. Outcomes and quality-of-life assessment after gastric per-oral endoscopic pyloromyotomy (with video). Gastrointest Endosc. 2017;86:282–292.
Rodriguez JH, Haskins IN, Strong AT, et al. Per oral endoscopic pyloromyotomy for refractory gastroparesis: initial results from a single institution. Surg Endosc. 2017;31:5381–5388.
Jacques J, Pagnon L, Hure F, Legros R, Charissoux A, Fauchais AL, Palat S, Ducrotte P, Martin B, Fontaine S, Bonbaddi NE, Clement MP, Sautereau D, Loustaud-Ratti V, Gourcerol G, Monteil J. Per-oral endoscopic pyloromyotomy is efficacious and safe for refractory gastroparesis: the first prospective study with a concomitant assessment of pyloric function. Gut 2018 (in press).
Snape WJ, Lin MS, Agarwal N, Shaw RE. Evaluation of the pylorus with concurrent intraluminal pressure and EndoFLIP in patients with nausea and vomiting. Neurogastroenterol Motil. 2016;28:758–764.
Patti MG, Feo CV, Arcerito M, et al. Effects of previous treatment on results of laparoscopic Heller myotomy for achalasia. Dig Dis Sci. 1999;44:2270–2276.
Author information
Authors and Affiliations
Contributions
Zubair Malik, MD was involved in study concept and design; data entry; analysis and interpretation of data; statistical analysis; drafting of manuscript. Rahul Kataria, MD, Adam C. Ehrlich, MD, Ron Schey, MD contributed to analysis and interpretation of data; critical revision of the manuscript for important intellectual content. Rani Modayil, MD helped in analysis and interpretation of data; statistical analysis; critical revision of the manuscript for important intellectual content. Henry P. Parkman, MD, Stavros Stavropoulos, MD were involved in study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content; study supervision.
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Malik, Z., Kataria, R., Modayil, R. et al. Gastric Per Oral Endoscopic Myotomy (G-POEM) for the Treatment of Refractory Gastroparesis: Early Experience. Dig Dis Sci 63, 2405–2412 (2018). https://doi.org/10.1007/s10620-018-4976-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4976-9