Abstract
Background and Aims
Our goal was to compare the diagnostic accuracy of FISH in the detection of malignancy compared with other standard diagnostic modalities, including brush cytology and biopsy specimens over a 10-year period of prospective data collection.
Methods
We conducted a review of all consecutive biliary strictures evaluated between 2006 and 2016. Patients with a final pathologic diagnosis or conclusive follow-up were included. We evaluated the performance of FISH polysomy (CEP 3, 7, and 17) and 9p21 deletion as well as cholangioscopic biopsy (CBx) and EUS-FNA. Statistical analysis was performed with the Mann–Whitney U and Fisher’s exact tests.
Results
Of 382 patients with indeterminate strictures, 281 met inclusion criteria. Forty-nine percent were malignant. Cytology, FISH polysomy, and FISH polysomy/9p21 showed a specificity of 99.3%. FISH polysomy/9p21 as a single modality was the most sensitive at 56% (p < 0.001). The sensitivity of FISH polysomy/9p21 and cytology was significantly higher than cytology alone at 63 versus 35% (p < 0.05). EUS-FNA for distal strictures and CBx for proximal strictures increased sensitivity from 33 to 93% (p < 0.001) and 48–76% (p = 0.05) in cytology-negative strictures.
Conclusions
The high specificity of FISH polysomy/9p21 suggests that a positive result is sufficient for diagnosing malignancy in indeterminate strictures. The significantly higher sensitivity of FISH polysomy/9p21 compared to cytology supports the use of FISH in all non-diagnostic cases. Although both EUS-FNA and CBx were complimentary, our results suggest that distal strictures should be evaluated by EUS initially. Proximal strictures may be evaluated by FISH first and then by CBx if inconclusive.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Although several recent therapeutic advances have been made with regard to biliary malignancies, the accurate diagnosis of malignancy in a biliary stricture remains a challenge [1, 2]. At present, biliary brushings obtained for cytology during endoscopic retrograde cholangiopancreatography (ERCP) remain the most common first-line diagnostic approach [3]. Despite a specificity of 100%, cytology has a sensitivity as low as 5–40% for the diagnosis of malignancy in biliary strictures [4]. As such, cytology is inadequate alone to rule out the presence of malignancy without follow-up diagnostic testing.
Fluorescence in situ hybridization (FISH) uses fluorescence-labeled probes to evaluate the presence of chromosomal abnormalities in cells obtained via routine biliary brushings. When FISH is added to routine cytology, several groups have demonstrated increased yield in diagnosing biliary malignancy [3, 5,6,7,8]. The best characterized aneuploid chromosomal regions are on chromosomes 3, 7 and 17 (CEP 3, 7, 17) [5, 7]. We have previously demonstrated that the detection of homozygous or heterozygous deletion of the 9p21 locus (p16) in addition to polysomy increases the diagnostic yield of biliary malignancy [7]. Recently, additional loci have been evaluated and shown slightly higher sensitivity for the detection of malignancy [5].
Although there are multiple reports on different size cohorts regarding the utility of FISH in the diagnosis of biliary strictures, we report here on the use of this modality over a 10-year period. Our primary goal was to evaluate the accuracy of FISH in this large cohort of prospectively followed patients and compare the accuracy to cytology and additional diagnostic modalities (such as endoscopic ultrasound-fine needle aspiration (EUS-FNA) and cholangioscopic biopsy (CBx)) that were performed in these cases.
Methods
Patient Population
This study was approved by the Institutional Review Board of Columbia University and New York Presbyterian Hospital. All consecutive patients who underwent diagnostic evaluation for biliary strictures between 2006 and 2016 were included provided that they had ≥ 12-month follow-up or a final pathological diagnosis. Among patients with concurrent stone disease, only those in whom a significant stricture (deemed necessary to both evaluate and treat by the performing endoscopist) were included. Patients were excluded if sampling was done for abnormalities other than a stricture on the cholangiogram or lacked FISH test results in their medical record. A stricture was designated as benign if at ≥ 12-month follow-up repeat imaging or ERCP documented the resolution or stability of prior ductal abnormalities. A diagnosis of malignancy was made when either biopsy or cytology specimens demonstrated malignancy, final pathology was obtained by surgery, or if the cause of death was secondary to pancreatobiliary malignancy. The diagnosis of PSC was made based on cholangiographic findings associated with laboratory abnormalities or liver biopsy combined with a lack of other etiology of the stricture.
Specimen Collection
Samples were obtained for both cytology and FISH using two standard cytology brushes during ERCP (RX cytology brush, Boston Scientific, Cambridge, MA or Infinity sampling device, US endoscopy, Mentor, OH). Specimens were obtained with at least 10 to-and-fro motions at the site of the dominant stricture for both cytology and FISH specimens. The brush was cut and placed into 15 mL of ThinPrep CytoLyt solution (Marlborough, Mass) and was transferred to the cytogenetics laboratory within 24 h. For the FISH analysis, a separate brush was used (always following the taking of the cytology specimen). The cytology from the biliary brushings was then analyzed by a cyto-pathologist. Samples were classified using the Bethesda Category scoring system for cytology, scaled from I to VI: “I—non-diagnostic,” “II—negative for malignancy,” “III—atypical,” “IV—neoplastic: benign or other,” “V—suspicious,” and “VI—positive or malignant.” For this study, all non-Bethesda scored cytology results were converted to the Bethesda Category scoring system from the pathology report. For the purposes of this study, we defined a positive cytology result as either Bethesda Categories V or VI (suspicious or malignant cells, positive cytology I) or positive only with Bethesda VI (malignant cells, positive cytology II).
Fluorescence In Situ Hybridization (FISH)
Cytology brushes were processed for FISH analysis as previously published and hybridized using the Urovysion (Abbott Molecular, Des Plaines, Ill) consisting of CEP 3 (orange), CEP 7 (green), CEP 17 (aqua), and 9p21 (p16, gold) [7]. Fluorescent signals were scored on 25–100 cells on 4′,6-diamidino-2-phenylindole (DAPI)-stained slides by using the Cytovision Imaging system attached to a Nikon Eclipse 600 microscope (Applied Imaging, Santa Clara, Calif). All FISH samples were analyzed at the Cytopathology Laboratory of Columbia University Medical Center. The following criteria were applied to select the cells to score: large nuclear size, irregular nuclear shape, patchy DAPI stain, and clustered but not overlapped cells. Signals were recorded as polysomy when there was a gain of two or more chromosomes in at least 5 cells. Homozygous deletion of 9p21 (p16) was considered when both copies were absent in at least 10 cells as per scoring criteria suggested by the manufacturer (Abott Molecular, Des Plaines, Ill), or if there was a heterozygous deletion in at least 6% of the total cells analyzed, the variation that was established by using normal specimens in the laboratory. The FISH abnormalities are reported in order of severity, i.e., if a patient had polysomy, 9p21 deletion, and trisomy 7, they were counted as having a polysomy.
Statistical Analysis
Demographic characteristics between patients with benign and malignant strictures were compared with Fisher’s exact test for categorical variables, and the nonparametric Mann–Whitney U test for continuous variables. Receiver operating characteristic (ROC) curves were then constructed. All statistical analyses were performed with SPSS (IBM SPSS Statistics for Windows, version 22.0. Armonk, NY: IBM Corp.).
Results
Patient Characteristics
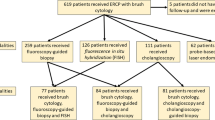
In total, 392 consecutive patients underwent 401 ERCP procedures with tissue obtained for cytology and FISH during the study period (Fig. 1). A total of 120 procedures were ultimately excluded from our analysis. 99 procedures were excluded for lack of adequate follow-up. 19 duplicate procedures were excluded. 2 of the 19 patients had negative FISH results on their first procedure, but had positive FISH results on the subsequent procedure. Because both procedures in these cases occurred within 6 weeks of each other, only the most significant FISH abnormality was included. 2 patients died without a definitive cause before a definitive diagnosis could be made and were excluded. After exclusion of patients with inadequate follow-up and duplicate procedures, 281 patients and procedures were included.
Of the 281 patients that met inclusion criteria, 143 (50.9%) patients were male with a median age of 65 at ERCP (Table 1). 42 patients had a history of PSC, of which 3 were found to have malignancy. 91 patients had an ERCP with stent placement prior to their index procedure. None of these patients had a diagnosis of malignancy when biliary sampling was performed. On average, patients diagnosed with biliary malignancy were significantly older than patients with benign strictures (p = 0.001). Patients with a history of stone disease were significantly more likely to have a benign stricture (p = 0.001). A total of 169 patients had proximal CBD strictures, and 105 patients had distal CBD strictures. Distal CBD strictures were significantly more likely to be malignant than proximal CBD strictures (p = 0.001). Patients with malignant strictures had significantly higher median serum CA 19-9 levels (125.5 U/mL vs. 17.0 U/mL, p = 0.001).
Diagnostic Accuracy
Cytology, when the presence of both suspicious and malignant cells (positive cytology I) was considered positive, had a sensitivity and specificity of 35 and 99%, respectively, for diagnosing malignancy. However, when only the presence of malignant cells was considered a positive (positive cytology II), sensitivity fell to 26% though the specificity increased to 100%. This change in the sensitivity was not statistically significant (35 vs. 26%, p = 0.149). The sensitivities of cytology I in patients with a previous stent placed and those without a previous stent were 25 and 40%, respectively (p = 0.088).
FISH, when considering only polysomy of chromosome 3, 7, and/or 17 as a marker of malignancy, had a sensitivity and specificity of 45 and 99%, respectively. When we included 9p21 heterozygous or homozygous deletions as a positive result, FISH sensitivity increased significantly to 55% while maintaining a specificity of 99% (p = .001). When trisomy 7 or 17 alone was also considered a positive FISH result, the sensitivity increased to 59%, though the specificity decreased to 91%. The combination of cytology I and FISH polysomy or 9p21 deletion (considered positive if either was positive) had the highest sensitivity of 63% with a preserved specificity of 98% (p < 0.001). The PPV and NPV of this strategy were 98 and 73%, respectively (Table 2). The sensitivities of cytology I and FISH polysomy or 9p21 deletion in patients with a previous stent placed and those without a previous stent were 66 and 62%, respectively (p = 0.707).
It is notable that only two false-positive results were included in our study. One patient had a false-positive result using FISH, showing polysomies of chromosomes 7 and 17 in 6.3% of cells analyzed. This patient had adequate follow-up and subsequently underwent a cholecystectomy for chronic cholecystitis. The gallbladder was noted to be perforated and necrotic; however, no dysplasia was noted upon pathological analysis. Although we considered this a false-positive result as the patient had adequate follow-up of > 12 months with resolution of a biliary stricture, detailed evaluation (i.e., ERCP) of the biliary tree has not been performed since the initial sample was obtained. A second patient had a false-positive cytology result, Bethesda Category V—suspicious. FISH testing was negative for polysomy and 9p21 (p16) deletion. This patient had a history of PSC. The initial brushing contained atypical epithelial cells with at least severe dysplasia suspicious for malignancy, but results of subsequent examinations up to two years of follow-up were negative for malignancy or cytologic atypia.
Our cohort included a small number of PSC patients and 3 PSC-associated malignancies. In patients with PSC, a sensitivity for cytology could not be calculated as there were true positive cytology results in PSC patients. FISH polysomy and 9p21 deletion had a sensitivity and specificity of 33.3 and 97.4%, respectively. Of the 6 patients with a CA 19-9 > 129 U/mL, 1 developed CCA in our cohort. In addition, none of the patients classified as benign PSC with an elevated CA 19-9 had aneuploidy.
Abnormalities Identified by FISH
A total of 102 (36%) patients in the study had at least one abnormal FISH result (Table 3). Of these patients with abnormal FISH results, 83 (81%) of these patients had malignancies. Sixty-two (22%) patients had FISH results showing polysomy of chromosome 3, 7, and/or 17, of which 61 (98%) had malignancy. The most common abnormality observed was polysomy, but 9p21 (p16) deletion alone was observed in 19.3% of all malignant cases (50.0% were homozygous, and 50.0% were heterozygous deletions). Though trisomy 7 was observed in 24 of 102 (23.5%) of cases with FISH abnormalities, only 6 of 24 (25%) of these cases were malignant.
Yield of Additional Diagnostic Modalities in Cytology-Negative Cases of Malignancy
We also evaluated the added value of additional sampling methods, such as EUS-FNA, or cholangioscopic biopsies in patients with cytology-negative strictures. 88 patients had cytology-negative malignant biliary strictures. 60 of 88 (68%) had a Bethesda Category III (atypical) result, 24 of 88 (27%) had a Bethesda Category II (benign) result, 3 of 88 (3%) had a Bethesda Category I (non-diagnostic) result, and only 1 of 88 (1%) had a Bethesda Category IV (neoplastic) result.
There were 69 patients with distal strictures and negative cytology. In this cohort, 35 patients underwent EUS and 28 were found to have malignancy. In this population of patients who underwent testing by FISH and EUS-FNA, FISH alone was diagnostic in 3 (10.0%), EUS-FNA alone in 18 (60.0%), and both were positive in 7 (23.3%) cases. The sensitivity and NPV of FISH and EUS-FNA in the entire cohort (in an intention to diagnose analysis including patients who had only one diagnostic study) were 77.8 and 70.6% compared to 37.8 and 46.2% for FISH alone (p = 0.001) (Table 4). When only considering patients who had additional sampling done in addition to FISH and cytology, the sensitivity and NPV of FISH and EUS-FNA were 93.3 and 71.4% compared to 33.3 and 20.0% for FISH alone (p = 0.001).
There were 157 patients with proximal strictures with negative cytology. Among patients with proximal biliary strictures and a negative cytology result who were found to have malignancy (n = 43), 25 (58.1%) underwent both FISH and cholangioscopic biopsies (CBx). In this population of indeterminate proximal strictures, FISH alone was diagnostic in 7 (28.0%), CBx alone in 7 (28.0%), and both were positive in 5 (20.0%) cases. In the entire cohort of patients with cytology-negative proximal strictures, the sensitivity and NPV of FISH and CBx were 67.4 and 89.0% compared to 51.2 and 84.3% for FISH alone (p = 0.133). When only considering patients who had additional sampling done in addition to FISH and cytology, the sensitivity and NPV of FISH and CBx were 76.0 and 89.3% compared to 48.0 and 79.4% for FISH alone (p = 0.05).
Discussion
For both technical and biological reasons, the diagnosis of malignancy in bile duct strictures remains difficult. Although cytological brushings are widely available and have a specificity ranging from 87 to 100%, one cannot rely on this modality alone due to low sensitivities of 4–60% [3, 8]. FISH has been shown to add considerable value to cytology, increasing the sensitivity while maintaining a comparable specificity to cytology alone when these two modalities are used together [3, 5, 7,8,9,10,11,12,13,14, –15].
This study presents one of the largest cohorts using FISH for the diagnosis of malignancy in biliary strictures. Perhaps the clinically most important finding was the confirmation that both FISH polysomy and the addition of 9p21 heterozygous or homozygous deletion detected in biliary brush specimens have a specificity of 98–100%. Overall, this high specificity provides strong evidence for considering a positive FISH result sufficient for the diagnosis of biliary malignancy. However, an important caveat has to be made for PSC. Our cohort contained relatively few PSC patients, making significant analysis difficult. Prior studies focused on this population have shown FISH abnormalities detected in patients with pre-malignancy or inflammation harboring these aneuploidies [16, 17].
Our study also shows that FISH has a significantly higher diagnostic yield than cytology alone. While the sensitivities of FISH (polysomy) and cytology were not significantly different, the inclusion of 9p21 deletion as a positive FISH result resulted in a significantly higher sensitivity. The sensitivity of the combination of cytology and FISH polysomy or polysomy and 9p21 deletion was significantly higher than sensitivity of cytology alone. Our results are comparable to sensitivities and specificities observed in prior studies at other institutions, and we summarized the characteristics of these studies in Table 5 for comparison [3, 5, 7, 8, 11,12,13,14,15]. We also compared the sensitivity of cytology in patients with a previous biliary stent placement and without, but found no significant difference. The presence of a stent can increase the likelihood of observing reactive atypia and has been previously studied as a cause of false-negative results in endoscopic brush cytology [18].
Although many other studies included trisomy 7 in their definitions of positive FISH results, our data (like others) showed a decrease in specificity by 10% when we included this as an indication of malignancy [3, 11,12,13]. In our practice, trisomy 7 is considered an equivocal result and is not sufficient on its own for diagnosis. Trisomy 7 has been previously shown to be prevalent in PSC-associated non-malignant strictures and due to the low overall specificity, and the possibility of this aneuploidy occurring in benign disease, was not considered a positive result for our purposes [3, 19].
For those patients with cytology-negative malignancies, the added benefit of FISH and complimentary CBx or EUS-FNA was examined. CBx showed a borderline significant benefit when compared to FISH in the entire cohort of cytology-negative proximal biliary strictures. EUS-FNA was found to have significant added benefit in the diagnosis of distal biliary strictures. Although only 61% of all patients had either EUS-FNA or CBx, these data would suggest that the evaluation of distal biliary strictures should start with brush cytology and EUS-FNA and specimens should be retained for FISH analysis in negative cases. On the other hand, for proximal strictures we would recommend cytology and FISH upfront and reserve CBx for those cases where a diagnosis is not established.
There are several limitations to this study, which may impact the generalized conclusions from the results. First, 25% of all procedures screened for inclusion were excluded from the subject population because they lacked adequate follow-up. Also, recent works have suggested somewhat higher sensitivity with the use of an alternative set of FISH probes and it is conceivable that a few FISH-negative cases could be identified by the use of these additional loci [5]. There were also a relatively small number of PSC patients (42 of 279; 15%) albeit the rate of cholangiocarcinoma in this population is consistent with the previously reported rate (5–36%) [20].
In summary, our results support the use of FISH (defined as positive by either CEP 3,7,17 polysomy and/or heterozygous or homozygous p16 deletion)) as sufficient for the diagnosis of cancer in non-PSC patients. FISH clearly increases the diagnostic yield of routine cytology without compromising the specificity in a primarily non-PSC-enriched population and does not require any additional procedures. We would advocate for a sequential analysis of specimens, with retention of brush specimens at all sampling procedures for FISH. Importantly, FISH specimens can be stored for several days. Therefore, our algorithm for distal strictures would be cytology/EUS-FNA first followed by FISH in negative cases and cytology/FISH first in proximal strictures followed by cholangioscopy in negative cases. However, prospective studies, incorporating cost analyses, will be needed to validate this approach.
Abbreviations
- AUC:
-
Area under the curve
- CA:
-
Cancer antigen
- CBD:
-
Common bile duct
- CBx:
-
Cholangioscopic biopsy
- CEP:
-
Chromosome enumeration probed
- EUS-FNA:
-
Endoscopic ultrasound-fine needle aspiration
- FISH:
-
Fluorescence in situ hybridization
- NPV:
-
Negative predictive value
- PPV:
-
Positive predictive value
- PSC:
-
Primary schlerosing cholangitis
- ROC:
-
Receiver operating characteristic
References
Shaib YH, Davila JA, McGlynn K, et al. Rising incidence of intrahepatic cholangiocarcinoma in the United States: a true increase? J Hepatol. 2004;40:472–477.
Van Beers BE. Diagnosis of cholangiocarcinoma. HPB (Oxford). 2008;10:87–93.
Moreno Luna LE, Kipp B, Halling KC, et al. Advanced cytologic techniques for the detection of malignant pancreatobiliary strictures. Gastroenterology. 2006;131:1064–1072.
Renshaw AA, Madge R, Jiroutek M, Granter SR. Bile duct brushing cytology: statistical analysis of proposed diagnostic criteria. Am J Clin Pathol. 1998;110:635–640.
Barr Fritcher EG, Voss JS, Brankley SM, et al. An optimized set of fluorescence in situ hybridization probes for detection of pancreatobiliary tract cancer in cytology brush samples. Gastroenterology. 2015;149:1813.e1–1824.e1.
Barr Fritcher EG, Voss JS, Jenkins SM, et al. Primary sclerosing cholangitis with equivocal cytology: fluorescence in situ hybridization and serum CA 19-9 predict risk of malignancy. Cancer Cytopathol. 2013;121:708–717.
Gonda TA, Glick MP, Sethi A, et al. Polysomy and p16 deletion by fluorescence in situ hybridization in the diagnosis of indeterminate biliary strictures. Gastrointest Endosc. 2012;75:74–79.
Kipp BR, Stadheim LM, Halling SA, et al. A comparison of routine cytology and fluorescence in situ hybridization for the detection of malignant bile duct strictures. Am J Gastroenterol. 2004;99:1675–1681.
Brugge W, Dewitt J, Klapman JB, et al. Techniques for cytologic sampling of pancreatic and bile duct lesions. Diagn Cytopathol. 2014;42:333–337.
Layfield LJ, Ehya H, Filie AC, et al. Utilization of ancillary studies in the cytologic diagnosis of biliary and pancreatic lesions: the Papanicolaou Society of Cytopathology Guidelines. Cytojournal. 2014;11:4.
Barr Fritcher EG, Kipp BR, Halling KC, et al. A multivariable model using advanced cytologic methods for the evaluation of indeterminate pancreatobiliary strictures. Gastroenterology. 2009;136:2180–2186.
Smoczynski M, Jablonska A, Matyskiel A, et al. Routine brush cytology and fluorescence in situ hybridization for assessment of pancreatobiliary strictures. Gastrointest Endosc. 2012;75:65–73.
Nanda A, Brown JM, Berger SH, et al. Triple modality testing by endoscopic retrograde cholangiopancreatography for the diagnosis of cholangiocarcinoma. Therap Adv Gastroenterol. 2015;8:56–65.
Salomao M, Gonda TA, Margolskee E, et al. Strategies for improving diagnostic accuracy of biliary strictures. Cancer Cytopathol. 2015;123:244–252.
Chaiteerakij R, Barr Fritcher EG, Angsuwatcharakon P, et al. Fluorescence in situ hybridization compared with conventional cytology for the diagnosis of malignant biliary tract strictures in Asian patients. Gastrointest Endosc. 2016;83:1228–1235.
Barr Fritcher EG, Kipp BR, Voss JS, et al. Primary sclerosing cholangitis patients with serial polysomy fluorescence in situ hybridization results are at increased risk of cholangiocarcinoma. Am J Gastroenterol. 2011;106:2023–2028.
Bangarulingam SY, Bjornsson E, Enders F, et al. Long-term outcomes of positive fluorescence in situ hybridization tests in primary sclerosing cholangitis. Hepatology. 2010;51:174–180.
Logrono R, Kurtycz DF, Molina CP, Trivedi VA, Wong JY, Block KP. Analysis of false-negative diagnoses on endoscopic brush cytology of biliary and pancreatic duct strictures: the experience at 2 university hospitals. Arch Pathol Lab Med. 2000;124:387–392.
Levy MJ, Baron TH, Clayton AC, et al. Prospective evaluation of advanced molecular markers and imaging techniques in patients with indeterminate bile duct strictures. Am J Gastroenterol. 2008;103:1263–1273.
Barr Fritcher EG, Kipp BR, Slezak JM, et al. Correlating routine cytology, quantitative nuclear morphometry by digital image analysis, and genetic alterations by fluorescence in situ hybridization to assess the sensitivity of cytology for detecting pancreatobiliary tract malignancy. Am J Clin Pathol. 2007;128:272–279.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brooks, C., Gausman, V., Kokoy-Mondragon, C. et al. Role of Fluorescent In Situ Hybridization, Cholangioscopic Biopsies, and EUS-FNA in the Evaluation of Biliary Strictures. Dig Dis Sci 63, 636–644 (2018). https://doi.org/10.1007/s10620-018-4906-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-018-4906-x