Abstract
Background
Gastric food residue frequently is observed on endoscopy despite fasting.
Aims
To delineate factors promoting endoscopic food retention in the stomach.
Methods
Two series of analyses were performed. Magnitudes of retained food in 834 patients from an endoscopy database were related to obstructive versus non-obstructive etiologies and gastric emptying findings. Emptying delays in 619 patients from a scintigraphy database were associated with endoscopic food retention, gastroparesis etiologies, and medications that modify gastric transit.
Results
On endoscopy, 310 (37 %) had large, 338 (41 %) showed medium, and 103 (12 %) exhibited small amounts of retained food in the stomach. Of 433 patients with definable etiologies of food retention, 106 (24 %) had obstructive causes. One hundred three of 327 (31 %) with non-obstructive conditions underwent scintigraphy showing mean 52 ± 29 % 4-h retention. From the scintigraphy database, 164/619 patients (26 %) with delayed emptying exhibited food retention on endoscopy. Four-hour scintigraphic retention was greater with versus without retained food (41 ± 25 vs. 32 ± 22 %, P < 0.001). Retained food occurred more frequently with postsurgical (28/69, 41 %) versus diabetic (33/139, 24 %) and idiopathic (65/294, 22 %) gastroparesis (P = 0.006). Opiate use was more prevalent with increasing food retention (P = 0.02), while other medications that delay or accelerate emptying did not relate to retained food.
Conclusions
Gastric food retention has obstructive and non-obstructive causes, and is found in one-quarter of gastroparesis, especially postsurgical cases. Gastric emptying delays correlate with amounts of retained food on endoscopy. Retention is influenced by opiates, but not other medications. These analyses delineate pathogenic factors promoting gastric food retention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Undigested food residue often is observed in the stomach during diagnostic upper endoscopy; however, little investigation has focused on its development. Gastric food retention has been mentioned in review articles; however, it was not discussed in a recently published societal guideline on the role of endoscopy in patients with gastroduodenal obstruction and upper-gut dysmotility syndromes [1, 2]. Other publications concentrating on endoscopic findings in gastroparesis describe mucosal injury patterns in the esophagus, stomach, and duodenum, but do not mention retained food [3, 4]. One investigation was devoted to retained food material in those with prior gastric surgery, noting a prevalence of 19 % in these patients compared to 0.3 % in a control population [5]. A subset of patients with food retention exhibit phytobezoars, organized masses of predominantly vegetable residue; however, this finding is rare in most large series [6]. Most phytobezoars have been reported in older studies in association with surgery for peptic ulcer disease, usually with performance of vagotomy [7–12]. Other less common causes of bezoars include diabetes and neuromuscular diseases such as myotonic dystrophy [6, 13–15].
Factors involved in the pathogenesis of gastric food retention have not been delineated. As many cases occur after gastric surgery with vagotomy suggests an important role for delayed gastric emptying, but attempts to attribute bezoar formation to impaired motor function have yielded conflicting results. Older studies reported normal gastric emptying in postsurgical patients with versus without bezoars, using non-standardized scintigraphic and non-scintigraphic methods (e.g., acetaminophen absorption) [7, 16]. However, others noted delayed emptying in postsurgical and non-operated patients with bezoars using fluoroscopic and other techniques [9, 11]. Nevertheless, some clinicians consider gastric food retention equivalent to delayed gastric emptying as evidenced by recent reports diagnosing acute gastroparesis based on endoscopic observations of food residue in the stomach days to weeks after cardiac ablation for atrial fibrillation [17, 18]. A standardized method to quantify solid-phase gastric emptying was proposed in 2000 and was advocated by the Neurogastroenterology and Motility Society and Society of Nuclear Medicine in 2008 [19, 20]. Relations of gastric food retention to consensus-adopted measures of gastric emptying have not been investigated, and assessments of medical and surgical disorders and medications contributing to its development have not been performed.
The main objective of this retrospective investigation was to correlate the prevalence and degree of food retention on upper endoscopy with underlying diseases, gastric emptying rates, and medication use patterns. Separate databases were accessed to address this aim from two different perspectives. Information gleaned from an endoscopy database included amounts of food residue retained in the stomach as well as the presence of any gastroduodenal obstruction responsible for impaired gastric evacuation. Endoscopy findings were related to other parameters from the electronic medical records to correlate food retention with degrees of gastric emptying delay using standardized scintigraphic methods [19]. A nuclear medicine database was accessed to identify patients with delayed gastric emptying who also had undergone endoscopy. The presence and degree of emptying delay was associated with endoscopic findings, etiologies of gastroparesis, and use of medications that slow and accelerate gut transit. These analyses were designed to (1) characterize the potential diagnostic importance of retained food as a measure of delayed gastric emptying and (2) form a foundation for studies on the pathogenesis of gastric food retention and on management approaches to this condition.
Methods
Patient Populations
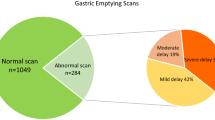
Information relating to patients undergoing testing from January 1, 2007, through September 1, 2012, from two clinical databases was accessed. Seven hundred fifty-one patients were retrospectively identified as having retained food residue in the stomach from a search of the Provation endoscopy database in the Medical Procedures Unit using the key words upper GI endoscopy, food retention, and gastroparesis. Food retention was quantified by the endoscopist by the menu options small, medium, and large. When no qualifier was selected, food retention was classified as undefined for these analyses. Six hundred nineteen patients were retrospectively identified as having delayed gastric emptying defined as >10 % retention of a 99mTc-sulfur colloid-labeled low-fat egg substitute meal from a search of the Nuclear Medicine database of procedures performed at this institution [19]. Two- and 4-h retention values were acquired and gastric emptying delays were defined as mild (10–20 % 4-h retention), moderate (21–35 % 4-h retention), and severe (>35 % 4-h retention) [21]. All patients from the Nuclear Medicine database had undergone endoscopy within 6 months of scintigraphic testing.
This investigation was approved by the University of Michigan Health System Institutional Review Board, which granted a waiver of informed consent to access the relevant databases.
Data Acquisition and Comparisons
Findings from the two databases were included in several analyses to define the relation of gastric food retention to a range of clinical factors. Additional clinical data were acquired by searching the CareWeb and MiChart electronic medical record systems. Patients from the endoscopy database were stratified into those without or with luminal obstruction based on review of endoscopic, radiographic, or surgical reports. The relation of mechanical obstruction to amounts of gastric food retention was defined. Obstructions were further characterized as gastric, duodenal, more distal small intestinal, or undefined. Percentages of patients from the endoscopy database with retained food who also showed scintigraphic delays in gastric emptying were calculated. Mean 2- and 4-h gastric retention values and percentages of patients with mild, moderate, and severe gastric emptying delays were determined. Some scintigraphic studies performed on patients in the endoscopy database were performed at outside institutions; thus, not all studies included 4-h retention values. These findings were complemented by characterizations of amounts of retained food among patients from the scintigraphy database of patients with delayed emptying. The prevalence and amounts of food retention also were related to the presence of severe versus mild–moderate gastric emptying delays. Mean 4-h scintigraphic retention values were compared in those with large, medium, and small amounts of retained food.
Endoscopic food retention was related to other factors. Demographic factors including sex and age at the time of endoscopic or scintigraphic testing were related to the presence or absence of endoscopic food retention among patients from the scintigraphy database. Etiologies of gastric emptying delays in patients from the Nuclear Medicine database were defined by the referring provider as diabetic, idiopathic, postsurgical, or undefined. Operations considered responsible for postsurgical gastric emptying delays included fundoplication, bariatric, esophagectomy, distal gastric resection, vagotomy, and undefined. Medications that delay gastric emptying including opiates, calcium channel antagonists (nifedipine, diltiazem, verapamil, amlodipine), anticholinergics (hyoscyamine, dicyclomine, scopolamine, oxybutynin, solifenacin), restless legs syndrome treatments (ropinirole, pramipexole), and tricyclic agents (amitriptyline, nortriptyline, desipramine, imipramine) were determined for each patient. Furthermore, durations of opiate use were stratified into 1–12 and >12 months before endoscopy from examination of outpatient notes to attempt to characterize chronicity of narcotic use prior to documenting retained food on endoscopy. Similarly, medications that accelerate gastric emptying (metoclopramide, erythromycin, domperidone, pyloric botulinum toxin injection within the past 6 months) were also ascertained.
Statistical Analyses
Data are expressed as mean ± SD or as number (N) with percentage (%). Chi-squared testing was employed to determine relations of gastric food retention to other parameters (severe versus mild–moderate gastric emptying delays, female sex, opiate use, use of other medications that delay gastric emptying, use of medications that accelerate gastric emptying, gastroparesis etiology), to compare relations of amounts of endoscopic retained food with other parameters (luminal obstruction, severe scintigraphic gastric emptying delays, female sex, use of other medications that delay gastric emptying, use of medications that accelerate gastric emptying, gastroparesis etiology). Two-tailed Student’s t testing was performed to compare endoscopic food retention across 4-h scintigraphic gastric retention rates and patient age. Single-factor analysis of variance (ANOVA) was employed to relate amounts of food retention to 4-h gastric retention values and patient age. Multivariate logistic regression was performed to define the relations of predictive variables (female sex, patient age >50 years, severe gastric emptying delays, postsurgical gastroparesis etiology, opiate use, use of other delaying medications, use of accelerating medications) to endoscopic retention of food residue. Statistical significance was defined by P values of <0.05.
Results
Prevalence of Gastric Food Retention and Relation to Mechanical Obstruction
The prevalence of varying degrees of gastric food retention from the endoscopy database was quantified in the group overall and in relation to the presence of mechanical obstruction. Amounts retained were reported as large in 310 (37 %), medium in 338 (41 %), small in 103 (14 %), and undefined in 83 (10 %) of 751 patients (Fig. 1). Medical record documentation was adequate to confirm the presence or absence of mechanical obstruction in 433 patients. Of these, 106 (24 %) had a luminal obstruction including 66 with gastric outlet obstruction, 24 with duodenal obstruction, 4 with distal small bowel obstruction, and 12 with an undefined site of obstruction. Patients with underlying obstructive causes were more likely to exhibit large amounts of retained food residue versus those with non-obstructive conditions (Table 1) (P < 0.001).
Relation of Gastric Food Retention to Gastric Emptying
The relation between gastric food retention and gastric emptying was assessed in the two databases. One hundred three of 327 (31 %) with non-obstructive conditions from the endoscopy database underwent gastric scintigraphy, with 4-h retention measured in 43 patients. Seventy-six of these 103 patients (74 %) exhibited gastric emptying delays with mean 2-h retention of 79 ± 20 % and mean 4-h retention of 52 ± 29 %. Emptying impairments were severe (>35 % 4-h retention) in 26 (60 %), moderate (21-35 % 4-h retention) in 8 (19 %), and mild (10–20 % 4-h retention) in 9 (21 %) of 43 patients with 4-h measurements.
One hundred sixty-four of the 619 patients (26 %) in the scintigraphy database with delayed gastric emptying exhibited gastric retention of food residue on endoscopy. Of these, amounts retained were large in 53 (9 % of total, 32 % with retention), medium in 66 (11 % of total, 40 % with retention), small in 38 (6 % of total, 23 % with retention), and undefined in 7 (1 % of total. 4 % with retention) patients (Fig. 2). Prevalence of gastric food retention was higher among 233 patients with severe emptying delays (>35 % 4-h retention) versus those with mild to moderate delays (P < 0.001) (Table 2). When comparing amounts of food retention against 4-h scintigraphic retention rates, there were trends to greater rates of large versus medium or small amounts retained among those with >35 versus ≤35 % 4-h retention (P = 0.06). Mean 4-h gastric retention showed positive relation to retained food on endoscopy being 41 ± 25 % among all food retainers versus 32 ± 22 % without food retention (P < 0.001) (Fig. 3). However, 4-h retention values were similar for large (46 ± 26 %) versus medium (38 ± 23 %) versus small (40 ± 25 %) amounts of food retention (P = 0.19).
This graph plots 4-h gastric retention rates on scintigraphic assessments of gastric emptying in relation to retained food on endoscopy. Mean 4-h retention rates were higher with gastric food retention compared to those without visible food residue (P < 0.001). However, 4-h gastric retention values were similar in those with large, medium, and small amounts of retained food (P = 0.19)
Relation of Gastric Food Retention to Other Factors
Demography
Gastric food retention was related to patient sex and age using data from the scintigraphy database. Among all patients, 72 % were women. Percentages who were female were similar in those with versus without endoscopic food retention (P = 0.46) (Table 3). Likewise, female sex distribution was not different in those with large, medium, and small amounts of food retention (P = 0.41). Patient age was nearly identical among those with versus without retained gastric food (P = 1.00). Similarly, age did not vary between those with large, medium, or small amounts of food retention (P = 0.45).
Etiologies
Retained food on endoscopy was related to gastroparesis etiologies using data from the scintigraphy database. One hundred thirty-nine (22 %) had underlying diabetes felt to be pathogenic of emptying delays, while 294 (47 %) had idiopathic disease, and 69 (11 %) had undergone prior gastroesophageal surgery believed to represent the cause of gastroparesis. Operations leading to gastroparesis included fundoplication for gastroesophageal reflux in 27, distal gastric resection in 15, bariatric surgery in 12, esophagectomy in 12, vagotomy with pyloromyotomy in 1, and undefined in 2 patients. Food retention was observed more often with postsurgical versus diabetic and idiopathic gastroparesis (P = 0.006) (Table 4). However, percentages of patients with medium or large versus small amounts of retained food were similar for diabetic, idiopathic, and postsurgical cases (P = 0.28).
Medication Use Profiles
Endoscopic food retention was related to use of opiates and other medications known to delay gastric emptying. Opiate use was reported by 204/619 patients (33 %) in the scintigraphy database. Opiate use >12 months in duration was noted for 75/204 patients (37 %) and 1–12 months for 72/204 patients (35 %). Durations of opiate intake could not be defined for 57/204 patients (28 %). Patients with retained gastric food more often used opiates than those without food retention (P = 0.04), with progressive increases in rates of opiate use from small to medium to large amounts of retained food (P = 0.03) (Table 5a). In contrast, use of other medications that delay gastric emptying (calcium channel antagonists, anticholinergics, restless legs treatments, tricyclics) was similar in those with versus without food retention (P = 0.92). In fact, use of other delaying agents was lower with retention of large versus medium or small amounts of food residue (P = 0.03).
Food retention on endoscopy also was related to use of medications that stimulate gastric emptying from the scintigraphy database. Overall, 170/619 (27 %) of patients used prokinetic agents. Rates were similar among patients with versus without retained food (P = 0.92) (Table 5b). Likewise, there were no differences in stimulatory medication use depending on retention of large versus medium versus small amounts of food retention (P = 0.86). When individual prokinetic drugs were examined, no differences in use of metoclopramide (P = 0.78), erythromycin (P = 1.00), domperidone (P = 0.10), or pyloric botulinum toxin injection (P = 0.55) were noted in those with versus without food retention.
Multivariate Logistic Regression to Define Predictors of Endoscopic Food Retention
Multivariate analysis was performed to identify factors predictive of gastric food retention on endoscopy (Table 6). Factors shown to confer an increased risk of retained food included severe gastric emptying delay (>35 % 4-h retention) (P = 0.001), postsurgical gastroparesis (P = 0.01), and opiate use (P = 0.03), while female sex, age >50 years, and use of other medications that delay or accelerate gastric emptying did not relate to food retention (P = NS).
Discussion
These analyses represent the most comprehensive assessment of factors responsible for gastric retention of food residue detected on upper gastrointestinal endoscopy. Complementary findings from large endoscopy and scintigraphy databases defined roles for delayed gastric emptying, mechanical obstruction, gastroparesis etiologies, and medication use profiles in relation to retained food in the stomach.
Findings from this study show a close association of retained gastric food residue to delays in gastric emptying. This relationship has not always been observed in the literature with some reports noting normal emptying in patients with postsurgical etiologies [7, 16]. However, these older studies had smaller sample sizes and used non-standardized methods to quantify emptying delays. Nearly three-quarters of patients with retained food from the endoscopic database in this study exhibited delays, which were mostly characterized as severe (>35 % 4-h retention). The finding of normal emptying in the other patients may be secondary to several factors. The low-fat digestible meal consumed during gastric scintigraphy likely is handled differently than the indigestible meal components that make up the retained food residue; thus, the emptying scan may not be adequately sensitive in some cases. This is analogous to the observed incomplete correlations observed with gastric emptying delays measured by scintigraphy versus indigestible wireless motility capsules [22]. Alternatively, this may merely reflect the well-described inherent intrasubject variability of emptying rates on serial measurements or may be secondary to temporary discontinuation of opiates prior to nuclear medicine testing [23]. Nevertheless, this strong association suggests that gastric scintigraphy may not be needed to document emptying impairments in patients with non-obstructive causes of gastric food retention on endoscopy. This issue warrants consideration by a panel of experts in future consensus documents on management of gastric emptying delays.
Conversely, only one-quarter of those with delayed emptying had associated food retention on endoscopy. Not surprisingly, prevalence of retained food was higher among patients with severely delayed gastric emptying. Furthermore, amounts of food retained trended higher with severe emptying delays. These findings suggest that most patients with gastroparesis are ultimately able to clear their stomachs of meal residue. It is not known if there was different dietary intake or if there were different mechanisms of gastric dysfunction in those with and without retained food. However, our observations are consistent with the interpretation that the absence of endoscopic food retention is not equivalent to normal gastric emptying.
The sample size of this investigation also afforded the capability to characterize different etiologies of endoscopic food retention in the stomach. On the endoscopic database, roughly one-quarter of patients were found to have a malignant or benign obstructive cause of retained food. In the majority of cases, the blockage was defined during diagnostic endoscopy although a small number of cases were a consequence of a downstream obstruction. Examination of the scintigraphy database permitted determination of which gastroparesis etiologies showed the greatest likelihood for gastric food retention. Rates were greatest in patients with postsurgical gastroparesis. Most of these individuals underwent either vagotomy or resection of the distal stomach—the region responsible for trituration of poorly digestible food components. From a pathophysiologic standpoint, this observation suggests the importance of vagal integrity in preventing this operative complication. Retained food was less prevalent with other causes, but was seen in similar percentages of patients with gastroparesis of diabetic versus idiopathic etiology. In other studies, diabetics with gastroparesis exhibit greater evidence of vagal impairment than patients with idiopathic disease [24, 25]. Thus, the observation of similar rates in these two disease etiologies suggests that food retention may not be vagally mediated in non-surgical cases.
The last series of analyses provided important information on the abilities of selected medications to induce gastric food retention. It is protocol at our institution to discontinue medications that delay or accelerate gastric emptying for at least 72 h before scintigraphic measurement when possible. Thus, the observation that opiate use was associated with food retention suggests that most of the residual material was chronic in nature, persisting within the gastric lumen for prolonged periods of uncertain duration. Additional analyses suggested that more than one-third of patients had been on opiates for greater than one year. It is likely this number is even higher as many patients were referred from outside institutions for care just prior to endoscopic and scintigraphic testing; we do not have detailed records from these other hospitals regarding medication use profiles. The mechanisms by which opiates promote food retention are unknown, but may involve local actions on the stomach and/or more central effects. Interestingly, other medications that slow gastric transit did not promote food retention in the stomach even though many could not be stopped prior to scintigraphic testing (e.g., calcium channel antagonists for hypertension, tricyclic agents for depression or pain control). Less than one-third of patients were given therapies to promote gastric evacuation despite documented emptying impairments. This value is lower than reported for multicenter databases that report prokinetic usage in 50–70 % of gastroparesis [26]. Furthermore, prokinetic use was similar in those with and without gastric food retention. However, no systematic assessment of symptoms was performed for this retrospective investigation; it is conceivable that patients in this study had relatively modest symptom severity that did not warrant treatment regardless of the presence of retained food in the stomach.
The observations of this investigation should be distinguished from the existing literature on bezoars. Bezoars are solid, organized masses of indigestible material and are comprised of undigested food (phytobezoar), hair (trichobezoar), medications (pharmacobezoars), or persimmons (diospyrobezoar). Phytobezoars most commonly present as complications of gastric surgery [7–12]. In most cases, the small, medium, and large amounts of retained food reported in this study were poorly organized and did not exhibit a mass-like consistency. Although a small number of endoscopic photos showed appearances consistent with bezoars, standard methods of disrupting bezoars such as mechanical and laser techniques or administering carbonated beverages or enzyme preparations were not employed for any patient in this report [7, 9, 10, 27, 28]. This suggests that bezoars requiring endotherapy or surgery are considerably less common than the less well-organized food collections characterized in this study.
There were limitations to this investigation. Because of its retrospective nature, concerns exist about non-standardized scintigraphic methods recorded on some patients from the endoscopy database as well as incomplete data collection including radiographic and operative findings (in those with obstruction or postsurgical gastroparesis) and medication use profiles. Furthermore, we chose not to examine the much larger endoscopy database cohort without retained food and the much larger scintigraphy database cohort with normal gastric emptying. Thus, important information on what fraction of those without any gastric impairments who are on opiates or other agents that influence motor function cannot be rigorously defined from our analyses. Characterization of food retention relied on qualitative assessments by a large group of endoscopists, who likely had varying definitions of what constituted small, medium, and large quantities of luminal food residue. It would have been desirable to subcategorize diabetics on the basis of glycemic control; however, hemoglobin A1c values drawn within around the time of endoscopic or scintigraphic testing were available only in a small minority of patients. Additionally, our center does not routinely record glucose values prior to endoscopy or scintigraphy; however, it is unlikely that acutely normalizing glycemia prior to testing would have significantly impacted the finding of retained food in most patients. It is probable that the food found in most patients particularly with medium to large amounts retained had been present for days to months and would not quickly empty upon lowering blood sugar values. There may have been differences in duration of fasting prior to gastric scintigraphy (typically performed 8–12 h after the last meal) versus endoscopy (some patients fast up to 20 or more hours before testing). However, all patients avoid solid food intake at least 8 h before endoscopy, so it is unlikely that any cases of food retention resulted from test performance too close to the time of the last meal. Finally, no consistent assessment of symptoms or dietary intake was obtained prior to evaluation. Thus, the clinical consequences of gastric food retention and the potential for dietary management for these individuals cannot be definitively determined.
Nevertheless, we believe our observations have clinical relevance and form a foundation for further investigation. The relation of endoscopy findings to scintigraphy results in the two databases suggest that detection of gastric food retention is specific, but not particularly sensitive for defining delayed gastric emptying. Quantification and characterization of symptoms in gastroparesis patients with endoscopic food retention will determine whether this finding is associated with a distinct clinical presentation compared to individuals without retained food. It should be noted that gastroparesis symptom severity correlates poorly with scintigraphic emptying of the highly digestible egg substitute meal performed at our institution [29]. Furthermore, evaluation of dietary interventions such as strict consumption of low-residue meals will determine whether this disease complication can be managed without medications. Large particle size diets recently have been shown to be beneficial in improving gastric function and reducing symptoms in diabetics with gastroparesis [30, 31]. Additional study may define the relative benefits of different prokinetic agents in evacuating food residue from the stomach.
In conclusion, we have shown that food retention in the stomach may result from mechanical obstruction as well as non-obstructive conditions. Retained food is detected on endoscopy in approximately one-quarter of patients with gastroparesis and is more often seen in individuals with a postsurgical cause of delayed gastric emptying suggesting the presence of selective motor dysfunctions between etiologies that promote this complication. There is a relation of endoscopic food retention with scintigraphically measured gastric emptying delays. Opiate use is strongly associated with retention of food residue in the stomach, suggesting this class of drugs should be used sparingly in these patients. Conversely, intake of other medication classes that delay or accelerate gastric emptying has little impact on this finding. These analyses represent the first detailed discrimination of potential pathogenic factors that promote gastric retention of food residue.
References
Sander R, Frankenberger U. The use of endoscopy in patients with gastrointestinal motility problems. J Clin Gastroenterol. 2001;33:185–190.
ASGE Standards of Practice Committee, Fukami N, Anderson MA, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011;74:13–21.
Parkman HP, Schwartz SS. Esophagitis and gastroduodenal disorders associated with diabetic gastroparesis. Arch Intern Med. 1987;147:1477–1480.
Maddern GJ, Chatterton BE, Collins PJ, Horowitz M, Shearman DJ, Jamieson GG. Solid and liquid gastric emptying in patients with gastro-oesophageal reflux. Br J Surg. 1985;72:344–347.
Watanabe H, Adachi W, Koide N, Yazawa I. Food residue at endoscopy in patients who have previously undergone distal gastrectomy: risk factors and patient preparation. Endoscopy. 2003;35:397–401.
Ahn YH, Maturu P, Steinheber FU, Goldman JM. Association of diabetes mellitus with gastric bezoar formation. Arch Intern Med. 1987;147:527–528.
Tohdo H, Haruma K, Kitadai Y, et al. Gastric emptying and bezoars in Japanese: report of five cases. Dig Dis Sci. 1993;38:1422–1425.
Goldstein HM, Cohen LE, Hagan RO, Wells RF. Gastric bezoars: a frequent complication in the postoperative ulcer patient. Radiology. 1973;107:341–344.
Hewitt AN, Levine MS, Rubesin SE, Laufer I. Gastric bezoars: reassessment of clinical and radiologic findings in 19 patients. Br J Radiol. 2009;82:901–907.
Zamir D, Goldblum C, Linova L, Polychuck I, Reitblat T, Yoffe B. Phytobezoars and trichobezoars: a 10-year experience. J Clin Gastroenterol. 2004;38:873–876.
Brady PG. Gastric phytobezoars consequent to delayed gastric emptying. Gastrointest Endosc. 1978;24:159–161.
Buchholz RR, Haisten AS. Phytobezoars following gastric surgery for duodenal ulcer. Surg Clin North Am. 1972;52:341–352.
Myer GW, Clark RD, Brotman M. Gastric phytobezoar and hypoglycemia: medical management. Cal Med. 1973;118:66–67.
Kuiper D. Gastric bezoar in a patient with myotonic dystrophy. Am J Dig Dis. 1971;16:529–534.
Kirks DR, Szemes GC. Autovagotomy and gastric bezoar. Gastroenterology. 1971;61:96–98.
Calabuig R, Navarro S, Carrio I, Artigas V, Mones J, Puig LaCalle J. Gastric emptying and bezoars. Am J Surg. 1989;157:287–290.
Knopp H, Halm U, Lamberts R, et al. Incidental and ablation-induced findings during upper gastrointestinal endoscopy in patients after ablation of atrial fibrillation: a retrospective study of 425 patients. Heart Rhythm. 2014;11:574–578.
Choi SW, Kang SH, Kwon OS, et al. A case of severe gastroparesis: indigestion and weight loss after catheter ablation of atrial fibrillation. PACE. 2012;35:e59–e61.
Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462.
Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–763.
Abell TL, Bernstein VK, Cutts T, et al. Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil. 2006;18:263–283.
Kuo B, McCallum RW, Koch KL, et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment Pharmacol Ther. 2008;27:186–196.
Rao SS, Camilleri M, Hasler WL, et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil. 2011;23:8–23.
Hasler WL, Coleski R, Chey WD, et al. Differences in intragastric pH in diabetic vs. idiopathic gastroparesis: relation to degree of gastric retention. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1384–G1391.
Gaddipati KV, Simonian HP, Kresge KM, Boden GH, Parkman HP. Abnormal ghrelin and pancreatic polypeptide responses in gastroparesis. Dig Dis Sci. 2006;51:1339–1346.
Parkman HP, Yates K, Hasler WL, et al. Similarities and differences between diabetic and idiopathic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:1056–1064.
Park SE, Ahn JY, Jung HY, et al. Clinical outcomes associated with treatment modalities for gastrointestinal bezoars. Gut Liver. 2014;8:400–407.
Wang YG, Seitz U, Li ZL, Soehendra N, Qiao XA. Endoscopic management of huge bezoars. Endoscopy. 1998;30:371–374.
Pasricha PJ, Colvin R, Yates K, et al. Characteristics of patients with chronic unexplained nausea and vomiting and normal gastric emptying. Clin Gastroenterol Hepatol. 2011;9:567–576.
Olausson EA, Alpsten M, Larsson A, Mattsson H, Andersson H, Attvall S. Small particle size of a solid meal increases gastric emptying and late postprandial glycemic response in diabetic subjects with gastroparesis. Diabetes Res Clin Pract. 2008;80:231–237.
Olausson EA, Storsrud S, Grundin H, Isaksson M, Attvall S, Simren M. A small particle size diet reduces upper gastrointestinal symptoms in patients with diabetic gastroparesis: a randomized controlled trial. Am J Gastroenterol. 2014;109:375–385.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict to interest
None.
Rights and permissions
About this article
Cite this article
Coleski, R., Baker, J.R. & Hasler, W.L. Endoscopic Gastric Food Retention in Relation to Scintigraphic Gastric Emptying Delays and Clinical Factors. Dig Dis Sci 61, 2593–2601 (2016). https://doi.org/10.1007/s10620-016-4173-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4173-7