Abstract
Nonalcoholic fatty liver disease (NAFLD) covers a spectrum of histological lesions ranging from steatosis to a complex pattern with hepatocyte injury and inflammation in an appropriate clinical context. The disease has been artificially dichotomized into NAFL (steatosis) and NASH (steatosis with hepatocellular injury and inflammation), but it is increasingly clear that intermediate patterns may exist. More than NASH, the stage of fibrosis was shown to govern prognosis, and for such evaluation, a liver biopsy of adequate size and width is needed. Like for any other chronic liver diseases, semi-quantitative histologic scores have been proposed. They are not useful in clinical practice but concur to categorize homogeneous group of patients according to their histology. Pediatric NAFLD is a growing concern. While a subgroup of children may harbor different but characteristic histological patterns, most of them display a mixed pattern or features similar to the adults. Today, liver histology is the mainstay for clinical trials. Biopsy is used both for enrollment and for assessing benefit of clinical trials. End points such as reversion of NASH or regression of fibrosis are acceptable but require a clear histological definition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nonalcoholic fatty liver disease (NAFLD) is a clinical-histological syndrome that refers to a spectrum of liver lesion ranging from steatosis (nonalcoholic fatty liver or NAFL) to more complex patterns with lesions of hepatocyte injury and inflammation (nonalcoholic steatohepatitis or NASH) with various degree of fibrosis in the absence of alcohol intake. NAFLD is rapidly increasing worldwide, consistent with the increased prevalence of obesity [1]. In nonalcoholic patients, steatosis and steatohepatitis may be observed in a variety of clinical situations, the most common being liver diseases related to the metabolic syndrome but strictly speaking, the term NAFLD may also apply to other diseases such as HCV infection, drugs, starvation, Wilson’s disease, or other rare conditions where the same histological features may be observed in addition to other etiology-related pathologic lesions [2, 3]. However, and given its high prevalence, the acronyms NAFLD and NASH refer usually to liver diseases associated with metabolic syndrome or its components.
Liver Biopsy in NAFLD: Limitation and Indication
Histopathologic evaluation remains central to all investigations in NAFLD, including clinical trials [4, 5]. However, liver biopsy is an invasive procedure and potentially harmful, carrying a low but real risk of morbidity and extremely low risk of mortality. Thus, and considering the huge number of patients with potential NAFLD, liver biopsy cannot be considered as a screening procedure but should be reserved to selected patients that deserve a case by case assessment with discussion of risks and benefits [6].
Beside the risks of adverse events, liver biopsy may fail because of internal limits to the biopsy procedure itself. As demonstrated for many other chronic liver diseases, the liver is not necessarily uniformly affected and since the volume of a needle biopsy sample represents a very minor fraction of the whole organ, sampling variation is a relevant issue to consider since a too small biopsy can result in substantial misdiagnosis and staging inaccuracy [7, 8]. This assumption should, however, be modulated for NAFLD since, in this context, histological lesions are highly systematized within the lobule focusing systematically on zone 3, at least in the early phases of the disease (Fig. 1). Adequacy of a liver biopsy sample rely on the opinion of the pathologist, but length and diameter of the biopsy are considered as valid surrogates [9]. While a 25-mm length is considered optimal for assessing and quantitating detailed lesion, 15-mm-long biopsy provides robust information [7, 10]. Not only length but also diameter of the core is also to consider. Indeed, narrow-bore needles often transect the lobule making impossible for the pathologist to analyze its various components and difficult to assess architectural distortion. A 16-gauge needle (or larger) is considered adequate [11]. The expertise of the pathologist who does the evaluation is also important to consider in biopsy interpretation [12]. Although expert liver pathologists produce more reproducible reports, general pathologists can perform as good if they are properly trained [13].
The 2012 guidelines from American Association for the Study of Liver Disease (AASLD) recommended to reserve liver biopsy for subjects who will benefit from it. Patients with potentially competing diagnoses and children with either an unclear diagnosis or in whom consideration is being given for medication may also have a biopsy [14]. The European Association for the Study of Liver Disease position statement differed slightly and recommended liver biopsy in all bariatric surgery subjects and as an end point in all clinical trials [15]. Today, despite numerous clinical trials, no single treatment can be recommended to all patients with NASH. In the near future, the place of liver biopsy might be subject to change according to, on one side, the development of new and more potent drugs and, in the other side, the development of accurate noninvasive markers.
As mentioned before, biopsy is recommended if more than one liver disease is suspected. Large biopsy series have documented that up to 5 % of patients with another diagnosed liver disease, such as chronic hepatitis C, autoimmune liver disease ,or primary biliary cirrhosis, had histologic evidence of concurrent steatohepatitis [2, 3].
Nonalcoholic Fatty Liver (NAFL)
It encompasses the larger group of patients which is characterized by steatosis alone or steatosis with mild associated lesions which are not severe enough to be classified into the NASH group.
Steatosis is a result of excess accumulation of triglyceride in the liver. The threshold for considering steatosis as abnormal feature is 5 % of hepatocytes. Steatosis is usually macrovesicular, but may be either purely large droplet or a mixture of small and large droplet (mediovesicular steatosis) (Fig. 1). In macrovesicular steatosis, the lipid vacuole fills nearly the entire hepatocyte, pushing the nucleus to the side. At the extreme end, these cells may look like adipocytes [16]. Mediovesicular steatosis occurs when there are one or more smaller vacuoles in the cytoplasm. These vacuoles are usually easily distinguished from one another and are few enough in number that they could be counted. Microvesicular steatosis is a rare form in which the hepatocyte cytoplasm is replaced by innumerable small vacuoles, giving the cell a foamy appearance. True diffuse microvesicular steatosis is uncommon, but it may occur in a patchy distribution in up to 10 % of NAFLD [17]. The steatosis may be distributed in a distinctly zone 3 (pericentral) centered pattern (Fig. 1) but abundant steatosis can be panacinar, and when resolving, may be irregular evenly throughout the acinus. Rarely steatosis may be localized in zone 1 (characteristic pattern of pediatric NAFLD), and as the disease progresses toward cirrhosis, the steatosis may become more irregularly distributed or may vanish [18].
A simple four scales grading (from 0 to 3) is used for grading steatosis. It takes into account only macro- and/or mediovesicular steatosis and assesses the percentage of hepatocyte decorated by steatotic vacuoles [19]. Normal liver (Grade 0) contains fat in <5 % of hepatocytes, while grade 1 steatosis refer to <33 % steatotic hepatocytes. In grade 2 and 3 steatosis, fat is present in at least 33 or 66 % of hepatocytes, respectively.
Patients with steatosis and no additional features of liver injury may follow a relatively benign clinical course with no increase in liver disease-related mortality compared with the general population of similar age and gender [20]. There are also experimental results suggesting that, in NAFLD, triglyceride accumulation may be protective for hepatocytes from the lipotoxic effects of ectopic fat accumulation [21, 22]. However, a recent meta-analysis suggests that simple steatosis may progress also to fibrosis but at a significantly lower rate than steatohepatitis [23].
There is a significant subgroup of patients with steatosis but with associated mild lesions such as few inflammatory cells or clarified/ballooned hepatocytes of normal size (Fig. 2). Together, these lesions are of too mild intensity to be named NASH. This group has been ignored for long time but may represent a significant proportion of patients. It is commonly accepted to include this lesion into the NAFL group although this question has not been addressed formally. Whether their prognosis is as benign as pure steatosis is unknown. Retrospective studies have shown that some cases may evolve to more severe disease, albeit at a lower rate than those with NASH while some prospective studies have suggested that these lesion may stabilize or even regress [24, 25].
Nonalcoholic Steatohepatitis (NASH)
The relationship between steatosis and steatohepatitis is unclear. Although progression from pure steatosis to steatohepatitis may occur, epidemiologic data support that they are two different entities with occasional shift from one to another and in both directions.
Although the natural history of NAFLD is still incompletely understood, it is clear that those who have the histologic pattern of NASH and advanced fibrosis are at much greater risk of developing end-stage liver disease, liver-related mortality or extra-hepatic mortality than the general population of the same age and sex [12, 20, 26].
As noted above, steatohepatitis is a pattern of liver injury which requires examination of liver tissue. Although several algorithms based on the combination of clinical and biological data have been proposed, there are no noninvasive tests that can be performed to firmly identify patients with steatohepatitis or distinguish steatohepatitis from pure steatosis [27, 28]. Therefore, if there is need to know with certainty whether or not a patient has NASH, a liver biopsy must be performed.
Since the seminal description by Ludwig et al. [29], the histological definition of NASH has changed with time and with pathologists. Now, it is uniformly accepted that two cardinal features: lobular inflammation and liver cell clarification/ballooning, are mandatory features for NASH diagnosis (Fig. 3) [30–32]. These patterns have been best characterized in adult liver, in which the lesions center around the terminal hepatic vein but once fibrosis progresses and parenchymal remodeling occurs, the lesions may lose preferential acinar localization. Several other histologic features may be associated but do not contribute for the diagnosis of NASH.
Inflammation is more often lobular in NASH, typically more prominent than portal inflammation in uncomplicated adult NAFLD. It is made mainly of clusters of mononuclear, but also Kupffer cells, microgranulomas with or without lipid droplets sometimes associated with hepatocyte dropout or apoptotic bodies. Aggregates of neutrophils are rare and become prominent only if many Mallory–Denk bodies are present and numerous. The degree of lobular inflammation is usually mild and when abundant should suggest another or an associated etiology such as alcohol or drug toxicity [30, 33]. Inflammatory foci may gather in zone 3 in early lesion but may be more diffused in advanced diseases. A four tier grading system has been defined by NASH clinical research network (NASH CRN) (from grade 0 to 3) according to the number of inflammatory foci in a given area while a three tier grading (from 0 to 2) is proposed in the SAF scoring system [19, 32].
Some degree of portal inflammation which is not a mandatory feature for NASH might be also recognized. It is usually milder than lobular inflammation. Mononuclear cells are typically predominant with no or limited foci of interface hepatitis. Occasionally, portal inflammation might become prominent [34]. It has been associated with more severe histologic injury and fibrosis in cross-sectional studies, suggesting that portal inflammation may be indicative of a worse prognosis [35].
Ballooning hepatocellular injury is the second key diagnostic feature in steatohepatitis. Ballooned hepatocytes need to display both a clear, flocculent, not vacuolar cytoplasm with a ballooned shape as defined by the loss of sharp angles of the liver cell (Fig. 4). Size may or may not be increased compared to the size of normal hepatocytes. In the NAFLD activity score (NAS), grading of ballooned cells is based mainly on number (none, few, many), while in the SAF score, it is mainly based on size of ballooned cells [19]. A significant increase (at least twice larger than the normal hepatocyte) defines grade 2 ballooning while grade 1 represents ballooned liver cells whose size is approximately the size of normal hepatocyte [32]. A study has shown that using these criteria, diagnosis and semi-quantification of ballooned cells may become very robust between pathologists [13]. In adult NASH, ballooned hepatocytes are most commonly seen in zone 3 where they are often intermixed with perisinusoidal collagen fibers (Fig. 5).
Recent works addressed the nature of ballooned hepatocytes with the use of electron microscopy or immunostaining. Using antibodies against cytokeratin 8/18, the ballooned hepatocytes have significantly reduced staining compared to normal hepatocytes [36]. This immunostaining might help to identify ballooned hepatocytes and distinguish them from steatotic hepatocytes, but it is not used in common practice yet [37]. The pathophysiological triggers of cytoplasmic ballooning are not well understood, but this pattern should be related to damage to the intracellular intermediate filaments generated from metabolism of free fatty acids [36, 38]. Fat accumulation in the endoplasmic reticulum of ballooned hepatocytes has been also observed by electron microscopy [39].
Hepatocyte ballooning and lobular inflammation are both necessary and sufficient features for the diagnosis of NASH in a background of steatotic liver.
Others features of hepatocellular injury may also be observed such as apoptotic bodies, but they are usually sparse and inconstant. Mallory–Denk body may be present but they are less well-formed than in alcoholic hepatitis or alcoholic steatohepatitis and sometimes detected only using p62 or ubiquitin immunohistochemistry [40]. They can be numerous in severe NASH, but a lot of Mallory–Denk bodies may suggest an associated alcoholic or toxic injury. The presence of Mallory–Denk bodies correlates with the histological severity of steatohepatitis and with other markers of progression and fibrosis in NASH [40, 41].
Other histological features such as clear nuclei, microgranulomas, lipogranulomas, megamitochondria, iron in hepatocytes, and reticuloendothelial cells may be observed, but they are not of diagnosis or prognosis value. Isolated arteries observed in zone 3 is a rare feature correlated with advanced fibrosis in NASH [42]. Ductular reaction refers to ductular proliferation at the portal tract interface. In NASH, the extent of ductular reaction is associated with fibrosis [43].
Fibrosis
Fibrosis is a major feature since most studies have shown an impact of stage of fibrosis on overall mortality and liver-related mortality independently, and regardless of the presence or severity of other histologic features [12, 44]. Although NASH is quite always associated with some degree of fibrosis, fibrosis of any stage might also be present in NAFL without features of NASH. The current concept is that, in these cases, fibrosis represents a form of NASH in remission.
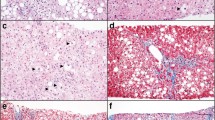
In NAFLD, fibrosis takes on a distinctive pattern. In early lesion, fibrosis begins as a delicate perisinusoidal deposition of collagen fibers in zone 3. In more advanced lesions, collagen fibers may encircle hepatocytes (Fig. 6). Pericellular fibrosis can progress without the development of any appreciable periportal fibrosis for a long time, but commonly, periportal fibrosis may develop. Therefore, a progression of fibrosis has been described by NASH CRN as follows: zone 3 perivenular and perisinusoidal is stage 1 (with a subdivision into 1a and 1b according to the amount of the deposit), and stage 1c is isolated periportal fibrosis; stage 2 includes portal and central fibrosis without bridging fibrosis; stage 3 is bridging fibrosis; and stage 4 is cirrhosis [19]. Even in advanced stages, dense perisinusoidal fibrosis can be a clue to the diagnosis and the dominant feature, especially when diabetes is present. This staging system is universally accepted since it is the most appropriate for NAFLD-associated fibrosis. Portal fibrosis in association with pericentral fibrosis (stage 2) suggests that portal fibrosis is a necessary feature for bridging fibrosis to develop. Since liver biopsy is only a cross-sectional view and series of repeated biopsies are rare, the relevance of this longitudinal scale reminds an open question.
Peculiarities of Pediatric NAFLD
NAFLD is the leading cause of chronic liver disease in children in the USA, with an estimated prevalence of 10–20 % [45]; it is likely to reach epidemic proportions worldwide as rates of obesity and insulin resistance increase among children [46]. Schwimmer et al. [18] were the first to systematically categorize histological features of pediatric NAFLD. In this study, one of the most consistent differences from adults was the distribution of the fat, and the preferential accentuation of portal inflammation and fibrosis around portal tract. This defines a subgroup of pediatric NASH with fatty liver in zone 1 (rather than zone 3), and no zone 3 perisinusoidal fibrosis [18]. However, in other studies, most children with NAFLD show either a typical adult form with predominating lesions in zone 3 or a mixed pattern [47, 48].
Scoring Systems in NAFLD
NAFLD display a continuous spectrum of steatosis, hepatocyte damages, inflammatory and fibrous lesions. Therefore, categorization of NAFLD in two subgroups (NASH, no NASH) is potentially ambiguous and is an oversimplification. Semi-quantitative scoring systems may partially avoid this limit. Scoring systems which have been developed in most chronic liver diseases have been shown useful by increasing reproducibility between pathologists, creating homogenous group of patients according to their histology, and providing an easier way to compare lesions when repeated biopsies are performed. Their main fields of application are clinical trials.
The NAS has been proposed by the NASH CRN and was based on the concept that the necroinflammatory lesions and the stage of fibrosis should be separately evaluated as the former is potentially more reversible than the latter [19]. From the analysis of several set of biopsies, steatosis, lobular inflammation, and ballooning were the lesions that correlated at best with the diagnoses of NASH. Thus, the NAS was created as an unweighted score for steatosis (0–3), lobular inflammation (0–3), and ballooning (0–2). Although the NASH CRN pointed repeatedly that the numeric value should not be considered a replacement of the pathologist’s diagnosis, it was used repeatedly as a criteria for diagnosing NASH and inclusion or exclusion of patients in clinical trials [4, 49, 50]. Since NAS is presumed to mirror disease activity, there is a rationale for expecting a close correlation between an increased NAS and the presence of NASH. Indeed, it was found that the majority of biopsy with a total NAS ≥5 correlated with the diagnosis of definite steatohepatitis, while NASH should be excluded if NAS <3 thus supporting the NAS as a score of activity [51]. Unfortunately, the NAS may not, on its own, provide any long-term prognostic information [26].
The potential explanations of the limitations of NAS are several. Inclusion of steatosis into the NAS might be confusing since it combines, in a global activity score, deleterious features such as liver cell damage and lobular inflammation with steatosis, the pejorative effects of which has not been shown definitively [21, 22]. Second, the weight of each of the three components of the NAS is unequal, with the lower for clarification/ballooning of hepatocytes which is considered as the major prognostic feature.
Another approach is the SAF score that assesses separately the grade of steatosis (S, from S0 to S3), the grade of activity (A from A0 to A4), and the stage of fibrosis (F from F0 to F4) [13, 32]. In the SAF, the activity score is defined by adding semi-quantitative score of lobular inflammation (0–2) and hepatocellular ballooning (0–2). The rationale for this scoring stems directly from its definition, and setting a threshold at 2 for this activity score enables distinguishing confidently quite all cases of NASH when A ≥ 2 [32]. SAF score would simplify comprehension by pathologists and hepatologists. Finally, this scoring can be used for any association of steatosis, fibrosis and activity especially those particular association that cannot be easily classified as NAFLD or NASH: steatosis with spotty lobular inflammation, steatosis and fibrosis but without ballooning injury or lobular inflammation, cirrhosis without steatosis etc. Nevertheless, the clinical and prognostic relevance of the SAF score remains to be shown.
Liver Biopsy in Clinical Trials for NASH
Because of the lack of validated noninvasive marker, clinical trials rely on biopsy both for deciding patient eligibility and for evaluation of the drug effect [50]. Indeed, histological end points are considered as valid surrogate for clinical end point such as mortality but the most relevant histological end points are still a matter of debate [4, 52]. Reduction of fibrosis should be the optimal criteria since fibrosis is the strongest prognostic factor. However, the kinetic of fibrosis regression is hardly compatible with the short delay between pre- and post-treatment biopsy (12–18 months). Assessing fibrosis change as a primary outcome may come at the cost of longer and/or larger trials. Although no change of fibrosis is expected in short time lapse, lack of fibrosis progression is clearly mandatory at least [5]. Sophisticated histological markers of fibrosis dynamic such as deactivation of hepatic stellate cells (as shown by alpha-smooth muscle immunohistochemistry), quantitative evaluation of fibrosis with morphometry, or using an expanded staging system might be relevant for answering the question [12]. However, sampling error might become an issue when using very precise measurement systems.
There have been several recommendations that resolution of NASH is a relevant end point for clinical trials [5, 15, 50]. Indeed, NASH is associated with a substantial increase in the long-term risk of developing cirrhosis and liver-related outcomes [20, 26]. Improvement in the NAS has been used as a surrogate for NASH resolution and often used as one of the end point to determine treatment efficacy in treatment trials. However, the NAS on its own did not provide any long-term prognostic information. Decreased activity as evaluated in the SAF deserves also consideration since it does not include steatosis, but more data are needed to show whether change in the NAS or the SAF is associated with the long-term prognosis of NAFLD. Thus, for the purpose of assessing the long-term prognosis, the focus should be on fibrosis stage while other histologic findings may have importance for understanding disease pathophysiology and predicting short-term disease progression/regression [4].
To date, there is no approved therapy for NASH although some drugs have shown dissociated effect on one or several of the histological components [53–57] or even promising results on regression of NASH and fibrosis [58]. Liver histology and the evaluation of relevant histological end point will be of paramount importance.
Key Messages
-
Liver biopsy is the reference tool for evaluation of NAFLD and to assess the presence of NASH and the stage of fibrosis. Noninvasive markers are urgently needed for clinical practice.
-
NAFLD is typically divided into NAFL (steatosis) and NASH. However, this dichotomous classification is an oversimplification since histology reveals continuous spectrum of lesions from simple steatosis to end-stage cirrhosis.
-
Fibrosis is the major long-term histological prognostic criteria. NASH is considered as the main trigger of fibrosis and a valid surrogate to assess short-term prognosis.
-
To date in clinical trials, histological end points are considered as valid surrogates for clinical outcome. Resolution of NASH is the most reasonable histological end point accessible in a time delay compatible with duration of clinical trials while regression of fibrosis would need longer follow-up.
References
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690.
Bedossa P, Moucari R, Chelbi E, et al. Evidence for a role of nonalcoholic steatohepatitis in hepatitis C: a prospective study. Hepatology. 2007;46:380–387.
Brunt EM, Ramrakhiani S, Cordes BG, et al. Concurrence of histologic features of steatohepatitis with other forms of chronic liver disease. Mod Pathol. 2003;16:49–56.
Kleiner DE, Bedossa P. Liver histology and clinical trials for nonalcoholic steatohepatitis-perspectives from 2 pathologists. Gastroenterology. 2015;149:1305–1308.
Sanyal AJ, Friedman SL, McCullough AJ, Dimick-Santos L. Challenges and opportunities in drug and biomarker development for nonalcoholic steatohepatitis: findings and recommendations from an American Association for the Study of Liver Diseases-U.S. Food and Drug Administration joint workshop. Hepatology. 2015;61:1392–1405.
Nalbantoglu IL, Brunt EM. Role of liver biopsy in nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20:9026–9037.
Bedossa P, Dargere D, Paradis V. Sampling variability of liver fibrosis in chronic hepatitis C. Hepatology. 2003;38:1449–1457.
Ratziu V, Charlotte F, Heurtier A, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128:1898–1906.
Vuppalanchi R, Unalp A, Van Natta ML, et al. Effects of liver biopsy sample length and number of readings on sampling variability in nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009;7:481–486.
Goldstein NS, Hastah F, Galan MV, Gordon SC. Fibrosis heterogeneity in nonalcoholic steatohepatitis and hepatitis C virus needle core biopsy specimens. Am J Clin Pathol. 2005;123:382–387.
Colloredo G, Guido M, Sonzogni A, Leandro G. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. J Hepatol. 2003;39:239–244.
Younossi ZM, Stepanova M, Rafiq N, et al. Pathologic criteria for nonalcoholic steatohepatitis: interprotocol agreement and ability to predict liver-related mortality. Hepatology. 2011;53:1874–1882.
Bedossa P, FLIP Pathology Consortium. Utility and appropriateness of the fatty liver inhibition of progression (FLIP) algorithm and steatosis, activity, and fibrosis (SAF) score in the evaluation of biopsies of nonalcoholic fatty liver disease. Hepatology. 2014;60:565–575.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Am J Gastroenterol. 2012;107:811–826.
Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–384.
Tiniakos DG. Nonalcoholic fatty liver disease/nonalcoholic steatohepatitis: histological diagnostic criteria and scoring systems. Eur J Gastroenterol Hepatol. 2010;22:643–650.
Tandra S, Yeh MM, Brunt EM, et al. Presence and significance of microvesicular steatosis in nonalcoholic fatty liver disease. J Hepatol. 2011;55:654–659.
Schwimmer JB, Behling C, Newbury R, et al. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42:641–649.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321.
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419.
Listenberger LL, Han X, Lewis SE, et al. Triglyceride accumulation protects against fatty acid-induced lipotoxicity. Proc Natl Acad Sci. 2003;100:3077–3082.
Yamaguchi K, Yang L, McCall S, et al. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology. 2007;45:1366–1374.
Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643–654.
Pais R, Charlotte F, Fedchuk L, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013;59:550–556.
McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015;62:1148–1155.
Ekstedt M, Franzen LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873.
Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001;121:91–100.
Campos GM, Bambha K, Vittinghoff E, et al. A clinical scoring system for predicting nonalcoholic steatohepatitis in morbidly obese patients. Hepatology. 2008;47:1916–1923.
Ludwig J, Viggiano TR, McGill DB, Oh BJ. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438.
Brunt EM. Pathology of nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol. 2010;7:195–203.
Yeh MM, Brunt EM. Pathological features of fatty liver disease. Gastroenterology. 2014;147:754–764.
Bedossa P, Poitou C, Veyrie N, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–1759.
Sakhuja P. Pathology of alcoholic liver disease, can it be differentiated from nonalcoholic steatohepatitis? World J Gastroenterol. 2014;20:16474–16479.
Brunt EM, Kleiner DE, Wilson LA, et al. Portal chronic inflammation in nonalcoholic fatty liver disease (NAFLD): a histologic marker of advanced NAFLD—clinicopathologic correlations from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49:809–820.
Argo CK, Northup PG, Al-Osaimi AM, Caldwell SH. Systematic review of risk factors for fibrosis progression in non-alcoholic steatohepatitis. J Hepatol. 2009;51:371–379.
Lackner C, Gogg-Kamerer M, Zatloukal K, Stumptner C, Brunt EM, Denk H. Ballooned hepatocytes in steatohepatitis: the value of keratin immunohistochemistry for diagnosis. J Hepatol. 2008;48:821–828.
Argo CK, Ikura Y, Lackner C, Caldwell SH. The fat droplet in hepatocellular ballooning and implications for scoring nonalcoholic steatohepatitis therapeutic response. Hepatology. 2015. doi:10.1002/hep.28009.
Caldwell S, Ikura Y, Dias D, et al. Hepatocellular ballooning in NASH. J Hepatol. 2010;53:719–723.
Caldwell SH, Redick JA, Chang CY, Davis CA, Argo CK, Al Osaimi KA. Enlarged hepatocytes in NAFLD examined with osmium fixation: does microsteatosis underlie cellular ballooning in NASH? Am J Gastroenterol. 2006;101:1677–1678.
Guy CD, Suzuki A, Burchette JL, et al. Costaining for keratins 8/18 plus ubiquitin improves detection of hepatocyte injury in nonalcoholic fatty liver disease. Hum Pathol. 2012;43:790–800.
Brunt EM, Janney CG, Di Bisceglie AM, Neuschwander-Tetri BA, Bacon BR. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am J Gastroenterol. 1999;94:2467–2474.
Gill RM, Belt P, Wilson L, Bass NM, Ferrell LD. Centrizonal arteries and microvessels in nonalcoholic steatohepatitis. Am J Surg Pathol. 2011;35:1400–1404.
Richardson MM, Jonsson JR, Powell EE, et al. Progressive fibrosis in nonalcoholic steatohepatitis: association with altered regeneration and a ductular reaction. Gastroenterology. 2007;133:80–90.
Ekstedt M, Hagstrom H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–1554.
Patton HM, Yates K, Unalp-Arida A, et al. Association between metabolic syndrome and liver histology among children with nonalcoholic Fatty liver disease. Am J Gastroenterol. 2010;105:2093–2102.
Molleston JP, White F, Teckman J, Fitzgerald JF. Obese children with steatohepatitis can develop cirrhosis in childhood. Am J Gastroenterol. 2002;97:2460–2462.
Nobili V, Marcellini M, Devito R, et al. NAFLD in children: a prospective clinical-pathological study and effect of lifestyle advice. Hepatology. 2006;44:458–465.
Carter-Kent C, Yerian LM, Brunt EM, et al. Nonalcoholic steatohepatitis in children: a multicenter clinicopathological study. Hepatology. 2009;50:1113–1120.
Fukusato T, Fukushima J, Shiga J, et al. Interobserver variation in the histopathological assessment of nonalcoholic steatohepatitis. Hepatol Res. 2005;33:122–127.
Sanyal AJ, Brunt EM, Kleiner DE, et al. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54:344–353.
Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA, Network NCR. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: distinct clinicopathologic meanings. Hepatology. 2011;53:810–820.
Kleiner DE, Brunt EM. Nonalcoholic fatty liver disease: pathologic patterns and biopsy evaluation in clinical research. Semin Liver Dis. 2012;32:3–13.
Belfort R, Harrison SA, Brown K, et al. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006;355:2297–2307.
Lavine JE, Schwimmer JB, Van Natta ML, et al. Effect of vitamin E or metformin for treatment of nonalcoholic fatty liver disease in children and adolescents: the TONIC randomized controlled trial. JAMA. 2011;305:1659–1668.
Torres DM, Jones FJ, Shaw JC, Williams CD, Ward JA, Harrison SA. Rosiglitazone versus rosiglitazone and metformin versus rosiglitazone and losartan in the treatment of nonalcoholic steatohepatitis in humans: a 12-month randomized, prospective, open-label trial. Hepatology. 2011;54:1631–1639.
Loomba R, Lutchman G, Kleiner DE, et al. Clinical trial: pilot study of metformin for the treatment of non-alcoholic steatohepatitis. Aliment Pharmacol Ther. 2009;29:172–182.
Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362:1675–1685.
Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet. 2015;385:956–965.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Rights and permissions
About this article
Cite this article
Bedossa, P. Histological Assessment of NAFLD. Dig Dis Sci 61, 1348–1355 (2016). https://doi.org/10.1007/s10620-016-4062-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4062-0