Abstract
Background
Osteopenia and osteoporosis are considered to be extra-intestinal manifestations of inflammatory bowel disease (IBD). Anti-tumor necrosis factor (TNF)-α biologics have been introduced as novel medications for an active IBD. However, it is still not well documented whether anti-TNF-α affects the frequency of bone loss or abnormality of bone mineral markers among patients with IBD.
Aims
This study was to investigate the biochemical basis of low bone mineral density (BMD) and increased turnover in IBD during infliximab (IFX) therapy.
Methods
Forty patients with Crohn’s disease (CD), 80 patients with ulcerative colitis (UC), and 65 age- and gender-matched controls were included. BMD was measured with dual-energy X-ray absorptiometry, and vitamins K and D were measured as serum undercarboxylated osteocalcin (ucOC) and 1,25-(OH)2D, respectively. Bone formation and resorption were based on measuring bone-specific alkaline phosphatase (BAP) and serum N-terminal telopeptide of type I collagen (NTx), respectively.
Results
Significantly lower BMD was found in patients with UC and CD as compared to controls (P < 0.05). BAP, 1,25-(OH)2D, ucOC, and NTx were significantly higher in CD patients, but not in UC patients as compared to controls (P < 0.05). Further, serum NTx level was significantly higher in CD patients who were receiving IFX as compared to CD patients who were not receiving IFX (P < 0.01).
Conclusions
A lower BMD and higher bone metabolism markers were found in CD patients as compared to controls or UC patients. A significant increased serum level of NTx, a biochemical marker of increased bone resorption, was observed in CD patients during IFX therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteopenia and osteoporosis are considered to be extra-intestinal manifestations of inflammatory bowel disease (IBD) [1]. Accordingly, the relative risk of fracture in IBD patients has been estimated to be 40 % higher than in the general population [2]. However, there is still no widely accepted consensus on the best evaluation method for the determination of osteoporosis in patients with IBD. Similarly, there is no established strategy for preventing or treating osteoporosis in IBD patients.
Osteoporosis is usually diagnosed by dual-energy X-ray absorptiometry (DEXA) scanning to quantify bone mineral density (BMD) [3]. BMD results are expressed as the number of standard deviations (SD) above or below the mean for a young adult population (T-score) or an age-matched population (Z-score) [4, 5]. DEXA scanning is a convenient noninvasive method for the evaluation of osteoporosis, but woman during pregnancy, or those expected to become pregnant, should not receive DEXA examination for the fear of increasing the incidence of congenital defects. However, it is possible to assess the state of bone metabolism by using biochemical bone metabolism markers in addition to BMD. Bone-specific alkaline phosphatase (BAP) is a marker of bone formation [6], while N-terminal telopeptide of type I collagen (NTx) is a biochemical marker of bone resorption [7]. Further, undercarboxylated osteocalcin (ucOC) has been shown to be a sensitive biomarker of vitamin K deficiency [8], while blood 1,25-(OH)2D concentration, which is an active form of vitamin D, has been found to be negatively correlated with BMD in patients with Crohn’s disease (CD) [9]. However, the role of these bone metabolism markers in the maintenance of bone health in IBD patients is not fully understood.
Recent studies have reported contradictory findings on osteoporosis and fractures in patients with CD and ulcerative colitis (UC) [10–15]. It would appear that osteoporosis in patients with CD is a multifactorial process. A greater risk of osteoporosis in CD than in UC might be attributed to the presence of small intestinal CD lesions causing malnutrition and impaired vitamin D or calcium absorption in CD patients [16]. Additionally, anti-tumor necrosis factor (TNF)-α biologics are suspected to increase the risk of osteoporosis [17]. However, currently there are no biochemical data to explain the mechanism by which TNF blockade leads to low BMD. This study was undertaken to investigate the biochemical basis of infliximab (IFX)-induced low bone density and increased turnover in patients with IBD.
Methods
Objectives
In a prospective setting, the objective of this study was to investigate the frequency of bone loss or abnormality of bone mineral markers among patients with IBD and to identify possible contributing risk factors. However, our major interest was to see whether IFX which is widely used in the treatment of patients with IBD affects bone turnover or other relevant bone turnover markers.
Study Populations
Between 2007 and 2011, 80 patients with UC (52 men, 28 women) and 40 patients with CD (27 men, 13 women) with a diagnosis of IBD [18] were included in this study. All patients had come to our IBD units for the treatment of IBD-related complications. We included patients between 25 and 60 years of age and excluded women who were pregnant or were hoping to become pregnant due to the potential risk from exposure to ionizing radiation by bone densitometry. Sixty-five age- and gender-matched healthy controls (33 men, 32 women) were also included (Table 1).
Measurement of Bone Mineral Density
BMD was measured at the lumbar spine (L2–L4) and femoral neck with dual-energy X-ray absorptiometry (Discovery A, Hologic, Bedford, MA, USA). BMD was expressed in absolute values (g/cm2), T-scores (one SD of the mean of a young adult gender-matched reference population), and Z-scores (one SD of the mean of an age- and gender-matched reference population).
Biochemical Measurements
Blood samples were centrifuged at 3000 rpm for 10 min at 4 °C. Serum samples were stored frozen at −20 °C until analysis. Serum undercarboxylated osteocalcin (ucOC) was measured by an electrochemiluminescence immunoassay (Sanko, Tokyo, Japan) for ucOC. Serum 1,25-(OH)2D was measured by a radioimmunoassay (Immunodiagnostic Systems, Boldon, UK). Serum N-terminal telopeptide of type I collagen (NTx), a marker of bone resorption, was measured by enzyme-linked immunosorbent assay (Ostex, Seattle, USA). Bone-specific alkaline phosphatase (BAP), a marker of bone formation, was measured by an enzyme immunoassay (Quidel, San Diego, CA, USA). All laboratory measurements were blindly carried out at an SRL (special research laboratory).
Ethical Considerations
Informed consent was obtained from all individual participants included in the study after explaining the nature of the procedures involved. Similarly, the study protocol was reviewed and approved by the Institutional Review Board at Hamamatsu University School of Medicine. The investigation was conducted in accordance with the Principle of Good Clinical Practice, and the ethical standards laid down in the 1964 Helsinki Declaration and its subsequent amendments.
Statistics
When appropriate, parametric data are presented as the mean ± SD values. Continuous data are compared by using a two-tailed Fisher’s exact test, unless stated otherwise. Correlations between two independent measurements were assessed by using the Pearson’s correlation coefficient. A P value of less than 0.05 was considered statistically significant.
Results
Patients’ Demographic Variables
The baseline demographic variables and laboratory data on the study populations are presented in Table 1. In patients who had received IFX (Tables 2 and 3), the median duration of IFX therapy was 15 months, range 6–24 months. Data presented in Table 1 show that when we analyzed BMD, the mean T-score of the femoral neck in CD and UC patients was significantly lower than in the controls (P < 0.05). Likewise, the mean Z-score of the femoral neck was significantly lower in patients with CD as compared to controls (P < 0.05) or UC patients (P < 0.05). Bone metabolism markers including 1,25-(OH)2D, bone-specific alkaline phosphatase (BAP), N-terminal telopeptide of type I collagen (NTx), and undercarboxylated osteocalcin (ucOC) were significantly higher in patients with CD, but not in patients with UC as compared to the controls (P < 0.05; Table 1). Similarly, the mean level of serum ucOC was significantly higher in patients with CD compared with patients with UC (P < 0.05).
IFX Therapy Was Associated with Increased Serum Level of NTx in Patient with CD
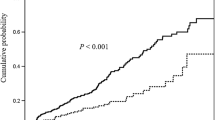
We were particularly interested to determine whether or not IFX therapy was associated with changes in BMD or bone metabolism markers in patients with CD. There was no significant difference in baseline demographic variables including the length of disease, disease location, previous CD surgery, corticosteroid use, or osteoprotective medications between patients with CD who were receiving IFX and CD patients who were not (Table 2). Likewise, the mean levels of BMD, T-score, and Z-score were not significantly lower in patients who were receiving IFX and those who were not (Tables 3, 4). Unexpectedly, there was no significant difference in the mean levels of T-score and Z-score between healthy controls and patients with CD who were taking corticosteroid (Fig. 1). Further, Fig. 2 shows that serum level of ucOC was significantly higher in CD patients as compared to controls regardless of IFX therapy, but the significance level was stronger in CD patients on IFX (P < 0.01) compared with CD patients not on IFX (P < 0.05). However, in patients with CD, the mean serum level of NTx (index of bone resorption) was significantly higher in patients who were receiving IFX compared with patients who were not (P < 0.01).
Serum levels of T-score and Z-score in patients with CD and healthy controls. Levels of T-score (a) and Z-score (b) in patients with CD who were not receiving IFX (n = 26), patients with CD who were receiving IFX (n = 14), and healthy controls (n = 65). Levels of T-score (c) and Z-score (d) in patients with CD who were not receiving corticosteroid (n = 26), patients with CD who were receiving corticosteroid (n = 14), and healthy controls (n = 65). Results represent the mean ± SD values. *P < 0.05; **P < 0.01
The Relation Between Serum NTx and T-Score in Patients with CD
We were interested to see whether or not the serum level of NTx was correlated with BMD in healthy controls and patients with CD. The regression lines using T-score as outcome variable (y) and serum NTx as predictor variable (x) were y = 0.048x − 0.771 and y = −0.037x − 0.195 for controls and CD patients, respectively. The regression coefficient for controls was significantly greater than that for CD patients (t = 3.55, P < 0.01). There was no statistically significant correlation between serum NTx and T-score in CD patients regardless of IFX therapy, except a greater tendency toward negative correlation between NTx and T-score in CD patients who were on IFX (Fig. 3). Other bone metabolism markers including 1,25-(OH)2D, BAP, and ucOC were correlated with BMD in controls and patients with CD. A statistically significant (P < 0.05) positive correlation (r = 0.275) was observed between serum ucOC level and BMD in healthy controls, but other bone metabolism markers were not associated with BMD in healthy controls (data not presented).
Correlation between T-score and serum NTx level in patients with CD and healthy controls. a Correlation between T-score and serum NTx in healthy controls (r = 0.17, P > 0.05) and patients with CD (r = 0.22, P > 0.05). The regression lines using T-score as the outcome variable (y) and NTx as the predictor variable (x) were y = 0.048x − 0.771 and y = −0.037x − 0.195 for the controls and CD patients, respectively. The regression coefficient for the controls was significantly greater than for CD patients (t = 3.55, P < 0.01). b The correlation between T-score and serum NTx level in patients with CD who were not receiving IFX (r = 0.17, P > 0.05) and patients with CD who were receiving IFX (r = 0.35, P > 0.05). The regression lines using T-score as the outcome variable (y) and NTx as the predictor variable (x) were y = 0.034x − 0.328 and y = −0.063x + 0.437 for patients with CD who were not receiving IFX and patients with CD who were receiving IFX, respectively. There was no significant difference in the regression coefficient between patients with CD who were not receiving IFX and patients with CD who were receiving IFX (t = −1.01, P > 0.05)
Discussion
From the observations described in this report, we could make the following statements on bone density, bone formation, and the related biochemical markers of bone turnover in patients with IBD. Compared with the controls, a lower level of BMD and a higher level of bone metabolism markers were seen in CD patients as compared to UC patients. The serum level of NTx was significantly higher in CD patients who were receiving IFX as compared to CD patients who were not receiving IFX, and this was the single most important finding of the present study and indicated that CD patients who are required for IFX therapy have an increased risk of bone resorption. There was a tendency toward negative correlation between the serum level of NTx and T-scores in CD patients, in particular those who were receiving IFX.
In this study, the mean Z-score of the femoral neck was significantly lower in patients with CD not only when compared with the controls, but also when compared with UC patients. Other studies have also shown that patients with CD are at an increased risk of low BMD compared with UC patients [10–13]. The presence of small intestinal CD lesions, which is common in CD patients, but not in UC patients, potentially can interfere with the absorption of vitamins and minerals, and contribute to the differences in BMD between CD and UC patients [16, 18]. Additionally, patients with CD are at a higher risk of developing intestinal strictures and often have abdominal discomfort as a primary symptom, which may lead to food avoidance and malnutrition.
In addition to measuring BMD, we assessed bone turnover markers in patients with IBD and controls. We found that the mean serum levels of 1,25-(OH)2D, BAP, NTx, and ucOC were significantly higher in patients with CD compared with the controls. These observations are in line with several recent studies. Abreu et al. [19] found that patients with CD have inappropriately elevated levels of 1,25-(OH)2D which is the active hormonal form of vitamin D and that the level of 1,25-(OH)2D correlated inversely with bone mineral density presumably because 1,25-(OH)2D mobilizes skeletal calcium stores. Nakajima et al. [20] reported that relative to healthy controls, serum level of ucOC, which is a sensitive biomarker of vitamin K deficiency, was significantly higher in patients with CD, but not in patients with UC, indicating that vitamin K was deficient in patients with CD. Gilman et al. [21] reported that compared with healthy controls, patients with CD had significantly higher concentrations of serum BAP (a sensitive marker of bone formation), and significantly higher concentrations of urinary NTx, a sensitive marker of bone resorption. These findings suggest that both the rates of bone resorption and bone formation are significantly increased in CD, reflecting an increased rate of bone turnover. An increased rate of bone turnover in elderly contributes to faster bone loss and is recognized as a risk factor for bone fracture [22].
We also were interested to see whether or not IFX affects the levels of bone metabolic markers in patients with CD. We found a significant increase in the level of serum NTx in patients with CD who were receiving IFX compared with patients who were not receiving IFX, indicating increased bone turnover associated with IFX therapy. At the time of this writing, we could not find any report describing the mechanism(s) associated with elevation of NTx in patients with Crohn’s disease. Potentially, this could be due to an excess collagen production or altered MMP–TIMP balance. However, an increased level of NTx is widely thought to indicate bone resorption and greater bone loss [23]. In other words, patients who have less bone density, and a high NTx level, may be at an increased risk of bone fracture [24, 25]. This risk is likely to be significantly higher in patients with IBD due to multiple medications they receive including biologics [17, 21]. Therefore, we believe that it is clinically relevant to measure NTx in a potentially at-risk population.
In this study, the T-score showed a declining tendency during a 6-month observation period in patients with CD who were receiving IFX (data not presented). The reason might be that these patients had more severe disease, which requires more aggressive treatment. A recent study show that the osteoclastogenic function of the Th17 TNFα+ cells that contribute to bone loss in IBD animal model [26]. Contrary to our findings, a number of studies have reported beneficial effect for IFX on bone turnover markers in patients with CD in the short term [27–31]. We believe that controlled long-term studies in large cohorts of patients are warranted to better understand the effects of IFX on osteoporosis.
The effect of corticosteroids on osteoporosis seen in patients with IBD is complex. While some studies have shown a clear relationship between lifetime corticosteroid dose and vertebral fracture rate or low BMD [32], other studies have suggested that BMD is unrelated to corticosteroid therapy [33–36]. In our study, BMD was significantly lower in patients with CD as compared to the controls, but not in patients with CD who were receiving corticosteroids. The conflicting results are probably a reflection of the heterogeneity of patient groups studied and the complex relationship between disease severity, systemic inflammation, and corticosteroid therapy.
A recent meta-analysis shows that bisphosphonate is effective for the treatment of low BMD patients with IBD and reduces the risk of vertebral fractures [37]. Our study indicates that CD patients receiving IFX considered having an increased risk of bone fracture because of low BMD and an increased bone resorption. Therefore, administration of bisphosphonate to these patients to reduce a risk of bone fracture should be considered.
In conclusion, we found that both bone resorption and bone formation were increased in patients with CD, but not in patients with UC. Furthermore, the serum level of NTx, which is a sensitive marker of bone resorption, was significantly increased in CD patients who were receiving IFX, indicating increased bone turnover associated with IFX therapy. Additionally, since there was a tendency toward negative correlation between NTx and T-score in CD patients who were receiving IFX, the risk of osteoporosis in patients with CD during IFX therapy may increase.
Abbreviations
- BAP:
-
Bone-specific alkaline phosphatase
- BMD:
-
Bone mineral density
- CD:
-
Crohn’s disease
- DEXA:
-
Dual-energy X-ray absorptiometry
- IBD:
-
Inflammatory bowel diseases
- IFX:
-
Infliximab
- NTx:
-
N-terminal telopeptide of type I collagen
- SD:
-
Standard deviation
- TNF:
-
Tumour necrosis factor
- ucOC:
-
Undercarboxylated osteocalcin
- UC:
-
Ulcerative colitis
References
Bischoff SC, Herrmann A, Göke M, Manns MP, von zur Mühlen A, Brabant G. Altered bone metabolism in inflammatory bowel disease. Am J Gastroenterol. 1997;92:1157–1163.
Ali T, Lam D, Bronze MS, Humphrey MB. Osteoporosis in inflammatory bowel disease. Am J Med. 2009;122:599–604.
Lewiecki EM, Borges JL. Bone density testing in clinical practice. Arq Bras Endocrinol Metabol. 2006;50:586–595.
NIH Consensus Development Panel on Osteoporosis Prevention. Diagnosis, and therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–795.
Genant HK, Engelke K, Fuerst T, et al. Noninvasive assessment of bone mineral and structure: state of the art. J Bone Miner Res. 1996;11:707–730.
Couttenye MM, D’Haese PC, Van Hoof VO, et al. Low serum levels of alkaline phosphatase of bone origin: a good marker of adynamic bone disease in haemodialysis patients. Nephrol Dial Transpl. 1996;11:1065–1072.
Eastell R, Mallinak N, Weiss S, et al. Biological variability of serum and urinary N-telopeptides of type I collagen in postmenopausal women. J Bone Miner Res. 2000;15:594–598.
Szulc P, Meunier PJ. Is vitamin K deficiency a risk factor for osteoporosis in Crohn’s disease? Lancet. 2001;357:1995–1996.
Miheller P, Muzes G, Hritz I, et al. Comparison of the effects of 1,25 dihydroxyvitamin D and 25 hydroxyvitamin D on bone pathology and disease activity in Crohn’s disease patients. Inflamm Bowel Dis. 2009;15:1656–1662.
Jahnsen J, Falch JA, Aadland E, Mowinckel P. Bone mineral density is reduced in patients with Crohn’s disease but not in patients with ulcerative colitis: a population based study. Gut. 1997;40:313–319.
Ghosh S, Cowen S, Hannan WJ, Ferguson A. Low bone mineral density in Crohn’s disease, but not in ulcerative colitis, at diagnosis. Gastroenterology. 1994;107:1031–1039.
Ardizzone S, Bollani S, Bettica P, Bevilacqua M, Molteni P, Bianchi Porro G. Altered bone metabolism in inflammatory bowel disease: there is a difference between Crohn’s disease and ulcerative colitis. J Intern Med. 2000;247:63–70.
Targownik LE, Bernstein CN, Nugent Z, Leslie WD. Inflammatory bowel disease has a small effect on bone mineral density and risk for osteoporosis. Clin Gastroenterol Hepatol. 2013;11:278–285.
Sinnott BP, Licata AA. Assessment of bone and mineral metabolism in inflammatory bowel disease: case series and review. Endocr Pract. 2006;12:622–629.
Loftus EV Jr, Achenbach SJ, Sandborn WJ, Tremaine WJ, Oberg AL, Melton LJ 3rd. Risk of fracture in ulcerative colitis: a population-based study from Olmsted County, Minnesota. Clin Gastroenterol Hepatol. 2003;1:465–473.
Leichtmann GA, Bengoa JM, Bolt MJ, Sitrin MD. Intestinal absorption of cholecalciferol and 25-hydroxycholecalciferol in patients with both Crohn’s disease and intestinal resection. Am J Clin Nutr. 1991;54:548–552.
Azzopardi N, Ellul P. Risk factors for osteoporosis in Crohn’s disease: infliximab, corticosteroids, body mass index, and age of onset. Inflamm Bowel Dis. 2013;19:1173–1178.
Carter MJ, Lobo AJ, Travis SP. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53:V1–V16.
Abreu MT, Kantorovich V, Vasiliauskas EA, et al. Measurement of vitamin D levels in inflammatory bowel disease patients reveals a subset of Crohn’s disease patients with elevated 1,25-dihydroxyvitamin D and low bone mineral density. Gut. 2004;53:1129–1136.
Nakajima S, Iijima H, Egawa S, et al. Association of vitamin K deficiency with bone metabolism and clinical disease activity in inflammatory bowel disease. Nutrition. 2011;27:1023–1028.
Gilman J, Shanahan F, Cashman KD. Altered levels of biochemical indices of bone turnover and bone-related vitamins in patients with Crohn’s disease and ulcerative colitis. Aliment Pharmacol Ther. 2006;23:1007–1016.
Riggs BL, Melton LJ 3rd, O’Fallon WM. Drug therapy for vertebral fractures in osteoporosis: evidence that decreases in bone turnover and increases in bone mass both determine antifracture efficacy. Bone. 1996;18:197S–201S.
Garnero P, Sornay-Rendu E, Duboeuf F, Delmas PD. Markers of bone turnover predict postmenopausal forearm bone loss over 4 years: the OFELY study. J Bone Miner Res. 1999;14:1614–1621.
Chesnut CH 3rd, Bell NH, Clark GS, et al. Hormone replacement therapy in postmenopausal women: urinary N-telopeptide of type I collagen monitors therapeutic effect and predicts response of bone mineral density. Am J Med. 1997;102:29–37.
Eastell R, Barton I, Hannon RA, Chines A, Garnero P, Delmas PD. Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate. J Bone Miner Res. 2003;18:1051–1056.
Ciucci T, Ibáñez L, Boucoiran A, et al. Bone marrow Th17 TNFα cells induce osteoclast differentiation, and link bone destruction to IBD. Gut. 2014. doi:10.1136/gutjnl-2014-306947.
Franchimont N, Putzeys V, Collette J, et al. Rapid improvement of bone metabolism after infliximab treatment in Crohn’s disease. Aliment Pharmacol Ther. 2004;20:607–614.
Ryan BM, Russel MG, Schurgers L, et al. Effect of antitumour necrosis factor-alpha therapy on bone turnover in patients with active Crohn’s disease: a prospective study. Aliment Pharmacol Ther. 2004;20:851–857.
Abreu MT, Geller JL, Vasiliauskas EA, et al. Treatment with infliximab is associated with increased markers of bone formation in patients with Crohn’s disease. J Clin Gastroenterol. 2006;40:55–63.
Miheller P, Muzes G, Zagoni T, Toth M, Racz K, Tulassay Z. Infliximab therapy improves the bone metabolism in fistulizing Crohn’s disease. Dig Dis. 2006;24:201–206.
Bernstein M, Irwin S, Greenberg GR. Maintenance infliximab treatment is associated with improved bone mineral density in Crohn’s disease. Am J Gastroenterol. 2005;100:2031–2035.
Compston JE, Judd D, Crawley EO, et al. Osteoporosis in patients with inflammatory bowel disease. Gut. 1987;28:410–415.
Bjarnason I, Macpherson A, Mackintosh C, Buxton-Thomas M, Forgacs I, Moniz C. Reduced bone density in patients with inflammatory bowel disease. Gut. 1997;40:228–233.
Pollak RD, Karmeli F, Eliakim R, Ackerman Z, Tabb K, Rachmilewitz D. Femoral neck osteopenia in patients with inflammatory bowel disease. Am J Gastroenterol. 1998;93:1483–1490.
Pigot F, Roux C, Chaussade S, et al. Low bone mineral density in patients with inflammatory bowel disease. Dig Dis Sci. 1992;37:1396–1403.
Robinson RJ, al-Azzawi F, Iqbal SJ, et al. Osteoporosis and determinants of bone density in patients with Crohn’s disease. Dig Dis Sci. 1998;43:2500–2506.
Melek J, Sakuraba A. Efficacy and safety of medical therapy for low bone mineral density in patients with inflammatory bowel disease: a meta-analysis and systematic review. Clin Gastroenterol Hepatol. 2014;12:32–44.
Acknowledgments
No external funding was used to carry out this study.
Authors’ Contributions
K. Sugimoto, H. Hanai, K. Ikeya, T. Iida, F. Watanabe: study concept and design; K. Sugimoto, S. Kawasaki, O. Arai, K. Umehara, S. Tani, S. Oishi, S. Osawa, T. Yamamoto, H. Hanai: acquisition of data, statistical analyses, and interpretation of data; K. Sugimoto, H. Hanai: drafting of the manuscript; K. Sugimoto, K. Ikeya, T. Iida, S. Kawasaki, O. Arai, K. Umehara, F. Watanabe, S. Tani, S. Oishi, S. Osawa, T. Yamamoto, H. Hanai: critical revision of the manuscript for important intellectual content, and approval of the final manuscript version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors hereby declare having no conflict of interest or funding interest in connection with the publication of this manuscript.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Sugimoto, K., Ikeya, K., Iida, T. et al. An Increased Serum N-Terminal Telopeptide of Type I Collagen, a Biochemical Marker of Increased Bone Resorption, Is Associated with Infliximab Therapy in Patients with Crohn’s Disease. Dig Dis Sci 61, 99–106 (2016). https://doi.org/10.1007/s10620-015-3838-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3838-y