Abstract
Hospitalizations after solid organ transplantation may affect patient outcomes. Identification of the factors attributed to them may decrease hospitalization rates, reduce overall cost, and improve post-transplant outcomes. We examined the risk factors for early hospitalization within 30 and 90 days after liver transplantation (LT).
Methods
Data on all deceased donor LT recipients (age ≥18 years) transplanted between 2/28/2002–2/27/2007 and discharged alive from the index hospitalization within 30 days of LT were collected (N = 267). Patients were followed up until December 31, 2013. Logistic regression was used to identify the predictors of 30-day hospitalization, and linear regression was used to identify the factors associated with number of days hospitalized during 30- and 90-day hospitalization after LT. Renal risk index (RRI), a recently developed and validated risk score that accurately predicts the post-LT ESRD based upon recipient factors at LT, was computed using RRI calculator (http://rri.med.umich.edu).
Results
One-third and more than half of the patients had at least one 30- and 90-day hospitalization, respectively. RRI decile (OR 1.12, P = 0.02) and serum sodium at LT (OR 0.90, P < 0.001) were independently associated with 30-day hospitalization after adjusting for MELD score. Serum creatinine at LT (β = 4.34, P = 0.001) and pre-LT admission days (β = 0.15, P = 0.027) affected the number of days hospitalized for 90-day hospitalization. RRI was also an independent predictor of post-LT mortality.
Conclusion
Early hospitalizations within 30 and 90 days after deceased donor LT are common. While all post-LT hospitalization cannot be prevented, efforts should be directed toward risk-based post-discharge care, and coordination of effective transitional care through ambulatory clinics. Implementation of such processes may attenuate early post-LT hospitalization and resource utilization and improve quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liver transplantation (LT) is an expensive life-saving procedure for patients with decompensated cirrhosis, with an estimated per-patient cost greater than half a million dollars. Post-discharge care and hospitalization within first 6 months of LT contribute significantly to this cost [1]. Some of the single-center studies have identified Child-Pugh C disease, age >60 years, and care at the intensive care unit at the time of LT as some of the factors associated with high resource utilization [2] [3]. Identification of LT recipients at risk for hospitalization based upon recipient factor(s) or previously validated risk models may decrease post-LT hospitalization, resource utilization, and improve post-LT outcomes.
We have recently developed and validated a risk calculator, called renal risk index (RRI), that accurately identifies LT recipients at risk of new-onset end-stage renal disease (ESRD) [4]. RRI score, based upon recipient factors at LT, represents the relative risk of developing incident post-LT ESRD compared to the reference patient. RRI stratifies LT recipients from the lowest to highest decile of post-LT ESRD risk. Additionally, RRI also predicts post-LT mortality [4]. The components of RRI are age at LT, African-American race, cholestatic disease, hepatitis C status, BMI at LT, pre-LT diabetes, serum creatinine, serum albumin, serum bilirubin, serum sodium, Status-1 listing, re-transplantation, history of transjugular intrahepatic porto-systemic shunt, and pre-LT dialysis. RRI may be a surrogate for the severity of overall sickness of a LT candidate going into transplant.
Reduction in hospital readmission has become a new target for quality improvement. The Centers for Medicare and Medicaid Services (CMS) will be directed to push hospitals to reduce 30-day readmission rates as part of the Affordable Care Act (ACA) [5]. ACA mandate requires the CMS to reduce payments to the hospitals for acute care readmission within 30 days of discharge or a surgical procedure as opposed to longer time periods. There are data in the non-transplant setting that hospitalization after a surgical procedure or discharge after medical condition such as pneumonia and congestive heart failure, adds significantly to morbidity and mortality [5, 6].
Although deceased donor LT is currently not included in the ACA mandate, we systematically studied the early hospitalization after LT at our center in order to examine the relationship between various recipient and donor factors and early hospitalization. Understanding these relationships would be an extremely important step toward unfolding the mechanism behind post-LT hospitalization which may lead to evidence-based development of point-of-care interventions to improve quality.
Our primary aim was to identify the risk factors associated with 30-day hospitalization after deceased donor LT. Our secondary aims were to identify the recipient and donor factors associated with number of days hospitalized during the 30- and 90-day post-LT period, respectively.
Methods
Patients and Data
Upon receiving approval from the institutional review board, we reviewed the data of all adult (age ≥18 years) deceased donor LT recipients who were transplanted at the University of Michigan between February 28, 2002, and February 27, 2007. We excluded repeat LT, living donor LT, and simultaneous liver and kidney transplant recipients. Patients who were hospitalized for more than 30 days after the index transplant or died during the index LT hospitalization were also excluded.
We collected the data on patient demographics, including race/ethnicity, etiology of liver disease, serum creatinine, bilirubin, INR, albumin and serum sodium, and dialysis status, model for end-stage liver disease (MELD) score at LT and body mass index (BMI), date of listing, date of transplant, hospital status at LT and length of stay of index LT. The donor data included donor age, donation after brain death (DBD), and donation after cardiac death (DCD), local, regional or national organ. Donor risk index (DRI) was not used as data on all the components of DRI were not available. RRI score and RRI decile were calculated as described by Sharma et al. [7], using a web-based calculator (https://rri.med.umich.edu). Patients were followed up from the day of transplant until death or December 31, 2013.
Statistical Analysis
Descriptive and Primary Outcome Analysis
Categorical variables were expressed as counts (%) and continuous variables were expressed as median. The primary outcome was 30-day hospitalization after index LT. LT recipients who were discharged alive within 30 days of index LT hospitalization were included in this analysis (N = 267). Age at LT, diagnosis, hepatocellular carcinoma, MELD, RRI decile, serum sodium, creatinine, bilirubin, INR, BMI, dialysis, donor age, DBD, discharge disposition of index LT hospitalization, length of stay of index LT hospitalization, and pre-LT admission days were the covariates tested in a univariate logistic regression analysis. Significant covariates (P < 0.05) in the univariate model were included in the multivariable logistic regression to analyze the factors associated with 30-day hospitalization. DBD (yes/no) was not significant in the univariate model; therefore, it was not tested in the multivariable model. Results were presented as odds ratio (OR) with 95 % confidence interval (CI), and P values were presented for the variables.
We hypothesized that 30-day hospitalization after LT was associated with the pre-LT degree of overall health of the recipients. Since MELD and RRI measured severity of the liver disease as well as severity of overall sickness, we tested MELD score and RRI decile in addition to other previously identified recipient and donor factors as covariates. Since creatinine and bilirubin were the components of MELD score and RRI, we performed multicollinearity diagnostic tests for RRI, MELD, and other covariates. MELD score and RRI were not found to be collinear based upon collinearity diagnostics.
Secondary Outcomes Analyses
The secondary outcomes were number of days hospitalized within the 30- and 90-day follow-up period and overall patient survival. We examined the factors affecting the number of days hospitalized during the 30- and 90-day follow-up period using linear regression model as two separate models. Since we were interested in the individual recipient and donor factors, RRI, MELD score, and DRI were not included in these models. Covariates with P < 0.05 were used in the multivariable model. Covariates significant (P < 0.05) in the univariate model were included in the multivariable linear regression. Results were presented as β coefficient and P value.
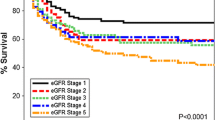
Kaplan–Meier analysis was used to assess the cumulative probability of survival after LT, and multivariable Cox regression analysis was used to assess the predictors. The time to death was from LT to the date of death, censored among survivors at the date of last follow-up (December 31, 2013). Results from the Cox model were presented as hazard ratio (HR) with 95 % CI and P values. All analyses were performed using SPSS version 22.0.
Results
Cohort Characteristics
There were a total of 322 primary deceased donor LT performed during the study period. After applying the exclusion criteria (index hospitalization >30 days = 47, death during index LT admission 30 days after transplant = 8), the cohort for primary outcome analysis consisted of 267 deceased donor LT recipients. All baseline characteristics including the median RRI and RRI decile were similar in the included and excluded LT recipients, with the exception of median MELD score (excluded: 21 vs. included: 17, P = 0.01).
Recipient characteristics at LT are shown in Table 1. Median age was 53 years, 69 % were male, and 45 % had hepatitis C as the etiology of liver disease. The median lab MELD score, BMI, and RRI at LT were 18, 28 kg/m2, and 1.4, respectively. The median donor age was 39 years.
The median serum sodium at LT was 137 mMol/L (interquartile range Q1:133; Q3:140). Only 10 (3.1 %) of the patients at LT had serum sodium <125 mMol/L and only 1 (0.3 %) patient had serum sodium >145 mMol/L.
Proportion of 30- and 90-Day Hospitalization
No hospitalization occurred in 176 (66 %) recipients. Eighty-three (31 %) of the LT recipients had one hospitalization, and eight (3 %) had two or more post-LT hospitalizations within 30 days of deceased donor LT. The causes of hospitalization were biliary complications (22 %), other surgical complications (including hepatic artery thrombosis, hemorrhage, wound infection/dehiscence, and venous outflow issues, 15 %), and infections excluding biliary source (21 %), other medical causes (24 %), rejection (1 %), tacrolimus toxicity (5 %), and miscellaneous causes (12 %).
One hundred and twenty-four LT recipients (46.4 %) did not have any admission within 90 days of LT. Seventy-three had at least 1 hospitalization (27.3 %) and seventy (26.3 %) had two or more hospitalizations within 90 days of LT.
Factors Associated with the Odds of 30-Day Post-LT Hospitalization
Lab MELD score (OR 1.06, P = 0.003), RRI decile (OR 1.11, P = 0.027), and serum sodium at LT (OR 0.91, P < 0.001) were associated with 30-day hospitalization on univariate analysis (Table 2).
In the multivariable logistic regression model, RRI decile (OR 1.12, P = 0.02) and serum sodium at LT (OR 0.90, P < 0.001) were the independent predictors of 30-day hospitalization after adjusting for lab MELD score (Table 2). Every unit increase in RRI decile was associated with 12 % increased odds of 30-day hospitalization. Every unit decrease in serum sodium at LT was associated with 10 % increased odds of 30-day hospitalization.
Factors Affecting Number of Days Hospitalized: 30-Day Follow-Up After LT
On univariate analysis, serum creatinine at LT (β = 1.44, P = 0.02), serum sodium at LT (β = −0.22, P = 0.02), and pre-LT admission days (β = 0.21, P = 0.04) were significantly associated with number of days hospitalized for 30-day hospitalization. On multivariate analysis, none of these variables were significant. There was a trend between serum creatinine and number of days hospitalized during the 30-day follow-up after LT, but it was not statistically significant (β = 1.23, P = 0.056).
Since we were interested in the effect of individual donor and recipient components on number of days hospitalized during the 30-day follow-up period, MELD score and RRI components were included in this model.
Factors Affecting Number of days Hospitalized: 90-Day Follow-Up After LT
In the univariate analysis, pre-LT admission days (β = 0.40, P = 0.04), donor age (β = 0.14, P = 0.03), serum creatinine at LT (β = 3.96, P = 0.001), serum bilirubin at LT (β = 0.35, P = 0.04), and serum sodium at LT (β = −0.41, P = 0.02) significantly affected the number of days hospitalized for 90-day hospitalization.
In the multivariable model, serum creatinine (β = 4.34, P = 0.001) and donor age (β = 0.15, P = 0.027) were independently associated with number of days hospitalized during the 90-day follow-up after adjusting for pre-LT admission days, serum bilirubin, and serum sodium at LT.
Predictors of Patient Survival
There were a total of 91 deaths during the follow-up period. The cumulative probability of 1-, 3-, and 5-year survival was 89, 78, and 73 % respectively. RRI decile (HR [95 % CI] = 1.15 [1.06–1.26], P = 0.001) and diagnosis of hepatitis C (HR [95 % CI] = 1.06 [1.03–2.51], P = 0.038) were the independent predictors of mortality after adjusting for MELD score, BMI, donor age, and pre-LT admission days.
Discussion
Our study showed that one-third of LT recipients had 30-day hospitalization after LT, and this proportion increased to more than half for 90-day hospitalization. RRI decile and serum sodium at LT were associated with 30-day hospitalization. High creatinine at LT and advanced donor age significantly contributed to the total number of days hospitalized within 90 days of LT. RRI decile and hepatitis C predicted overall patient survival.
Our study established an association between RRI decile and 30-day hospitalization. RRI was derived from a cohort of 43,514 LT recipients. It consists of 14 recipient risk factors and represents the relative risk of developing incident post-LT ESRD compared to the reference patient. Risk of post-LT ESRD increased with the increase in RRI decile [4]. Furthermore, increase in RRI decile was also associated with increased post-transplant mortality [4]. Our study showed twelve percent increased risk of 30-day hospitalization with every unit increase in RRI decile. This effect was independent of MELD score and serum creatinine at LT. RRI was also an independent predictor of post-LT survival. We think that RRI is a unique domain that reflects the overall severity of sickness of a candidate at LT which is not captured by MELD at LT. Therefore, those with high RRI decile were more likely to have an increased risk of hospitalization after LT independent of their MELD score and renal function at LT.
It has been previously shown that low serum sodium levels were associated with an increased index LT length of stay and early post-LT outcomes [8, 9]. We also found an independent association between serum sodium and 30-day hospitalization. Every unit decrease in serum sodium at LT was associated with 10 % increased odds of 30-day hospitalization. Given that the patients with MELD score ≥12 and low serum sodium receive survival benefit from LT [10], more patients with hyponatremia may get LT. These results may have implications in the future in terms of resource utilization among hyponatremic patients because of the implementation of MELD-Na for liver allocation [11].
In addition to other factors, Pereira et al. [2] found an association of increased 30-day hospitalization with pre-LT hospitalization within 90 days, pre-LT serum creatinine, and index LT length of stay. In our study, we observed a trend toward increase in total number of days hospitalized during the first 30 days with every unit increase in creatinine. This trend became statistically significant for the number of days hospitalized for 90-day hospitalization. Our study also showed an independent association of donor age with increase in number of days hospitalized during the first 90 days. Donor age also predicts graft failure and is one of the components of DRI [12].
Our study did not find an association between MELD score at LT and 30-day hospitalization similar to Buchanan et al. [13]. MELD is an excellent predictor of waitlist mortality, but its validity in predicting the resource utilization and post-LT survival is often questioned.
The main limitation of our study is the retrospective observational design from a single center which may not be generalizable to other centers. Moreover, the observational study design may result in bias due to patient selection and unmeasured patient characteristics. Furthermore, given the small sample size, our study is not powered to develop and validate risk prediction models. The majority of the complications following LT leading to readmission were biliary, infectious, or technical in nature. However, our study did not examine the correlation between RRI and surgical complications. Despite these limitations, this hypothesis-generating study highlights the burden of early post-LT hospitalization and identified important risk factors associated with post-LT hospitalization.
In conclusion, 30- and 90-day post-LT hospitalizations are common among LT recipients and should not be included in the ACA mandate of reducing payments for acute care readmission. RRI predicted the 30-day hospitalization and post-LT mortality. It is difficult to modify recipient and donor risk factors given the narrow window of opportunity for transplantation. Finally, future research should be directed toward risk-based post-discharge care and coordination of effective transitional care through ambulatory clinics. A transitional care model that involves following up patients closely in a multidisciplinary transplant clinic with protocol-driven care administered by extended provider under the direct supervision of transplant physician or surgeon should be tested in the future. Implementation of such processes may attenuate early post-LT hospitalization and resource utilization and improve quality.
Abbreviations
- BMI:
-
Body mass index
- LT:
-
Liver transplantation
- MELD:
-
Model for end-stage liver disease
- RRI:
-
Renal risk index
References
Bentley ST, Hanson SG, Hauboldt RA. US organ and tissue transplant cost estimates and discussion. Milliman Research Report: Milliman Inc., 2011:1–14.
Pereira AA, Bhattacharya R, Carithers R, et al. Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transplant. 2012;18:1037–1045.
Shankar N, Marotta P, Wall W, et al. Defining readmission risk factors for liver transplantation recipients. Gastroenterol Hepatol (NY). 2011;7:585–590.
Sharma P, Goodrich NP, Schaubel DE, Guidinger MK, Merion RM. Patient-specific prediction of ESRD after liver transplantation. J Am Soc Nephrol. 2013;24:2045–2052.
Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–505.
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428.
Sharma P, Perlmutter A. Renal risk index calculator; 2013. https://RRI.med.umich.edu.
Leise MD, Yun BC, Larson JJ, et al. Effect of the pretransplant serum sodium concentration on outcomes following liver transplantation. Liver Transpl. 2014;20:687–697.
Londono MC, Guevara M, Rimola A, et al. Hyponatremia impairs early posttransplantation outcome in patients with cirrhosis undergoing liver transplantation. Gastroenterology. 2006;130:1135–1143.
Sharma P, Schaubel DE, Goodrich NP, Merion RM. Serum sodium and survival benefit of liver transplantation. Liver Transpl. 2015;21:308–313.
Liver and Intestinal Organ Transplantation Committee. Proposal to add serum sodium to the MELD score; 2013. http://optn.transplant.hrsa.gov/converge/CommitteeReports/broad_main_liver&intestinalorgantransplantationcommittee_7_2_2014_15_56.pdf. Accessed 12 Nov 2014.
Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783–790.
Buchanan P, Dzebisashvili N, Lentine KL, et al. Liver transplantation cost in the model for end-stage liver disease era: looking beyond the transplant admission. Liver Transpl. 2009;15:1270–1277.
Acknowledgments
This research was presented, in part, as a free communication at the national meeting of American Association for the Study of Liver Diseases, 2014 held at Boston, MA. Dr. Sharma is supported by National Institutes of Health (NIH) Grant K08-DK-088946, R03-DK-102480 and research award from American College of Gastroenterology.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yu, J., Hosmer, A., Parks, T. et al. Predictors of Early Hospitalization After Deceased Donor Liver Transplantation. Dig Dis Sci 60, 3242–3247 (2015). https://doi.org/10.1007/s10620-015-3753-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3753-2