Abstract
Background
Previous studies analyzing lipid profile in small cohorts of patients with rheumatic and inflammatory bowel diseases (IBD) treated with TNFα blockers showed conflicting results. We aim to evaluate the effect of anti-TNFα monoclonal antibodies, infliximab and adalimumab, on lipid profile in IBD patients followed up to 3 years.
Methods
Clinical charts of 128 consecutive IBD patients, who received at least three doses of infliximab or two doses of adalimumab, and with a clinical follow-up of at least 1 year, were retrospectively reviewed. Lipid profiles (total, HDL and LDL cholesterol, and triglycerides) before beginning the treatment and after 1 and 3 years of follow-up were collected. Multiple linear regression analysis was performed considering total cholesterol difference at basal time, 1 and 3 years as a dependent variable.
Results
There was not a statistically significant difference between pre- and post-treatment lipid profiles. However, the subgroup with normal-range total cholesterol level before anti-TNFα treatment (n = 82) showed a significant increase in total cholesterol after 1 and 3 years, and a significant increase in LDL cholesterol after 3 years. The subgroup with basal normal-range triglycerides showed a significant increase after 1 and 3 years of follow-up. Atherogenic index resulted significantly increased after 3 years of anti-TNFα treatment. Multivariate analysis showed no influence of age, gender, type of IBD, body mass index, or the presence of two or more cardiovascular risk factors.
Conclusions
No significant changes in lipid profile of IBD patients on anti-TNFα therapy were observed after 1 and 3 years of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the beginning of biological anti-TNFα therapy in the management of immune-mediated inflammatory disorders, including inflammatory bowel disease (IBD), safety issues have remained a major concern for clinicians, especially in the long term. Clinical trials and post-marketing observational studies have focused on infectious, immune and neoplastic adverse events, but there is scarce information about cardiovascular or metabolic complications.
Previous studies concerning lipid profile in patients with rheumatic diseases treated with TNFα blockers showed conflicting results. Thus, it was initially observed that 2 weeks after first infliximab infusion, there was an improvement in lipid profile due to an increase in HDL cholesterol (HDL-c) levels [1]; however, this effect seems to be transient, since 12 months after infusion, there were no significant differences in HDL-c levels, and rising concentrations of total cholesterol and LDL cholesterol (LDL-c) levels were observed [2]. Another study demonstrated an increase in HDL-c levels only in the first month after initiating infliximab in patients with psoriatic arthritis (PA) [3]. Moreover, it was also observed that infliximab therapy leads to an increase in triglycerides levels in small cohorts of patients with PA [4, 5].
Lipid profile has been specifically evaluated in IBD patients [6] of whom a pro-atherogenic lipid profile—higher LDL-c and triglycerides levels—has been detected, particularly in males. Furthermore, to our knowledge, there are two previous studies that have evaluated the lipid profile in IBD patients after biologic therapy, both of them showing a rise in total cholesterol and HDL-c levels after infliximab induction and maintenance doses [7, 8], with stable concentrations of LDL-c and triglycerides. Nevertheless, long-term follow-up was not evaluated, and no other biologic agent other than infliximab was examined.
The objective of this study was to analyze the effect of TNFα blockers on lipid profile of IBD patients, including long-term (up to 3 years) follow-up results.
Patients and Methods
A total of 190 consecutive patients diagnosed with IBD and treated with anti-TNFα therapy (infliximab or adalimumab) were evaluated in the period of January 2005 to March 2012. IBD diagnosis was made in all of the patients following standard clinical, radiological, endoscopic and histological criteria. Only patients who received at least three doses of infliximab (5 mg/kg at weeks 0, 2, and 6) or two doses of adalimumab (160 mg at week 0, followed by 80 mg at week 2), and with a clinical follow-up of at least 1 year, were finally considered. After retrospective review of clinical charts, following variables were collected immediately before starting biologics: age, sex, type of IBD [Crohn’s disease (CD), ulcerative colitis (UC), and indeterminate colitis (IC)], Montreal classification for CD (age, behavior, and localization) and for UC (extension), body mass index (BMI), the presence of cardiovascular risk factors—high blood pressure, diabetes mellitus, obesity (BMI ≥ 25), alcohol intake (more than 20 g per day of alcohol), and active smoking habit [9]—and concomitant medications. Laboratory parameters were also collected, including complete fasting lipid panel (total cholesterol, HDL-c, LDL-c, and triglycerides), albumin, and glucose and inflammatory markers (C reactive protein (RCP) and fibrinogen). Every variable was analyzed within 1 month before the biologic first dose and then after 1-year (±2 months) and 3-year (±4 months) periods.
Statistical methods (SPSS 20.0, SPSS Inc., Chicago, IL, USA) include categorical variables description, as total number of cases (n), relative frequency (%), mean and standard deviation (SD), and range of continuous variables. Lipid profile results were expressed as mean values with standard deviation. Differences between laboratory test results before and 1 or 3 years after therapy were evaluated with paired samples T test, considering P < 0.05 as statistically significant difference. A multiple linear regression analysis was carried out, taking into account the difference in total cholesterol (after 1 and 3 years) as dependent variable.
Results
From 190 initial patients, 62 were excluded as they did not fit inclusion criteria: 23 did not received at least induction doses (three in infliximab cases or two in adalimumab cases); in 27 patients, follow-up was less than 1 year, and in 12 patients, there were clinical or laboratory features that could not be evaluated in their clinical charts. A total of 128 patients were finally included in the study. Of them, 126 (98.4 %) received scheduled maintenance treatment (mean time: 33.5 months); moreover, 54.8 % of patients treated with infliximab (n = 62) and 60 % of patients treated with adalimumab (n = 9) required dose escalation every 4 weeks or every week, respectively. A total of 114 were treated with only one TNFα blocker (infliximab = 104, adalimumab = 10), while 14 received both of them. We chose for statistical analysis the lipid panel concerning only the first biologic agent used in each patient. Clinical features, including cardiovascular risk factors of patients considered, are summarized in Table 1. 50 % of patients were females. Mean (range) age was 43.5 (17–85) years. CD was diagnosed in 92 patients, UC in 32, and IC in four cases. Mean (SD) BMI previous to therapy was 23.9 kg/m2 (4.9), with a significant increase at 1 year of 0.74 kg/m2 (2.5) and at 3 years of 1.44 kg/m2 (3.5) (P = 0.003 and P < 0.001, respectively). Montreal classification for both CD and UC is shown in Table 2.
First, we compared lipid profile before treatment and after 1 year; as shown in Table 3, no statistically significant differences were noted in triglycerides levels (128.70 ± 81.45 vs 127.26 ± 85.01; P = NS), total cholesterol (180.84 ± 42.50 vs 181.66 ± 52.22; P = NS), LDL-c (106.61 ± 69.51 vs 96.11 ± 28.34; P = NS), and HDL-c (53.89 ± 17.14 vs 53.41 ± 14.14; P = NS). When compared lipid profile before treatment and after 3 years, no significance was found in any parameter: total cholesterol (180.84 ± 42.50 vs 185.19 ± 32.40; P = NS), LDL-c (106.61 ± 69.52 vs 105.35 ± 29.76; P = NS), HDL-c (53.89 ± 17.14 vs 53.58 ± 15.32; P = NS), and triglycerides (128.70 ± 81.44 vs 137.62 ± 107.22; P = NS). No differences on lipid profile were demonstrated after 1 or 3 years in the subgroup of patients with infliximab or adalimumab dose escalation during the analysis period (data not shown). In addition, no significant correlation between total cholesterol or triglycerides and CRP was perceived before treatment or 1/3 years after anti-TNF therapy.
Subsequently, we evaluated a subgroup of patients (n = 82) whose total cholesterol values before treatment were equal or less than 200 mg/dL and were not on statins treatment. A statistically significant increase in total cholesterol values between basal time and 1 (159.13 ± 26.06 vs 172.76 ± 54.87; P = 0.029) or 3 years (159.13 ± 26.60 vs 176.57 ± 30.22; P < 0.001) was observed in this sub-analysis. LDL-c did not increase significantly in the first year (86.61 ± 22.89 vs 90.48 ± 27.05; P = 0.205, NS), but did significantly rise after a 3-year period comparing to baseline (86.61 ± 22.89 vs 97.9 ± 2.88; P = 0.04). On the other hand, HDL-c remained stable after 1 (51.97 ± 15.37 vs 51.90 ± 14.86; P = NS) and 3 years (51.97 ± 15.37 vs 54.02 ± 17.22 P = NS) (see Table 4). Furthermore, we calculated the atherogenicity index (total cholesterol/HDL-c) in both periods in the patients of this subgroup; no significant changes in 1-year period (3.29 ± 0.95 vs 3.38 ± 0.95, P = NS) were found, but a statistically significant increase in 3-year period (n = 39) (3.10 ± 0.85 vs 3.53 ± 1.21, P = 0.008) was observed.
Another subgroup, excluding patients with basal levels of triglycerides above 150 mg/dL, was analyzed (n = 77). A significant increase was noticed in 1-year period (86.32 ± 26.62 vs 103.71 ± 58.94; P = 0.01) and 3-year period (86.32 ± 26.62 vs 110.98 ± 56.65; P = 0.026) in those patients with basal levels of triglycerides below 150 mg/dL (Table 4).
Finally, multivariate analysis shown that there is no influence of age, sex, type of IBD, difference of BMI, or presence of two or more cardiovascular risk factors in the increase in total cholesterol values neither after 1 (Table 5) nor 3 years (Table 6) of anti-TNFα treatment.
Discussion
The results of the present study show that anti-TNFα therapy with infliximab or adalimumab in IBD patients does not significantly change lipid profile after 1 and 3 years of treatment. Nevertheless, in those patients with normal lipid profile at baseline—total cholesterol less than 200 mg/dL and triglycerides less than 150 mg/dL—anti-TNFα treatment leads to an increase in total cholesterol values, at the expense of LDL-c fraction, as well as triglycerides, after 1 and 3 years of follow-up. Multivariate analysis showed no influence of age, sex, type of IBD (CD and UC), difference of BMI, or presence of two or more cardiovascular risk factors (high blood pressure, diabetes mellitus, obesity, smoking, and alcohol habit). The reason why this effect was only observed in patients with normal lipid profile at baseline is not clear, but such a quantitatively modest change may not be detected in patients with hyperlipidemia prior to treatment. We have not found another examples in the scientific literature of drug-induced hyperlipidemia (antipsychotics, thiazides, and oral contraceptives) only in such patients with normal baseline profile, and we cannot provide and evidence-based mechanistic explanation. To be confirmed, this conclusion needs further biological and clinical studies.
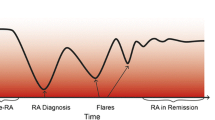
Chronic inflammatory diseases have been identified as risk factors for atherothrombotic events. Nevertheless, a systematic review evaluating 11 studies concluded that IBD was not associated with increased cardiovascular mortality [10], and a recent meta-analysis found that patients with UC and CD had higher rates of death from colorectal cancer, pulmonary disease, and nonalcoholic liver disease, but mortality from cardiovascular disease was decreased [11]. However, it should be taken into account that cardiovascular mortality could be a suboptimal surrogate for cardiovascular disease incidence; in this sense, a more recent Danish nationwide study [12] examined the risk not only of death, but also of cardiovascular complications in a large cohort of IBD patients and found overall increased risk of myocardial infarction (RR = 1.17), stroke (RR = 1.15), and also cardiovascular-related death (RR = 1.35), increasing during flares and persistent IBD activity periods. Similar results were observed in two recent meta-analyses [13, 14], where an increased risk of ischemic heart disease and stroke was identified among IBD patients. This increased risk could be related to endothelial [15] and platelets [16] dysfunction; the potential contribution of IBD treatment has not been evaluated. Regarding metabolic syndrome (MS)—characterized by central obesity, elevated triglycerides levels, low HDL-c levels, impaired fasting glucose, and hypertension—a study from Japan [17] found that its prevalence in a cohort of 102 quiescent IBD patients was comparable to general population; however, among IBD patients, MS prevalence was significantly higher in UC (23 %) than in CD patients (7.1 %), finding age as an independent risk factor for its development.
In agreement with our findings, previous studies suggested a relationship between TNFα blockers and worsening of lipid profile, mainly in patients with rheumatic diseases. A prospective study [1] in 33 patients with rheumatoid arthritis (RA) observed an increase in HDL-c values after 2 weeks of monoclonal antibodies therapy; meanwhile, LDL-c and triglycerides kept without variation. The same authors analyzed in another prospective analysis [2] the lipid profile in 55 patients with RA under infliximab therapy compared with the same laboratory test in 55 controls, during 1 year. The results show that the increase in HDL-c levels does not persist over time, as we observed in our study. However, statistically significant rise in total cholesterol and LDL-c levels was identified after 12 months. On the other hand, Spanakis et al. [3] demonstrated an increase in HDL-c levels in patients with PA, but only in the first month after initiating infliximab. With respect to triglycerides, two studies in patients with PA show results in agreement with ours: Antoniou et al. [4] observed a significant increase in triglycerides levels in eight patients with PA after infliximab therapy. In the second one [5], the authors demonstrated rising triglycerides plasmatic levels after 3 months of infliximab therapy in 15 patients with PA; in this study, however, atherogenicity index remained stable. This result contrasts with our observation of an increase in atherogenic index after 3 years in those patients with normal basal levels of cholesterol; this fact could be due to a larger follow-up and sample size in our study.
The effect of biologic treatment on lipid plasmatic concentration in IBD patients has been previously evaluated in two studies. In a Greek study [7], 22 patients on infliximab therapy (5 mg/kg at weeks 0, 2, and 6 and then every 8 weeks) were followed up during only 14 weeks, showing at the end of that period an increase in total cholesterol and HDL-c levels. In another study from Lille (France) [8], the authors prospectively analyzed lipid panel in 111 CD patients on infliximab therapy during 41 weeks, demonstrating rising in total cholesterol and HDL-c levels. However, and in contrast to our data, LDL-c and TG levels remained stable. We would like to emphasize that largest differences showed in our work were detected after 3 years from the beginning of therapy, whereas the average period of follow-up in this study is 41 weeks.
The potential mechanisms of such effects are unknown. Immune-mediated inflammatory disorders are characterized by elevated catabolism, high rates of lipolysis, and decreased lipogenesis. It is tempted to hypothesize that improving disease activity of patients with moderate to severe disease with anti-TNFα therapy may lead to a better absorption of nutrients, including lipids; specifically, attenuation of mucosal inflammation in distal ileum may improve malabsorption of bile acids and cholesterol. Neither can we rule out an effect of an expansion of diet, due to an overall improvement in health status. Likewise, it is well known that TNFα infusion can lead itself to a cachexia-like state [18, 19]. Blocking this molecule may ameliorate malnourishment, including lipid profile; in this sense, we did not evaluate the correlation between anti-TNFα response and lipid profile changes in our retrospective analysis. This point deserves further investigation. And, finally, we could not rule out the influence of aging, that is well known to lead to a worsening in lipid profile, increased total cholesterol and LDL-c, as seen in general population [20, 21].
In conclusion, taking into account our results, no differences in lipid profile have been observed in the whole cohort of IBD patients on anti-TNFα. However, this therapy may have a damaging effect on lipid profile in IBD patients with pre-treatment low values, increasing atherogenic index in IBD patients. Nevertheless, whether this increase has clinical relevance or not—i.e., an impact on total cardiovascular risk—remains unknown due to the complex relationship between the strong anti-inflammatory effects and changes in the natural history of the disease. In the light of all this data and above considerations, it seems mandatory to evaluate prospectively cardiovascular events in large cohorts of patients treated with anti-TNFα antibodies in a long-term follow-up period.
References
Popa C, Netea MG, Radstake T, et al. Influence of anti-tumour necrosis factor therapy on cardiovascular risk factors in patients with active rheumatoid arthritis. Ann Rheum Dis. 2005;64:303–305.
Popa C, van den Hoogen FH, Radstake TR, et al. Modulation of lipoprotein plasma concentrations during long-term anti-TNF therapy in patients with active rheumatoid arthritis. Ann Rheum Dis. 2007;66:1503–1507.
Spanakis E, Sidiropoulos P, Papadakis J, et al. Modest but sustained increase of serum high density lipoprotein cholesterol levels in patients with inflammatory arthritides treated with infliximab. J Rheumatol. 2006;33:2440–2446.
Antoniou C, Dessinioti C, Katsambas A, Stratigos AJ. Elevated triglyceride and cholesterol levels after intravenous antitumour necrosis factor-alpha therapy in a patient with psoriatic arthritis and psoriasis vulgaris. Br J Dermatol. 2007;156:1090–1091.
Castro KR, Aikawa NE, Saad CG, et al. Infliximab induces increase in triglyceride levels in psoriatic arthritis patients. Clin Dev Immunol. 2011;2011:352686.
Sappati Biyyani RS, Putka BS, Mullen KD. Dyslipidemia and lipoprotein profiles in patients with inflammatory bowel disease. J Clin Lipidol. 2010;4:478–482.
Koutroubakis IE, Oustamanolakis P, Malliaraki N, et al. Effects of tumor necrosis factor alpha inhibition with infliximab on lipid levels and insulin resistance in patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2009;21:283–288.
Parmentier-Decrucq E, Duhamel A, Ernst O, et al. Effects of infliximab therapy on abdominal fat and metabolic profile in patients with Crohn’s disease. Inflamm Bowel Dis. 2009;15:1476–1484.
Nunes T, Etchevers MJ, Merino O, et al. Does smoking influence Crohn’s disease in the biologic era? The TABACROHN study. Inflamm Bowel Dis. 2013;19:23–29.
Dorn SD, Sandler RS. Inflammatory bowel disease is not a risk factor for cardiovascular disease mortality: results from a systematic review and meta-analysis. Am J Gastroenterol. 2007;102:662–667.
Bewtra M, Kaiser LM, TenHave T, Lewis JD. Crohn’s disease and ulcerative colitis are associated with elevated standardized mortality ratios: a meta-analysis. Inflamm Bowel Dis. 2013;19:599–613.
Kristensen SL, Ahlehoff O, Lindhardsen J, et al. Disease activity in inflammatory bowel disease is associated with increased risk of myocardial infarction, stroke and cardiovascular death—a Danish nationwide cohort study. PLoS ONE. 2013;8:e56944.
Fumery M, Xiaocang C, Dauchet L, Gower-Rousseau C, Peyrin-Biroulet L, Colombel JF. Thromboembolic events and cardiovascular mortality in inflammatory bowel diseases: a meta-analysis of observational studies. J Crohns Colitis. 2014;8:469–479.
Singh S, Singh H, Loftus EV Jr, Pardi DS. Risk of cerebrovascular accidents and ischemic heart disease in patients with inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:382–393.
Principi M, Mastrolonardo M, Scicchitano P, et al. Endothelial function and cardiovascular risk in active inflammatory bowel diseases. J Crohns Colitis. 2013;7:e427–e433.
Menchen L, Marin-Jimenez I, Arias-Salgado EG, et al. Matrix metalloproteinase 9 is involved in Crohn’s disease-associated platelet hyperactivation through the release of soluble CD40 ligand. Gut. 2009;58:920–928.
Nagahori M, Hyun SB, Totsuka T, et al. Prevalence of metabolic syndrome is comparable between inflammatory bowel disease patients and the general population. J Gastroenterol. 2010;45:1008–1013.
Tracey KJ, Wei H, Manogue KR, et al. Cachectin/tumor necrosis factor induces cachexia, anemia, and inflammation. J Exp Med. 1988;167:1211–1227.
Fong Y, Moldawer LL, Marano M, et al. Cachectin/TNF or IL-1 alpha induces cachexia with redistribution of body proteins. Am J Physiol. 1989;256:R659–R665.
Ericsson S, Eriksson M, Vitols S, Einarsson K, Berglund L, Angelin B. Influence of age on the metabolism of plasma low density lipoproteins in healthy males. J Clin Invest. 1991;87:591–596.
Ericsson S, Berglund L, Frostegard J, Einarsson K, Angelin B. The influence of age on low density lipoprotein metabolism: effects of cholestyramine treatment in young and old healthy male subjects. J Intern Med. 1997;242:329–337.
Acknowledgments
Supported by Grants from Spanish Ministry of Health (Instituto de Salud Carlos III-ISCIII-FIS 10/01912 and CIBEREHD) to LM.
Conflict of interest
The authors declare that they have no conflict of interest, financial or otherwise, with respect to this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miranda-Bautista, J., de Gracia-Fernández, C., López-Ibáñez, M. et al. Lipid Profile in Inflammatory Bowel Disease Patients on Anti-TNFα Therapy. Dig Dis Sci 60, 2130–2135 (2015). https://doi.org/10.1007/s10620-015-3577-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3577-0