Abstract
Background and Aim
Elderly patients are frequently affected by gallstone-related disease. Current guidelines support cholecystectomy after a first acute biliary complication. In the aging, these recommendations are irregularly followed.
Methods
We analyzed data from patients 65 or older admitted between June 30, 2004 and June 30, 2013 with a diagnosis of acute pancreatitis, cholangitis, or cholecystitis. Diagnosis and severity assessment were defined according to current guidelines. Harms, mortality, and cholecystectomy rates were evaluated. Baseline factors independently predicting cholecystectomy were identified.
Results
A total of 491 patients were included. The median age was 78.8 years, and 51.7 % were women. Acute cholecystitis was present in 51.7 %, acute pancreatitis in 36.5 %, and acute cholangitis in 11.8 %. Cholecystectomy was performed in 47.1 %. Age, myocardial infarct, dementia, diabetes, nonmetastatic tumor, and severe liver disease were risk factors for not undergoing surgery. Complications related to hospital stay appeared in 33 % of patients. Surgery, cholecystostomy, and ERCP presented harms in 21–25 %. Overall mortality rate was 5.4 %: 10.4 % in acute cholangitis, 6.8 % in acute cholecystitis, and 2.2 % in acute pancreatitis. Mild cases presented a 1.3 % mortality, while 28.6 % of severe cases died. After discharge, 24.7 % of patients presented a new biliary complication, 9.7 % of them severe. Relapse was more frequent in patients managed without invasive procedures, 42.3 % than in cholecystectomy patients, 9.9 % (p < 0.001) and than in ERCP patients, 19.4 % (p = 0.01).
Conclusions
Cholecystectomy should be recommended to elderly patients after a first acute biliary complication. If not previously performed, ERCP should be offered as an alternative when surgery is contraindicated or refused.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background and Aim
Gallstones are a common finding in the elderly. They are present in 15 % of men and 25 % of women of age 70, with higher prevalences in older patients [1]. Patients asymptomatic at diagnosis present an 18 % risk of developing symptoms during the next 15 years [2]. About 1.5 % of symptomatic patients develop a biliary complication, acute pancreatitis, acute cholecystitis, or acute cholangitis, annually [3]. Although acute pancreatitis and cholecystitis are the two most common gastrointestinal diagnoses causing hospital admissions, their overall in-hospital mortality is below 2 % [4]. Acute cholangitis is a far less frequent disease, but with higher mortality rates [5]. Cholecystectomy is the recommended approach after a biliary complication. In mild cases, it should be performed during the first admission, while severe cases may be delayed until resolution of the acute episode [6, 7].
Management of biliary complications in the elderly may suppose a challenge. Atypical or mild symptoms are more frequently present, comorbidity influences prognosis and treatment options, and surgery in the acute setting involves higher risks compared to younger patients [8]. Treatment decisions are therefore not as straightforward. Life expectancy, surgery risks, and patients’ opinions should be taken into account.
The aim of this study was to describe the natural history of acute biliary complications in the elderly. We intend to describe severity degrees distribution, mortality, and adverse events and harms related to treatment options, focusing on factors influencing treatment decisions and readmission rates related to biliary complications.
Methods
We conducted a single-center retrospective observational analysis in the Fuenlabrada University Hospital. The study protocol was approved by the ethics committee of our center. The STROBE statement recommendations [9] were followed in the design of the study and in the development of this paper.
Patient Selection
All patients 65 or older admitted between June 30, 2004 and June 30, 2013 with a diagnosis of acute pancreatitis, cholangitis, or cholecystitis were suitable for inclusion. Patients were identified using an electronic database which includes all patients discharged or deceased in our hospital and codifies all diagnoses as stated in the discharge reports. Diagnoses are codified according to the International Classification of Disease 9-Clinical Modification (ICD 9-CM). Patients with the following codes were included: 577.0 (acute pancreatitis), 576.1 (acute cholangitis), 575.0, 575.10, 575.12, 575.3, 575.4, 574.00, 574.01, 574.3, 574.4, 574.6, 574.7, and 574.8 (acute cholecystitis). Exclusion criteria were stated as follows:
-
1.
Patients not fulfilling diagnostic criteria for acute pancreatitis according to the 2012 revised Atlanta criteria [10] or diagnostic criteria for acute cholecystitis or acute cholangitis according to the 2013 version of the Tokyo guidelines [11, 12].
-
2.
A previous episode of acute pancreatitis, acute cholecystitis, or acute cholangitis documented in the patient’s medical record.
-
3.
Previous cholecystectomy documented in the patient’s medical record and confirmed in imaging studies.
-
4.
Presence of a pancreatobiliary tumor identified previously or during the acute biliary complication causing admission.
-
5.
Acute pancreatitis of nonbiliary cause or acute acalculous cholecystitis.
-
6.
Lack of follow-up of at least 6 months in patients surviving the first biliary complication, if no new acute biliary event developed earlier.
Data Retrieval
Medical electronic records of all patients presenting inclusion criteria were reviewed. Electronic records include all notes by physicians and nurses during admission and out-patient visits as well as reports of analysis, cultures, imaging studies, and all other procedures performed. Discharge reports after every hospital admission are also kept in the database. After evaluation of exclusion criteria, patients’ data were collected into a newly created database between December 2013 and March 2014. In case of unclear or contradictory statements in the medical record, a consensus decision was met. Based on a previous analysis of the incidence of acute pancreatitis in our area, communicated in the 2012 annual meeting of the Spanish Gastroenterology Association, we estimated 400 patients would be included in our dataset.
Definitions
Severity was estimated according to the Atlanta classification for acute pancreatitis [10] and to the 2013 Tokyo Guidelines for acute cholecystitis [11] and acute cholangitis [12]. Charlson comorbidity index (CCI) is a weighted score of 17 comorbid conditions developed as a 1-year mortality predictor after hospital discharge. CCI variables were defined as described elsewhere [13]. Complications stated as such in discharge reports or, if not stated, identified while reviewing the records were included only if they matched the definitions given in the study protocol (“Appendix”). Complications evaluated included adverse events and harms related to the therapeutic procedures performed (endoscopic retrograde cholangiopancreatography (ERCP), cholecystostomy, or cholecystectomy) or to the acute process and hospital stay. In patients receiving cholecystectomy during their first hospital stay, nosocomial infection and thromboembolic disease appearing before surgery were considered related to hospital stay. If they appeared after surgery, they were considered surgery related. Types of cholecystectomy included only open and laparoscopic. Laparoscopic procedures converted to open surgery were categorized as open. ERCP attempts in which the papilla was not reached (due to previous abdominal surgery, esophageal stenosis…) and there were no cannulation attempts were not categorized as ERCP. Relapse was defined as a new episode of acute pancreatitis, cholangitis, or cholecystitis after discharge according to the diagnostic criteria previously exposed. End of follow-up was defined in the presence of death, relapse, discharge of the out-patient clinic, or, in the absence of the previous, the last medical visit stated in the electronic medical record.
Statistical Analysis
The analysis was performed with STATA (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP). Categorical variables were described with percentages and 95 % confidence intervals. Continuous variables with a normal distribution are presented with mean and standard deviation and those without a normal distribution are summarized with median and interquartile range. Chi-square tests were used to determine differences between categorical variables. Student’s t tests were employed to compare normally distributed continuous variables and Wilcoxon rank sum tests for those not normally distributed. Patients without follow-up were included in the severity distribution and mortality during first admission analysis. They were excluded from all other analysis. Time to event curves were constructed with the Kaplan–Meier method, and comparisons were performed using the log rank test. Multivariate logistic regression was used to estimate the variables that independently predicted nonsurgical treatment. The logistic regression analysis modeled the odds of undergoing cholecystectomy. The main end point was relapse after hospital release. Other end points were mortality during admission and complications and harms appearing during admission.
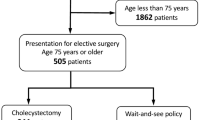
Results
Patient selection process is shown in Fig. 1. Between June 30, 2004 and June 30, 2013, 855 potential eligible patients were identified. A total of 364 (42.6 %) were excluded, 84 (9.8 %) for lacking follow-up. Fifty-one patients (6 %) were excluded due to previous cholecystectomy. All of them presented also a previous acute biliary complication. Four cases of acute acalculous cholecystitis were identified, two were diagnosed postoperatively and two based on imaging studies. Of the 491 included patients, 254 (51.7 %) were women, and the median age was 78.8 (IQR: 71.9–84.7). Patients’ baseline comorbidities according to the CCI are described in Table 1. On univariate analysis, age, heart failure, myocardial infarct, dementia, metastatic, and nonmetastatic tumor were associated with nonsurgical treatment. Logistic regression showed age, myocardial infarct, dementia, diabetes, nonmetastatic tumor, and severe liver disease, defined as cirrhosis with portal hypertension, as independent risk factors for not undergoing surgery (Table 2).
Diagnoses and Severity Distribution
This analysis was performed including patients without follow-up. Acute cholecystitis was observed in 280 (48.9 %) patients, acute pancreatitis in 226 (39.4 %), and acute cholangitis in 67 (11.7 %). Distribution of mild, moderate and severe cases according to the diagnosis is displayed in Table 3. Acute pancreatitis cases were mostly mild 63.7 %; only 6.2 % were severe. Acute cholecystitis and acute cholangitis presented similar distributions; over 80 % of patients presented mild or moderate disease, while 11.4 % of acute cholecystitis and 14.9 % of acute cholangitis were severe (Table 3).
Management
Patients were admitted to a surgery ward in 39.9 % of cases, 32.4 % to a gastroenterology one, and 27.3 % to an internal medicine one. The median length of stay was 9 days (IQR: 7–14). Length of stay for acute pancreatitis was 10 days (7–14), for acute cholecystitis 9 days (6–13), and for acute cholangitis 12 days (8–18). Overall, 5.7 % of patients were treated on the intensive care unit (ICU). Admission to the ICU depended on disease severity. None of the mild cases was admitted, while 4 % (1.6–8.1 %) and 40.4 % (27–54.9 %) of moderate and severe cases, respectively, were treated in the ICU.
Cholecystectomy was the definitive treatment in 231 (47.1 %) patients. It was the only invasive procedure in 204, while 20 received also an ERCP and 5 a cholecystostomy, and in two cases both an ERCP and a cholecystostomy were performed before operating. Surgery was performed during first admission in 109 (47.2 %) patients. The median delay for patients receiving cholecystectomy after discharge was 84 days (41–146.5). Laparoscopic surgery was done in 80.4 % of patients. Isolated cholecystostomy was the treatment of choice in 43 (8.8 %) patients. ERCP alone was performed in 32 (6.5 %) patients. Both ERCP and cholecystostomy without further surgery were performed in 2 (0.4 %) patients. One hundred and eighty-three (37.3 %) patients were handled without employing invasive procedures.
Adverse Events
Harms were identified in 283 (57.6 %) patients, as shown in Table 4. The most common complication related to hospital stay was delirium which appeared in 13 % of patients. Complications classified as “other” were identified in 7 %; most of them were acute urinary retention; six cases presented acute upper gastrointestinal bleedings; one patients suffered a stroke and two cases of acute coronary syndrome were diagnosed. Surgery presented complications in 21 % of operated patients. The most frequent adverse events were categorized as others and included mainly incisional hernias and seromas, while one patient presented a surgical wound hemorrhage. Nosocomial infection was detected in 7 % of patients and ileus in 4 %. No surgery-related thromboembolic events were identified. ERCP was performed in 56 patients; adverse events were diagnosed in 24 % of them. Acute pancreatitis was diagnosed in 16 %. There were no cases of hollow viscus perforation or infection related to the procedure. Fifty patients received a cholecystostomy. Adverse events were present in 24 % of them. Drainage tube dislocation was the most common. Patients without adverse events presented shorter length of stay (8 vs. 12 days; p < 0.001) and lower mortality rates (0 vs. 14.9 %; p < 0.001) compared with patients suffering any adverse event.
In-Hospital Mortality
Mortality during first admission was calculated including patients without follow-up. Thus, of 575 patients, 31 (5.4 %) died during their first admission. Mortality rates according to diagnosis are shown in Table 3. Acute cholangitis presented a mortality rate of 10.4 % (95 % CI 5–20.5 %). Acute cholecystitis and acute pancreatitis presented lower mortality rates, 6.8 % (4.4–10.4 %) and 2.2 % (0.9–5.2 %), respectively. According to severity, mild cases presented a very low mortality, 1.3 % (0.03–2.6 %) while 28.6 % (16.3–40.8 %) of severe cases died. Patients undergoing surgery presented lower in-hospital mortality, but it did not reach statistical significance after adjustment according to baseline characteristics. Mortality was not related to the number of procedures undertaken.
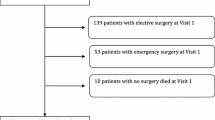
New Biliary Events
Of the 491 included patients, 460 survived the first admission. After discharge, 113 (24.7 %) patients presented a new biliary complication. Acute pancreatitis was diagnosed in 44.3 % of cases, while acute cholecystitis and acute cholangitis were responsible of 30.1 % and 25.7 %, respectively. Overall, 9.7 % of the new episodes were severe. New biliary events were more frequent in patients managed without invasive procedures, 42.3 % (35.4–49.2 %), than in cholecystectomy patients, 9.9 % (5.9–13.8 %) (p < 0.001) and than in ERCP patients, 19.4 % (4.6–34.1 %) (p = 0.01). Differences between ERCP and cholecystectomy did not reach statistical significance (p = 0.15) (Fig. 2). In patients managed conservatively, 25.9 % of all relapses were diagnosed in the first 3 months after discharge.
Kaplan–Meier unadjusted 60-month probability of developing new biliary events. Cholecystectomy includes patients receiving cholecystectomy plus any other treatment; ERCP includes patients receiving ERCP alone or with cholecystostomy; “Other” includes patients receiving cholecystostomy alone or supportive care only
Among patients not presenting new biliary events, 38 (8.3 %) died during follow-up, 37 (8 %) were lost after at least 6 months of follow-up, and 272 (59.1 %) were still being followed or had been discharged from the outpatient clinic. Median time of follow-up for patients without further biliary complications was 22.1 months (11.8–44.7).
Discussion
To our knowledge, this is the first work describing severity distribution of acute biliary events in the elderly according to the 2012 acute pancreatitis and Tokyo 2013 guidelines definitions. A series of patients validating the new acute pancreatitis classification was published in 2012 [14]. It included 137 patients, 69 % mild, 20 % moderately severe, and 11 % severe. Our severity distribution shows a higher number of moderately severe cases, due to systemic complications relating to baseline comorbidities. The very low mortality rate of mild cases mirrors previously published data. On the other hand, severe cases presented a low mortality rate of 7.1 %, but, with a total number of 14 cases of severe acute pancreatitis in our sample, such estimate should be taken with caution. The proportions of severe cases in acute cholecystitis and acute cholangitis are similar to those previously described [15].
Overall, 24.7 % of surviving patients presented a new acute biliary event. Relapse depended heavily on the assigned treatment. Our results resemble those published previously. A study including over 8,000 medicare beneficiaries 65 or older presenting with acute pancreatitis between 1996 and 2005 showed that patients undergoing cholecystectomy presented a 3.8 % gallstone-related readmission rate while, in patients not receiving surgery, it peaked to 43.5 % in a 2-year follow-up [16]. Another similarly designed study by the same group focusing on acute cholecystitis (nearly 30,000 subjects) presented analogous results. Cholecystectomy patients presented a 2-year relapse rate of 4.4 %, while 38 % of patients not receiving surgery required readmission [17]. Several reasons may contribute to our higher relapse rate after surgery. The main one might be longer follow-up in our patients. The 2-year relapse rate in our cholecystectomy group is 7.2 % (3.8–10.6 %), which is similar to those previously described. Other possible causes like common bile duct evaluation before surgery or its exploration during surgery were not retrieved.
The 47.1 % cholecystectomy rate found in our center is below those reported by Riall et al. and Trust et al. In those studies, 57 and 75 % of patients underwent cholecystectomy during admission. Age and comorbidities of patients included in these analyses are similar to patients described in ours. Decision-making process is not usually stated in medical records. Surgery risks might have been deemed too high by the surgical team or by the attending physicians in cases managed in medicine wards. Patients might have declined a recommended surgical procedure. Our data do not allow us to identify the motives of our low cholecystectomy rate.
Over 50 % of our patients presented at least one complication. This high proportion of patients might be related to their advanced age, the number of invasive procedures performed, and the exhaustive review of medical records. The Spanish National Study of Adverse Events analyzed retrospectively data retrieved from 24 hospitals along the country. Medical care-related harms were identified in 9.3 % of the over 5,000 screened patients [18]. Other authors evaluating harms in surgical wards estimated percentages between 11 and 17 % [19, 20]. Definitions of harms and the methods to measure them are still a matter of debate [21]. Some measures (e g, patient safety indicator method) focus on specific types of harms, while others, like the global trigger tool, focus on all-cause harm. Different methods offer very different proportions of patients affected, making comparisons difficult. Thus, in the same sample of patients, four times more adverse events were identified using the global trigger tool than using the patient safety indicator method [22]. Our retrieval of adverse events did not follow any of the standardized harm detection methods, but can be categorized as an all-cause harm approach. Some of the most frequent complications included in our analysis were present at admission, and others are attributable to the disease itself (e.g., delirium). Some procedure-related events did not suppose a longer length of stay or further procedures (e.g., drainage tube dislocation). Until consensus is gained, we favor an all-cause method, as harms identified might later be classified according to its causes or possibility of avoidance.
There are a few drawbacks in the present study. First of all, this is a retrospective study from a single center. Our data, especially those regarding treatment decisions, may not adequately represent trends in our country. The 10 years scanned may not only represent contemporary management tendencies. The patient selection may have overestimated the proportion of moderate and severe cases. Although all cases were reviewed and those not fulfilling updated diagnostic criteria were excluded, thus reducing false-positive diagnoses, misdiagnosed patients could not be retrieved. As exposed before, the harm rate identified in our study may be difficult to compare with similar studies depending on the measure employed.
We consider our work offers a complete picture of acute biliary events in the elderly in our area. Severity distribution resembles findings from studies including younger samples. Thus, age and baseline comorbidities influence the overall mortality rates, over 5 % in acute cholangitis and cholecystitis. Efforts should be placed on minimizing avoidable harms, and unavoidable ones should be expected and diagnosed early. Treatment decisions show a major influence in prognosis after the first event. Patients should be informed about risks and options. Cholecystectomy should be offered, regardless of age, unless the patient presents a poor performance status or has a short life expectancy. If surgical risk is deemed too high and ERCP was not included in the management of the acute episode, it should be considered a plausible option to decrease the relapse risk.
References
Khang KU, Wargo JA. Gallstone disease in the elderly. In: Rosenthal RA, Zenilman ME, Katlic MR, eds. Principles and practice of geriatric surgery. Berlin: Springer; 2001:690–710.
Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982;307:798–800.
McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985;202:59–63.
Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187.
Rosing DK, De Virgilio C, Nguyen AT, El Masry M, Kaji AH, Stabile BE. Cholangitis: analysis of admission prognostic indicators and outcomes. Am Surg. 2007;73:949–954.
Tenner S, Baillie J, DeWitt J, Vege SS. American College of Gastroenterology. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol. 2013;108:1400–1415.
Yamashita Y, Takada T, Strasberg SM, et al. TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:89–96.
Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433–435.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Banks PA, Bollen TL, Dervenis C, et al. Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111.
Yokoe M, Takada T, Strasberg SM, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:35–46.
Kiriyama S, Takada T, Strasberg SM, et al. TG13 guidelines for diagnosis and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2013;20:24–34.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383.
Talukdar R, Clemens M, Vege SS. Moderately severe acute pancreatitis: prospective validation of this new subgroup of acute pancreatitis. Pancreas. 2012;41:306–309.
Kimura Y, Takada T, Strasberg SM, et al. TG13 current terminology, etiology, and epidemiology of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013;20:8–23.
Trust MD, Sheffield KM, Boyd CA, et al. Gallstone pancreatitis in older patients: Are we operating enough? Surgery. 2011;150:515–525.
Riall TS, Zhang D, Townsend CM Jr, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010;210:668–677.
Aranaz-Andrés JM, Aibar-Remón C, Vitaller-Burillo J, et al. Impact and preventability of adverse events in Spanish public hospitals: results of the Spanish National Study of Adverse Events (ENEAS). Int J Qual Health Care. 2009;21:408–414.
Aranaz-Andrés JM, Ruiz-López P, Aibar-Remón C, et al. Adverse events in general and digestive surgery departments in Spanish hospitals. Cir Esp. 2007;82:268–277.
Júdez Legaristi D, Aibar Remón C, Ortega Maján MT, Aguilella Diago V, Aranaz Andrés JM, Gutiérrez Cía I. Incidence of adverse events in a general surgery unit. Cir Esp. 2009;86:79–86.
Parry G, Cline A, Goldmann D. Deciphering harm measurement. JAMA. 2012;307:2155–2156.
Classen DC, Resar R, Griffin F, et al. “Global trigger tool” shows that adverse events in hospitals may be ten times greater than previously measured. Health Aff. 2011;30:581–589.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Adverse events and harms definitions:
Thromboembolic disease
Deep vein thrombosis confirmed with Doppler ultrasound or pulmonary embolism confirmed with computer tomography, gammagraphy, or cardiac ultrasound.
Acute kidney injury
Accepted if serum creatinine rises abruptly from baseline levels by 0.5 mg/dl or increases by 50 % or more.
Decompensation of chronic disease
Decompensation of previously known heart failure, kidney failure, chronic obstructive pulmonary disease, or hematological disease needing specific therapy, different from the patient’s usual treatment.
Delirium
Accepted if suggestive symptoms (acute, fluctuating change in mental status, altered level of consciousness, disorganized thinking) were recorded and specific pharmacological treatment or physical restraints were prescribed.
Nosocomial infection
Development of infection at least 3 days after admission; accepted if a positive urine or blood culture was present, a positive C difficile toxin assay and diarrhea were present or respiratory symptoms with a newly developed infiltrate on the chest X ray appeared.
Other complications
Newly diagnosed problems or diseases stated as secondary to the hospital stay or to the pharmacological treatments prescribed during hospital stay.
Post-ERCP pancreatitis
Condition presenting the following criteria: (1) new or worsened abdominal pain, (2) new or prolongation of hospitalization for at least 2 days, and (3) serum amylase or lipase three times or more the upper normal limit, measured 24 h after the procedure.
ERCP-related digestive bleeding
Decrease of at least 1 g/dl in hemoglobin value after ERCP and hematemesis, melena, or endoscopic demonstration of papillary bleeding or bleeding stigmata.
Perforation
Abdominal pain and radiological or surgical proof of a hollow viscus perforation.
Acute biliary infection
Development of new signs and symptoms fulfilling the 2013 Tokyo guidelines criteria for the diagnosis of acute cholangitis or acute cholecystitis.
Other complications related to the ERCP
Problems arising after the procedure and stated as secondary to the procedure itself (including sedation).
Cholecystostomy-related bleeding
Decrease of at least 1 g/dl in hemoglobin value after cholecystostomy and overt superficial bleeding, passage of melena, radiological documentation of hemoperitoneum, radiological, or endoscopic proof of hemobilia.
Biliary leak
Radiological or surgical proof of passage of bile to the peritoneum
Hollow viscus perforation
Abdominal pain and radiological or surgical proof of a hollow viscus perforation following a cholecystostomy.
Drainage tube dislocation
Involuntary removal or dislocation of the drainage tube, abandoning its intravesicular location.
Pneumothorax
Abnormal collection of air in the pleural space appearing after cholecystostomy.
Sepsis
Development of sepsis criteria (or worsening of condition to severe sepsis or septic shock if sepsis criteria were present previous to cholecystostomy) after the procedure.
Other cholecystostomy-related complications
Problems arising after the procedure and stated as secondary to the procedure itself (including sedation).
Surgery-related nosocomial infection
Development of infection at least 3 days after admission, accepted if a positive urine or blood culture was present, a positive C difficile toxin assay and diarrhea were present or respiratory symptoms with a newly developed infiltrate on the chest X ray appeared after cholecystectomy.
Surgical wound infection
Development of local signs of infection and/or a positive culture of the wound exudate.
Surgery-related thromboembolic disease
Deep vein thrombosis confirmed with Doppler ultrasound or pulmonary embolism confirmed with computer tomography, gammagraphy, or cardiac ultrasound appearing after cholecystectomy.
Ileus
Abdominal distention accompanied by nausea, constipation, and an abnormal bowel abdominal auscultation without an obstructive cause.
Bile duct injury
Endoscopic or radiological demonstration of a biliary leak or stenosis after cholecystectomy.
Other surgery-related complications
Problems arising after the surgical procedure and stated as secondary to the procedure itself (including sedation).
Rights and permissions
About this article
Cite this article
García-Alonso, F.J., de Lucas Gallego, M., Bonillo Cambrodón, D. et al. Gallstone-Related Disease in the Elderly: Is There Room for Improvement?. Dig Dis Sci 60, 1770–1777 (2015). https://doi.org/10.1007/s10620-014-3497-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3497-4