Abstract
Ovarian cancer is one of the gynecological malignancies ranked third in incidence and first in mortality in the world. Homoboxb8 (HOXB8) has been demonstrated to play crucial roles in various tumors. However, the function of HOXB8 in ovarian cancer remains to be addressed. Quantitative real-time polymerase chain reaction, immunohistochemistry staining and western blot assays demonstrated that HOXB8 expression was up-regulated in human ovarian cancer tissues and cells. The results of CCK-8 and colony formation assays indicated that HOXB8 promoted the proliferation of ovarian cancer cells. Transwell and immunofluorescence (IF) staining assay demonstrated that HOXB8 promoted the migration and invasion of ovarian cancer cells. Importantly, mechanism analysis implied that HOXB8 increased the expression of β-catenin and phosphorylation of STAT3, and the downstream target molecules of Cyclin D1, c-Myc, TWIST1, MMP7 and MMP9, indicating that HOXB8 could promote the activation of Wnt/β-catenin and STAT3 pathways. Moreover, HOXB8 knockdown suppressed xenograft tumor growth, and inhibited the levels of HOXB8 and Ki-67, while increasing the level of E-cadherin in mice. In conclusion, HOXB8 promotes cell proliferation, migration and invasion through modulating Wnt/β-catenin and STAT3 signaling pathways in ovarian cancer, suggesting that HOXB8 may provide a promising target for the therapy of ovarian cancer.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is one of the gynecological malignancies ranked third in incidence and first in mortality in the world (Siegel et al. 2019).According to statistics, 238,700 new cases of ovarian cancer occur worldwide each year, and 151,900 deaths occur annually (Torre et al. 2018).Ovarian cancer is characterized by rapid progression, early metastasis, strong aggressiveness and poor prognosis, and the 5-year survival rate and tumor-free rate are always around 15–30% (Barnett 2016; Gadducci et al. 2019).Currently, platinum-based chemotherapy, supplemented as satisfactorily as possible after tumor cell reduction, is the standard treatment for ovarian cancer. However, the recurrence rate of ovarian cancer patients is very high clinically, and the patients with recurrence are not sensitive to platinum chemotherapy. If ovarian cancer can be detected and treated at an early stage, it can significantly improve the prognosis of patients with ovarian cancer. Therefore, finding relevant novel therapeutic targets and exploring the molecular mechanism of ovarian cancer progression are of great significance for patients with ovarian cancer.
The Homeobox (HOX) gene is a 183 bp sequence encoding 61 amino acid homology domains. HOX protein plays an important role in tumorigenesis by regulating cell growth, migration, cell cycle and apoptosis (Eoh et al. 2017; Morgan and El-Tanani 2016; Wang et al. 2016). Homoboxb8 (HOXB8) is a family of members of HOX. Studies have shown that HOXB8 is abnormally expressed in human tumors, and its expression is closely related to the occurrence, development and metastasis of osteosarcoma, gastric cancer, colorectal cancer, and other malignant tumors (Ding et al. 2017; Guo et al. 2019; Shen et al. 2016). Literature studies have shown that HOXB8 is often highly expressed in ovarian serous carcinoma, a is related to the shortened survival of metastatic serous carcinoma (Stavnes et al. 2013). However, its role in ovarian cancer and its mechanism are still unclear. The purpose of this study is to study its expression in human ovarian cancer cells and its biological effects. Our results show that HOXB8 gene can regulate the occurrence and metastasis of ovarian cancer by regulating Wnt/β-catenin and STAT3 signaling pathways. Therefore, HOXB8 may be a new target for the treatment of ovarian cancer.
Materials and methods
Patients and tissue samples
55 pairs of ovarian cancer tissues and matched adjacent normal ovarian tissues were collected from ovarian cancer patients who underwent resection at Wuhan NO.1 Hospital. All the collected tissue samples were stored at − 80 °C before use. This study was approved by the Ethics Committee of Wuhan NO.1 Hospital and the written informed consent of each patient was obtained before the surgery.
Cell culture and transfection
Human ovarian cancer cell lines (CAOV3, SKOV3, OVCAR4, A2780, TOV-21G) and normal ovarian epithelial cell line HOSEpiC were purchased from the American Type Culture Collection (ATCC, Manassas, VA, USA). All cells were grown in DMEM medium (Gibco, Grand Island, NY, USA) containing with 10% fetal bovine serum (FBS, Gibco), 100 U/ml penicillin and 100 µg/ml streptomycin (Sigma, St. Louis, MO, USA) in a humidified incubator containing 5% CO2 at 37 °C. The HOXB8 cDNA sequence was cloned into the pcDNA3.1 vector and was transfected into cells to up-regulate HOXB8 expression (labeled as HOXB8) and pcDNA3.1 empty vector was used as the control (labeled as Vector). ShRNAs targeting HOXB8 and control shRNA (shNC) were designed and synthesized to down-regulate HOXB8 expression (shHOXB8#1 and shHOXB8#2) by Genepharm Co., Ltd. (Shanghai, China). The HOXB8 shRNA sequences were as follows: shHOXB8#1, 5′-GCTCTTATTTCGTCAACTCACTGTTCTCC-3′; and shHOXB8#2, 5′-GAGCTGGAGAAGGAGTTCCTATTTAATCC-3′. The plasmids were transfected into cells by Lipofectamine® 2000 (Invitrogen, NY, USA) according to the manufacturer’s protocols.
Quantitative real-time polymerase chain reaction (qRT-PCR)
Total RNA of tissues or cells was isolated using Trizol reagent (Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. cDNA was synthesized using a PrimeScript™ 1st Strand cDNA Synthesis kit (Takara, Dalian, China). RT-qPCR was performed on the ABI 7500 real-time PCR system (Applied Biosystems, Foster City, CA, USA) with the SYBR Green PCR kit (Takara, Dalian, China). The relative mRNA expression levels were performed using the 2−ΔΔCt method with GAPDH as an internal control. The sequences of primers were as follows: HOXB8, forward: 5′-ACGTGCTTCTTTGTAATGACCA-3′, and reverse: 5′-TGTAACAATTGCCCACAGCG-3′; GAPDH forward, 5′-GGAGTCCACTGGCGTCTT−3′ and reverse, 5′-AGTCCTTCCACGATACCAA-3′.
Immunohistochemistry (IHC) staining
Tissue sections were deparaffinized and dehydrated using graded ethanol solutions. Then the tissue specimens were incubated with 3% H2O2, subjected to primary antibody targeting HOXB8 (dilution 1:100, BS-6539R, Bioss), E-cadherin (dilution 1:50, ab1416, Abcam, Cambridge,MA, USA ) and Ki-67 (dilution 1:200, ab15580, Abcam) overnight. After washing with phosphate-buffered saline (PBS), the sections were covered with the horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG (dilution 1:1000, ab6721, Abcam) secondary antibody, detected with 3,3’-diaminobenzidine (DAB), and counterstained with hematoxylin.
Western blot
Total proteins were extracted with RIPA lysis buffer (Sigma) and Protein concentration was determined by the BCA protein assay kit (Thermo Scientific, Rockford, Illinois). Equal amounts of the protein were separated on a 10% SDS-polyacrylamide gel electrophoresis (SDS-PAGE). The proteins were transferred onto the polyvinylidene difluoride (PVDF) membranes (Millipore) and blocked with 5% nonfat milk for 1 h at room temperature. Then, the membranes were incubated with the following primary antibodies overnight at 4 °C: anti-HOXB8 (dilution 1:500, BS-6539R, Bioss), anti-β-catenin (dilution 1:1000, ab16051, Abcam), anti-CyclinD1 (dilution 1:200, ab16663, Abcam), anti-c-Myc (dilution 1:1000, ab32072, Abcam), STAT3 (dilution 1:2000, ab119352, Abcam), p-STAT3 (dilution 1:5000, ab76315, Abcam), anti-Twist (dilution 1:1000, ab50887, Abcam), anti-MMP-7 (dilution 1:1000, ab5706, Abcam), anti-MMP9 (dilution 1:1000, ab76003, Abcam), and anti-GAPDH (dilution 1:10,000, ab181602, Abcam). Subsequently, the membranes were incubated with the HRP-conjugated secondary antibody for 1 h at room temperature. The protein bands were developed using the enhanced chemiluminescence reagent (Pierce, Rockford, IL, USA).
Cell proliferation assays
For CCK-8 assay, 2000 cells/well were seeded at a 96-well plate. 10 µl of CCK-8 solution (C0038, Beyotime biotechnology, China) was added to each well at different times points (0, 24, 48, and 72 h) according to the manufacturer’s protocols. After incubation for 2 h at 37 °C, the absorbance was measured by a microplate reader at 450 nm. For colony formation assay, 500 cells were seeded in a -well plate and the medium was replaced every 3 days for 2 weeks. Then the colonies were fixed with 4% paraformaldehyde and stained with 0.1% crystal violet (Sigma–Aldrich, St. Louis, MO, USA). The number of visible colonies were manually counted and photographed.
Cell migration and invasion assays
Cell migration assays were conducted using Transwell chambers (8 μm pore size; Corning Co. NY, USA). The lower chamber was filled with 600 µl of DMEM containing 10% FBS. 1 × 104 cells were suspended in 200 µl serum-free DMEM and plated into the upper chamber. After incubation for 24 h, the number of cells on the lower surface of the polycarbonate membranes was fixed with 4% paraformaldehyde and stained visually with 0.1% crystal violet, then counted and photographed under a light microscope. Cell invasion assays were done using the same procedure except that the upper chambers were pre-coated with Matrigel (BD Biosciences, CA, USA).
Immunofluorescence (IF) staining
2 × 104 cells were seeded on the culture slides in 6-well plates for IF staining. After incubation for 24 h, the cells attached to the slides were washed 3 times in PBS, and then fixed in 4% paraformaldehyde at 4 °C for 20 min. Subsequently, the cells were infiltrated with 2% Triton X-100 (Sigma-Aldrich) and sealed with 2% fetal bovine serum albumin (BSA, Sigma-Aldrich) for 30 min. The cells were incubated with the following primary antibodies at room temperature overnight: anti-E-cadherin (dilution 1:500, ab40772, Abcam) and N-cadherin (dilution 1:500, ab98952, Abcam). Then the cells were incubated with anti-mouse IgG secondary antibody (dilution 1:1000, ab150117) for 2 h. Later, the nuclei were counterstained with DAPI for 10 min. Cells were photographed under a fluorescence microscope. (Olympus, Japan).
Xenograft tumor model
All animal experiments were performed in accordance with the Institutional Animal Care and Use Committee of Wuhan NO.1 Hospital. 1 × 106 SKOV3 cells transfected with shHOXB8 or shNC were suspended in 200 µl of PBS and subcutaneously injected into the left flank of 6-week-old female BALB/c nude mice (n=6 per group). Tumor size was measured every 3 days using an electronic caliper, and calculated according to the formula: Volume = length × width2 × 0.5. The mice were sacrificed and tumors were removed and individually weighed after 4 weeks.
Statistical analysis
Data analysis was processed using GraphPad Prism 7 (GraphPad Inc., La Jolla, CA, USA) from more than three independent repeats and represented as the mean ± the standard deviations (SD). Comparisons between two groups or among multiple groups were conducted using Student’s t-test or one-way analysis of variance (ANOVA) with Tukey post doc analysis. P < 0.05 was considered as statistically significant.
Results
HOXB8 expression is upregulated in ovarian cancer tissues and cells
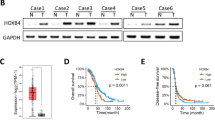
To determine HOXB8 expression levels in ovarian cancer, 55 ovarian cancer tissues and matched adjacent normal ovarian tissues were examined using qRT-PCR. The results suggested that the mRNA level of HOXB8 in ovarian cancer tissues are significantly increased compared with non-cancerous tissues (Fig. 1A). As also evidenced through IHC staining, HOXB8 protein was significantly higher in ovarian cancer tissues in relative than the matched adjacent ovarian tissues (Fig. 1B). In addition, the mRNA levels of HOXB8 were significantly increased in ovarian cancer cell lines (CAOV3, SKOV3, OVCAR4, A2780, TOV-21G) compared to the normal ovarian epithelial cell line HOSEpiC (Fig. 1C). And we found that that among all cancer cell lines, HOXB8 was the least expressed in A2780 cells and relatively higher in SKOV3 cells (Fig. 1C). Consistently, the WB experiment also yielded similar results (Fig. 1D). Therefore, the A2780 cell line was selected as candidate cell line for HOXB8 overexpression, while SKOV3 cell line was selected as candidate cell line for HOXB8 knockdown. Together, the above observations reveal that HOXB8 expression is upregulated in ovarian cancer tissues and cells.
HOXB8 expression is upregulated in ovarian cancer tissues and cells. A The mRNA level of HOXB8 in 55 paired ovarian cancer tissues and matched adjacent normal ovarian tissues were measured by qRT-PCR. B The HOXB8 level was detected by staining with IHC (scale bar = 200 μm, magnification, ×100). C, D The mRNA (F) and protein (G) levels of HOXB8 in in ovarian cancer cell lines (CAOV3, SKOV3, OVCAR4, A2780, TOV-21G) and the normal ovarian epithelial cell line HOSEpiC were determined by qRT-PCR and western blot assays. Data are shown as mean ± SD; *P < 0.05, **P < 0.01 and ***P < 0.001
HOXB8 promotes the proliferation of ovarian cancer cells
To provide further evidence for the effects of HOXB8 in ovarian cancer development, we overexpressed the HOXB8 in A2780 cells and knockdown HOXB8 in SKOV3 cells. The transfected efficiencies were confirmed by qRT-PCR and western blot assays. As displayed in Fig. 2A, B, HOXB8 expression was significantly increased in HOXB8 group compared to the vector group, which indicated that overexpression of HOXB8 is successful in A2780 cells (Fig. 2A, B). Moreover, each shRNA could effectively knock down HOXB8 expression, sh-HOXB8#2 exerted the best knockdown efficiency in SKOV3 cells therefore was selected for further functional and mechanistic investigations (Fig. 2A, B). After that, we observed through CCK-8 assay that overexpression of HOXB8 significantly promoted the growth rate of A2780 cells while knockdown of HOXB8 prohibited the growth rate of SKOV3 cells (Fig. 2C). Additional colony formation assay revealed that elevated HOXB8 expression resulted in an increase in colony number in A2780 cell line, whereas HOXB8 knockdown resulted in fewer colonies in the SKOV3 cell line (Fig. 2D). These results demonstrate that HOXB8 can promote the proliferation of ovarian cancer cells.
HOXB8 promotes the proliferation of ovarian cancer cells. A, B QRT-qPCR (A) and western blot (B) assays were used to measure the transfection efficiency of HOXB8 in A2780 and SKOV3 cells. C CCK-8 assay was used to evaluate the cell viabilities of A2780 and SKOV3 cells. D Colony formation assay was used to determine the number of cell clones in A2780 and SKOV3 cells. Data are shown as mean ± SD; *P < 0.05, **P < 0.01 and ***P < 0.001
HOXB8 promotes the migration and invasion of ovarian cancer cells
Transwell assay was performed to evaluate the migration and invasion of ovarian cancer cells. Our results indicated that upregulation of HOXB8 obviously increased the migration and invasion abilities of A2780 cells whereas downregulation of HOXB8 observed the opposite results in SKOV3 cells (Fig. 3A, B). Subsequent immunofluorescence analysis implied that overexpression of HOXB8 significantly reduced the expression of epithelial markers E-cadherin, whereas increased the expression levels of mesenchymal markers N-cadherin in A2780 cells. However, knockdown of HOXB8 exerted an opposing effect in SKOV3 cells (Fig. 3C). These data indicate that HOXB8 enhances the migratory and invasive capabilities of ovarian cancer cells.
HOXB8 promotes the migration and invasion of ovarian cancer cells. A, B Transwell assay was used to evaluate the migration and invasion capabilities of A2780 and SKOV3 cells (scale bar = 50 μm, magnification, ×400). (C) The levels of E-cadherin and N-cadherin in A2780 and SKOV3 cells were measured by immunofluorescence analysis. Data are shown as mean ± SD; *P < 0.05, **P < 0.01 and ***P < 0.001
HOXB8 may promote the progression of ovarian cancer by regulating Wnt/β-catenin and STAT3 signaling pathways
The Wnt/β-catenin and STAT3 signaling pathways are classical intracellular signaling pathway involved in tumorigenesis and metastasis (Kamran et al. 2013; Zhan et al. 2017). The dysregulation of Wnt/β-catenin and STAT3 signaling pathways has been reported in ovarian cancer, and is believed to regulate cell proliferation, migration and invasion of ovarian cancer (Arend et al. 2013; Liang et al. 2020). Since it has been reported that HOXB8 affects Wnt/β-catenin and STAT3 signaling pathways to regulate tumor progression (Guo et al. 2019; Li et al. 2019; Wang et al. 2019), we explored whether HOXB8 promotes proliferation, migration and invasion through the above pathways in ovarian cancer. The results of western blot analysis revealed that the overexpression of HOXB8 resulted in increased key members of Wnt/β-catenin and STAT3 signaling pathways including β-catenin and phosphorylation of STAT3 (Fig. 4A). Further western blot results observed the notable up-regulation protein levels of Cyclin D1 and c-Myc (Fig. 4A) when A2780 cells were overexpressed HOXB8, all of them are the critical targeted molecules of Wnt/β-catenin signaling and related to cell growth (Yang et al. 2015). Meanwhile, the protein levels of downstream TWIST1, MMP7 and MMP9 were also strikingly increased following upregulation of HOXB8 treatment in A2780 cells, all of them are closely correlated with cell invasion and migration (Fig. 4A). Consistently, knockdown of HOXB8 inhibited the Wnt/β-catenin and STAT3 signaling pathways and downstream proteins in SKOV3 cells (Fig. 4B). Together, these findings suggest that HOXB8 might modulate ovarian cancer progression through Wnt/β-catenin and STAT3 signaling pathways.
HOXB8 may promote the progression of ovarian cancer by regulating Wnt/β-catenin and STAT3 signaling pathways. A The levels of β-catenin, p-STAT3, STAT3, c-Myc, cyclin D1, TWIST1, MMP7 and MMP9 in A2780 cells were determined by western blot assay. B The levels of β-catenin, p-STAT3, STAT3, c-Myc, cyclin D1, TWIST1, MMP7 and MMP9 in SKOV3 cells were determined by western blot assay. Data are shown as mean ± SD; *P < 0.05, **P < 0.01 and ***P < 0.001
Knockdown of HOXB8 inhibits the growth of ovarian cancer xenograft tumors in vivo
To further validate the significance of HOXB8 on tumor growth in vivo, xenograft tumor model was established. SKOV3-shHOXB8 and its control (shNC) were subcutaneously injected into the nude mice. Tumor sizes and weights in shHOXB8 group derived from SKOV3 cells were reduced compared to the shNC group (Fig. 5A–C). Moreover, the results of IHC assay demonstrated that HOXB8 and Ki-67 levels were markedly reduced while E-cadherin level was significantly increased in tumor tissues from the shHOXB8 group compared to the shNC group (Fig. 5D). All observations in vivo suggested that knockdown of HOXB8 inhibited tumorigenesis of ovarian cancer.
Knockdown of HOXB8 inhibits the growth of ovarian cancer xenograft tumors in vivo. A Photographs of tumors excised from the mice injected with SKOV3 cells transfected with shNC or shHOXB8. B, C Tumor growth curves (B) and weight (C) of mice injected with SKOV3 cells. (D)The levels of HOXB8, Ki-67 and E-cadherin in tumors from mice injected with SKOV3 cells were evaluated by IHC staining (scale bar = 200 μm, magnification, ×100). Data are shown as mean ± SD; *P < 0.05, **P < 0.01 and ***P < 0.001
Discussion
Heredity, poor lifestyle and environmental factors are the major risk factors for ovarian cancer (Mallen et al. 2018). Because the symptoms of early ovarian cancer are not obvious and hidden, 70% of the patients have been diagnosed as clinical advanced stage (Stewart et al. 2019). In recent years, the clinical application of targeted drugs has significantly improved the therapeutic effect of ovarian cancer patients (Cortez et al. 2018). Unfortunately, treatment for patients with advanced ovarian cancer is far from satisfactory, and their overall survival rate is relatively low (Siegel et al. 2019). A better understanding of the molecular mechanisms of ovarian cancer is critical for better preclinical risk assessment, early diagnosis, effective treatment, and prognostic prediction.
Increasing evidences have revealed that HOXB8 plays a variety of biological functions in in tumor initiation and progression. For instance, Ding. et al. reported that HOXB8 is highly expressed in metastatic tissues compared to non-metastatic tissues, and overexpression of HOXB8 can promote the migration, invasion and epithelial-mesenchymal transformation (EMT)of gastric cancer cells (Ding et al. 2017). Li. et al. suggested that HOXB8 knockout can suppress the proliferation and migration of colorectal cancer (CRC) cells through the Wnt/β-catenin signaling pathway, and down-regulate c-myc, CyclinD1 and other factors (Li et al. 2019). HOXB8 also can induce cellular proliferation, invasion and EMT in vitro as well as carcinogenesis and metastasis in vivo by activating STAT3 in CRC (Wang et al. 2019). A recent study indicates that HOXB8 enhances colorectal cancer invasiveness through activating BACH1 (Ying et al. 2020). In addition, HOXB8 knockdown can inhibit the occurrence and metastasis of osteosarcoma by regulating the Wnt/β-catenin signaling pathway (Guo et al. 2019).These findings suggest that HOXB8 may be a potential biomarker for cancer response detection and prognosis evaluation. Of note, in serous ovarian cancer, higher HOXB8 expression in effusion is associated with shorter overall survival and progression-free survival (Stavnes et al. 2013). Indeed, the research about tumorigenesis role of HOXB8 is little in ovarian cancer. In the present study, the HOXB8 level was confirmed to be upregulated in ovarian cancer tissues and cells. Functional experiments validated that HOXB8 promoted the proliferation, migration and invasion of ovarian cancer cells in vitro. In addition, HOXB8 knockdown inhibited the growth of xenograft tumors in vivo. These data reveal for the first time the role of HOXB8 in ovarian cancer as an oncogenic gene.
Wnt/β-catenin signaling pathway is involved in various ovarian cancer progression, such as proliferation, migration and invasion (Arend et al. 2013; Gatcliffe et al. 2008). C-myc, cyclin D1 and MMP-7 are the recognized target genes of β-catenin/TCF transcription factor complex, and are the main carcinogenic drivers of tumor growth and metastasis (Ghosh et al. 2019). Activation of STAT3 can enhance the proliferation, invasion, angiogenesis and drug resistance of ovarian cancer cells, providing an attractive target for ovarian cancer treatment and prevention (Liang et al. 2020; Saini et al. 2017). However, a large part of the upstream regulatory mechanism of Wnt/β-catenin and STAT3 are still unknown. Previous studies have shown that HOXB8 can regulate the Wnt/β-catenin and STAT3 signaling pathways to promote tumor progression (Guo et al. 2019; Li et al. 2019; Wang et al. 2019), so we hypothesized that the role of HOXB8 in ovarian cancer may be realized through the above mechanisms. Our further mechanism research focused and found that HOXB8 promoted β-catenin, p-STAT3 and its downstream proliferation, migration and invasion related proteins. These evidences imply that the mechanism of HOXB8 regulating the proliferation, migration and invasion of ovarian may be partly through Wnt/β-catenin and STAT3 signaling pathways.
Conclusions
In the present study, we reported that HOXB8 is highly expressed in ovarian cancer and cells. We prove for the first time that HOXB8 promotes the cell growth, migration, and invasion of ovarian cancer in vitro, as well as tumor formation in vivo. In addition, our data indicate that HOXB8 exerts its carcinogenic function by activating Wnt/β-catenin and STAT3 signaling pathways, which suggests the potential of HOXB8 as a predictive biomarker or therapeutic target for ovarian cancer.
Data availability
All data generated or analyzed during this study are included in this published article.
Code availability
Not Applicable.
References
Arend RC, Londoño-Joshi AI, Straughn JM, Buchsbaum DJ (2013) The Wnt/β-catenin pathway in ovarian cancer: a review. Gynecol Oncol 131:772–779. https://doi.org/10.1016/j.ygyno.2013.09.034
Barnett RJTL (2016) Ovar Cancer 387:1265
Cortez AJ, Tudrej P, Kujawa KA, Lisowska KM (2018) Advances in ovarian cancer therapy. Cancer Chemother Pharmacol 81:17–38. https://doi.org/10.1007/s00280-017-3501-8
Ding W-J, Zhou M, Chen M-M, Qu C-Y (2017) HOXB8 promotes tumor metastasis and the epithelial–mesenchymal transition via ZEB2 targets in gastric cancer. J Cancer Res Clin Oncol 143:385–397. https://doi.org/10.1007/s00432-016-2283-4
Eoh KJ, Kim HJ, Lee J-Y, Nam EJ, Kim S, Kim SW, Kim YT (2017) Dysregulated expression of homeobox family genes may influence survival outcomes of patients with epithelial ovarian cancer: analysis of data from the cancer genome atlas. Oncotarget 8:70579–70585. https://doi.org/10.18632/oncotarget.19771
Gadducci A et al (2019) Current strategies for the targeted treatment of high-grade serous epithelial ovarian cancer and relevance of BRCA mutational status. J Ovar Res 12:9. https://doi.org/10.1186/s13048-019-0484-6
Gatcliffe TA, Monk BJ, Planutis K, Holcombe RF (2008) Wnt signaling in ovarian tumorigenesis. Int J Gynecol Cancer 18:954. https://doi.org/10.1111/j.1525-1438.2007.01127.x
Ghosh N, Hossain U, Mandal A, Sil PC (2019) The Wnt signaling pathway: a potential therapeutic target against cancer. Ann N Y Acad Sci 1443:54–74. https://doi.org/10.1111/nyas.14027
Guo J, Zhang T, Dou D (2019) Knockdown of HOXB8 inhibits tumor growth and metastasis by the inactivation of Wnt/β-catenin signaling pathway in osteosarcoma. Eur J Pharmacol 854:22–27. https://doi.org/10.1016/j.ejphar.2019.04.004
Kamran MZ, Patil P, Gude RP (2013) Role of STAT3 in cancer metastasis and translational advances. BioMed Res Int 2013:421821. https://doi.org/10.1155/2013/421821
Li X, Lin H, Jiang F, Lou Y, Ji L, Li S (2019) Knock-down of HOXB8 prohibits proliferation and migration of colorectal cancer cells via wnt/β-catenin signaling pathway. Med Sci Monit: Int Med J Exp Clin Res 25:711–720. https://doi.org/10.12659/MSM.912218
Liang R, Chen X, Chen L, Wan F, Chen K, Sun Y, Zhu X (2020) STAT3 signaling in ovarian cancer: a potential therapeutic target. J Cancer 11:837–848. https://doi.org/10.7150/jca.35011
Mallen AR, Townsend MK, Tworoger SS (2018) Risk factors for ovarian carcinoma. Hematol/oncol Clin 32:891–902
Morgan R, El-Tanani M (2016) HOX genes as potential markers of circulating tumour cells. Curr Mol Med 16:322–327
Saini U et al (2017) Elevated STAT3 expression in ovarian cancer ascites promotes invasion and metastasis: a potential therapeutic target. Oncogene 36:168–181. https://doi.org/10.1038/onc.2016.197
Shen S, Pan J, Lu X, Chi P (2016) Role of miR-196 and its target gene HoxB8 in the development and proliferation of human colorectal cancer and the impact of neoadjuvant chemotherapy with FOLFOX4 on their expression. Oncol Lett 12:4041–4047
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA: Cancer J Clin 69:7–34. https://doi.org/10.3322/caac.21551
Stavnes HT et al (2013) HOXB8 expression in ovarian serous carcinoma effusions is associated with shorter survival. Gynecol Oncol 129:358–363. https://doi.org/10.1016/j.ygyno.2013.02.021
Stewart C, Ralyea C, Lockwood S (2019) Ovarian cancer: an integrated review. Semin Oncol Nurs 35:151–156. https://doi.org/10.1016/j.soncn.2019.02.001
Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD et al (2018) Ovarian cancer statistics, 2018. CA: Cancer J Clin 68(4):284–296. https://doi.org/10.3322/caac.21456
Wang T et al (2019) HOXB8 enhances the proliferation and metastasis of colorectal cancer cells by promoting EMT via STAT3 activation. Cancer Cell Int 19:3. https://doi.org/10.1186/s12935-018-0717-6
Wang Y, Dang Y, Liu J, Ouyang X (2016) The function of homeobox genes and lncRNAs in cancer. Oncol Lett 12:1635–1641
Yang J, Wei D, Wang W, Shen B, Xu S, Cao Y (2015) TRAF4 enhances oral squamous cell carcinoma cell growth, invasion and migration by Wnt-β-catenin signaling pathway. Int J Clin Exp Pathol 8:11837–11846
Ying Y et al (2020) Oncogenic HOXB8 is driven by MYC-regulated super-enhancer and potentiates colorectal cancer invasiveness via BACH1. Oncogene 39:1004–1017. https://doi.org/10.1038/s41388-019-1013-1
Zhan T, Rindtorff N, Boutros M (2017) Wnt signaling in cancer. Oncogene 36:1461–1473. https://doi.org/10.1038/onc.2016.304
Acknowledgements
Not Applicable.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
LDL designed the study, supervised the data collection, analyzed the data, LFW interpreted the data and prepare the manuscript for publication, and XJL supervised the data collection, analyzed the data and reviewed the draft of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors state that there are no conflicts of interest to disclose.
Ethical approval
All experiments in this study were approved by the Animal Care and Use Committee of Wuhan NO.1 Hospital and performed in accordance with the Guide for the Care and Use of Laboratory Animals.
Consent to participate
Not Applicable.
Consent for publication
Written informed consent was obtained from a legally authorized representative (s) for anonymized patient information to be published in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, L., Wang, L. & Li, X. The roles of HOXB8 through activating Wnt/β-catenin and STAT3 signaling pathways in the growth, migration and invasion of ovarian cancer cells. Cytotechnology 74, 77–87 (2022). https://doi.org/10.1007/s10616-021-00508-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10616-021-00508-w