Abstract
Background
Cognitive vulnerability-stress models explain depression as the result of an interaction between negative cognitive styles and stressful life events; however, the specific content of the cognitive diathesis varies by model.
Methods
This study examined three cognitive diatheses (i.e., unprimed cognitions, cognitive reactivity, and mood reactivity) in a prospective longitudinal design assessing currently non-depressed college students (N = 322) at the start of the semester with follow-up at the end of the semester, approximately 3 months later. At baseline, depressive symptoms, major depression history, negative life events in the past year, unprimed dysfunctional attitudes, and both cognitive reactivity and mood reactivity over a dysphoric mood induction were assessed. Depressive symptoms and negative life events in the interim were assessed at follow-up.
Results
After controlling for gender, past year negative life events, and baseline depression severity; unprimed dysfunctional attitudes significantly predicted subsequent depression severity, whereas cognitive reactivity and mood reactivity did not. None of the cognitive vulnerabilities interacted with negative life events over the interim to predict later depression. After controlling for gender, past year negative life events, baseline depression severity, and history of depression; mood reactivity and the mood reactivity × depression history interaction significantly predicted later depressive symptoms. Greater levels of mood reactivity predicted higher depressive symptoms in those with a history of depression and lower depressive symptoms in those without history of depression.
Conclusions
Results suggest that different vulnerabilities may be relevant to predicting increases in depressive symptoms over time in those individuals who have not previously been depressed vs. those who have.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Depression is one of the world’s leading disabilities and a disorder that is prone to recurrence (Moussavi et al. 2007; Klein and Allman 2014). Much research has aimed to determine the causes of depression and its recurrence within a diathesis-stress framework. Various cognitive vulnerability-stress models explain depression as the result of an interaction between negative cognitive styles and stressful life events (Alloy et al. 2006a, b). The assumption that an individual’s interpretations of her experiences and the meaning she assigns to them determine whether depression develops in the face of stress is consistent across all cognitive vulnerability models; however, the specific content of the cognitive diathesis varies from model to model. According to Beck’s model (1967, 1987), people have a set of core beliefs, or schemas, that affect the way they view themselves and the world. Beck’s model proposes that depression ensues when a stressful life event activates negative schemas containing dysfunctional attitudes.
Different methods have been used to test cognitive vulnerability hypotheses, including measuring baseline unprimed cognitions (e.g., using a self-report measure) and depressive symptoms and then re-assessing depressive symptoms and stressful life events at a follow-up timepoint. For example, Alloy et al. (2000) used unprimed cognitions on the Dysfunctional Attitudes Scale (DAS; Weissman and Beck 1978) and the Cognitive Style Questionnaire (CSQ; Abramson and Metalsky 1989) to group currently nondepressed undergraduates into low and high cognitive risk for depression groups based on scores in the highest and lowest quartile on both scales, respectively. In examining retrospective reports of depression history, the high cognitive risk group had a higher lifetime prevalence of major depressive disorder and more severe episodes relative to the low cognitive risk group (Alloy et al. 2000). When followed prospectively for 2.5 years, high cognitive risk students were over 6 times more likely to develop a major depressive episode relative to low cognitive risk students, including both first onsets and recurrences (Alloy et al. 2006a, b). As an advantage, cognitive vulnerability studies that use unprimed cognitions on established scales lend themselves to relatively straightforward prospective, longitudinal designs. As a possible disadvantage, these designs assume that cognitive vulnerabilities are traits that can be assessed at any time due to their stability and, therefore, do not model the activation of negative cognitive styles in response to stressful life events in the onset of depression, as proposed in Beck’s cognitive model.
Studies using unprimed cognitions generally support Beck’s cognitive model. In one such study, high school students were assessed for depressive symptoms, history of depression, negative life events, and cognitive vulnerabilities and returned a year later for follow-up assessment (Lewinsohn et al. 2001). Results showed a significant dysfunctional attitudes by negative life events interaction, such that participants high in dysfunctional attitudes and high in negative life events had the highest incidence of depression. In another large, longitudinal study, over 8500 nondepressed pregnant women were assessed for depressive symptoms and negative self-schemata at 18 weeks of pregnancy and reassessed for depressive symptoms at 32 weeks of pregnancy (Evans et al. 2005). After adjusting for baseline depressive symptoms and history of depression, women in the highest third of the sample on negative self-schema scores were more likely to become depressed between 18 and 32 weeks of pregnancy than women in the lowest third of the sample.
Hankin et al. (2004) conducted multiple studies to examine the cognitive vulnerability-stress model. In Study 1, undergraduate students were assessed for cognitive vulnerabilities on the DAS and CSQ, negative life events, and depressive symptoms at baseline and then reassessed for depressive symptoms 5 weeks later (Time 2). For both the DAS and CSQ, results showed a significant interaction between cognitive vulnerability and negative life events in predicting depressive symptoms at Time 2, such that higher cognitive vulnerability combined with a higher number of negative life events was associated with greater depressive symptoms at Time 2. In Study 2, undergraduate students were assessed for cognitive vulnerabilities (DAS and CSQ), negative life events, and depressive symptoms at baseline and then reassessed for depressive symptoms 2 years later. Results paralleled those of Study 1, with a significant cognitive vulnerability by life events interaction in predicting future depressive symptoms. In Study 3, mood, CSQ, and DAS were assessed in a sample of undergraduate students 1 to 2 weeks before a midterm exam. Each cognitive vulnerability interacted with a naturally occurring stressor (i.e., an index of exam failure calculated as actual minus aspired exam grade) in predicting depression 5 days after receiving the grade. Specifically, higher cognitive vulnerability combined with poorer exam performance relative to one’s standard was associated with more depressive symptoms. All three of these studies found specificity for the cognitive vulnerability (measured via unprimed cognitions) by life events interaction in predicting growth in depression symptoms over time. More recent studies of unprimed cognitions have investigated the role of expectations in predicting depression, including studies showing that self-report expectations of suicidal risk predicted follow-up suicidal behavior and that positive-expectation hopelessness predicted depressive symptoms (Czyz et al. 2016; Horwitz et al. 2017).
Miranda and Persons (1988) proposed the mood state dependent hypothesis, which asserts that dysfunctional attitudes are stable vulnerability factors for depression but are only accessible in the context of a negative mood state, as opposed to representing a trait that can be accessed at any time. In a test of this hypothesis, participants with a history of depression experiencing greater levels of current dysphoric affect reported higher unprimed dysfunctional attitudes than those with a history of depression experiencing lower levels of current dysphoric affect (Miranda and Persons 1988). In contrast, unprimed dysfunctional attitudes were relatively low among those with no history of depression, regardless of current dysphoric mood state. These results suggest that dysfunctional attitudes are mood-state dependent among formerly depressed individuals, but do not inform whether dysphoric mood-congruent dysfunctional attitudes are antecedents to or consequences of clinical depression.
Mood priming, which involves inducing a dysphoric mood state with the goal of accessing cognitive vulnerabilities, provides another methodology for testing cognitive vulnerability-stress hypotheses. It models the activation of a (dormant) cognitive vulnerability to depression in response to stress, per Beck’s model. Mood priming designs incorporate various mood induction procedures that demonstrate good psychometrics for successfully inducing transient negative mood states (Westermann et al. 1996). The resulting sad mood is intended to briefly simulate a negative life event but to a lesser degree and, consequently, elicit negative schemas. However, the nature of negative mood priming limits the testable population to currently nondepressed individuals due to ethical concerns.
The cognitive vulnerability construct most examined in mood priming studies is cognitive reactivity, defined as the change in DAS scores from before to after a dysphoric mood induction (Segal et al. 1999). Rather than using a simple change score, newer studies have operationalized cognitive reactivity as residualized DAS change scores, derived from regressing post-mood induction DAS scores on pre-mood induction DAS scores. One such study, Segal et al. (2006), examined cognitive reactivity as a predictor of relapse in depressed participants treated to remission with cognitive-behavioral therapy (CBT) or antidepressants. Those with greater cognitive reactivity in remission were significantly more likely to develop a depressive relapse over 18 months of follow-up than those who were lower in cognitive reactivity, regardless of treatment modality. These results support cognitive reactivity as a cognitive vulnerability for depression relapse, but do not inform whether it represents a risk factor for a first episode of depression.
Wenze et al. (2010) examined cognitive reactivity in a naturally occurring context in a general college student sample. Rather than using a dysphoric mood induction paradigm, they used an experience sampling technique to assess for cognitive reactivity in participants’ everyday lives based on mood and thought data collected throughout the day for a 1-week period. Participants with a stronger link between negative mood and negative cognitions reported more depressive symptoms at a 6-month follow-up, and this index of cognitive reactivity was a more robust predictor of depressive symptoms than baseline unprimed dysfunctional attitudes or initial depressive symptoms.
A few studies, however, have failed to support cognitive reactivity in predicting subsequent depression. In a study of 187 remitted depressed patients, van Rijsbergen and colleagues (2013) found that cognitive reactivity was not predictive of relapse over 5.5 years of follow-up. However, unprimed DAS scores at baseline and participants’ mood reactivity—derived from the difference in self-rated mood scores on a visual analogue scale from before to after a dysphoric mood induction—were each significantly predictive of depressive relapse. Similarly, Jarrett et al. (2012) failed to find that cognitive reactivity predicted relapse in a sample of depressed patients who initially responded to cognitive therapy and then received 8-months of continuation phase treatment. In fact, 20% of the sample did not report experiencing the intended worsening of mood after the induction, which the authors argued might have been a by-product of their sample’s prior experience with cognitive therapy (i.e., active use of cognitive strategies in response to the dysphoric mood induction to fortify themselves against the effects). However, unprimed dysfunctional attitudes predicted depressive relapse or recurrence over the 32 months of follow-up (Jarrett et al. 2012).
In summary, there are different methods of studying cognitive vulnerability-stress models of depression including designs that use unprimed cognitions, cognitive reactivity, and mood reactivity. Unprimed dysfunctional attitudes are the most well-established of the cognitive vulnerability constructs in predicting depression, and research using dysfunctional attitudes to measure cognitive vulnerability generally supports Beck’s model of depression (Beck 2008). In contrast, evidence is more mixed on the predictive ability of cognitive reactivity, and mood reactivity is a newer and less studied construct compared to either unprimed cognitions or cognitive reactivity. Mood reactivity has been posited to model the ability to regulate emotion during stressful events (van Rijsbergen et al. 2013), and it remains unknown whether this construct is cognitively mediated or may represent a personality factor. Further, as mood priming studies have generally been conducted in populations treated for depression, mood reactivity and cognitive reactivity have been examined less in general samples.
The current study examined unprimed cognitions, cognitive reactivity, and mood reactivity in a prospective longitudinal design, assessing currently non-depressed college students at the start of the semester with follow-up at the end of the semester, approximately 3 months later. At the baseline assessment, depressive symptoms were measured along with three measures of cognitive vulnerability: unprimed dysfunctional attitudes, cognitive reactivity, and mood reactivity. Depressive symptoms and stressful life events in the interim were assessed at follow-up. To our knowledge, this is one of the first studies to examine the relative predictive ability of these three measures of cognitive vulnerability to depression. Given that unprimed dysfunctional attitudes have the most robust support as a predictor of depression relapse and growth in depressive symptoms over time in the literature, unprimed dysfunctional attitudes were expected to be more strongly predictive of an increase in depressive symptoms than cognitive reactivity or mood reactivity. In addition, this relationship was expected to be strongest among those with a history of major depression and those who endorsed greater stress associated with negative life events in the interim. Consistent with a diathesis-stress framework for depression, greater stress from life events should be positively associated with follow-up depressive symptoms. Further, having at least one episode of depression increases the risk for subsequent episodes (Burcusa and Iacono 2007). Therefore, we expected dysfunctional attitudes would be more strongly associated with subsequent depression symptoms in those with greater stress and history of depression.
Methods
Participant Screening and Enrollments
Undergraduate students, 18 years and older, were recruited at the University of Vermont to receive psychology course credit for participation. Within the first 3 weeks of classes starting, volunteers were screened for eligibility in an initial session where they reviewed an informed consent form. If consenting, participants completed a depressive symptom measure, the Beck Depression Inventory-Second Edition (BDI-II; Beck et al. 1996) and were deemed eligible if they obtained a score in the normal mood range (0–13). Due to ethical concerns related to undergoing a dysphoric mood induction procedure at Time 1, recruitment was limited to nondepressed participants.
Procedures
This study was approved by the University of Vermont’s institutional review board on human subjects research. Participants were assessed at two timepoints—at the beginning of the semester (Time 1) and at the end of the semester (Time 2). Data collection continued every fall and spring semester over 4 consecutive academic years, with participants completing the study within one academic semester. At Time 1, participants completed several measures, including the Dysfunctional Attitudes Scale (DAS; Weissman and Beck 1978), the Diagnostic Inventory for Depression (DID; Zimmerman et al. 2004) modified to assess for a past major depressive episode according to DSM-IV criteria, and the Life Experiences Survey (LES; Sarason et al. 1978). At Time 1, participants also underwent a sad mood induction procedure (see description below), rated their mood on a visual analogue scale pre- and post-mood induction, and completed another DAS (alternate version, A or B). At Time 2, participants completed the BDI-II, the DID (which assessed whether participants met DSM-IV criteria for a current major depressive episode), and the LES (which assessed for stressful life events since Time 1).
A sad mood induction procedure, as described in Segal et al. (2006), was used in the study. Participants were first asked to write about “a memory that makes you sad.” Afterwards, they were instructed to continue thinking about it to “try to get into a sad mood” while orchestra music (“Russia under the Mongolian Yoke” by Prokofiev) played at half-speed for 10 min.
Measures
Dysfunctional Attitudes Scale (DAS)
The Dysfunctional Attitudes Scale (DAS; Weissman and Beck 1978) consists of two parallel forms (Forms A and B) that measure belief in 40 statements frequently endorsed by depressed individuals. Statements such as “I am nothing if a person I love does not love me” are rated on a 7-point Likert scale for degree of belief. The DAS has shown high test–retest reliability (Weissman and Beck 1978) as well as high internal consistency (Dobson and Breiter 1983) when using undergraduate samples. In this study, DAS Form A α = 0.82 and DAS Form B α = 0.75.
Visual Analogue Scale (VAS)
Participants rated their mood state by drawing a mark on a 150-mm line with “neutral” in the middle, flanked by the words “sad” (left) and “happy” (right) before and after the mood induction procedure. The VAS is commonly used to index mood before and after a dysphoric mood induction in cognitive reactivity studies (Segal et al. 2006; van Rijsbergen et al. 2013).
Beck Depression Inventory-Second Edition (BDI-II)
The Beck Depression Inventory-Second Edition is a measure of depressive symptom severity (BDI-II; Beck et al. 1996). The BDI-II consists of 21 items, each rated on a 4-point Likert scale (0 to 3) based on the past 2 weeks. Summed responses create a total BDI-II score, with a score of 0 to 13 indicating normal mood/minimal depressive symptoms. The BDI-II has shown good convergent validity as well as good test–retest reliability (Beck et al. 1996). Time 1 BDI-II α = 0.70 and Time 2 BDI-II α = 0.88 in this study.
Life Experiences Survey (LES)
The Life Experiences Survey (LES; Sarason et al. 1978) consists of 57 potentially stressful events that participants mark as having experienced or not experienced in the past year. The 57 items include 10 items specific to college students and 3 additional items in which a participant can write in events not listed. For each experienced life event, participants rate the perceived impact on a 7-point Likert scale ranging from -3 (“extremely negative”) to 3 (“extremely positive”). Positive and negative ratings are separately summed to yield a positive and negative impact scores, respectively. The current study uses only negative impact scores. At Time 2, the past year timeline was replaced with past semester to capture stressful life events in the interim between assessments. Time 1 (past year) negative life events subscale α = 0.62 and Time 2 (past semester) negative life events subscale α = 0.69 in this study.
Diagnostic Inventory for Depression (DID)
The Diagnostic Inventory for Depression (DID; Zimmerman et al. 2004) is a self-report measure of DSM-IV criteria for a current major depressive episode (MDE). The 38-item scale is focused on the past week and contains 3 items that measure the frequency of depressed mood, loss of interest in usual activities, and loss of pleasure. The other items assess for severity of the remaining DSM-IV MDE symptoms and psychosocial impairment. Based on the algorithm in Zimmerman et al. (2004), a categorical variable to estimate presence of an MDE was created, aligning with the DSM-IV criteria for MDE diagnosis. In this study, the DID was used to assess depression history at Time 1 and current depression status at Time 2. The current study modified the DID instructions at Time 1 to “focus on the time in your life when you felt the most sad or depressed.”
Psychometric properties for the DID are good, including internal consistency, convergent and divergent validity, and test–retest reliability (Zimmerman et al. 2004). Further, good diagnostic agreement exists between the DID and the Structured Clinical Interview for DSM-IV (SCID; First et al. 1995) within a psychiatric outpatient population (Zimmerman et al. 2004). In this study, Chronbach’s alpha for the symptom severity items of the DID were 0.92 for the lifetime version administered at Time 1 and 0.89 for the current version administered at Time 2.
Data Analytic Plan
All analyses were conducted in SPSS, version 26. The data analysis consisted of three hierarchical regressions to compare the predictive ability of unprimed dysfunctional attitudes, cognitive reactivity, and mood reactivity in predicting growth in depressive symptoms from Time 1 to Time 2. Time 2 BDI-II score served as the dependent variable. In all regressions, the variables in the interactions were first centered at zero. At Time 1, 331 participants enrolled in the study, and only 9 (2.7%) failed to return for follow-up at Time 2. Only participants who provided Time 2 data (N = 322) were included in these analyses. Sex, race/ethnicity (i.e., White non-Hispanic vs. all others), Time 1 LES (NLE; impact of negative life events in the past year), year in school, and semester of participation were examined as potential covariates in the model and included in the analyses only if they were significantly associated with the outcome variable.
The three models included covariates in Step 1, Time 1 BDI-II in Step 2, and Time 2 (past semester) NLE in Step 3. At Step 4, each respective cognitive vulnerability (mood reactivity, cognitive reactivity, or baseline DAS) was entered. Variables were centered around zero then multiplied to create an interaction term (cognitive vulnerability × past semester negative life events), which was added in Step 5. To account for the variance in pre-mood induction DAS scores, cognitive reactivity was computed using residualized DAS change scores derived from regressing post-mood induction DAS scores on pre-mood induction DAS scores and saving the standardized residuals (Zres-CR). This method is consistent with procedures in Segal et al. (2006). Similarly, mood reactivity was computed as a residualized change score (Zres-MR). The three regression models’ respective predictive abilities were compared using the effect size, \({R}^{2}\) change, or the unique variance in Time 2 depressive symptoms accounted for by the cognitive vulnerability over and above other variables.
Our second set of three regression models added a layer of complexity to the former models. Like the first set of regressions, each model followed the same structure for each respective cognitive vulnerability. Step 1 included the covariates. Step 2 added Time 1 BDI-II score. Step 3 included a dichotomous history of a major depressive episode variable based on DID. We added Time 2 (past semester) NLE in Step 4 and the cognitive vulnerability (CR, MR, or baseline DAS) in Step 5. Step 6 included past semester NLE score by depressive episode history interaction term. Step 7 added another interaction term, cognitive vulnerability by past semester NLE. Step 8 consisted of a cognitive vulnerability by history of depression interaction. Finally, Step 9 included a three-way interaction term with the cognitive vulnerability, past semester NLE, and history of depression.
Results
Descriptive statistics for study variables are presented in Table 1, and bivariate correlations are presented in Table 2. Our sample consisted of 322 adult undergraduate students. Most participants were White (n = 281; 87%), female (n = 258; 80%), and in their first year in college (n = 156; 48%). Many participants (n = 101; 31%) had a previous history of major depression. Only 1 participant was experiencing a current major depressive episode at Time 2 using DID criteria. As shown in Table 1, fewer than 5% of cases (n = 11) had any missing data. Therefore, missing data were handled using listwise deletion over multiple imputation. Missing cases for each study variable are presented in Table 1. Skewed variables, past year NLE, past semester NLE, and Time 2 BDI-II, were transformed using square root transformations before conducting analyses.
To verify that the sad mood induction was successful, we compared mean mood ratings on the VAS before and after the mood induction. Participants rated their moods, on average, 91.22 mm (SD = 19.84) before and 55.61 mm (SD = 19.55) after the sad mood induction. Based on the VAS anchors, these means fall in the “neutral” to “happy” range before vs. the “neutral” to “sad” range after the induction procedure. On average, participants reported a 35.61 (SD = 21.49) unit decrease (i.e., worsening) in mood over the induction. A substantial majority (97%, n = 311) of participants’ moods got worse over the mood induction. Approximately 1% (n = 4) of participants’ moods stayed the same, and paradoxically, a small proportion of participants’ moods (2%; n = 6) improved following the mood induction.
Potential covariates were first analyzed to determine inclusion in the analyses. Based on bivariate correlations with the outcome variable (Time 2 depressive symptoms on the BDI-II), gender and negative impact score from the Time 1 LES (past year NLE), were the only covariates significantly associated with the outcome and were, therefore, included in the subsequent hierarchical regression models. The remaining proposed covariates (i.e., year in school, ethnicity, semester of participation) were dropped from the analyses. In order to test mood reactivity (MR Model), cognitive reactivity (CR Model), and baseline DAS (DAS Model) as predictors of later depressive symptoms, three separate hierarchical regressions were then conducted.
Cognitive Reactivity Model
The overall model at Step 1 was statistically significant (F [2, 315] = 23.73, p = < 0.001), and the overall model remained significant throughout all steps in this regression (see Table 3). In Step 1, gender was significantly associated with Time 2 BDI-II (b = -0.32, t[317] = -2.34, p = 0.018). However, past year NLE was not significantly associated with Time 2 BDI-II, b = 0.06, t(317) = 1.07, p = 0.279. Together, gender and past year NLE accounted for 13% of the variance in Time 2 BDI-II, \(\Delta {R}^{2}\) = 0.13, \(\Delta F\) = 23.73, p < 0.001. Step 2 showed that Time 1 BDI-II significantly predicted Time 2 BDI-II, b = 0.12, t(317) = 10.06, p < 0.001. Adding Time 1 BDI-II to the model increased the variance accounted for by the model by 22% from previous steps, \(\Delta {R}^{2}\) = 0.22, \(\Delta F\) = 107.71, p < 0.001. Similarly, Time 2 (past semester) NLE in Step 3 added 7% unique variance in Time 2 BDI-II over and above the previous steps, \(\Delta {R}^{2}\) = 0.07, \(\Delta F\) = 40.08, p < 0.001. In Step 4, cognitive reactivity (Zres-CR) did not significantly predict Time 2 BDI-II (b = 0.04, t[317] = 0.63, p = 0.526). Similarly, the addition of an interaction term, Zres-CR × Time 2 (past semester) NLE, at Step 5 was not significantly associated with Time 2 BDI-II, b = 0.03, t(317) = 0.75, p = 0.449.
Mood Reactivity Model
In Step 1, the overall model, including covariates (i.e., gender and past year NLE), was statistically significant (F [2, 315] = 23.73, p = < 0.001), and the model remained significant throughout the remaining steps (see Table 3). In Step 4, mood reactivity (Zres-MR) did not significantly predict Time 2 BDI-II (b = -0.03, t[317] = -0.48, p = 0.633), nor did it account for unique variance over and above previous steps (\(\Delta {R}^{2}\) = 0.001, \(\Delta F\) = 0.16, p = 0.689). Likewise for Step 5, including the Zres-MR × past semester NLE interaction term did not significantly predict Time 2 BDI-II (b = 0.03, t[317] = 0.71, p = 0.482) nor significantly improve the model (\(\Delta {R}^{2}\) = 0.001, \(\Delta F\) = 0.50, p = 0.482).
Unprimed DAS Model
The overall model including gender, Time 1 (past year) NLE, Time 1 BDI-II, Time 2 (past semester) NLE, baseline unprimed DAS score, and the interaction term for baseline DAS × past semester NLE was statistically significant (F [6, 311] = 39.96, p < 0.001). Details of all the steps in the regression model are listed in Table 3. Baseline DAS, which was added in Step 4, was significantly associated with Time 2 BDI-II (b = 0.01, t[317] = 2.07, p = 0.039). Further, baseline DAS accounted for 1% of the unique variance in Time 2 BDI-II over and above previous steps (\(\Delta {R}^{2}\) = 0.01, \(\Delta F\) = 4.23, p = 0.041). However, the baseline DAS × past semester NLE interaction term added in Step 5 did not predict Time 2 BDI-II (b = -0.00, t[317] = -0.84, p = 0.404), nor did the addition of the interaction term significantly improve the model (\(\Delta {R}^{2}\) = 0.001, \(\Delta F\) = 0.70, p = 0.404).
Comparative Predictive Abilities of the Unprimed DAS, Cognitive Reactivity, and Mood Reactivity Models
Compared to mood reactivity and cognitive reactivity, unprimed DAS scores emerged as the strongest predictor of follow-up depressive symptoms on the BDI-II based on the significant unique variance it accounted for over and above the previous steps (\(\Delta {R}^{2}\) = 0.01, \(\Delta F\) = 40.08, p = 0.041). In contrast, the change in \({R}^{2}\) for cognitive reactivity (Zres-CR) and mood reactivity (Zres-MR) was less than 1% and did not correspond with a significant change in the overall predictive ability of their respective models (\(\Delta {R}^{2}\) = 0.002, \(\Delta F\) = 0.88, p = 0.350; \(\Delta {R}^{2}\) = 0.001, \(\Delta F\)= 0.16, p = 0.689). Further, neither cognitive reactivity (b = 0.04, t[317] = 0.63, p = 0.526) nor mood reactivity (b = -0.03, t[317] = 0.48, p = 0.633) was significantly associated with the outcome variable. In contrast, unprimed DAS scores had a small but significant association with the outcome variable, such that a unit increase in DAS score corresponded to a 0.01 unit increase in Time 2 BDI-II score (b = 0.01, t[317] = 2.07, p = 0.039). This finding supports our hypothesis that unprimed dysfunctional attitudes would more strongly predict an increase in depressive symptoms relative to cognitive reactivity or mood reactivity. Negative life events was not a significant moderator of the relationship between Time 2 BDI-II scores and any of the cognitive vulnerabilities: Zres-CR (b = 0.03, t[317] = 0.75, p = 0.449), Zres-MR (b = 0.03, t[317] = 0.71, p = 0.482) or DAS scores (b = -0.00, t[317] = -0.84, p = 0.404). Thus, the hypothesis that the relationship between each cognitive vulnerability and the outcome variable would be strongest among those who endorsed greater stress associated with negative life events in the interim was not supported. The variance in Time 2 depressive symptoms accounted for by each overall model was similar (Zres-MR: \({R}^{2}\) = 0.43, Zres-CR: \({R}^{2}\) = 0.43, DAS: \({R}^{2}\) = 0.44).
Cognitive Vulnerabilities and Prior History of Major Depressive Disorder
In the expanded cognitive reactivity hierarchical model, the overall model remained significant throughout all nine steps (see Table 4). In Step 5, cognitive reactivity did not significantly predict Time 2 BDI-II (b = -0.00, t[310] = -0.05, p = 0.962). Similarly, the interaction terms added in Steps 6 through 9 were not predictive of Time 2 BDI-II (see Table 4).
Results for the expanded hierarchical model using unprimed DAS scores are displayed in Table 4. The predictive ability of the model remained significant throughout all nine steps. Results showed a main effect of history of depression in Step 3 (b = 0.40, t[310] = 3.31, p < 0.001). Unlike in the first DAS Model, the addition of baseline DAS to the model was not significantly associated with Time 2 BDI-II (b = 0.01, t[310] = 1.35, p = 0.180) after accounting for gender, past year NLE, Time 1 BDI-II, and history of depression. The four interaction terms added in Steps 6 through 9 were also not predictive of Time 2 BDI-II.
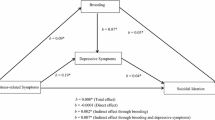
Results for the expanded hierarchical model using mood reactivity are displayed in Table 4. Only one interaction term, mood reactivity (Zres-MR) by depression history, was statistically significant in predicting Time 2 BDI-II and the other three interaction terms were not. Those three interactions (past semester NLE × history of depression, Zres-MR × past semester NLE, and Zres-MR × past semester NLE × history of depression) were subsequently dropped from the analyses in favor of a more parsimonious model, with six total steps reflected in Table 4. The overall model was statistically significant throughout all six steps. In Step 5, Zres-MR was added to the model, and results showed a significant main effect for this cognitive vulnerability. For each SD increase in mood reactivity, there was a 0.14 unit decrease in Time 2 BDI-II score (b = -0.14, t[310] = -2.16, p = 0.032). However, Zres-MR did not contribute significantly to the variance accounted for by the model, \(\Delta {R}^{2}\) < 0.001, \(\Delta F\) = 0.23, p = 0.633. In Step 6, the interaction of mood reactivity by history of depression significantly predicted Time 2 BDI-II (b = 0.33, t[310] = 3.04, p = 0.003), and this interaction term accounted for 2% of the unique variance in Time 2 BDI-II over and above previous steps, (\(\Delta {R}^{2}\) = 0.02, \(\Delta F\) = 9.23, p = 0.003).
For the purposes of probing the interaction, this model was run in the PROCESS macro for SPSS. For those with a history of depression, each SD increase in mood reactivity corresponded to a 0.19 unit increase in Time 2 BDI-II, (b = 0.19, t[310] = 2.17, p = 0.031). For those without a history of depression, each SD increase in mood reactivity corresponded to a 0.14 unit decrease in Time 2 BDI-II, (b = -0.14, t[310] = 2.16, p = 0.032). The interaction is plotted in Fig. 1. As illustrated in Fig. 1, the difference between depression history status groups in Time 2 BDI-II scores is apparent at the sample mean for mood reactivity and even more pronounced at one SD above that sample mean. In contrast, at one SD below the mean level of mood reactivity in the sample, Time 2 BDI-II scores did not differ according to history of depression.
Comparative Predictive Abilities of the Unprimed DAS, Cognitive Reactivity, and Mood Reactivity Models including History of Depression
In the more complex models including prior history of major depression, DAS no longer predicted increases in Time 2 BDI-II scores (b = 0.01, t[310] = 1.35, p = 0.180) and cognitive reactivity (Zres-CR) was still not significantly associated with Time 2 BDI-II scores (b = -0.00, t[310] = -0.05, p = 0.962). Mood reactivity (Zres-MR) was significantly associated with Time 2 BDI-II scores (b = -0.14, t[310] = -2.16, p = 0.032). However, the addition of the Zres-MR did not significantly improve the overall model (\(\Delta {R}^{2}\) < 0.001, \(\Delta F\) = 0.16, p = 0.689). The R2 change values were similar among all the cognitive vulnerabilities (Zres-MR: \(\Delta {R}^{2}\) < 0.001, Zres-CR: \(\Delta {R}^{2}\) = 0.002, DAS: \(\Delta {R}^{2}\) = 0.006). As in the simple models, negative life events did not moderate any of the relationships between the cognitive vulnerabilities and Time 2 BDI-II. However, history of depression moderated the relationship between Zres-MR and Time 2 BDI-II scores (b = 0.33, t[310] = 3.04, p = 0.003), which supports our hypothesis that the relationship between the cognitive vulnerabilities and Time 2 BDI-II would be strongest for those with a history of depression. The variance in Time 2 BDI-II accounted for by each overall model was similar (Zres-MR: \({R}^{2}\) = 0.46, Zres-CR: \({R}^{2}\) = 0.45, DAS: \({R}^{2}\) = 0.45).
Discussion
According to cognitive vulnerability-stress models, depression is the result of an interaction between a cognitive vulnerability and stressful life events. However, the specific content of the cognitive diathesis varies from model to model. The current study examined the relative predictive ability of three cognitive diatheses (i.e., unprimed cognitions, cognitive reactivity, and mood reactivity) using a prospective longitudinal design assessing currently non-depressed college students at the start of the semester with follow-up at the end of the semester, approximately 3 months later. To our knowledge, this is one of the few studies to test these three cognitive vulnerabilities and compare them.
Gender and baseline depression severity emerged as significant and robust predictors of Time 2 depression severity across all models. Gender, together with impact from negative life events over the past year, accounted for approximately 13% of the variance in follow-up depression scores, and baseline depression accounted for an additional 22% above and beyond these two covariates. After controlling for gender, impact of negative life events over the past year, and baseline depression severity on the BDI-II, only unprimed cognitions (i.e., DAS scores) significantly predicted subsequent depression severity on the BDI-II, accounting for a significant but small (1%) amount of unique variance in follow-up depressive symptoms. In contrast, neither cognitive reactivity nor mood reactivity to a dysphoric mood induction predicted later depression severity. These results support our hypothesis that baseline DAS score would emerge as the strongest predictor of follow-up depressive symptoms among these three cognitive vulnerabilities. This finding is consistent with other studies that found unprimed cognitions predict later depressive symptoms in college students (Alloy et al. 2000; Alloy, Abramson, Whitehouse, et al. 2006) and in pregnant women (Evans et al. 2005). However, these studies did not examine whether unprimed cognitions interacted with negative life events to predict later depression severity, as our study did.
Contrary to cognitive vulnerability-stress models and our a priori hypothesis, none of the three cognitive vulnerabilities interacted with the impact of negative life events over the interim (i.e., the semester) to significantly predict later depression. This contrasts with findings from some studies. Most like the current study, Hankin et al. (2004) also used an undergraduate sample with an even shorter follow-up period (i.e., 5 weeks) and found that dysfunctional attitudes interacted with negative life events to predict follow-up depressive symptoms. Beck’s (1967, 1987) model proposes that the cognitive diathesis of negative schemata containing dysfunctional attitudes interacts with the stress of negative life events to trigger depression. Given that we studied change in depressive symptoms over time, not clinical depression onset, the current study is not a test of Beck’s model. Some studies designed to test Beck’s model have been supportive. For example, Lewinsohn et al. (2001) found a significant interaction between dysfunctional attitudes and negative life events in predicting depression onset a year later in adolescents.
After examining the main effect of each cognitive vulnerability and its interaction with past semester negative life events, we also examined prior history of major depression and the 3-way interaction of each cognitive vulnerability, depression history, past semester life events in predicting subsequent depressive symptoms. With the addition of these two predictor variables, the more complex predictive models accounted for greater overall variance in follow-up depressive symptoms relative to the simpler models that did not consider prior depression history. Across all three complex models, baseline depression severity on the BDI-II, gender, past semester negative life events, and a history of depression were each significant predictors of follow-up depressive symptoms.
The best of the complex models included mood reactivity as the cognitive vulnerability and accounted for 46% of the variance in follow-up BDI-II scores. Mood reactivity, but not unprimed DAS scores or cognitive reactivity, significantly predicted follow-up depressive symptoms. Further, we found a significant mood reactivity × history of depression interaction, such that greater levels of mood reactivity predicted higher depressive symptoms in those with a history of depression and lower levels of depressive symptoms in those without a history of depression, thus supporting our hypothesis that the predictive ability would be stronger for those with a history of depression than those without such a history. The difference in follow-up depression scores for participants with vs. without prior major depression was apparent at the sample mean (and accentuated at one SD above that sample mean) for mood reactivity. In contrast, follow-up depression scores for participants with relatively low mood reactivity (1 SD below the sample mean) did not differ based on prior experience with major depression. No other interaction terms in the complex models were significantly predictive of follow-up depressive symptoms.
As operationalized in our study, mood reactivity models self-rated change in mood on a scale from before to after reflecting on a sad memory and listening to dysphoric music. The finding that greater mood reactivity to a sad mood induction was associated with larger increases in follow-up depression scores in those with prior major depression fits with theory. According to the elaborated cognitive vulnerability-stress theory of depression (Hankin and Abramson 2001), initial negative affect in reaction to a negative life event can lead to depression in the context of underlying cognitive vulnerabilities. However, the finding that greater mood reactivity to a dysphoric mood induction was associated with larger decreases in follow-up depression scores in participants without any major depressive episodes was unexpected. This finding may reflect the resilience of people who become initially more intensely sad in response to negative life events, yet do not develop clinical depression. For such individuals, it is possible that a negative life event elicits relatively intense initial negative affect that resolves more quickly than it does for those with a history of depression, for whom the sadness might linger due to cognitive vulnerabilities. This interpretation assumes that those with history of depression have higher levels of the assumed moderator (i.e., cognitive vulnerabilities) of the relationship between transient negative affect in response to life events and depression than those without depression history. Indeed, on average, those with a history of depression had significantly higher unprimed DAS scores (M = 144.69, SD = 19.95) than those without a history of depression (M = 139.18, SD = 17.52), t[313] = -2.49, p = 0.013). High mood reactivity on its own may not be a clinically concerning problem. Rather, high mood reactivity may serve to maintain or exacerbate depressed mood only in previously depressed populations and might even be protective in never-depressed individuals.
These results suggest that different cognitive vulnerabilities may be relevant to predicting later increases in depressive symptoms over time, in general, vs. within formerly depressed individuals, specifically. Unprimed dysfunctional attitudes were associated with subsequent increases in depressive symptoms, in general, whereas mood reactivity to a sad mood induction was related to subsequent increases in depressive symptoms among those with a history of major depression. If the research question surrounds detecting those at risk for elevations in depressive symptomatology over time, unprimed DAS represents a good candidate cognitive vulnerability predictor. As a benefit, the DAS is a practical, low-cost, efficient way of identifying those who may be at risk for increased depressive symptoms. On the other hand, if the research question surrounds identifying formerly depressed patients at risk for future increases in depressive symptoms, the added predictive value of administering a dysphoric mood induction procedure and measuring mood reactivity may be worth the costs of the added time and expense.
The current study examined change in depressive symptoms over an approximately 3-month follow-up interval rather than major depression onset. However, our findings are in line with van Rijsbergen et al.’s (2013) finding that cognitive reactivity did not predict time to relapse over 5.5 years of follow-up in formerly depressed patients, but both mood reactivity and unprimed DAS did. The authors concluded that mood reactivity may be a potential vulnerability for depression relapse, which supports the potential utility of doing a mood induction procedure with formerly depressed individuals beyond simply administering the DAS.
The primary limitation of this study is the sample. Our decision to include only students with BDI-II scores restricted to the normal range (0–13) was deemed necessary due to ethical concerns associated with subjecting clinically depressed individuals to a dysphoric mood induction. Perhaps as a function of this choice, raw BDI-II mean scores (8.07 at Time 1 and 6.21 at Time 2) indicate minimal development of depressive symptoms over the semester and, on average, a slight improvement in symptoms over the semester. These observed BDI-II scores limit the interpretability of our statistically significant findings, which were very small in terms of clinical significance, in relation to testing cognitive vulnerability models of depression. It would have been preferable to have a second depression outcome measure beyond the BDI-II. Although approximately one-third of this sample had prior history of depression, only one (of 322) subjects had current depression at Time 2. All of these characteristics underscore the remarkable health of this sample, as a whole, including those with prior history of depression who appear to be a particularly recovered group, despite the short follow-up interval.
The generalizability of our findings is limited by our relatively homogenous undergraduate sample and self-report measure of major depression history. Several of the aforementioned studies used a sample of individuals with a history of depression, ascertained by clinical interview. For example, van Rijsbergen et al. (2013) study’s sample had an average of 6.5 previous major depressive episodes. Although nearly a third (31%) of our sample had a prior history of depression based on the DID, only 1 participant in our sample met DID criteria for a current major depressive episode at follow-up. This low frequency precluded any analyses on Time 2 depression status as an outcome and restricted our analyses to examining change in depressive symptoms over the interim. We also do not have data on the number of prior major depressive episodes participants had. Further, the perceived impact of negative life events that occurred in one semester was relatively low using the LES as an indicator (see Table 1), and future research using similar samples should consider alternate stress indicators. Our relatively short follow-up interval covering one academic semester is another limitation. Given more time, we might have observed more variability in later depression severity and negative life events over the interim and more onsets of clinical depression.
Before entering each cognitive vulnerability predictor, our analyses adjusted for initial depressive symptom severity, gender, and the impact of negative life events over both the past year and the intervening semester, which together were robust predictors of follow-up depression severity, accounting for approximately 42% of the variance in Time 2 BDI-II scores. Although this is a strength of our approach, accounting for additional unique variance in later depressive symptoms over and beyond these robust predictors was a challenge, given the significant correlations between each of the three cognitive vulnerabilities and baseline BDI-II scores and both past year and semester NLE scores. As another limitation, it is possible that our mood induction procedure instructions to “get into a sad mood” created participant bias to act in a way that the experimenter desired (i.e., artificially inflating levels of sadness), despite the good psychometric properties for this procedure (Westermann et al. 1996).
Recent research on the cognitive model has shown that situational expectations mediate the relationship between beliefs, such as dysfunctional attitudes, and depression (Kube et al. 2018a, b). Future research should consider exploring situational expectations as an additional cognitive vulnerability and potential mediator to explore. Further, future research stemming from this work should include a longer follow-up period and more frequent assessments. As mentioned, a longer interim between cognitive vulnerability assessment and follow-up would be useful for allowing more time for both depressive symptoms to develop and potential negative life events to occur. More frequent assessments of cognitive vulnerabilities, stressful life events, and depressive symptoms would allow for longitudinal analyses to elucidate potentially causal relationships between these constructs over time.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Alloy, L. B., Abramson, L. Y., Hogan, M. E., Whitehouse, W. G., Rose, D. T., Robinson, M. S., et al. (2000). The Temple-Wisconsin Cognitive Vulnerability to Depression Project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of abnormal psychology, 109(3), 403–418. https://doi.org/10.1037/0021-843X.109.3.403
Alloy, L. B., Abramson, L. Y., Walshaw, P. D., & Neeren, A. M. (2006). Cognitive vulnerability to unipolar and bipolar mood disorders. Journal of Social and Clinical Psychology, 25(7), 726–754.
Alloy, L. B., Abramson, L. Y., Whitehouse, W. G., Hogan, M. E., Panzarella, C., & Rose, D. T. (2006). Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology, 115(1), 145–156.
Abramson, L. Y., & Metalsky, G. I. (1989). The Cognitive Style Questionnaire: Measurement of negative cognitive styles about self and consequences. Unpublished manuscript.
Beck, A. T. (1967). Depression: Clinical, experimental, and theoretical aspects. New York: Hoeber.
Beck, A. T. (1987). Cognitive models of depression. Journal of Cognitive Psychotherapy, 1(1), 5–37.
Beck, A. T. (2008). The evolution of the cognitive model of depression and its neurobiological correlates. American Journal of Psychiatry, 165(8), 969–977.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory-II. San Antonio, 78(2), 490-498.
Burcusa, S. L., & Iacono, W. G. (2007). Risk for recurrence in depression. Clinical Psychology Review, 27(8), 959–985. https://doi.org/10.1016/j.cpr.2007.02.005
Czyz, E. K., Horwitz, A. G., & King, C. A. (2016). Self-rated expectations of suicidal behavior predict future suicide attempts among adolescent and young adult psychiatric emergency patients. Depression and Anxiety, 33(6), 512–519. https://doi.org/10.1002/da.22514
Dobson, K. S., & Breiter, H. J. (1983). Cognitive assessment of depression: Reliability and validity of three measures. Journal of Abnormal Psychology, 92(1), 107–109. https://doi.org/10.1037/0021-843X.92.1.107
Evans, J., Heron, J., Lewis, G., Araya, R., & Wolke, D. (2005). Negative self-schemas and the onset of depression in women: Longitudinal study. The British Journal of Psychiatry, 186(4), 302–307.
First, M. B., Spitzer, R. L., Gibbon, M. & Williams, J.B. (1996). Structured Clinical Interview for the DSM-IV Axis I Disorders.
Hankin, B. L., & Abramson, L. Y. (2001). Development of gender differences in depression: An elaborated cognitive vulnerability–transactional stress theory. Psychological Bulletin, 127(6), 773–796.
Hankin, B. L., Abramson, L. Y., Miller, N., & Haeffel, G. J. (2004). Cognitive vulnerability-stress theories of depression: Examining affective specificity in the prediction of depression versus anxiety in three prospective studies. Cognitive Therapy and Research, 28(3), 309–345.
Horwitz, A. G., Berona, J., Czyz, E. K., Yeguez, C. E., & King, C. A. (2017). Positive and negative expectations of hopelessness as longitudinal predictors of depression, suicidal ideation, and suicidal behavior in high-risk adolescents. Suicide and Life-Threatening Behavior, 47(2), 168–176. https://doi.org/10.1111/sltb.12273
Jarrett, R. B., Minhajuddin, A., Borman, P. D., Dunlap, L., Segal, Z. V., Kidner, C. L., et al. (2012). Cognitive reactivity, dysfunctional attitudes, and depressive relapse and recurrence in cognitive therapy responders. Behaviour Research and Therapy, 50(5), 280. https://doi.org/10.1016/j.brat.2012.01.008
Kërqeli, A., Kelpi, M., & Tsigilis, N. (2013). Dysfunctional Attitudes and their effect on depression. Procedia—Social and Behavioral Sciences, 84, 196–204. https://doi.org/10.1016/j.sbspro.2013.06.534
Klein, D. N., & Allmann, A. E. S. (2014). Course of depression: Persistence and recurrence. In I. H. Gotlib & C. L. Hammen (Eds.), Handbook of depression (pp. 64–83). New York: Guilford Press.
Kube, T., Glombiewski, J. A., & Rief, W. (2018). Situational expectations mediate the effect of global beliefs on depressive symptoms: A 1-year prospective study using a student sample. Current Opinion in Psychiatry, 31(5), 409–416. https://doi.org/10.1097/YCO.0000000000000443
Kube, T., Siebers, V. H. A., Herzog, P., Glombiewski, J. A., Doering, B. K., & Rief, W. (2018). Integrating situation-specific dysfunctional expectations and dispositional optimism into the cognitive model of depression—A path-analytic approach. Journal of Affective Disorders, 229, 199–205. https://doi.org/10.1016/j.jad.2017.12.082
Lewinsohn, P. M., Joiner, T. E., Jr., & Rohde, P. (2001). Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. Journal of Abnormal Psychology, 110(2), 203–215. https://doi.org/10.1037/0021-843X.110.2.203
Lewinsohn, P. M., Zeiss, A. M., & Duncan, E. M. (1989). Probability of relapse after recovery from an episode of depression. Journal of Abnormal Psychology, 98(2), 107. https://doi.org/10.1037/0021-843X.98.2.107
Miranda, J., & Persons, J. B. (1988). Dysfunctional attitudes are mood-state dependent. Journal of Abnormal Psychology, 97(1), 76–79. https://doi.org/10.1037/0021-843X.97.1.76
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustun, B. (2007). Depression, chronic diseases, and decrements in health: Results from the world health surveys. The Lancet, 370(9590), 851–858.
Sarason, I. G., Johnson, J. H., & Siegel, J. M. (1978). Assessing the impact of life changes: Development of the life experiences survey. Journal of Consulting and Clinical Psychology, 46(5), 932–946. https://doi.org/10.1037/0022-006X.46.5.932
Scher, C. D., Ingram, R. E., & Segal, Z. V. (2005). Cognitive reactivity and vulnerability: Empirical evaluation of construct activation and cognitive diatheses in unipolar depression. Clinical Psychology Review, 25(4), 487–510. https://doi.org/10.1016/j.cpr.2005.01.005
Segal, Z. V., Gemar, M., & Williams, S. (1999). Differential cognitive response to a mood challenge following successful cognitive therapy or pharmacotherapy for unipolar depression. Journal of Abnormal Psychology, 108(1), 3–10.
Segal, Z. V., Kennedy, S., Gemar, M., Hood, K., Pedersen, R., & Buis, T. (2006). Cognitive reactivity to sad mood provocation and the prediction of depressive relapse. Archives of General Psychiatry, 63(7), 749–755. https://doi.org/10.1001/archpsyc.63.7.749
van Rijsbergen, G. D., Bockting, C. L. H., Burger, H., Spinhoven, P., Koeter, M. W. J., Ruhé, H. G., et al. (2013). Mood reactivity rather than cognitive reactivity is predictive of depressive relapse: A randomized study with 5.5-year follow-up. Journal of Consulting and Clinical Psychology, 81(3), 508–517.
Weissman, A., & Beck, A. T. (1978). Development and validation of the Dysfunctional Attitude Scale. Paper presented at the meeting of the Association for the Advancement of Behavior Therapy, Chicago, November, 1978.
Wenze, S. J., Gunthert, K. C., & Forand, N. R. (2010). Cognitive reactivity in everyday life as a prospective predictor of depressive symptoms. Cognitive Therapy and Research, 34(6), 554–562. https://doi.org/10.1007/s10608-010-9299-x
Westermann, R., Spies, K., Stahl, G., & Hesse, F. W. (1996). Relative effectiveness and validity of mood induction procedures: A meta-analysis. European Journal of Social Psychology, 26(4), 557–580. https://doi.org/10.1002/(SICI)1099-0992(199607)26:4
Zimmerman, M., Sheeran, T., & Young, D. (2004). The Diagnostic Inventory for Depression: A self-report scale to diagnose DSM-IV major depressive disorder. Journal of Clinical Psychology, 60(1), 87–110. https://doi.org/10.1002/jclp.10207
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception and design. Jessica Perez performed the data analyses and drafted the initial version of the manuscript. Kelly Rohan designed the parent study, acquired the data, and made critical revisions to the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Jessica Perez and Kelly J. Rohan declare no conflicts of interest to disclose.
Ethical Approval
This study was approved by the University of Vermont’s Committees on Human Research. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Perez, J., Rohan, K.J. Cognitive Predictors of Depressive Symptoms: Cognitive Reactivity, Mood Reactivity, and Dysfunctional Attitudes. Cogn Ther Res 45, 123–135 (2021). https://doi.org/10.1007/s10608-020-10174-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-020-10174-5