Abstract
The current study used double-blind, placebo-controlled design to examine the effect of intranasal oxytocin (OT) on emotion recognition (ER) and visual attention in 60 outpatients presenting for assessment and treatment of emotional disorders. Our primary hypothesis was that OT would improve recognition of happy faces in depressed participants. The main effect of OT on ER accuracy, speed, and proportion of fixations in the eye region was not significant. Diagnostic group (i.e., presence/absence of a depressive disorder) moderated the effect of OT on ER, but not as expected: OT significantly slowed ER speed for all emotions in participants with anxiety disorders, but did not affect performance in participants with depressive disorders. Depressed participants fixated significantly less in the eye region of sad faces than anxious participants. Before OT can be used to target ER biases, additional research is needed to explicate the differential impact of OT on ER speed in patients with anxiety versus mood disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The process of identifying emotions in another person, most commonly through facial expression, is known as emotion recognition (ER). Individuals use facial expression to interpret others’ interactions, adjust their behaviors, and avoid conflict. The ability to accurately identify and interpret emotional facial expressions is highly important to social interactions (Joormann et al. 2006). ER has been linked to altruistic behaviors (Marsh et al. 2008), higher relationship quality, and a lower rate of depression (Carton et al. 1999). Deficits in ER are connected to a variety of mental health symptoms including distress, social anxiety, social avoidance, depression, antisocial behaviors, and psychopathy (McClure and Nowicki 2001). Social cognitive deficits such as biases in ER predict social function (Shahrestani et al. 2013; Shultz and Dunbar 2012) and thus the enhancement of ER has the potential to improve social functioning in healthy controls and across clinical populations.
Previous research has shown that biased processing of emotional facial expressions predicts the course of a depressive episode, recovery from depression, and recurrence of depressive episodes (Bouhuys et al. 1999a, b; Hale 1998; Persad and Polivy 1993). There have been differences in results across studies for whether depression-related biases are based on a general emotion identification deficit (e.g., Persad and Polivy 1993) or a bias in specific emotional expressions (e.g., Gur et al. 1992). In a study examining ER using a forced-choice intensity judgment, Yoon et al. (2009) found that compared to controls and social anxiety participants, those with depression were less likely to judge subtle happy expressions as more intense than neutral expressions. This bias for happy versus neutral faces was specific to depression, suggesting that those with depression are less apt to identify positive affect in subtle facial expressions. A depression-specific bias in accurately identifying happy expressions had been previously shown by Joormann et al. (2006), who concluded that those with depression required significantly greater intensity of a happy facial expression to correctly label the happy face than both social anxiety and non-anxious control groups.
Oxytocin (OT) has been shown to enhance ER ability (e.g., Lischke et al. 2012). In a comprehensive review of OT and social behavior, Heinrichs and colleagues (2009) discuss how OT is released in response to positive social interactions, attenuating endocrine responses to stress, and serving as a potential mediator for stress-protective effects of social support. OT has also been shown to enhance processing of positive versus negative emotional information in healthy males (Di Simplicio et al. 2009).
A significant limitation of the current research is that much of the work in OT and ER has been conducted in healthy control samples with no known deficits in ER. Additionally, use of varied methodologies may contribute to inconsistent findings (i.e., Guastella and MacLeod 2012), making results difficult to generalize. While many studies report that OT improves the perception of happy faces (Marsh et al. 2010; Schulze et al. 2011), other studies (Fischer-Shofty et al. 2010) have found a more general effect of OT on ER, with OT improving perception of angry, sad, and fearful faces. In a meta-analysis examining the effects of intranasal OT on face recognition (Van Ijzendoon and Bakermans-Kranenburg 2012), results showed that OT enhances recognition of facial expressions of emotions based on a homogeneous set of studies (k = 13, N = 408). The effect of OT on ER was significant, but weak (Cohen’s d = 0.02). Thus, whether OT is useful in enhancing ER in clinical samples is less clear. In fact, in a recent meta-analysis on the effects of OT on ER, a single dose of OT did not significantly influence interpretation and expression of emotions in clinical populations including patients with anorexia, autism spectrum disorders, alcohol dependence, depression, opioid dependence, and schizophrenia (Leppanen et al. 2017).
In a study of the physiological, behavioral, and subjective effects of intranasal OT in 18 males with major depression, OT improved social cognition (performance on the “reading the mind in the eyes” test) (MacDonald et al. 2013). Additionally, OT produced an increase in anxiety and a decrease in nonverbal behaviors that cut off social contact. Because OT has been used as an adjunct treatment for social anxiety, and depression and social anxiety share features, it is important to understand how OT’s cognitive and behavioral effects are moderated by context and other factors (Bartz et al. 2011; Ellenbogen et al. 2013).
A common explanation for why emotional faces are more easily detectable after OT administration is increased attention towards the eye region (e.g., Domes et al. 2013; Guastella et al. 2008). Recently, researchers have explored the enhanced orienting of attention in response to emotional gaze cues after intranasal OT in healthy controls (Tollenaar et al. 2013). In a randomized placebo-controlled double-blind study 20 healthy males received OT or placebo and performed a gaze cueing task with happy, fearful, and neutral faces. OT significantly increased gaze cueing scores for happy and fearful faces relative to placebo. There were no significant effects for neutral expressions, and trait anxiety and depression did not moderate OT’s effects (Tollenaar et al. 2013).
In a recent double-blind, randomized, controlled study examining the effect of OT on attention to angry and happy faces in chronic depression (Domes et al. 2016), 43 patients received a single dose of OT nasal spray and completed a facial dot probe task. While Domes and colleagues (2016) did not specifically measure visual attention with an eye tracker, reaction times to neutral probes presented at the same location as faces depicting happy, angry, or neutral expressions were recorded as a measure of attention. OT was shown to reduce allocation of attention towards angry expressions, and sustain attention towards happy expressions under conditions of heightened awareness. Based on this finding, there was initial evidence for an OT-induced modulation of attention in people with depression.
Interestingly, individuals with emotional disorders show altered patterns of visual attention while exploring faces, yet the reasons for this are unknown. In a meta-analysis of eye tracking attention in the affective disorders, Armstrong and Olatunji (2012) summarized 33 studies using eye-tracking technology to study anxiety and depression. Compared to controls, anxious individuals show increased vigilance to threat during free viewing and visual search. Depressed individuals, on the other hand, were characterized by reduced orienting to positive stimuli, reduced maintenance of gaze on positive stimuli, and increased maintenance of gaze on dysphoric stimuli (Armstrong and Olatunji 2012). These authors suggested that the strong anhedonic bias in depression is not unique to depression, but also related to low positive affect. Further research using eye-tracking technology is warranted to elucidate the role of attentional biases in depression, and to determine the impact of intranasal OT on attentional biases across mood and anxiety disorders. The current study explored the effect of intranasal OT on ER performance in a sample of outpatients at a clinic for mood and anxiety disorders. These effects were compared in two groups that were formed based on the presence or absence of anxiety or mood disorder diagnoses: a depression group (DEP) and an anxiety-only group (ANX).
Based on the accumulating evidence of biases in recognizing happiness in depression outlined above, we predicted that the DEP group would require more emotional intensity to recognize happy faces compared to the ANX group. We also predicted that DEP participants who received OT would be faster in accurately identifying happy faces compared to DEP participants who received placebo. Next, we hypothesized that there would be group differences in eye gaze fixation in emotionally relevant areas of the face (eye region) between participants who received OT and those who received placebo. We also examined eye gaze fixation patterns between DEP and ANX groups. Finally, we explored the association between attention to regions of interest (entire face, eye, mouth) and ER performance to determine if performance was influenced by visual attention.
Method
Participants
The sample consisted of 60 participants who presented for assessment and treatment at the Center for Anxiety and Related Disorders (CARD) at Boston University. Participants completed a phone screen to determine eligibility. Eligible participants were men and women 18 years or older with a principal diagnosis of an anxiety or unipolar mood disorder. Patients were also required to meet stabilization/wash-out criteria for psychotropic medications and psychotherapy for the time periods preceding and overlapping their diagnostic assessment. Participants were contacted within 1 week of their initial intake at CARD to complete this study. The average number of days between study visits was 11.23 (SD = 2.82, range 4–14). The study was completed in one visit of approximately 90 min. All participants provided written, informed consent and were paid for participation.
Exclusionary criteria were as follows: (1) current delusions or hallucinations, (2) current suicidal or homicidal risk meriting intervention, (3) two or more hospitalizations in the last 5 years for severe psychopathology (psychosis, suicide attempts), (4) not fluent English speakers (those unable to complete CARD phone screen and ADIS-5 interview in English), (5) pregnancy, (6) a current or past autism spectrum disorder diagnosis, (7) regular smokers (smoking > 15 cigarettes/day), or consumers of non-prescription or illicit drugs (except for oral contraceptives), (8) major sensory impairment and/or visual acuity score (binocular) worse than 20/40, (9) a current respiratory illness requiring medication (i.e., allergy, cold, or flu symptoms), and (10) presence of a chronic medical condition (i.e., heart disease, uncontrolled hypertension, myocardial infarction, cardiac arrhythmia, kidney or liver disease, vascular disease, epilepsy, migraine, asthma, nephritis, diabetes or another endocrine disease, frequent or unexplained fainting, stroke, aneurism or brain hemorrhage, or other neurological illness).
The sample was predominantly female (n = 37; 61.7%), Caucasian (n = 48; 80%; Asian = 6.7%; African American = 10%, Other/not reported = 3.3%), and non-Hispanic (n = 54; 90%). The average age was 27.33 (SD = 9.94, range 18–65). The majority of the sample was right-handed (n = 53, 88.3%) and right-eye dominant (n = 46, 76.7%). Most participants (n = 37, 61.7%) used corrective eyewear for the ER task, with 56.7% wearing glasses and 5% using contact lenses. Visual acuity was calculated while participants used corrective eyewear. The average visual acuity score was above 20/20 (M = 1.19), and ranged from 0.58 to 1.34 (SD = .17). Based on exclusionary criteria of vision being 20/40 or better, all participants were eligible. Of note, there were no significant differences between DEP and ANX groups based on age (p = .33), sex (p = .43) race (p = .16), eye dominance (p = .55) or hand dominance (p = .24).
Diagnoses were established using the Anxiety and Related Disorders Interview Schedule for DSM-5 (ADIS-5; Brown and Barlow 2014). When administering the ADIS-5, interviewers assign each diagnosis a clinical severity rating (CSR) 0–8, representing the degree of distress and/or impairment in functioning associated with each diagnosis. Diagnoses with a CSR of 4 or higher are considered to be at a clinical level (i.e., at or above DSM-5 diagnostic threshold). By design, 50% of the sample (n = 30) met criteria for a clinical diagnosis of a mood disorder (DEP), and 50% met criteria for anxiety disorders without a mood disorder (ANX). In the DEP group, clinical diagnoses of major depressive disorder (MDD), persistent depressive disorder, other specified depressive disorder, and unspecified depressive disorder were accepted (but did not have to be principal). For the ANX group, diagnoses of panic, agoraphobia, specific phobia, separation anxiety, social anxiety, generalized anxiety, other specified and unspecified anxiety, obsessive–compulsive, and posttraumatic stress disorders were accepted. Participants in the ANX group could not have a current clinical mood disorder. Participants with two or more depressive episodes in the last year who were currently experiencing symptoms that are clinically significant but sub-diagnostic threshold (clinical severity rating of 3 out of 8 on the ADIS-5 for DEP disorders) were excluded from the ANX group. For the entire sample, the breakdown of principal diagnoses was as follows: generalized anxiety disorder (23.3%), social phobia (21.7%), co-principal diagnosis (10%), specific phobia (10%), persistent depressive disorder (8.3%), obsessive–compulsive disorder (8.3%), major depressive disorder (6.7%), body dysmorphic disorder (3.3%), other specified anxiety disorder (3.3%), panic disorder (1.7%), other specified obsessive–compulsive and related disorder (1.7%), other specified trauma/stressor-related disorder (1.7%). A co-principal diagnosis refers to two diagnoses that have the same CSR and are determined to be equally interfering and distressing. Of note, 21 of 30 participants (70%) in the DEP group had a principal or co-principal anxiety disorder.
Task
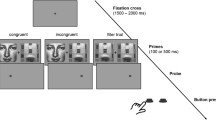
The facial morphing task entails watching “movies” of computer-morphed faces that change slowly from a neutral to a fully emotional expression, see Fig. 1. Stimuli faces were taken from Ekman and Friesen’s (1976) Pictures of Facial Affect (see Joormann and Gotlib 2006). After responding to two practice trials, participants were shown 40 morphed sequences (male and female actor expressing angry, happy, fear, and sad emotion five times each) of the faces in random order. Using Matlab software, each face was presented for 500 ms on a Hewlett Packard FP2141sb 21″ CRT monitor operating at 60hz. The black-and-white face images were approximately 12.25 × 9 cm in size. Faces were presented in the middle of the screen using a black background.
Emotion recognition task procedure. Participants were presented with a neutral face (0% emotionality), which progressed in 2% increments toward 100% emotionality. Each increment of emotionality, or frame, was displayed for 500 ms, with every fifth frame shown 1, 2, 3, 4, or 5 times the normal 500 ms length, to jitter the relationship between time and emotional intensity. Participants were asked to press a keyboard key as soon as they detected an identifiable emotional expression. Pressing the key stops the movie and asks participants to identify the face as expressing happiness, sadness, fear, or anger. The computer records the identification rating and emotional intensity of the face that is displayed at the moment of the key press
Participants pressed a designated key on a keyboard as soon as they detected an identifiable emotional expression. Participants then identified which expression, happiness, sadness, fear, or anger was being expressed on the face. Both the identified emotion (accuracy) and the intensity of the facial emotion were recorded on each trial.
Intensity scores were based on the intensity of the morphed expression at the time of the keyboard press, with possible scores ranging from 0 (neutral) to 100 (fully morphed emotion). Higher intensity scores signify that participants required greater emotion to identify the emotion type, and thus, higher intensity is indicative of slower recognition. Intensity scores were only calculated for trials where participants were accurate. Accuracy scores ranged .4–1.0 with lowest mean score for anger, .83 (SD = .17), and highest mean accuracy score of .995 (SD = .02) for happiness. Given the lack of variance for ER accuracy in happy faces, we utilized intensity scores for all reported analyses. Trials where participants pressed the space bar to select face type at 0% intensity (i.e., neutral) were not scored as accurate or incorrect, and intensity scores were not calculated. We decided to exclude such trials because they almost certainly do not reflect what the test is measuring, which is the minimum emotional intensity required to accurately identify an emotional face. Additionally, the key press at 0% intensity implies that the participants were holding down the space bar when the trial began and never saw the emotional face stimulus.
Eye Tracking
Hardware
An Applied Science Laboratories Eye-Trac 6 eye-tracking system was used to record the position of eye gaze throughout the task. The system has maximum accuracy of 0.5 degrees of visual angle, with a resolution of 0.25 degrees. The temporal resolution of the camera was set at 120 Hz. A chin rest was used to reduce head movement. After adjusting the camera of the eyetracker to be centered on the participant’s dominant eye, which was determined using a hole-in-the-card test (see Durand and Gould 1910), a short calibration sequence was administered. The participant looks at 9 points across the display monitor, after which the system will be able to accurately and continually calculate the participant’s point of gaze relative to the display will be performed by the researcher.
Data Reduction
After the initial 9-point calibration, the accuracy of the system was checked at the beginning of each trial for a period of 1500 milliseconds during which the participant fixated centrally. An average of the calibration checks across the 40 trials was used to refine the original calibration. In each trial, data were analyzed only if valid eye data were collected for at least 50% of the trial. If a particular participant lost more than 50% of their trials, their data were not analyzed at all. Additionally, if a participant’s data showed an overall proportion of less than 50% of fixation data in the face region, the participant’s eye data were not analyzed. This data reduction system eliminates erroneous and/or missing data due to various issues such as calibration, mechanical problems, and experimenter error.
Procedure
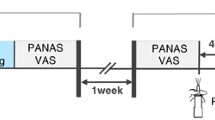
This study was a double-blind, placebo-controlled design. It was approved by the university’s Institutional Review Board, and the Food and Drug Administration. Upon arrival, participants were consented and randomized to receive either intranasal OT or placebo using a counterbalanced randomization sheet. The study nurse was not blind to the participant’s assigned drug condition so that she could provide the appropriate nasal spray to the participant. The experimenter and participants were blind to drug condition. During consent, participants were asked to verify that they had not smoked or used drugs or alcohol within the last 24 h, they had not exercised to drank caffeine within the last four hours, and that they had not eaten or drank anything with the exception of water within the last two hours. Female participants completed a urine pregnancy test facilitated by the study nurse. Participants were administered nasal spray OT or placebo under the supervision of the study nurse. All participants received a single dose of 24 international units (IU) of OT or placebo, intranasally (3 sprays per nostril, 4 IU per spray). Administration of 24 IU of OT has been shown to affect behavior in previous work (e.g., Bartz et al. 2011; Rilling et al. 2014). No participants reported side effects from the drug administration.
After drug administration, participants waited for approximately 40 min before starting the ER task. They were asked to refrain from potentially emotionally stimulating events (i.e., making phone calls, going online, and responding to emails) while waiting. They were provided with a standardized selection of magazines to read while in the waiting room. Approximately 30 min into the wait time, participants were moved to the testing room. They were administered a brief test of visual acuity, with a cutoff score of 20/40 required for continued testing. Participants then completed two practice trials and the ER task. Participants generally began the ER task between 40 and 45 min following drug administration. The average wait time was 42.93 min (SD = 3.81, range 40–60). The ER task took approximately 20 min.
Data Analyses
SPSS 20.0 and Mplus 7.4 were used to conduct the analyses. Correlations and regressions were used to test the effect of OT and group status on ER performance and visual attention. Regression analyses were conducted in Mplus using an estimator robust to non-normality (robust maximum likelihood, MLR).
Eye Fixation Variables
Eye movement parameters reflecting the topographical characteristics of scanning behavior were the proportion of fixations on previously defined regions of interest of the face: entire face, eye region, and mouth region. For the whole trial, we calculated average percent fixation data in the eye region relative to data in the face, and mouth region relative to face (see Lischke et al. 2012). Fixations were defined as the participant keeping their gaze within a 1 degree area for at least 100 milliseconds. From the reduced eye data, we extracted the proportion of fixation data relative to other data (i.e., sum of time length of each fixation during the trial divided by length of the trial) in each region of interest (i.e., face, eyes, mouth) for each face type (i.e., happy, sad, angry, fearful). Specifically, Face/Total = the proportion of fixation data captured in the face region relative to all fixation data captured; Eye/face = the proportion of fixation data captured in the eye region relative to the proportion of data captured in the face region; Mouth/face = the proportion of fixation data captured in the mouth region relative to proportion of data captured in the face region.
Results
Emotion Recognition Performance
ER accuracy and intensity variables for each face type were evaluated for normality. Accuracy data were non-normal for each face (all: skew = − 1.26 (0.31), kurtosis = 2.58 (0.61); happy: skew = − 4.24 (0.31), kurtosis = 16.49 (0.61); sad: skew = − 1.97 (0.31), kurtosis = 3.07 (0.61); angry: skew = − .62 (0.31), kurtosis = − .65 (0.61); fear: skew = − 1.84 (0.31), kurtosis = 3.76 (0.61)). For intensity data, angry faces were normally distributed, skew = .60 (.31), kurtosis = .35 (.61), and Q-Q plots appeared normal. The remainder of intensity data for each of the emotional face types was non-normal (all: skew = .87 (.31), kurtosis = 1.27 (.61); happy: skew = − .91 (0.31), kurtosis = .89 (0.61); sad: skew = .73 (0.31), kurtosis = 1.10 (0.61); fear: skew = .82 (0.31), kurtosis = .98 (0.61)). In our sample, overall accuracy scores ranged from .65 to 1 (M = .92, SD = .07). Overall intensity scores ranged from 21.03 to 75.53 (M = 40.50, SD = 11.02). See Fig. 2 for ER scores displayed by group and emotion category.
We predicted that the DEP group would require significantly more intensity to recognizing happy faces than the ANX group. Contrary to expectation, there were no significant differences between DEP and ANX groups on intensity scores for any face types (p > .05). We predicted that relative to DEP participants who received placebo, DEP participants who received OT would perform faster in their recognition of happy faces. To test this, we conducted a regression in which ER performance (dependent variable) was regressed onto drug condition and group (independent variables). The OT group was represented by a dummy code (OT = 1, placebo = 0). The regression also examined the interaction between OT and diagnostic group (DEP versus ANX), which was dummy coded (DEP = 1, ANX = 0). We conducted regression using the Mplus estimator MLR, due to non-normal data. A positive and significant main effect for OT, meaning that OT improves performance relative to placebo for happy faces, would partially support our hypothesis. A significant interaction term would support the hypothesis that OT improves recognition of happy faces specifically in depression. Overall intensity scores plotted by drug condition and emotion category are shown in Fig. 3. As shown in Table 1, a significant Group x Drug interaction effect was obtained for emotional intensity of happy face recognition (B = -9.70, p < .05). The strength of the effect was small (f2 = .08).
Emotion recognition intensity by drug condition and emotion category. a Level of emotional intensity to accurately identify the emotional expression on faces, for depressed (DEP) and anxious (ANX) participants, under oxytocin (OT) and placebo (PLAC) conditions. The interaction of Group × Drug is significant (p < .001). b Depicts emotion recognition intensity scores broken down by emotion category. DEP group revealed no significant differences between OT and placebo conditions, while ANX group showed significantly slower performance in the OT condition (p < .01)
Additionally, we examined the main effects and Group x Drug interaction in the prediction of other ER outcomes. The significant interaction effects for intensity of all faces (B = − 15.05, p < .01), happy faces (described above), sad faces (B = − 18.02, p < .01), angry faces (B = − 20.09, p < .01), and fearful faces (B = − 10.73, p < .05) reveal that while depression status and OT do not independently predict ER performance (the main effects were not significant), the interaction of these two conditions significantly predicted ER intensity for all of the face types. In predicting ER intensity, the addition of the interaction term uniquely accounted for 7–14% of the variance. The effect sizes of the significant interaction effects were small to medium per Cohen’s (1988) standards (f2 range .08–.16).
For intensity of happy faces, the regression coefficient for the omnibus interaction effect was 9.70, indicating that the effect of diagnostic group on intensity of happy faces differed 9.70 units as a function of the moderator (drug condition). To further examine the nature of the interaction effect, conditional slopes were considered that reflected the com slope of the outcome (e.g., intensity of happy faces) on the predictor (e.g., Group) at a specific value of the moderator (e.g., Drug condition). Compared to ANX participants, DEP participants had significantly higher intensity of happiness scores in the placebo condition (simple slope = 6.39, p < .05), but did not significantly differ in the OT condition (simple slope = − 3.31, p > .05). OT was associated with higher intensity (slower speed) than placebo for ANX patients (simple slope = 6.35, p < .05), but this effect was not significant in DEP patients where average intensity was 3.35 units lower in OT (p > .05). Thus, contrary to expectations, OT significantly slowed performance on happy faces for ANX participants, but OT had no significant impact on ER for happy faces in the DEP group. The results followed the same pattern in the remaining emotion categories.
Eye Fixation Data
Of the 60 participants recruited, 13 were excluded from eye tracking analyses due to erroneous or missing eye data. Of the 47 participants with eye data used in the analysis, nine were DEP participants who received OT, and 13 were ANX participants who received OT, 13 were DEP participants received placebo, and 12 were ANX participants who received placebo.
To test the main and interaction effects of Group and Drug on eye fixations, we conducted a hierarchical regression in which proportion of fixations in the eye region for each face type (dependent variable) was regressed onto diagnostic group and drug condition (independent variables), and the interaction between diagnostic group and drug. We created a composite score of proportion of fixations across trials, and also examined fixations across all four emotions. Figure 4 presents proportion of fixations in the eye region of each face type by drug and group status. Contrary to expectations, regressions indicated that the main effects of OT were not significant in predicting proportion of fixations in the eye region for any emotion category (p > .05). Instead, DEP status significantly predicted proportion of fixations in the eye region of sad faces (B = − 15.67, p < .05), but this effect was not found in any other emotion category. The size of this effect was small (f2 = .08), per Cohen’s guidelines (1988). DEP participants fixated less in the eye region of sad faces than ANX participants. The Group x Drug interaction effects were not significant in predicting proportion of fixations in the eye region for any emotion type.
Proportion of fixations in the eye region. a Proportion of fixations in the eye region for depressed (DEP) and anxious (ANX) participants in oxytocin (OT) and placebo (PLAC) conditions. b Depicts proportion of fixations in the eye region broken down by emotion category. In both a and b, no comparisons were statistically significant (p > .05)
Association Between Visual Attention and ER Performance
To determine the association between proportion of fixations in the face, eye, and mouth regions and intensity scores on the ER task, we conducted a series of correlation analyses for each emotion category. Results showed that increased attention (greater proportion of fixations) in the face region of happy faces (r = − .33, p < .05) and eye region of fearful faces (r = − .37, p < .05) was associated with significantly faster responding (i.e., smaller intensity scores). Results indicated that the relationship between attention to the mouth region and ER performance were not significant.
Effects of Sex on Emotion Recognition
We examined the effect of sex on ER by regressing accuracy and intensity scores onto a dummy code (0 = female, 1 = male). There were significant between-group sex differences for intensity of all faces (averaged) (p < .05), happy faces (p < .001), angry faces (p < .05), and fearful faces (p < .05). The only emotional face type that sex did not significantly impact was sadness (p > .05). For all other face intensities, females required a significantly lower intensity of the emotional face expression to accurately recognize the emotion. Sex did not moderate the relationship between ER and OT (p > .05). Thus, we can conclude that females were faster than males in recognizing happy, angry, and fearful faces, but OT and sex did not interact to influence ER performance.
Association Between Prediction of Drug Condition and Performance
Participants provided guesses about which condition (OT versus placebo) they were in at the end of the study. We tested for placebo effects by comparing what participants thought they received to what they actually received. Participants were generally not accurate in perceiving their drug condition, as only 56.6% were correct in their predictions. A 2 × 2 Chi square test was conducted to determine actual versus perceived drug condition. The results of this test were not significant, χ2 (1, N = 60) = 1.11, p = .29. There was not a statistically significant association between actual and perceived drug condition. Additionally, we compared ER accuracy and intensity scores between participants who believed they received OT and those who believed they received placebo using ANOVA analyses. There were no significant differences in ER performance based on whether participants believed they received OT compared to placebo.
Discussion
The present study used a double-blind, placebo-controlled design to explore the impact of OT on visual attention and ER performance. Although many studies have investigated OT’s effects on ER (see Shahrestani et al. 2013, for a meta-analysis) or visual attention in affective disorders (see Armstrong and Olatunji 2012, for a review), this study is novel in its exploration of OT and visual attention in a diagnostically diverse sample of outpatients with emotional disorders. Indeed, this study was the first to examine if the effects of OT on ER and visual attention were moderated by mood disorder status.
Based on the extant literature, we expected the DEP group would be slower and less accurate in identifying happy faces (e.g., Joormann et al. 2006, Yoon et al. 2009). This hypothesis was not upheld, as group status did not predict ER intensity for happy faces. A potential explanation for the nonsignificant main effect of Group on ER is that the clinical severity of mood disorders in the DEP group was not sufficiently high to find the conjectured ER deficits. As noted earlier, ADIS-5 interviewers assigned CSRs for all disorders that met the DSM-5 diagnostic threshold (CSR = 4–8). In our sample, the clinical severity of DSM-5 mood disorders in the DEP group was relatively low (CSR M = 4.8). In fact, 25 of the 30 cases had CSRs no higher than 5, which is considered in the mild to moderate range of clinical depression. It would be informative in future studies to recruit participants with an even broader range of clinical mood symptoms, which may aid in the identification of diagnostic group differences.
We found significant Group x Drug interaction effects for ER intensity. OT impacted DEP and ANX participants in opposite ways, making ANX participants slower and DEP participants faster. Examination of the nature of this interaction indicated that the effect of OT on ER performance in DEP participants was not significant. OT significantly increased the amount of emotional intensity required for ANX participants to accurately recognize the emotion of the face stimuli (slowed performance). On the other hand, OT did not significantly alter the amount of emotional intensity required for DEP participants to accurately recognize the emotion of the face stimuli, although the effect approached significance in the opposite direction in the ANX group. Taken together, our results show that OT had a greater effect on slowing ANX participants’ ER performance for all face types than it did on improving DEP performance. We expected that OT would make DEP participants faster and more accurate in identifying happiness, but this hypothesis was not upheld, as the significant Group x Drug interaction effect is not due to OT improving DEP speed, but rather, OT slowing down ANX participants. It is possible that OT increases symptoms of anxiety in the ANX group, thus slowing their performance, but OT combined with anxiety and depression (DEP group) does not produce this anxiogenic effect because mood disorder status interacts with OT in some unknown manner. Other researchers have noted the “acute anxiogenesis” that occurs with OT (MacDonald et al. 2013), and our study adds to the literature on the perplexing, heterogeneous subjective effects of intranasal OT. Overall, these findings emphasize the importance of considering both contextual and inter-individual factors to better understand why OT affected DEP and ANX participants differently. Factors including genetic variation, childhood trauma, hormonal status, the salience of the social environment, and attachment style may amplify the positive or negative effects of OT for some individuals (Olff et al. 2013).
Contrary to expectations, we did not find a significant relationship between eye gaze in the eye region and OT administration. This inconsistency with the prior literature could be due to the fact that much of the eye tracking literature on OT uses healthy male participants (e.g., Domes et al. 2013; Guastella et al. 2008), or autism spectrum disorder, and we used a clinical sample of men and women with mood and anxiety disorders. The main effect of Group was significant in predicting proportion of fixations in the eye region of sad faces: DEP participants fixated less on the eyes of sad faces than ANX participants. Further research is needed to examine why OT had a nonsignificant effect in DEP cases in speed and visual attention, and a slowing effect on ANX participants. These studies should include additional variables (i.e., trust, empathy, confidence, time visual stimuli are presented) that may account for why the drug manipulation impacted DEP and ANX groups differently.
Although our findings did not indicate a significant relationship between OT and visual attention, participants were faster in identifying fear if they made more fixations in the eye region of fearful faces. Additionally, the more participants looked at the eye region of happy faces, the faster they performed in identifying happiness. Our findings are at odds with Lischke et al. (2012), who found that OT improved ER, but did not impact eye gaze, as we found a significant connection between gaze and ER performance, which was not specific to the OT group. A notable difference between these two studies is that the current study used a clinical sample. Our study also used dynamic faces, which is an update from prior studies that used static faces and found a direct connection between gaze in the eye region and OT (e.g., Guastella et al. 2008). In comparing results from ER tests with static faces to those with dynamic faces, there is reason to believe that the eye region is especially salient in static faces (cf. Emery 2000), which may account for differences between studies. Some researchers have suggested that with dynamic faces, the orienting effect of OT to eye gaze probably becomes less relevant with the increasing duration of the stimulus (Lischke et al. 2012).
It is also possible that OT increases the salience of social cues and benefits individuals most who are less in tune with social information, but does not benefit individuals who are already socially adept (Hubble et al. 2017). This may explain why OT has shown significant effects on ER in samples with autism spectrum disorder, but did not have a significant effect in our sample. An evaluation of ER in the context of traditional neuropsychological measures is recommended, as factors such as intelligence and attention have been associated with ER performance (Marsh and Blair 2008).
Although the clinical sample was a notable strength of our research design, some limitations should be considered. For instance, a recent review by Walum et al. (2016) concluded that the majority of research using intranasal OT is underpowered, which heightens the probability that most published OT findings will not be replicated because of high false negative rates. Based on this current state of affairs, results on OT’s effects on human behavior should be interpreted with “healthy skepticism” (Walum et al. 2016). As previously noted, we could not use 13 out of 60 participants’ eye data due to mechanical or calibration errors, which limited our sample size by almost 22%. Thus, the eye tracking results should be interpreted with caution. Using more fine-grained eye tracking methods or advanced technologies is a recommended direction for future research.
One of the major barriers to progress in understanding ER lies in in the tasks that researchers use to measure ER. Of the basic emotion categories traditionally examined in research, happiness is typically the most easily recognized across tasks, making tasks using happy stimuli particularly vulnerable to ceiling effects (cf., Ekman et al. 1987). These ceiling effects make findings of preserved or intact happiness recognition in a particular age or clinical group difficult to interpret. Due to the ceiling effects of happiness recognition (accuracy) in our sample, we were unable to examine group differences between depressed and anxious participants because of no variance between the groups. However, due to our design where the intensity of the face stimuli was systematically varied, examining group differences in intensity scores was possible. Notably, the larger range of scores shown here suggests a lack of ceiling effect.
While our nasal spray administration was standardized per the recommendations of Guastella et al. (2013), for several reasons, this method does not guarantee that each participant received the exact same dosage (see Quintana et al. 2016, for a review). First, physical and chemical factors such as stability, lipophilicity, and molecular weight can influence intranasal drug delivery. Next, nasal cavity physiology can limit the accuracy and consistency of drugs administered nasally. Additionally, similar and reliable spray deposition and bioavailability need to be achieved. Lastly, the optimal dosage in clinical participants is unknown. Of note, future OT studies including females should also examine the potential confounding influences of hormone cycling, as this was not controlled for in the current study, which is a limitation. A final limitation of this study is the lack of healthy control group for comparison to DEP and ANX groups.
Future studies should examine the impact of intranasal OT on depression and anxiety symptoms during treatment. ER deficits in depression are only one aspect of the disorder, and it is unknown whether improvements in ER via OT administration or otherwise would improve the symptoms of depression (or anxiety). Treatments that reduce depression may be ineffective in preventing their development (McQuaid et al. 2014). Studies aimed at correcting ER biases could be developed as an adjunct treatment for emotional disorders, but it is not yet determined what, if any, role of OT would play in this intervention. The specific role of OT in depression and anxiety treatments requires additional research to clarify the mechanism responsible for its differential impact across disorders.
In sum, there remains much to be learned about the effects of OT on ER in patients with mood and anxiety disorders, and the variables that may moderate this relationship (e.g., personality, genetic, contextual factors). The differential impact of OT on ER in the ANX and DEP groups suggests that, in clinical samples, the nature of OT’s effects on ER vary depending on the patient’s symptoms. Instead of the posited beneficial effect, we found that OT interacts with anxiety disorder status to have a deleterious effect on ER. The specific symptom features or processes that underlie this differential response pattern await future research.
References
Armstrong, T., & Olatunji, B. O. (2012). Eye tracking of attention in the affective disorders: A meta-analytic review and synthesis. Clinical Psychology Review, 32, 704–723.
Bartz, J. A., Zaki, J., Bolger, N., & Ochsner, K. N. (2011). Social effects of oxytocin in humans: Context and person matter. Trends in Cognitive Sciences, 15, 301–309.
Bouhuys, A. L., Geerts, E., & Gordijn, M. C. M. (1999). Depressed patients’ perceptions of facial emotions in depressed and remitted states are associated with relapse: A longitudinal study. Journal of Nervous and Mental Disease, 187, 595–602.
Bouhuys, A. L., Geerts, E., & Gordijn, M. C. M. (1999). Gender specific mechanisms associated with outcome of depression: Perception of emotions, coping and interpersonal functioning. Psychiatry Research, 85, 247–261.
Brown, T. A., & Barlow, D. H. (2014). Anxiety and related disorders interview schedule for DSM-5—adult and lifetime version: Clinician manual. New York: Oxford University Press.
Carton, J. S., Kessler, E. A., & Pape, C. L. (1999). Nonverbal decoding skills and relationship well-being in adults. Journal of Nonverbal Behavior, 23, 91–100.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Hillside: Erlbaum.
Di Simplicio, M., Massey-Chase, R., Cowen, P. J., & Harmer, C. J. (2009). Oxytocin enhances processing of positive versus negative emotional information in healthy male volunteers. Journal of Psychopharmacology, 23, 241–248.
Domes, G., Normann, C., & Heinrichs, M. (2016). The effect of oxytocin on attention to angry and happy faces in chronic depression. BMC Psychiatry, 16, 92.
Domes, G., Steiner, A., Porges, S. W., & Heinrichs, M. (2013). Oxytocin differentially modulates eye gaze to naturalistic social signals of happiness and anger. Psychoneuroendocrinology, 38, 1198–1202.
Durand, A. C., & Gould, G. M. (1910). A method of determining ocular dominance. Journal of the American Medical Association, 55, 369–370.
Ekman, P., & Friesen, W. V. (1976). Pictures of facial affect. Palo Alto: Consulting Psychologists Press.
Ekman, P., Friesen, W. V., O’Sullivan, M., Chan, A., Diacoyanni-Tarlatzis, I., Heider, K.,.. . Tzavaras, A. (1987). Universals and cultural differences in the judgments of facial expressions of emotion. Journal of Personality and Social Psychology, 53(4), 712–717.
Ellenbogen, M. A., Linnen, A., Cardoso, C., & Joober, R. (2013). Intranasal oxytocin impedes the ability to ignore task-irrelevant facial expressions of sadness in students with depressive symptoms. Psychoneuroendocrinology, 38, 387–398.
Emery, N. J. (2000). The eyes have it: the neuroethology, function and evolution of social gaze. Neuroscience and Biobehavioral Reviews, 24, 581–604.
Fischer-Shofty, M., Shamay-Tsoory, S. G., Harari, H., & Levkovitz, Y. (2010). The effect of intranasal administration of oxytocin on fear recognition. Neuropsychologia, 48, 179–184.
Guastella, A. J., Hickie, I. B., McGuinness, M. M., Otis, M., Woods, E. A., Disinger, H. M., &… Banati, R. B. (2013). Recommendations for the standardization of oxytocin nasal administration and guidelines for its reporting in human research. Psychoneuroendocrinology, 38, 612–625.
Guastella, A. J., & MacLeod, C. (2012). A critical review of the influence of oxytocin nasal spray on social cognition in humans: Evidence and future directions. Hormones And Behavior, 61, 410–418.
Guastella, A. J., Mitchell, P. B., & Dadds, M. R. (2008). Oxytocin increases gaze to the eye region of human faces. Biological Psychiatry, 63, 3–5.
Gur, R. C., Erwin, R. J., Gur, R. E., Zwil, A. S., Heimberg, C., & Kraemer, H. C. (1992). Facial emotion discrimination: II. Behavioral findings in depression. Psychiatry Research, 42, 241–251.
Hale, W. W., III (1998). Judgment of facial expressions and depression persistence. Psychiatry Research, 80, 265–274.
Heinrichs, M., von Dawans, B., & Domes, G. (2009). Oxytocin, vasopressin, and human social behavior. Frontiers in Neuroendocrinology, 30, 548–557.
Hubble, K., Daughters, K., Manstead, A. S. R., Rees, A., Thapar, & van Goozen, S. H. M. (2017). Oxytocin reduces face proecssing time but leaves recognition accuracy and eye-gaze unaffected. Journal of the International Neuropsychological Society, 23, 23–33.
Joormann, J., & Gotlib, I. H. (2006). Is this happiness I see?: Biases in the identification of emotional facial expressions in depression and social phobia. Journal of Abnormal Psychology, 115, 705–714.
Leppanen, J., Ng, K. W., Tchanturia, K., & Treasure, J. (2017). Meta-analysis of the effects of intranasal oxytocin on interpretation and expression of emotions. Neuroscience and Biobehavioral Reviews, 78, 125–144.
Lischke, A., Berger, C., Prehn, K., Heinrichs, M., Herpertz, S. C., & Domes, G. (2012). Intranasal oxytocin enhances emotion recognition from dynamic facial expressions and leaves eye-gaze unaffected. Psychoneuroendocrinology, 37, 475–481.
MacDonald, K., MacDonald, T. M., Brüne, M., Lamb, K., Wilson, M. P., Golshan, S., & Feifel, D. (2013). Oxytocin and psychotherapy: A pilot study of its physiological, behavioral and subjective effects in males with depression. Psychoneuroendocrinology, 38, 2831–2843.
Marsh, A. A., & Blair, R. J. R. (2008). Deficits in facial affect recognition among antisocial populations: A meta-analysis. Neuroscience and Biobehavioral Reviews, 32, 454–465.
Marsh, A. A., Yu, H. H., Pine, D. S., & Blair, R. J. R. (2010). Oxytocin improves specific recognition of positive facial expressions. Psychopharmacology (Berl), 209, 225–232.
McClure, E. B., & Nowicki, S. J. (2001). Associations between social anxiety and nonverbal processing skill in preadolescent boys and girls. Journal of Nonverbal Behavior, 25, 3–19.
McQuaid, R. J., McInnis, O. A., Abizaid, A., & Anisman, H. (2014). Making room for oxytocin in understanding depression. Neuroscience and Behavioral Reviews, 45, 305–322.
Olff, M., Frijling, J. L., Kubzansky, L. D., Bradley, B., Ellenbogen, M. A., Cardoso, C., & … van Zuiden, M. (2013). The role of oxytocin in social bonding, stress regulation and mental health: An update on the moderating effects of context and interindividual differences. Psychoneuroendocrinology, 38, 1883–1894.
Persad, S. M., & Polivy, J. (1993). Differences between depressed and nondepressed individuals in the recognition of and response to facial emotional cues. Journal of Abnormal Psychology, 102, 358–368.
Quintana, D. S., Guastella, A. J., Westlye, L. T., & Andreassen, O. A. (2016). The promise and pitfalls of intranasally administered psychopharmacological agents for the treatment of psychiatric disorders. Molecular Psychiatry, 21, 29–38.
Rilling, J. K., Demarco, A. C., Hackett, P. D., Chen, X., Gautam, P., Stair, S., &. Pagnoni, G. (2014). Sex differences in the neural and behavioral response to intranasal oxytocin and vasopressin during human social interaction. Psychoneuroendocrinology, 39, 237–248.
Schulze, L., Lischke, A., Greif, J., Herpertz, S. C., Heinrichs, M., & Domes, G. (2011). Oxytocin increases recognition of masked emotional faces. Psychoneuroendocrinology, 36, 1378–1382.
Shahrestani, S., Kemp, A. H., & Guastella, A. J. (2013). The impact of a single administration of intranasal oxytocin on the recognition of basic emotions in humans: A meta-analysis. Neuropsychopharmacology, 38, 1929–1936.
Shultz, S., & Dunbar, R. M. (2012). The social brain hypothesis: An evolutionary perspective on the neurobiology of social behaviour. In S. Richmond, G. Rees, S. L. Edwards, S. Richmond, G. Rees & S. L. Edwards (Eds.), I know what you’re thinking: Brain imaging and mental privacy (pp. 13–28). New York: Oxford University Press.
Tollenaar, M. S., Chatzimanoli, M., van der Wee, N. A., & Putman, P. (2013). Enhanced orienting of attention in response to emotional gaze cues after oxytocin administration in healthy young men. Psychoneuroendocrinology, 38, 1797–1802.
Van Ijzendoorn, M. H., & Bakermans-Kranenburg, M. J. (2012). A sniff of trust: Meta-analysis of the effects of intranasal oxytocin administration on face recognition, trust to in-group, and trust to out-group. Psychoneuroendocrinology, 37, 438–443.
Walum, H., Waldman, I. D., & Young, L. J. (2016). Statistical and methodological considerations for the interpretation of intranasal oxytocin studies. Biological Psychiatry, 79, 251–257.
Yoon, K. L., Joormann, J., & Gotlib, I. H. (2009). Judging the intensity of facial expressions of emotion: Depression-related biases in the processing of positive affect. Journal of Abnormal Psychology, 118, 223–228.
Acknowledgements
The authors thank Alice Cronin-Golomb and Kristin Long for their assistance with this study. This research was supported by Grant MH039096 awarded by the National Institute of Mental Health (Brown) and the Boston University Clara Mayo Fellowship (Rutter).
Funding
This study was funded by the National Institute of Mental Health Grant MH039096.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Lauren A. Rutter, Daniel J. Norton, Bonnie S. Brown and Timothy A. Brown declare that they have no conflict of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rutter, L.A., Norton, D.J., Brown, B.S. et al. A Double-Blind Placebo Controlled Study of Intranasal Oxytocin’s Effect on Emotion Recognition and Visual Attention in Outpatients with Emotional Disorders. Cogn Ther Res 43, 523–534 (2019). https://doi.org/10.1007/s10608-018-9974-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-018-9974-x