Abstract
This study aims to investigate the intricacies of inpatient psychosocial rehabilitation by examining a community-based mental health inpatient rehabilitation service in Nova Scotia, Canada. It provides a comparative analysis with national standards using the Quality Indicator for Rehabilitative Care (QuIRC) and offers recommendations for improvement. The study will link findings to research on enhancing specific domains, focusing on strategies to address identified challenges and leverage opportunities to meet or exceed national benchmarks in promoting recovery and social inclusion. This study utilizes the QuIRC as a primary assessment tool to evaluate the quality of care in psychiatric and psychosocial rehabilitation care unit. The QuIRC assessment findings reveal crucial insights across several domains, including the living and therapeutic environment, treatments and interventions, self-management and autonomy, social interface, human rights, and recovery-based practices. The study identifies strengths and areas for improvement by comparing unit scores with national averages in Canada, offering a detailed examination of the quality of care provided in a community-based psychosocial rehabilitation service. Using the QuIRC identifies strengths and areas for improvement of current care provided, opening opportunities for positive change and improved quality of care. By highlighting the critical indicators of the quality of care and best practices derived from the QuIRC assessment, this study provides practical insights that can be directly applied by practitioners, policymakers, and stakeholders, fostering an understanding of essential elements that support effective mental health rehabilitation within community settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
This article provides a detailed analysis of the Quality Indicator for Rehabilitative Care (QuIRC) assessment conducted at a community-based psychosocial rehabilitation unit that has been in operation since 2012. The evaluation encompasses demographic information, staffing details, and the unit’s performance across seven care domains. It identifies strengths and areas for improvement and offers recommendations to enhance the quality of care.
The Quality Indicator for Rehabilitative Care (QuIRC) is a standardized, international quality assessment webtool (www.quirc.eu) for inpatient and community rehabilitation units. Although completed by managers of the service, during its development, the ratings were validated against service users’ experiences of care and autonomy and were found to correlate well. The QuIRC tool assesses the provision of care across seven domains: (1) living environment, (2) therapeutic environment, (3) treatments and interventions, (4) self-management and autonomy, (5) social interface, (6) human rights, and (7) recovery-based practice. The tool is the product of collaborative work involving 11 centers in 10 European countries and was determined based on the evidence on crucial components of care gleaned from different studies and systematic reviews (Killaspy et al., 2009; 2011; 2012a, b; Taylor et al., 2009; Turton et al., 2010).
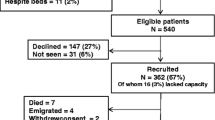
The studied psychosocial rehabilitaion unit was established in 2012 in Nova Scotia, Canada, it had 40 beds and specializes in inpatient rehabilitative care for patients with severe and persistent mental illness (SPMI). This manuscript discusses the findings from the QuIRC assessment performed on December 7, 2015, delivering insights into the unit’s performance across crucial care domains.
Demographic and Staffing Overview
At the time of the assessment, 37.5% of the beds were occupied, with a patient demographic of 60% males. The mean age was (37) for males and (44) for females. The mean Length of Stay (LOS) for males and females was (155) and (251) days, respectively. Female patients stayed longer by 96 days, but there was no statistically significant difference between the mean of LOS of both genders, independent t-test, p = 0.1 (95% CI -224 to 32). The source of referrals was mainly from acute inpatient services, 79%, followed by community-based services, 14%, and other clinical settings, e.g. short stay unit and locked rehab wards, 7%. The most common diagnosis was schizophrenia 44%, followed by schizoaffective disorder 11%, drug-induced psychosis 10%, personality disorders 9%, learning disability and psychosis 7.5%, organic brain syndrome 7.5%, bipolar disorder 5%, the rest were psychosis not otherwise specified (NOS), and autistic spectrum disorder 6%.
No patients were detained involuntarily, and there was no maximum length of stay. The staff comprised 45 full-time equivalent (FTE) employees, including psychiatrists, occupational therapists, recreational therapists, nurses, support workers, social workers, and arts therapists, with a turnover of 13% in the two years prior to the study.
Domain-wise Performance
Table (1) Presents a comparative analysis of the unit’s performance against national averages, highlighting its strengths and potential areas for enhancement in the context of psychosocial rehabilitation domains.
Domain-Specific Analysis and Recommendations, as Suggested by the QuIRC
-
1.
Living Environment (LE): The unit scored 75%, above the country average of 64%. Recommendations to excel further include enhancing outdoor space, creating a homelike environment, minimizing rules, and promoting resident decision-making. However, the essential practices to excel further include providing pleasant outdoor spaces and creating a home-like environment. Flexible visiting hours and minimal rules promote comfort and autonomy. Communicating facility guidelines ensures mutual respect, while flexible mealtimes accommodate individual preferences. Involving residents in decision-making and community activities enriches their experience and promotes well-being.
-
2.
Therapeutic Environment (TE): With a score of 68%, recommendations to enhance this domain would include prioritizing a high staff-to-service user ratio, minimizing staff turnover, and reducing reliance on temporary staff. Promote continuous professional development, ensure adequate supervision, and adhere to evidence-based guidelines. Conduct regular audits, use benchmarking for performance evaluation, and collaborate with external agencies. Deliver client-centered care by involving patients and their families in decision-making and encouraging community participation. These strategies will significantly improve care quality and service delivery.
-
3.
Treatments and Interventions (TI): Excelling at 73%, the unit was encouraged to improve further by facilitating meaningful engagement in mainstream activities like education, employment, voluntary work, and essential leisure. This includes providing access to psychological interventions, regular medication, and health assessments and promoting a healthy lifestyle. Integrating medical, psychological, and social support is prioritized while minimizing and carefully managing physical restraint and seclusion through proper training and clear protocols, with ongoing review and support for staff and residents.
-
4.
Self-Management & Autonomy (SMA): Scoring 63%, suggested improvements included enhancing service delivery and empowering patients, residents, and service users; the unit should facilitate the gradual assumption of personal care responsibilities through relevant programs, promote active engagement in care decisions and facility operations, and hold regular community meetings. Precise information on decision-making powers, support for community participation, relationship maintenance, and respect for privacy are essential. Offering choices in daily routines and providing access to self-catering and laundry facilities enhance autonomy and quality of life.
-
5.
Social Interface (SI): Excelling with 81%, recommendations aimed at encouraging community engagement through voting, family involvement, and linking with community resources is crucial. Supporting meaningful occupation in mainstream settings promotes social integration and personal growth in education, training, employment, and leisure activities.
-
6.
Human Rights (HR): With a 67% score, ensuring and promoting patient rights involves providing clear information about their rights and accessible complaint procedures for resolving grievances. Engaging individuals in care decisions promotes autonomy while accessing advocacy services supports navigating complex systems. Promoting citizenship through community involvement fosters social integration. Regular physical assessments monitor health status, and minimizing physical restraint and seclusion emphasizes dignity and alternative approaches to safety. These practices uphold patient-centred care, respecting rights, and enhancing healthcare quality.
-
7.
Recovery-Based Practice (RBP): The unit scores 64%. It would be crucial to empower patients in decision-making about their treatment and care to improve this domain. This includes promoting their involvement in the facility management and community activities and facilitating family support. Providing clear information about their decision-making powers and promoting the gradual assumption of personal care responsibilities fosters independence. Encouraging civic engagement through voting and community involvement enhances social integration. Emphasizing a healthy lifestyle complements these efforts, ensuring comprehensive well-being and quality of life. These practices collectively promote autonomy, community integration, and holistic health in patient-centred care approaches.
Conclusion
This analysis of a community-based inpatient psychosocial rehabilitation unit’s performance through the QuIRC assessment highlights notable strengths and areas for improvement. Implementing the recommended actions can significantly enhance the quality of care, aligning with the commitment to delivering patient-centred psychosocial rehabilitative care.
References
Killaspy, H., King, M., Wright, C., & Others (2009). Study protocol for the development of a European measure of best practice for people with long-term mental health problems in institutional care (DEMoBinc). Bmc Psychiatry, 9, Article36. https://doi.org/10.1186/1471-244X-9-36
Killaspy, H., White, S., Wright, C., & Others (2011). The development of the Quality Indicator for Rehabilitative Care (QuIRC): A measure of best practice for facilities for people with longer-term mental health problems. Bmc Psychiatry, 11, 35. https://doi.org/10.1186/1471-244X-11-35
Killaspy, H., White, S., Wright, C., & Others (2012a). Association between service user experiences and staff rated quality of care in European facilities for people with longer-term mental health problems. Plos One, 7(6), e38070. https://doi.org/10.1371/journal.pone.0038070
Killaspy, H., White, S., Wright, C., et al. (2012b). European facilities for people with longer-term mental health problems. Plos One, 7(6). https://doi.org/10.1371/journal.pone.0038070. Article e38070
Taylor, T. L., Killaspy, H., Wright, C., & Others (2009). A systematic review of the international published literature relating to quality of institutional care for people with longer-term mental health problems. Bmc Psychiatry, 9. https://doi.org/10.1186/1471-244X-9-55. Article 55
Turton, P., Wright, C., White, S., & Others (2010). Promoting recovery in long-term mental health institutional care: An international Delphi study of stakeholder views. Psychiatric Services, 61(3), 293–299. https://doi.org/10.1176/ps.2010.61.3.293
Acknowledgements
We sincerely thank the dedicated team members of our psychosocial rehabilitation unit whose unwavering commitment to patient care and recovery exemplifies excellence in healthcare. Their collective efforts, marked by innovative treatment strategies, compassionate patient interactions, and strong interprofessional collaboration, significantly contributed to the therapeutic environment we strive to uphold. Their resilience and collaborative spirit enhanced patient outcomes and foster a supportive workplace culture conducive to professional growth and mutual respect. It is with great appreciation that we acknowledge their invaluable contributions to our shared mission of providing high-quality rehabilitative care.
Funding
Not Applicable.
Author information
Authors and Affiliations
Contributions
The first draft of the manuscript was written by Dr. Mahmoud A. Awara who along with the second author contributed to the study conception and design, material preparation, data collection and analysis.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
Nova Scotia Health Research Ethics Board (REB) has approved this study for publication after REB review exemption - REB FILE #:1,030,461.
Competing Interests
Not Applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Awara, M., Green, J.T. Exploring the Quality-of-Care Dynamics of Inpatient Psychosocial Rehabilitation in Community-Based Mental Health Services: A Comprehensive Analysis. Community Ment Health J (2024). https://doi.org/10.1007/s10597-024-01325-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10597-024-01325-z