Abstract
The Clubhouse model of psychosocial rehabilitation supports individuals with mental health challenges using a person centered and recovery-oriented approach. Clubhouses around the world have been found to be effective in supporting their member’s recovery. However, there is a lack of multi-site and longitudinal studies on the Clubhouse model. Therefore, the purpose of the present study was to longitudinally assess the psychosocial outcomes of Clubhouse members across six accredited Clubhouses in Canada. Due to the COVID-19 pandemic occurring midway through the study, a secondary aim was to assess the impact of the pandemic on the psychosocial outcomes of Clubhouse members. A total of 462 Clubhouse members consented to participate in the study. Members completed a questionnaire battery every 6 months over a 2-year period (five data points total). The last three data points were collected during the COVID-19 pandemic. Psychosocial outcomes included mental health symptoms, substance use, community integration, and satisfaction with life, and were analyzed using multilevel growth models. The results indicated that satisfaction with life and psychological integration increased over the study period, while mental health symptoms, substance use, and physical integration decreased. Examining Clubhouse participation, length of Clubhouse membership and frequency of Clubhouse use predicted higher life satisfaction, lower substance use, and fewer mental health symptoms over the study period. The results of the present study provide invaluable insight into the psychosocial impact of Clubhouses on Canadian Clubhouse members, particularly during COVID-19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recovery-oriented mental healthcare that emphasizes living a hopeful, satisfying, and contributing life, has made significant impacts across mental health systems around the world. In Canada, policy and practice has implemented a “recovery orientation” and the creation of recovery-oriented guidelines (Mental Health Commission of Canada, 2015). Many recovery-oriented services exist in the country, including psychosocial rehabilitation programs, that aim to facilitate recovery by emphasizing individuals’ strengths and providing access to resources to live successfully in the community.
The Clubhouse model of psychosocial rehabilitation is one such program that takes a person-centered and recovery-oriented approach to supporting its members (McKay et al., 2018). For those who have experienced mental health challenges, participating in Clubhouses offers an opportunity to re-engage in the relationships, employment, education, and support they need to continue their recovery. Clubhouses are located in the community and offer programming such as the “work-ordered day”, transitional and supported employment, social and recreational events, and affordable housing. Over 320 Clubhouses currently exist in more than 30 countries around the world. In Canada, there are 13 Clubhouses, of which eight are accredited by Clubhouse International.
Clubhouses have been found to be effective at reducing loneliness, isolation, and mental health symptoms, and increase meaningful work and sense of community (McKay et al., 2018). The Clubhouse model has been studied around the world, however, few studies to date have been conducted with Canadian Clubhouses. Therefore, the purpose of the present study was to assess the longitudinal psychosocial outcomes of Canadian Clubhouse members. Further, the present study occurred before and during the COVID-19, and so a secondary aim of the study was to assess the trajectories of Clubhouse members during the pandemic.
The Clubhouse Model
The Clubhouse model follows a set of values that underscores that meaningful work, as well as social and recreational opportunities, are an important part of a person’s path to recovery. The main program component of the Clubhouse is the work-ordered day. This component involves the structure of the day-to-day activities within a Clubhouse, where staff and members work side-by-side to run the Clubhouse. The Clubhouse is organized into various units in which members can choose to work, to help members develop self-esteem, confidence, and friendships. Members also have the opportunity to be involved in administration, research, and evaluation of Clubhouse effectiveness. Clubhouses must follow a set of standards that form the basis of a Clubhouse Accreditation process. These standards provide oversight on membership, relationships, space, work-ordered day, employment, education, as well as governance and administration.
Effectiveness of The Clubhouse Model
Clubhouses around the world have demonstrated effectiveness in supporting the recovery of their members. A systematic review of research on Clubhouses noted a positive impact on employment outcomes, hospitalization rates, social networks, and quality of life (McKay et al., 2018). The authors discuss numerous limitations with the current evidence base of Clubhouses, including that a third of the studies included were conducted more than ten years prior, a lack of rigorous methods, and a need to study accredited Clubhouses that have fidelity to the model. Therefore, there is a need to update the evidence base.
Since this review, several studies have been conducted, using various methodologies. A randomized controlled trial (RCT) conducted in China found that compared to the control group, Clubhouse members had reductions in psychiatric symptoms and better social function, self-determination, and quality of life at the 6-month follow up, but no differences were found in hospitalization rates (Chen et al., 2020). A quantitative participatory study conducted in a Clubhouse in Paris found that over an 18-month period, members experienced improvements in quality of life, self-efficacy, psychosocial skills, mental health symptoms, and hospitalization rates (Bouvet, et al., 2021). Further, numerous qualitative studies have been conducted that have noted the impact of Clubhouses on the lives of members (Desai et al., 2021; Pernice et al. 2021; Tanaka et al., 2021; Vescey et al., 2023). To our knowledge, there has never been a multi-site, longitudinal study on the psychosocial outcomes of Clubhouse members.
To date, there is a scarcity of research on the Clubhouse model in Canada. Studies have been completed that have developed and tested a program theory of a Clubhouse in Canada (Mutschler et al., 2018; Rouse et al., 2017). Other studies in Canada have examined the hospitalization rates of Clubhouse members (Russell et al., 2022) and qualitatively examined the implementation of Transitional Employment in a Clubhouse (Reidel et al., 2021). Our research team has recently published papers examining the hospitalization rates and employment outcomes of Canadian Clubhouse members during the COVID-19 pandemic (Junaid et al., 2023; Mutschler et al., 2023). Further examination of the longitudinal psychosocial outcomes of Clubhouse members across Canada is needed.
Clubhouse Outcomes during COVID-19
Individuals with severe mental illness have significant challenges with social isolation, due to mental health symptoms, marginalization, and stigma (Wang et al., 2017). During the COVID-19 pandemic, those with mental health concerns faced increased psychosocial problems (e.g., isolation, fear, anxiety), poorer physical health, and lack of access to care (Sukut & Ayhan Balik, 2021). Further, Clubhouses in Canada had to adapt their programming in order to align with public health mandates on social distancing. Program adaptations included moving all programming to virtual formats, increasing phone calls to members, and providing meals (Mutschler et al., 2021). Few studies have been conducted on how Clubhouse members were supported by Clubhouses during the pandemic. Hinchey and colleagues (2022) found that Clubhouse members with high levels of engagement during the pandemic reported better mental and physical health ratings over time than those with low levels of engagement. Junaid et al. (2023) found a significant reduction in employment for Clubhouse members who were unable to access the employment opportunities offered by the Clubhouse because of the pandemic. Given the few studies conducted to date, there is a considerable gap in the literature on how Clubhouse members’ psychosocial functioning was impacted by the global pandemic.
Purpose
Clubhouses around the world have been found to be effective in supporting their member’s recovery (McKay et al., 2018). No multi-site study has been conducted to date, and few longitudinal studies have documented Clubhouse members’ outcomes. Therefore, the purpose of the present study was to longitudinally assess the psychosocial outcomes of Clubhouse members across six accredited Clubhouses in Canada. Due to the COVID-19 pandemic occurring midway through the study, a secondary aim was to assess the impact of the pandemic on the psychosocial outcomes of Clubhouse members.
Method
Sample
Six accredited Clubhouses across Canada were involved in the present study: Alberta (n = 1), Ontario (n = 2), Nova Scotia (n = 1), and Prince Edward Island (n = 2). The number of active members (attended the Clubhouse in the past 90 days) from each Clubhouse is: 1200 (Progress Place), 163 (Oak Centre), 172 (Potential Place), 100 (Crossroads), 326 (Fitzroy), and 144 (Notre Dame Place). From this population, a total of 462 Clubhouse members across the six sites consented to participate in the study. The average age of participants was 48.8 years (SD = 12.6) and 43.8% were female. The most commonly self-reported mental health diagnoses were depression (45.9%), anxiety (40.6%), and schizophrenia (35.1%). Full demographic information can be found in Table 1. Clubhouse utilization rates can be found in Table 2.
Measures
Self-reported demographic information was provided by Clubhouse members in the baseline survey, including age, gender, education, housing status, and mental health diagnosis. Various psychosocial measures were administered at each timepoint. The Satisfaction with Life Scale (SWLS) is a 5-item Likert measure of global life satisfaction (Diener et al., 1985). In the present study, internal consistency (alphas) ranged from 0.87- 0.91. The Modified Colorado Symptom Index (MCSI) is a 14-item Likert scale that measures psychological symptoms (Conrad et al., 2001). It has been found to be a reliable and valid measure with individuals who have mental illness and histories of homelessness (alphas = 0.89- 0.90). The GAIN Short Screener (GAIN-SS) is a 5-item Likert screener used to assess substance use (Dennis et al., 2006). It has good reliability (alphas = 0.76- 0.83) and validity as a screener of potential substance use problems. Lastly, the Community Integration Scale is an 11-item Likert measure made up of two subscales. The physical integration subscale assesses participation in a variety of activities (e.g., attend community event, recreational activity, library, volunteer activity); the psychological subscale measures one’s feeling of social connection and belonging in the community (Goering et al., 2011). Alphas ranged from 0.66–0.80. Further, participants were asked how long they have been a Clubhouse member (rated on a 6-point Likert scale from 1 (less than 1 year) to 6 (more than 10 years), and how often they used the Clubhouse in the past three months (Everyday, A couple of times a week, Once a week, Once every couple of weeks, Only for special events, Have not attended in person or virtually in the past three months). Of note, this scale is reversed scored with everyday scored as 1 and none scored as 6.
Procedure
The present study used a participatory approach involving relationship building between the researchers and Clubhouses over the past decade (Rouse et al., 2017). The research partnership between a Clubhouse and researchers at a university in the same city resulted in several participatory research projects, including the development of a program theory (Mutschler et al., 2018). Through this partnership, relationships were also built with Clubhouses across Canada. The study received ethics approval from Toronto Metropolitan University (formerly Ryerson University), Nova Scotia Health Authority, and the Health Research Ethics Board of Alberta.
The lead researcher traveled to all Clubhouses and provided workshops to a local research team made up of directors, staff, and members about the study and how to recruit, consent, and administer the survey. The investigators created a training manual and survey guide for all Clubhouses to troubleshoot difficulties in the research process. The guide contained information on how to administer the survey to participants, including how to discuss consent, definitions for difficult words in the questions, and a list of frequently asked questions and answers. The training occurred over one full day at the Clubhouse sites.
Data Collection
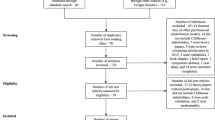
During a 1-month period, the research team at each Clubhouse site engaged members in the survey. The inclusion criterion for the study was that members must have utilized the Clubhouse within the last 90 days. Members who were unable to consent to the study (i.e., were not able to understand the purpose or tasks involved in the study) were excluded. The research team completed the consent process with interested members and assisted them in completing the 1-h questionnaire, if required. Members completed the survey every six months between March 2019 and April 2021 for a total of 5 assessment intervals.
The 1-year data point was collected in March 2020, and subsequent datapoints occurred while lockdowns and social distancing were occurring in Canada. If Clubhouses were physically closed, members completed the surveys over the phone with staff or were mailed the survey. Completion rates across the five timepoints were as follows: baseline n = 459; 6-month n = 381; 12-month n = 274; 18-month n = 306; 24-month n = 304. Drop out from the study was defined as three datapoints that were not completed. A total of 92 Clubhouse members in the present study were missing three or more datapoints. Primary reasons for dropout were no longer a member, unable to be reached by staff, or no longer interested in participating.
Statistical Analyses
Analyses were conducted in SPSS version 28 (IBM, 2021). Changes in the outcomes of interest (i.e., substance use, mental health, life satisfaction, and community integration) were examined using multilevel growth models. Multilevel models account for dependency in repeated measures and have the ability to use all available data making them robust to datasets with missing data due to attrition. For each model, participant age and length of time as a Clubhouse member were included as covariates to control for potential between person differences in outcomes across these variables. Frequency of Clubhouse use in the three months prior to each assessment wave was also included as a time varying covariate to account for within person differences in Clubhouse use. Time was coded categorically with five time points (i.e., baseline, six months, 12 months, 18 months, 24 months). Standardized Cohen’s d effect size estimates were calculated for each outcome using the procedure outlined by Feingold (2009) in which the model-estimated change accounting for significant covariates from baseline to the final assessment (i.e., the 24-month assessment) is divided by the baseline standard deviation of each outcome variable (Feingold, 2009). All models were estimated using the maximum likelihood estimator and included random intercepts and slopes. The present study contained up to 40% missing data at any one time point which is below the recommended limit of 50% missing data for maximum likelihood to produce unbiased estimates shown in simulation studies (Schlomer et al., 2010).
Results
Descriptive statistics of the primary outcomes at each time point and effect size estimates of change in the outcomes from baseline to the 24-month assessment can be found in Table 3. These are further described below.
Life Satisfaction
Using the SWLS and controlling for length of Clubhouse membership and frequency of Clubhouse use, life satisfaction significantly increased over the study period (b = 0.30, p = 0.028, d = 0.24). Longer length of Clubhouse membership predicted greater life satisfaction (b = 0.30, p = 0.003) and greater frequency of Clubhouse use at each assessment interval predicted greater life satisfaction (b = -0.53, p < 0.001).
Mental Health Symptoms
Using the MCSI and controlling for length of Clubhouse membership and frequency of Clubhouse use, mental health symptoms significantly decreased over the study period (b = -79, p < 0.001, d = 0.50). Longer length of Clubhouse membership significantly predicted fewer mental health symptoms over the study period (b = -0.62, p < 0.001), whereas frequency of Clubhouse use at each assessment interval did not predict mental health symptoms (b = 0.30, p = 0.122).
Substance Use
Using the GAIN-SS and controlling for length of Clubhouse membership and frequency of Clubhouse use, substance use significantly decreased over the study period (b = -0.27, p < 0.001, d = 0.26). Longer length of Clubhouse membership predicted lower substance use (b = -0.26, p < 0.001) and greater frequency of Clubhouse use at each assessment interval predicted lower substance use (b = 0.23, p = 0.001).
Community Integration
Physical Integration
Using the CIS and controlling for length of Clubhouse membership and frequency of Clubhouse use, physical integration significantly decreased over the study period (b = -0.43, p < 0.001, d = 1.29). Length of Clubhouse membership did not predict physical integration over the study period (b = 0.03, p = 0.192), but greater frequency of Clubhouse use at each assessment interval predicted greater physical integration (b = -0.23, p < 0.001).
Psychological Integration
Using the CIS and controlling for length of Clubhouse membership and frequency of Clubhouse use, psychological integration significantly increased over the study period (b = 0.16, p = 0.017, d = 0.17). Neither length of Clubhouse membership (b = 0.04, p = 0.446) nor frequency of Clubhouse use at each assessment (b = 0.00, p = 0.952) predicted psychological integration over the study period.
Discussion
To date, there has never been a multi-site, longitudinal study of Clubhouse members from accredited Clubhouses. The purpose of the present study was to longitudinally assess the psychosocial outcomes of Canadian Clubhouse members. A secondary aim was to explore the trajectories of outcomes pre- and during the COVID-19 pandemic. The results indicated that satisfaction with life and psychological integration increased over the study period, while mental health symptoms, substance use, and physical integration decreased. Examining Clubhouse participation, length of Clubhouse membership and frequency of Clubhouse use predicted higher life satisfaction, lower substance use, and fewer mental health symptoms over the study period. Clubhouse participation had mixed effects for community integration subscales. The results of the present study provide invaluable insight into the psychosocial impact of Clubhouses on Canadian Clubhouse members, particularly during COVID-19.
The COVID-19 pandemic had a significant impact on the mental health of Canadians. There was an overall increase in reported mental health symptoms as well as service needs in the general population (Martin & Cooper, 2020). However, the present study found that mental health symptoms, substance use, and overall satisfaction with life improved. The longer and more frequently members attended the Clubhouse, the more positive outcomes they experienced. It is possible that having the familiarity of the Clubhouse as a source of support prior to the pandemic, provided a buffering effect for the negative outcomes that were seen more generally in the population throughout the pandemic. These results are similar to those found in other studies during this time period, which indicated that members who were more engaged reported higher wellness rankings than those who attended less frequently (Hinchey et al., 2022). Virtual Clubhouse attendance during the pandemic was also associated with well-being outcomes (Michon et al., 2021). Another study indicated that during the pandemic, many health and social services closed altogether, leaving Clubhouse members with a lack of support. Clubhouses were able to pivot their services in order to meet the increased needs of Clubhouse members during this time (Mutschler et al., 2021). These results, in addition to those in the present study, suggest that Clubhouses had a significant role in supporting individuals with severe mental illness during the pandemic.
A particularly interesting finding from the present study is the community integration outcomes. Physical integration (e.g., going to events/activities in the community) significantly decreased over the study period. As expected, more Clubhouse engagement predicted higher physical integration. The significant decrease in physical integration aligns with the overall policy mandates in Canada during this time, which resulted in a decrease in in-person events available. Despite the decrease in activities in the community that one could attend, the present study found that psychological integration (e.g., felt sense of community/belonging) increased over the study period. Previous studies have documented the ways in which Clubhouses adapted their programming to meet the needs of their members during the pandemic (Michon et al., 2021; Hinchey et al., 2022). In Canada, Clubhouses increased communication with members (i.e., phone and video calls), expanding their meal programs, and delivering virtual programming through technology (Mutschler et al., 2021). One explanation for the increase in psychological integration, despite the decrease in physical integration, is the program adaptations put into place by the Clubhouses, which ultimately buffered negative psychosocial outcomes for members. The results of the present study highlight the importance of offering virtual programming options for members, which could allow for those who are unwell, live in rural areas, or are otherwise unable to attend in person the ability to connect with the Clubhouse community in a meaningful way. The results suggest that even during the pandemic, individuals can maintain their psychological integration in the midst of physical separation.
Limitations and Future Directions
The present study has numerous strengths, including the use of a multi-site, longitudinal design. The study used a participatory approach that involved collaboration with Clubhouse staff and members to design and implement the present study, thus aligning with the Clubhouse standards and values. Despite the numerous strengths, limitations exist. First, the impact of COVID-19 on the present study is significant, in that there was a decrease in participation rates across the study timepoints. The number of members across the data points was still large, providing significant power in the analyses. It is possible that those who completed the survey at various time points were at a different functioning level than those who did not participate. Further, the adaptations of the Clubhouse due to the pandemic may have impacted results of the study. Future research is needed to examine the trajectories of Clubhouse members who use both virtual and in person Clubhouse services. The sample chosen for the present study were members who had used the Clubhouse in the past three months. This group of members had high frequency of participation pre-pandemic, which could suggest they were highly satisfied with Clubhouse services. Understanding the outcomes of those who use the Clubhouse less frequently or who disengage from services may provide integral information on how Clubhouses can best meet the needs of their members.
Conclusion
The present study examined the psychosocial outcomes of members of six accredited Canadian Clubhouses over 24 months. The study adds to the growing evidence base of Clubhouses around the world, as well as the impact of COVID-19 on Clubhouse members. The results suggest that Clubhouses may have buffered the psychosocial impact of the pandemic. Mental health symptoms and substance use decreased, while psychological integration and satisfaction with life increased. The study provides evidence on how virtual services can provide positive outcomes for Clubhouse members who are unable to attend in person. Future research is needed to further understand the impact of the pandemic on those who may have used the Clubhouse less frequently, and the differences between those who use virtual versus in-person services.
References
Bouvet, C., Battin, C., Cappelaere, C., et al. (2021). Psychosocial Change in Members of Clubhouse Paris (France) Over an 18-Month Period: A Longitudinal Mixed Methods Study. Community Mental Health Journal, 57, 853–863. https://doi.org/10.1007/s10597-020-00654-z
Chen, Y., Yau, E., Lam, C., Deng, H., Weng, Y., Liu, T., & Mo, X. (2020). A 6-month randomized controlled pilot study on the effects of the clubhouse model of psychosocial rehabilitation with Chinese individuals with schizophrenia. Administration and Policy in Mental Health and Mental Health Services Research, 47, 107–114.
Conrad, K. J., Yagelka, J. R., Matters, M. D., Rich, A. R., Williams, V., & Buchanan, M. (2001). Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Mental Health Services Research, 3, 141–153.
Dennis, M. L., Chan, Y. F., & Funk, R. R. (2006). Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. The American Journal on Addictions, 15, s80–s91.
Desai, M. U., Manning, R., III., Pavlo, A. J., Blackman, K., Ocasio, L., Crespo, M., & Flanagan, E. (2021). An “oasis within a desert”, but the desert remains: Clubhouse members’ experiences of social belonging and societal oppression. American Journal of Orthopsychiatry, 91(2), 294.
Diener, E. D., Emmons, R. A., Larsen, R. J., & Griffin, S. (1985). The satisfaction with life scale. Journal of Personality Assessment, 49(1), 71–75.
Feingold, A. (2009). Effect sizes for growth-modeling analysis for controlledclinical trials in the same metric as for classical analysis. Psychological Methods, 14(1), 43–53. https://doi.org/10.1037/a0014699
Goering, P. N., Streiner, D. L., Adair, C., et al. (2011). The At Home/Chez Soi trial protocol: A pragmatic, multi-site, randomised controlled trial of a Housing First intervention for homeless individuals with mental illness in five Canadian cities. British Medical Journal Open, 1, e000323. https://doi.org/10.1136/bmjopen-2011-000323
Hinchey, L., Michon, A., Drews, J., et al. (2022). Clubhouses as essential communities during the COVID-19 pandemic. Journal of Psychosocial Rehabilitation and Mental Health, 9, 149–15. https://doi.org/10.1007/s40737-021-00242-8
IBM Corporation. (2021). IBM SPSS statistics for Windows (Version 28.0).
Junaid, S., Mutschler, C., McShane, K., Canadian Clubhouse Research Group. (2023). The Impact of COVID-19 on Clubhouse Employment Programs. Community Mental Health Journal, 59(3), 523–530.
Martin, L., & Cooper, M. (2020). Mental health during COVID-19 outbreak wave 1. Mental Health Research Canada & Pollara strategic insights. Retrieved July 30, 2020, from https://www.mhrc.ca/wp-content/uploads/2020/05/Full-Report-of-Findings-of-Survey-FINAL.pdf
McKay, C., Nugent, K. L., Johnsen, M., Eaton, W. W., & Lidz, C. W. (2018). A systematic review of evidence for the clubhouse model of psychosocial rehabilitation. Administration and Policy in Mental Health and Mental Health Services Research, 45, 28–47.
Mental Health Commission of Canada. (2015). Recovery guidelines Ottawa, ON: Author. ©2015 Mental Health Commission of Canada
Michon, A., Hinchey, L., Pernice, F., Drews, J., Price, M., Christian, J., ... & Kellogg, L. (2021). Responding to the global pandemic: a pulse of the well-being of clubhouse communities moving virtual. Journal of Psychosocial Rehabilitation and Mental Health, 8(2), 171–183.
Mutschler, C., Rouse, J., McShane, K., & Habal-Brosek, C. (2018). Developing a realist theory of psychosocial rehabilitation: The Clubhouse model. BMC Health Services Research, 18(1), 1–12.
Mutschler, C., Junaid, S., McShane, K., Canadian Clubhouse Research Group. (2021). Clubhouses response to Covid-19: Member challenges and clubhouse adaptations. Community Mental Health Journal, 57, 424–437.
Mutschler, C., McShane, K., Liebman, R., Junaid, S., & The Canadian Clubhouse Research Group. (2023). A multisite longitudinal evaluation of canadian clubhouse members: Impact on hospitalizations and community functioning. Psychiatric Rehabilitation Journal. Advance online publication. https://doi.org/10.1037/prj0000581
Pernice, F. M., Price, M. H., & Rice, K. (2021). Why we come: Clubhouse members seek connection, purpose and meaning. Community Mental Health Journal, 57, 446–456.
Reidel, K., Abriel, S., Tavares, R., Roark, M., McLellan, R., & Kehayia, E. (2021). Transitional employment programs within clubhouses as a means of promoting recovery for individuals living with mental illness: Reviewing the case for Québec. Canadian Journal of Community Mental Health, 40(1), 1–34.
Rouse, J., Mutschler, C., McShane, K., & Habal-Brosek, C. (2017). Qualitative participatory evaluation of a psychosocial rehabilitation program for individuals with severe mental illness. International Journal of Mental Health, 46(2), 139–156.
Russell, M. J., Lifeso, N., Fazio, J., Piatt, C., Kelton, F., Cui, X., & Nwachukwu, I. (2022). Clubhouse Model and its impact on psychiatric hospitalization in Canada: A cohort study. Canadian Journal of Community Mental Health, 40(3), 29–44.
Schlomer, G. L., Bauman, S., & Card, N. A. (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. https://doi.org/10.1037/a0018082
Sukut, O., & Ayhan Balik, C. H. (2021). The impact of COVID-19 pandemic on people with severe mental illness. Perspectives in Psychiatric Care, 57(2), 953–956.
Tanaka, K., Stein, E., Craig, T. J., Kinn, L. G., & Williams, J. (2021). Conceptualizing participation in the community mental health context: Beginning with the Clubhouse model. International Journal of Qualitative Studies on Health and Well-Being, 16(1), 1950890.
Vescey, L., Yoon, J., Rice, K., Davidson, L., & Desai, M. (2023). A return to lived experiencers themselves: Participatory action research of and by psychosocial clubhouse members. Frontiers in Psychology, 13, 962137.
Wang, J., Lloyd-Evans, B., Giacco, D., Forsyth, R., Nebo, C., Mann, F., & Johnson, S. (2017). Social isolation in mental health: A conceptual and methodological review. Social Psychiatry and Psychiatric Epidemiology, 52(12), 1451–1461. https://doi.org/10.1007/s00127-017-1446-1
Funding
The study was funded by a Mitacs Accelerate Grant.
Author information
Authors and Affiliations
Consortia
Contributions
Christina Mutschler and Kelly McShane contributed to the study conception and design. Material preparation, data collection and analysis were performed by Christina Mutschler, Rachel Liebman, and the Canadian Clubhouse Research Group. The first draft of the manuscript was written by Christina Mutschler and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study received ethics approval from Toronto Metropolitan University (formerly Ryerson University), Nova Scotia Health Authority, and the Health Research Ethics Board of Alberta.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Competing Interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Canadian Clubhouse Research Group contains all directors, staff, and members from the following Clubhouses: Crossroads, Fitzroy Centre, Notre Dame Place, Oak Centre, Potential Place, and Progress Place.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mutschler, C., McShane, K., Liebman, R. et al. Psychosocial Outcomes of Canadian Clubhouse Members: A Multi-Site Longitudinal Evaluation. Community Ment Health J (2024). https://doi.org/10.1007/s10597-024-01280-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10597-024-01280-9