Abstract
Nonadherence to antidepressants is widespread and poses a significant barrier to optimal management and treatment of depression in community settings. The objective of this study was to compare self-reported and electronic monitoring of adherence to antidepressants and to examine the relationship of these measures with depressive symptoms in a medically underserved community. Adherence to antidepressants was measured in 38 primary care patients from the West Philadelphia area using self-report and electronic monitoring (Medication Event Monitoring System caps). Self-report and electronic monitoring of antidepressant adherence showed fair agreement at baseline, slight agreement at 6 weeks, and slight agreement at 12 weeks. Adherence to antidepressants as assessed by electronic monitors was significantly associated with depression remission at 12 weeks [adjusted odds ratio 18.6, 95% confidence interval (1.05, 330.56)]. Compared with electronic monitoring, self-reported adherence tended to overestimate medication adherence to antidepressants. Adherence assessed by electronic monitoring was associated with depression remission.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite evidence supporting the effectiveness of pharmacotherapy in reducing depressive symptoms nonadherence to antidepressant medications is widespread. Research indicates that nearly half of patients taking antidepressants do not meet adherence thresholds for optimal clinical benefits (Olfson et al. 2006; Sansone and Sansone 2012). Nonadherence to antidepressant medications poses a significant barrier to optimal management and treatment for depression in community settings, especially among patients with comorbid chronic diseases such as diabetes (Bauer et al. 2014; Cipriani et al. 2018). Social determinants of health have also been identified as critical indicators of self-care and mental health outcomes in community and other settings (Alegria et al. 2018). Persons that lack basic goods necessary to promote health and treat disease (e.g. medications, housing, and transportation) are at increased risk for noncompliance and adverse health outcomes (Kahn et al. 2000; Yoshikawa et al. 2012). Structural and functional social support as well as psychological indicators (e.g. self-efficacy and empowerment) are critical predictors of patient engagement and compliance with medical regimens including depression and diabetes care (Kleinberg et al. 2013; Salazar-Fraile et al. 2018; Voils et al. 2005).
Reliable measures of adherence are essential for improving depression outcomes as they provide the foundation for care management, research and other applications. In order to achieve clinical treatment goals, accurate adherence assessment allows for prescribing decisions that most effectively promote patient health. Furthermore, research relies on adherence data to examine drug effectiveness for clinical outcomes. Self-reported adherence assessment is the most commonly used approach because of low cost and easy implementation in a variety of settings (Garfield et al. 2011). However, the validity of self-reports has been found to be poor as bias, namely social desirability and recall, result in overestimates of adherence (Garber et al. 2004; Nguyen et al. 2014). Electronic monitoring of adherence records the exact date and time the bottle is opened and allows researchers to document patterns of adherence. This approach has been found to provide the most valid and reliable adherence data when compared to other adherence measures (Osterberg 2005).
We sought to compare self-reported adherence and electronic monitoring of adherence with antidepressants in a sample of patients with depression and diabetes as well as financial, social and emotional needs residing in West Philadelphia, a designated medically underserved community. Previous investigations have primarily compared self-reported adherence and electronic monitoring of adherence to antidepressants in samples of persons with Major Depressive Disorder in which recruitment was limited to mental health specialty settings (e.g. mental health clinic or psychiatry department) (Bosman et al. 2014; Interian 2010; Lee et al. 2010; Nakonezny et al. 2010). Our goal was to provide critical inferences for enhanced care provision for disadvantaged populations. No known studies have been conducted specifically within designated medically underserved communities. Furthermore, few studies have evaluated the relationship between various adherence measures and depression outcomes (Bosman et al. 2014; Interian 2010). This study examined the measurement of adherence using both self-reported adherence and electronic monitoring of adherence in relation to depression outcomes among patients with diabetes as well as financial, social, and emotional needs and a range of depressive symptoms, recruited from primary care practices in West Philadelphia. West Philadelphia has been designated as a Health Resources and Service Administration (HRSA) Medically Underserved Area and is a HRSA-designated Low Income Primary Care Health Professions Shortage Area. The residents of West Philadelphia experience higher rates of chronic disease than adults in other geographic areas and have drawn national attention for their increased need for enhanced care provision.
The objective of our study was to compare self-reported adherence and electronic monitoring of adherence to antidepressants over 12 weeks and to examine the relationship of these two measures with depressive symptoms in a medically underserved community. To accomplish these goals, we employed data from the randomized trial of an integrated intervention for Type 2 diabetes mellitus (T2DM) and depression that addressed patients’ financial, social, and emotional needs versus an integrated intervention alone. We hypothesized that: (1) self-reported adherence would overestimate adherence compared with electronic monitoring of adherence for antidepressants and (2) patients with ≥ 80% adherence to an antidepressant medication measured using electronic monitoring would be more likely to achieve remission of their depression (9-item Patient Health Questionnaire < 5) at 12 weeks compared with patients who did not achieve ≥ 80% adherence at 12 weeks.
The study protocol was approved by the University of Pennsylvania, Perelman School of Medicine Institutional Review Board.
Methods
Recruitment Procedures
Recruitment for this study was conducted in three primary care practices in West Philadelphia, Pennsylvania between 2013 and 2015. Electronic medical records were used to ascertain patients with a diagnosis of type 2 diabetes mellitus (T2DM) and a prescription for an oral hypoglycemic agent within the last year. From the identified patients, persons with an upcoming appointment were approached for inclusion/exclusion criteria screening. To be included in the study participants needed to be 30 years and older and have a diagnosis of T2DM. Research studies exclude a majority of potential participants limiting widespread inference in real world contexts. Our aim was to include patients with a range of depressive symptoms consistent with the relapsing and remitting progression of depression in community settings (Angst 1988). Exclusion criteria were: inability to provide informed consent; significant cognitive impairments at baseline (Mini-Mental State Examination [MMSE] (Crum et al. 1993) < 21); patients who resided in a care facility that administered medications on a set schedule; and patients who were unwilling or unable to use the Medication Event Monitoring System (MEMS). Additional study details are provided in prior work (de Vries McClintock et al. 2016).
Measurement Strategy
We obtained sample characteristics from patients using standard questions on patients’ baseline age, self-reported ethnicity, gender, marital status, and education. The medical Outcomes Study Short Form (SF-36) was utilized to measure patient’s functional status (Stewart et al. 1988). Medication bottles were used to record the names, doses, and frequencies of medications prescribed. Patients were asked if they were given oral instructions to change the dose or frequency of the medications they were taking and the patient’s self-report was recorded. Medical comorbidity was assessed via self-report at baseline. Cognitive status was evaluated using a mental status examination by the total score on the MMSE at baseline. The MMSE has been extensively employed for clinical and research purposes (McHorney 1996; Stadnyk et al. 1998; Stewart 1992; Stewart et al. 1988, 1989; Wells et al. 1989). Financial, social and emotional needs were assessed by asking patients about needs that they “really wanted help with” or “were really important to them.” The unmet needs assessed were not having enough money to cover expenses, pain, worry about safety, ability to exercise, feeling depressed or anxious, trouble getting transportation, alcohol, street drugs or taking more medication than prescribed, memory or solving problems, law/legal concerns, reading a newspaper or computer screen, eating a diabetic diet, taking blood sugar and knowing what to do with the results, feeling alone, concern about children, guidance on medication usage, relationships with family/others, having no one to help, needing a new place to live, physical illness, unable to lose weight, thoughts of death or suicide, difficulty getting medications, difficulty with dressing or bathing and not having enough time to take care of myself. Participants were considered to have an unmet financial, social, or emotional need if they assessed the unmet need as something that they “really needed help with” or indicated “was very important to them.”
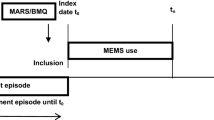
Adherence
Adherence to antidepressants was measured using both self-reports and electronic monitoring during a 2-week run in phase as well as at 6 and 12 weeks. The Brief Medication Questionnaire 5-item Regimen Screen was used to measure self-reported adherence. Consistent with prior work, those who took at least 80% of their medication were considered adherent (George et al. 2000). MEMS was used for electronic monitoring of adherence as they record the precise date and time of container opening. MEMS adherence was measured by comparing the proportion of vial openings in relation to the prescribed doses for the past week. Self-reported adherence was assessed at the end of the 2-week follow-up, 6, and 12 weeks by asking patients about adherence in the prior week in order to minimize recall bias and elicit more accurate responses, similar to previous research (Hashmi et al. 2007; Heckman et al. 2004; Odegard and Gray 2008; Rickles and Svarstad 2007). To avoid potential bias, patients were blinded to which week of participation was being employed for analysis.
Depression
The 9-item Patient Health Questionnaire (PHQ-9) was employed to measure depressive symptoms at baseline and 12 weeks. The PHQ-9 was created as a self-administered version of the PRIME-MD diagnostic instrument for mental disorders. The PHQ-9 has been found to be a reliable tool for screening and monitoring of depression in primary care settings (Kroenke et al. 2001). It scores the 9 DSM-V criteria for depression on a scale of “0” (not at all) to “3” (nearly every day).
Analytic Strategy
Adherence was measured by dividing the number of doses taken by the number of doses prescribed over the past week. That quotient was then multiplied by 100 to obtain an adherence percentage. The proportion of prescribed doses taken was highly skewed and did not meet normality assumptions, and thus adherence was dichotomized at a threshold of 80%. The 80% threshold was used because it is both conservative in measuring nonadherence and it is consistent with prior investigations on mental health (Lee et al. 2010; Thompson et al. 2000).
Our analysis was conducted in two phases. During phase one, a kappa coefficient was used to determine the level of agreement between self-reported adherence and electronic monitoring at the dichotomized threshold of 80%. The kappa coefficient was employed because it provides the chance corrected agreement between the self-report and electronic monitoring adherence methods. During the second phase, our goal was to study the relationship of > 80% medication adherence, using both methods, in relation to depression remission (PHQ-9 score of < 5 at follow-up (Kroenke et al. 2001). Logistic regression was used to assess the relationship between depression remission and adherence to antidepressants. Both the odds ratios and the 95% confidence intervals were reported. In order to account for potentially influential variables, the final multivariate logistic regression model was adjusted for age, ethnicity, gender, marital status, educational attainment, functional status, frequency of medication administration, number of medications, number of medical conditions, cognitive status, intervention condition, and baseline depressive symptoms. STATA version 14 (College Station, Texas, USA) was used for the analyses.
Results
Sample Characteristics
Baseline characteristics for the study sample are shown in Table 1. A total of 38 participants were included in the study with a mean age of 62.61 years (standard deviation, s.d. = 10.88). A majority of the participants were women (81.58%). Participants were primarily identified as African American (68.42%) and other reported ethnicities included White (23.68%), and Hispanic (7.90%). The mean number of medications taken was 10.55 (s.d. = 3.85). In total, 36 participants took their antidepressant once per day (94.74%) and 2 participants took it twice per day (5.26%). The mean 9-item Patient Health Questionnaire (PHQ-9) score was 7.61 (s.d. = 5.02). Half of the participants were allocated to the intervention group (50%). Participants indicated that they had one unmet financial, social, and emotional need (10.53%), 2–3 unmet needs (21.05%), 4–5 unmet needs (15.79%), or 6 or more unmet needs (52.63%) that they “really wanted helped with” or “were very important to them.”
Adherence
Table 2 depicts the kappa coefficient results for the proportion of participants who were ≥ 80% adherent to their antidepressant medications. At baseline, ≥ 80% adherence rates for antidepressants measured by electronic monitoring and self-report were 52.6% (n = 20) and 89.5% (n = 34), respectively. The ≥ 80% adherence rates at 6 weeks were 47.4% (n = 18) for electronic monitoring adherence and 86.8% (n = 33) for self-reported adherence. At 12 weeks, ≥ 80% adherence rates for electronic monitoring adherence and self-reported adherence were 47.4% (n = 18) and 92.1% (n = 35), respectively. At baseline, electronic monitoring and self-reported adherence showed fair agreement (kappa = 0.231, P < 0.05). At 6 weeks and 12 weeks, electronic monitoring and self-reported adherence showed slight agreement (kappa = 0.139, P = 0.094; kappa = 0.170, P < 0.05, respectively).
Clinical Outcome
The relationship between > 80% adherence for antidepressants, measured via self-reported and electronic monitoring adherence, and depression at 12 weeks can be found in Table 3. Participants who achieved > 80% adherence to antidepressant medications measured with electronic monitoring were more likely to achieve remission of depression in comparison with patients who did not achieve > 80% adherence at 12 weeks [PHQ-9 < 5, unadjusted OR 5.25, 95% CI (1.26, 21.86)]. This relationship remained significant after adjusting for age, ethnicity, gender, marital status, educational attainment, functional status, lives alone, frequency of antidepressant administration, cognitive status, intervention condition, and baseline depression [PHQ-9 < 5, adjusted OR 18.61, 95% CI (1.05, 330.56)].
Discussion
Our principal finding is that among patients with diabetes, depression as well as unmet financial, social, and emotional needs, self-reported adherence in comparison with electronic monitoring overestimates antidepressant adherence in a medically underserved community. In addition, the patients who were adherent to antidepressants, assessed using electronic monitoring, were more likely to have remitted depression at the final study visit. The findings provide insight into measurement of antidepressant adherence informing research initiatives and clinical care provision in underserved communities.
Prior to discussing our findings, potential limitations are important to address. First, our sample was recruited from three primary care practices in which patient characteristics may differ from other community settings. However, these practices serve diverse patient populations and are probably similar to other primary care practices in the geographic area. Second, healthy adherer bias in which patients who achieved depression remission may have engaged in additional health promoting behaviors may have influenced these findings. We did not collect data on additional lifestyle behaviors such as smoking. Third, our standard for comparison was electronic monitoring using MEMS Caps which have the potential to overestimate adherence because events are recorded by bottle top removal which does not guarantee medication ingestion. However, electronic monitoring has a low failure rate and may be more sensitive than other adherence measures (Farmer 1999; George et al. 2000). Fourth, the 80% threshold for medication adherence has been examined for some medications and not others. However, in this study the 80% threshold has been assessed for the majority of the medications taken (Choudhry et al. 2009; George et al. 2000; Lee et al. 2010). Fifth, the Hawthorne effect, in which patients more likely to adhere to their medical regimens because they are participating in a study, may influence adherence (Campbell et al. 1995). However, nonadherence is still common when patients are followed in study settings (Croghan et al. 1997; Melfi et al. 1998; Tedlow et al. 1996). Sixth, the small sample size of this study limits the generalizability of findings beyond the sample that was drawn. It is notable that significant associations were found despite the small sample size and further research is needed to validate these findings in larger samples. Despite these limitations our results deserve attention because this is the first known study to compare self-reported and electronic monitoring of adherence for antidepressants in a sample of patients with unmet financial, social, and emotional needs in a community setting. An evaluation of antidepressant adherence among persons with economic and socio-cultural barriers is critical for the management and treatment of depression in this population.
We found that patients consistently overestimated self-reported antidepressant adherence in comparison with electronic monitoring. Our findings are aligned with prior studies reporting that self-report measures of antidepressants indicate higher adherence rates than electronic measures (Garber et al. 2004; Nguyen et al. 2014). Past literature has attributed overestimation of medication to many reasons including patient-provider interactional dynamics, poor understanding of prescribed regimens, cognitive impairment, biases and research settings/measures (Brown and Bussell 2011; Shi et al. 2010). The reasons for overestimation by self-report in this work may be due to inaccurate recall. Previous research found that patients believe they took medication while accidently missing pill taking because of poor memory, multiple medical conditions including diabetes, and study setting (Neath 1993). Other contributing factors may have included social desirability in which persons feel compelled to respond in ways that are consistent with social norms (Marlowe and Crowne 1961). This bias has been identified in prior work as largely contributing to over reporting of medication adherence (Stone et al. 2000). Of note, the mean number of medications taken per participants in this sample was approximately ten. The number of medications taken has been found to influence adherence in numerous studies. While studies have reported conflicting findings, increased numbers of medications taken have been associated with poor adherence as measured by both self-reports and electronic monitoring (Abada et al. 2019; Claxton et al. 2001). Our findings build on prior work by evaluating the relationship between self-report, electronic monitoring adherence, and depressive symptoms in a sample taking many medications in underserved communities.
We found that patients who were adherent to antidepressants measured using electronic monitoring had significantly improved depressive symptoms compared to patients who were nonadherent. Our results are primarily consistent with prior work reporting that an association between greater electronic monitoring adherence and improved depression in community settings exists (Lee et al. 2010). Some previous investigations have indicated that despite maintenance of adherence thresholds measured by electronic monitoring improved depression may not be achieved. However, these findings are limited by small sample sizes, study design, and varied outcome assessment suggesting that more robust investigations may yield more meaningful results (Barbui et al. 2011; Rapaport and Judd 1998; Stewart et al. 1992). Prior work indicates that technological applications may provide a cost-effective solution to improve knowledge, behaviors and/or outcomes (Iribarren et al. 2017). Further research is needed to evaluate the cost effectiveness of different technological approaches including MEMS caps for improving medication adherence and clinical indicators in real world settings.
In March 2016 the Institute of Medicine released a report focused on addressing social determinants of health. Social determinants are defined as those conditions in which people are born, grow, live, work and age (World Health Organization 2019). This report emphasized a need for research and clinical initiatives that encompass and address social determinants of health (Medicine, National Academies of Sciences, & Medicine 2016). Among the most influential are those determinants that are financial, social, and emotional in nature. For instance, persons that lack social support and/or basic material goods such as transportation and housing are at increased risk for nonadherence and poor clinical outcomes (Kahn et al. 2000; Kleinberg et al. 2013; Salazar-Fraile et al. 2018; Voils et al. 2005; Yoshikawa et al. 2012). The report calls for a focus that incorporates care in which effective services and care management can be provided in the context of persons experiencing a range of socioeconomic determinants that influence self-care and adherence to medical regimens. In this work we examined measures for antidepressant medication adherence among persons with unmet financial, social, and emotional needs who resided in West Philadelphia. West Philadelphia has been designated as a medically underserved community and adults in West Philadelphia bear a proportionally higher chronic disease burden than their counterparts in other geographic areas, thus the need is great for enhanced access and quality of primary and mental health care. Our findings have implications for healthcare providers and public health initiatives working with underserved communities and can help shape effective care, outreach and research in vulnerable populations.
Effective treatment of depression is highly dependent on adherence to medication regimens. Poor medication adherence has been shown to be a major barrier for patients seeking to reduce their depressive symptoms, particularly in underserved communities. Therefore, it is important that regular monitoring and discussion about medication adherence occurs during clinical encounters. Our data suggests that over time self-reported adherence continued to overestimate adherence in comparison with electronic monitoring. Self-report measures should be used with caution since reliability and accuracy may not be certain. Physicians who suspect nonadherence should examine factors that contribute to nonadherence and address them in order to minimize the potential for poor health prognoses and adverse clinical outcomes. Improved management and adherence to antidepressants could have a beneficial public health impact on patient clinical outcomes, leading to improved health status in underserved communities.
References
Abada, S., Clark, L. E., Sinha, A. K., Xia, R., Pace-Murphy, K., Flores, R. J., et al. (2019). Medication regimen complexity and low adherence in older community-dwelling adults with substantiated self-neglect. Journal of Applied Gerontology,38(6), 866–883.
Alegria, M., NeMoyer, A., Falgas Bague, I., Wang, Y., & Alvarez, K. (2018). Social determinants of mental health: Where we are and where we need to go. Current Psychiatry Reports,20(11), 95. https://doi.org/10.1007/s11920-018-0969-9.
Angst, J. (1988). Clinical course of affective disorders. Depressive Illness. https://doi.org/10.1007/978-3-642-73546-2_1.
Barbui, C., Cipriani, A., Patel, V., Ayuso-Mateos, J. L., & van Ommeren, M. (2011). Efficacy of antidepressants and benzodiazepines in minor depression: Systematic review and meta-analysis. The British Journal of Psychiatry,198(1), 11–16. https://doi.org/10.1192/bjp.bp.109.076448.
Bauer, A., Parker, M., Schillinger, D., Katon, W., Adler, N., Adams, A., et al. (2014). Associations between antidepressant adherence and shared decision-making, patient-provider trust, and communication among adults with diabetes: Diabetes Study of Northern California (DISTANCE). Journal of General Internal Medicine,29(8), 1139–1147.
Bosman, J., Ter Horst, P. G., Smit, J. P., Dijkstra, J. R., Beekhuis, H. R., Slingersland, R. J., et al. (2014). Adherence of antidepressants during pregnancy: MEMS compared with three other methods. Therapeutic Advances in Psychopharmacology,4(2), 61–69. https://doi.org/10.1177/2045125313511486.
Brown, M. T., & Bussell, J. K. (2011). Medication adherence: WHO cares? Mayo Clinic Proceedings,86(4), 304–314. https://doi.org/10.4065/mcp.2010.0575.
Campbell, J. P., Maxey, V. A., & Watson, W. A. (1995). Hawthorne effect: Implications for prehospital research. Annals of Emergency Medicine,26(5), 590–594.
Choudhry, N. K., Shrank, W. H., Levin, R. L., Lee, J. L., Jan, S. A., Brookhart, M. A., et al. (2009). Measuring concurrent adherence to multiple related medications. The American Journal of Managed Care,15(7), 457–464.
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., … Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. Lancet, 391(10128), 1357–1366. doi:10.1016/s0140-6736(17)32802-7.
Claxton, A. J., Cramer, J. B., & Pierce, C. (2001). A systematic review of the associations between dose regimens and medication compliance. Clinical Therapeutics,23(8), 1296–1310.
Croghan, T. W., Lair, T. J., Engelhart, L., Crown, W. E., Copley-Merriman, C., Melfi, C. A., et al. (1997). Effect of antidepressant therapy on health care utilization and costs in primary care. Psychiatric Services (Washington, D. C.),48(11), 1420–1426. https://doi.org/10.1176/ps.48.11.1420.
Crum, R. M., Anthony, J. C., Bassett, S. S., & Folstein, M. F. (1993). Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA,269(18), 2386–2391.
de Vries McClintock, H. F., Boyle, K. B., Rooney, K., & Bogner, H. R. (2016). Diabetes and depression care: A randomized controlled pilot trial. American Journal of Health Behavior,40(4), 503–513. https://doi.org/10.5993/ajhb.40.4.12.
Farmer, K. C. (1999). Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clinical Therapeutics,21(6), 1074–1090. https://doi.org/10.1016/s0149-2918(99)80026-5. (discussion 1073).
Garber, M. C., Nau, D. P., Erickson, S. R., Aikens, J. E., & Lawrence, J. B. (2004). The concordance of self-report with other measures of medication adherence: A summary of the literature. Medical Care,42(7), 649–652.
Garfield, S., Clifford, S., Eliasson, L., Barber, N., & Willson, A. (2011). Suitability of measures of self-reported medication adherence for routine clinical use: A systematic review. BMC Medical Research Methodology,11, 149. https://doi.org/10.1186/1471-2288-11-149.
George, C. F., Peveler, R. C., Heiliger, S., & Thompson, C. (2000). Compliance with tricyclic antidepressants: The value of four different methods of assessment. British Journal of Clinical Pharmacology,50(2), 166–171.
Hashmi, S. K., Afridi, M. B., Abbas, K., Sajwani, R. A., Saleheen, D., Frossard, P. M., …, Ahmad, U. (2007). Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS ONE, 2(3), e280. doi:10.1371/journal.pone.0000280.
Heckman, B. D., Catz, S. L., Heckman, T. G., Miller, J. G., & Kalichman, S. C. (2004). Adherence to antiretroviral therapy in rural persons living with HIV disease in the United States. AIDS Care,16(2), 219–230. https://doi.org/10.1080/09540120410001641066.
Interian, A. (2010). A brief self-report measure to assess antidepressant adherence among Spanish-speaking Latinos. Journal of Clinical Psychopharmacology,30(6), 755–757. https://doi.org/10.1097/JCP.0b013e3181fb57f8.
Iribarren, S. J., Cato, K., Falzon, L., & Stone, P. W. (2017). What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS ONE,12(2), e0170581.
Kahn, R. S., Wise, P. H., Kennedy, B. P., & Kawachi, I. (2000). State income inequality, household income, and maternal mental and physical health: Cross sectional national survey. BMJ,321(7272), 1311–1315. https://doi.org/10.1136/bmj.321.7272.1311.
Kleinberg, A., Aluoja, A., & Vasar, V. (2013). Social support in depression: Structural and functional factors, perceived control and help-seeking. Epidemiology and Psychiatric Sciences,22(4), 345–353. https://doi.org/10.1017/s2045796013000504.
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine,16(9), 606–613.
Lee, M. S., Lee, H. Y., Kang, S. G., Yang, J., Ahn, H., Rhee, M., …, Kim, S. H. (2010). Variables influencing antidepressant medication adherence for treating outpatients with depressive disorders. Journal of Affective Disorders, 123(1–3), 216–221. doi:10.1016/j.jad.2009.10.002.
Marlowe, D., & Crowne, D. P. (1961). Social desirability and response to perceived situational demands. Journal of Consulting Psychology,25, 109–115.
McHorney, C. A. (1996). Measuring and monitoring general health status in elderly persons: Practical and methodological issues in using the SF-36 Health Survey. Gerontologist,36(5), 571–583.
Melfi, C. A., Chawla, A. J., Croghan, T. W., Hanna, M. P., Kennedy, S., & Sredl, K. (1998). The effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depression. Archives of General Psychiatry,55(12), 1128–1132.
Nakonezny, P. A., Hughes, C. W., Mayes, T. L., Sternweis-Yang, K. H., Kennard, B. D., Byerly, M. J., et al. (2010). A comparison of various methods of measuring antidepressant medication adherence among children and adolescents with major depressive disorder in a 12-week open trial of fluoxetine. Journal of Child and Adolescent Psychopharmacology,20(5), 431–439. https://doi.org/10.1089/cap.2009.0108.
National Academies of Sciences, Engineering, and Medicine. (2016). A framework for educating health professionals to address the social determinants of health. Washington, DC: The National Academies Press.
Neath, I. (1993). Distinctiveness and serial position effects in recognition. Memory & Cognition,21(5), 689–698.
Nguyen, T. M., La Caze, A., & Cottrell, N. (2014). What are validated self-report adherence scales really measuring?: A systematic review. British Journal of Clinical Pharmacology,77(3), 427–445. https://doi.org/10.1111/bcp.12194.
Odegard, P. S., & Gray, S. L. (2008). Barriers to medication adherence in poorly controlled diabetes mellitus. The Diabetes Educator,34(4), 692–697. https://doi.org/10.1177/0145721708320558.
Olfson, M., Marcus, S. C., Tedeschi, M., & Wan, G. J. (2006). Continuity of antidepressant treatment for adults with depression in the United States. American Journal of Psychiatry,163(1), 101–108. https://doi.org/10.1176/appi.ajp.163.1.101.
Osterberg, L. B. T. (2005). Adherence to medication. The New England Journal of Medicine,353(5), 487–497. https://doi.org/10.1056/NEJMra050100.
Rapaport, M. H., & Judd, L. L. (1998). Minor depressive disorder and subsyndromal depressive symptoms: Functional impairment and response to treatment. Journal of Affective Disorders,48(2–3), 227–232.
Rickles, N. M., & Svarstad, B. L. (2007). Relationships between multiple self-reported nonadherence measures and pharmacy records. Research in Social and Administrative Pharmacy,3(4), 363–377. https://doi.org/10.1016/j.sapharm.2006.11.001.
Salazar-Fraile, J., Sempere-Verdu, E., Perez-Hoyos, S., Tabares-Seisdedos, R., & Gomez-Beneyto, M. (2018). Five interpersonal factors are predictive of the response to treatment of major depression with antidepressants in primary care. Frontiers in Psychiatry,9, 416. https://doi.org/10.3389/fpsyt.2018.00416.
Sansone, R. A., & Sansone, L. A. (2012). Antidepressant adherence: Are patients taking their medications? Innovations in Clinical Neuroscience,9(5–6), 41–46.
Shi, L., Liu, J., Koleva, Y., Fonseca, V., Kalsekar, A., & Pawaskar, M. (2010). Concordance of adherence measurement using self-reported adherence questionnaires and medication monitoring devices. Pharmacoeconomics,28(12), 1097–1107. https://doi.org/10.2165/11537400-000000000-00000.
Stadnyk, K., Calder, J., & Rockwood, K. (1998). Testing the measurement properties of the Short Form-36 Health Survey in a frail elderly population. Journal of Clinical Epidemiology,51(10), 827–835.
Stewart, A. L. (1992). Measuring functioning and well-being: The medical outcomes study. Durham, NC: Duke University Press.
Stewart, A. L., Greenfield, S., Hays, R. D., Wells, K., Rogers, W. H., Berry, S. D., …,Ware, J. E., Jr. (1989). Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA, 262(7), 907–913.
Stewart, A. L., Hays, R. D., & Ware, J. E., Jr. (1988). The MOS short-form general health survey. Reliability and validity in a patient population. Medical Care,26(7), 724–735.
Stewart, J. W., McGrath, P. J., & Quitkin, F. M. (1992). Can mildly depressed outpatients with atypical depression benefit from antidepressants? American Journal of Psychiatry,149(5), 615–619. https://doi.org/10.1176/ajp.149.5.615.
Stone, A. A., Bachrach, C. A., Jobe, J. B., Kurtzman, H. S., & Cain, V. S. (2000). The scient of self-report: Implications for research and practice (1st ed.). Mahwah, NJ: Lawrence Erlbaum Associates Inc.
Tedlow, J. R., Maurizio, F., Uebelacker, L. A., Alpert, J. E., Nierenberg, A. A., & Rosenbaum, J. F. (1996). Are study dropouts different from completers? Biological Psychiatry,40(7), 668–670. https://doi.org/10.1016/0006-3223(96)00204-1.
Thompson, C., Peveler, R. C., Stephenson, D., & McKendrick, J. (2000). Compliance with antidepressant medication in the treatment of major depressive disorder in primary care: A randomized comparison of fluoxetine and a tricyclic antidepressant. American Journal of Psychiatry,157(3), 338–343. https://doi.org/10.1176/appi.ajp.157.3.338.
Voils, C. I., Steffens, D. C., Flint, E. P., & Bosworth, H. B. (2005). Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. The American Journal of Geriatric Psychiatry,13(2), 157–165. https://doi.org/10.1176/appi.ajgp.13.2.157.
Wells, K. B., Stewart, A., Hays, R. D., Burnam, M. A., Rogers, W., Daniels, M., …, Ware, J. (1989). The functioning and well-being of depressed patients. Results from the Medical Outcomes Study. JAMA, 262(7), 914–919.
World Health Oraganization. (2019). Social determinants of health. Retrieved May 15, 2019, from https://www.who.int/social_determinants/sdh_definition/en/.
Yoshikawa, H., Aber, J. L., & Beardslee, W. R. (2012). The effects of poverty on the mental, emotional, and behavioral health of children and youth: Implications for prevention. American Psychologist,67(4), 272–284. https://doi.org/10.1037/a0028015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or any other kind of conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
McClintock, H.F., BeKampis, A.N., Hartmann, E. et al. Adherence to Antidepressants in Underserved Communities: A Comparison of Electronic Monitoring and Self-report Measures. Community Ment Health J 56, 727–734 (2020). https://doi.org/10.1007/s10597-019-00533-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-019-00533-2