Abstract
With the recent movement toward a personal-recovery paradigm to treat schizophrenia, the locus of mental health care delivery has shifted toward community-based care. Family caregivers comprise a substantial component of that community, and are often providing care for longer periods, but often have no formal training or support. Caregiver-directed psychosocial interventions (CDPI) have been developed to train and assist caregivers in their efforts to maximize the odds of treatment success for those in their care. This meta-analysis compared CDPI versus treatment as usual (TAU) on outcomes such as hospitalization, relapse, non-compliance, and “other outcomes” (emergency services utilization, suicide attempt, and death). A systematic literature search (2005–2015) was conducted to identify randomized controlled trials of outpatient administered CDPI versus TAU to treat adult patients recovering from schizophrenia. Relative risks (RR) with 95% confidence intervals derived via random effects meta-analysis were calculated to compare CDPI versus TAU on the aforementioned outcomes. Eighteen of the 693 citations were retained for analysis. Overall RR for CDPI versus TAU suggested improved outcomes associated with CDPI: hospitalization [0.62 (0.46, 0.84) p < 0.00001], relapse [0.58 (0.47, 0.73) p < 0.00001] and other outcomes [0.70 (0.19, 2.57) p = 0.59]. CDPI was associated with significantly better compliance with medication and clinical activities combined [0.38 (0.19, 0.74) p = 0.005]. Medication compliance alone favored CDPI but was non-significant. Compliance with clinical activities alone favored CDPI significantly [0.22 (0.11, 0.47) p < 0.00001]. CDPI is associated with reductions in hospitalization, relapse, and treatment non-compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Changes in health care reimbursement and policy have shifted care for chronic psychiatric illnesses such as schizophrenia from inpatient settings and to community-based settings (Awad and Voruganti 2008; Brundtland 2001; Dosman and Keating 2005). Much of this care responsibility outside of traditional institutions has fallen upon families and individual family caregivers (Viana et al. 2013; Eassom et al. 2014) for whom caregiver-directed psychosocial interventions (CDPIs) have been developed. CDPIs can broadly be described (Pharoah et al. 2010) as interventions seeking to: (a) construct an alliance between the caregiver and the person with schizophrenia; (b) reduce adverse family atmosphere (i.e., lowering the emotional climate in the family by reducing stress and burden on relatives); (c) enhance the capacity of caregivers to anticipate and solve problems; (d) reduce expressions of anger and guilt by the family; (e) maintain reasonable expectations for patient performance; (f) encourage relatives to set and keep to appropriate limits while maintaining some degree of separation when needed; and (g) attain desirable change in caregiver’s behavior and belief systems.
Caregiver-directed psychosocial interventions can complement psychiatric care and help caregivers to better understand mental illness, with the aim of improving coping skills. The interventions themselves facilitate healthy support behaviors toward the affected family member and aim to reduce conflict and tension. In schizophrenia specifically, these programs range from providing general information on the psychiatric condition and care, to more comprehensive interventions that include psychoeducation, consultation, family interventions, and therapies (Pharoah et al. 2010). It is important to understand that CDPIs include an element of caregiver participation, and most often also contain associated interventions with the consumer.
Reductions in family caregiver burden associated with CDPIs have been demonstrated in terms of reducing burden on caregiver quality of life, functioning financial strain and stress related conditions (Berglund et al. 2003). The impact of caregiver intervention programs on the outcomes of their mentally ill family members is paradoxically less well-studied, particularly as it relates to relapse and associated acute services utilization.
Previous meta-analyses (Pharoah et al. 2010; Okpokoro et al. 2014; Zhao et al. 2015) have suggested that incorporating family interventions into care can reduce relapses, encourage compliance with medications, and reduce social impairment in persons with schizophrenia. Support in the form of family therapy, when added to antipsychotic medication, is more effective than medication alone in the prevention of relapse. To date, no systematic review or meta-analysis has specifically focused on directly observable patient outcomes pertaining to resource and services utilization, such as: hospitalizations, need for emergency services, and suicide. Herein we report a meta-analysis of CDPI interventions with respect to these observable patient outcomes.
Methods
Systematic Literature Search
The literature was systematically searched for studies describing CDPIs implemented for schizophrenia. In this study, CDPI was defined as an intervention that is: (1) directed toward the caregiver (or caregivers) of a person with schizophrenia, (2) administered by a health care professional in a pre- defined format over multiple sessions, and (3) is psychosocial in nature insofar as it shares any of the aforementioned goals (a–g above). The designation of caregiver was defined at the discretion of each study author, but for the sake of the present review and analysis can be defined as a non-healthcare professional who has a close relationship with the patient and assumed responsibility for the patient’s welfare.
In the present meta-analysis CDPI was compared to treatment as usual (TAU). The latter was defined at the discretion of the authors of the reviewed studies such that TAU could be any treatment for schizophrenia that did not include a caregiver-directed component as described here.
Electronic searches were conducted in PubMed/Medline, PsycNet, and the Cochrane Central Register of Controlled Trials using the following search strategy: (schizophrenia or schizophreniform) AND ((family OR “family directed” OR psychosocial OR caregiver OR “caregiver directed” OR psychoeducational OR psycho-educational OR “behavioral family” OR behavioral) AND (intervention OR education OR psycho-education OR psychoeducation)).
The searches were limited with regard to time frame (2004–2015, inclusive), design (randomized controlled trials), and language (English). Review articles captured by the searches were retained separately so that they could be hand-searched for additional relevant records not captured by the search strategy, but the reviews themselves were not retained for analysis.
Citations yielded by the search strategy and that met the aforementioned criteria were de-duplicated and assessed in iterative rounds—first abstracts, then full text. The following inclusion criteria were applied:
Report and design (a) published in-full and in a peer-reviewed journal, (b) categorized as a randomized controlled trial, (c) randomization occurred in an outpatient treatment setting, (d) participants were randomized to either CDPI or TAU, (e) outcomes measured at pre-defined follow-up intervals, and (f) fewer than 50% of study participants lost to follow-up.
Participants (a) consumers (i.e., persons diagnosed with schizophrenia or schizophreniform disorder) and caregivers were aged ≥ 18 years old, (b) caregivers were family members or individuals with a close relationship to the consumer that existed before randomization to treatment, and (c) caregivers were not healthcare or mental health service providers of the services under investigation. There was no limit applied to the type of schizophrenia.
Outcomes (measured with the consumer as the unit of analysis) (a) inpatient hospitalization, (b) relapse, (c) non-compliance with any intervention received in the study period, and (d) “other events” (suicide attempt, psychiatric emergency services utilization, and death).
Analysis
Analysis was conducted in Review Manager (version 5.3). All outcomes measured were binary and were assessed by relative risk. Confidence intervals (CI, 95%) were derived from a random-effects model given the expected heterogeneity among the studies. Inter-study heterogeneity was assessed using Cochran’s Q and Higgins I2. Outcome data were categorized for stratified outcomes pertaining to the length of follow-up (i.e., outcomes at 0–12, 13–24, and ≥ 24 months post CDPI initiation).
To account for differing intervention durations, follow-up times were adjusted so as to be in relation to randomization and not completion of the intervention. For example, consider a trial in which the intervention was applied for 12 months. Outcomes were measured at 6 months post-randomization, 12 months post-randomization, and 6 months after the intervention was completed. In this case, the outcomes would here be analyzed at 6, 12, and 18 months. Due to the modest number of retained studies for each outcome, we did not control for individual study characteristics. The analyses were also weighted by the sample sizes of the contributing studies. Where necessary, the directionality of binary outcome data was inverted to be consistent with the outcome used in this meta-analysis.
Intervention length and session volume may have some meaningful impact on outcomes (Okpokoro et al. 2014; Zhao et al. 2015). Therefore, Kruskal–Wallis tests were used to individually assess whether (1) intervention length or (2) session frequency were associated with relative risks. Continuous independent variables were transformed to two-level categorical variables. Intervention lengths were categorized as ≤ 52 weeks or > 52 weeks. Session frequency was calculated as the number of sessions divided by the number of weeks over which sessions were applied, and was categorized as ≤ 0.50 or > 0.50.
This study did not include human or animal subjects and was therefore not subject to Institutional Review Board (IRB) approval. This study was funded by Janssen Scientific Affairs, LLC, of which EK, CB, and EE are employees. JC is an employee of EPI-Q, Inc., which received consulting fees from Janssen Scientific Affairs, LLC related to the design and implementation of this study. KA is an employee of MyHealios, Inc., which has an ongoing partnership with Janssen Scientific Affairs, LLC to design and adapt a psychosocial intervention employed in Janssen-supported clinical trials. Neither KA nor MyHealios, Inc. received compensation related to the design, implementation, or report of this study. All authors certify responsibility for this manuscript.
Results
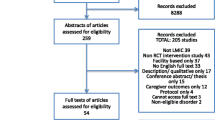
Of 693 unique citations retrieved, 18 studies (Bradley et al. 2006; Bressi et al. 2008; Carra et al. 2007; Chatterjee et al. 2014; Pharoah et al. 2010; Dai 2007; Giron et al. 2010; Grawe et al. 2006; Guo et al. 2010; Hasan et al. 2015; Kulhara et al. 2009; McDonell et al. 2006; Nasr and Kausar 2009; Palma-Sevillano et al. 2011; Secher et al. 2015; Sellwood et al. 2007; Sungur et al. 2011; Valencia et al. 2013) met inclusion criteria and were retained for analysis. The record adjudication process showing the number of records at each step is presented in Fig. 1, and a detailed description of the salient characteristics of each of the included studies—including a description of the CDPI employed in each—is reported in Table 1. The mean duration of the interventions was 57 weeks (± 32), and the mean number of sessions was 28 (± 17). Together, these equate to 0.56 (± 0.34) sessions per week on average.
As summarized in Figs. 2, 3, 4, 5, the relative risk of patients experiencing any negative outcome was lower in the CDPI group compared to the TAU group. The relative risk of hospitalization is shown in Fig. 2, with a significant overall effect across all follow-up periods: RR = 0.62 (95% CI 0.46–0.84, p < 0.00001). When stratified by follow-up time, the only stratum to have reached significance was 0–12 months follow-up: RR = 0.56 (95% CI 0.38–0.82, p < 0.00001). Other follow-up strata directionally favored CDPI but were individually non-significant. Similar relationships were found for the relative risk of relapse (Fig. 3). The overall effect of CDPI versus TAU was statistically significant: RR: 0.58 (95% CI 0.47–0.73, p < 0.00001), as was the effect at 0–12 months follow-up: RR = 0.49 (95% CI 0.37–0.66, p < 0.00001).
Other outcomes, which included suicide attempt, psychiatric emergency services utilization, and death was the only outcome category for which the overall relative risk was not significant: [RR = 0.70 (95% CI 0.19–2.57, p = 0.59) p = 0.59], although it did favor CDPI (Fig. 4).
In one study three of the four sub-comparisons did not favor CDPI (Grawe et al. 2006). Follow-up times were not consistently reported, preventing further stratification.
The relative risk of a patient not adhering to treatment was significantly lower for CDPI versus TAU (Fig. 5): RR = 0.38 (95% CI 0.19–0.74, p = 0.005). When stratified into medication and non-medication adherence, the reduction in medication non-adherence was not statistically significant for CDPI (RR 0.57, 95% CI 0.25, 1.29) but was significant for adherence to non-medication clinical activities: RR = 0.22 (95% CI 0.11–0.47, p < 0.00001). Follow-up times were not consistently reported, preventing further stratification. There was considerable variability in these characteristics found across the retained studies (Table 1).
Discussion
A systematic electronic literature review of multiple bibliographic databases yielded data to conduct a meta-analysis to compare the outcomes of CDPI and TAU for schizophrenia. This analysis indicated that CDPI is associated with significantly lower relative risks versus TAU of relapse, hospitalization, and overall non-compliance. Risks of suicide, psychiatric emergency services utilization, and death favored CDPI but were not significant. The benefits of CDPI reported here are consistent with previous meta-analyses that have focused primarily on endpoints measured with patient- or observer-reported outcome instruments.
While the overall effects in favor of CDPI were significant for three of the four outcome categories, these effects diminished with time for the two outcomes that had follow-up stratified data (i.e., relapse and hospitalization). It has been previously observed (Pharoah et al. 2010; Okpokoro et al. 2014) that the effects of the intervention diminish during the follow-up period where no intervention is received. However, the trends continued to favor CDPI, and so it is possible that that patient/caregiver attrition played a role in the lack of statistical significance across follow-up times. Also note that follow-up-stratified outcomes were most frequently available for 0–12 months, which was the only follow-up subgroup with significant differences between CDPI and TAU.
With regard to an explanation for CDPI’s association with favorable outcomes, the present findings are consistent with two possible etiologies that are not mutually exclusive. The first is the stress-diathesis model, based on the observation that emotional and interpersonal stress are associated with increased risk of relapse (Hesse et al. 2015). Accordingly, caregivers participating in CDPI may have been more likely to engage in clearer communication and better problem-solving for/with schizophrenia patients under their care, which can be reasonably assumed to reduce relapse risk. The second etiology may be increased treatment adherence in the form of a significantly higher attendance rate for clinical activities, thereby permitting more regular assessment of mental state by qualified professionals. A likely rationale for this relationship is that caregivers participating in CDPI are more effective at negotiating treatment adherence. This is consistent with previous reports that higher levels of patient contact with family members and greater family involvement in the treatment process were both associated with greater treatment engagement (Kreyenbuhl et al. 2009; Glick et al. 2011). Notably, the association of CDPI to medication adherence favored CDPI but was not significant. Further research is warranted to assess the impact of CDPI on patients’ adherence to pharmacological treatment, since up to 60% of persons being treated for schizophrenia are non-adherent to medication therapy (Valenstein et al. 2006).
The “other outcomes” grouping consisting of suicide attempt, psychiatric emergency services utilization, and death was the only outcome for which a significant relative risk was not found, and considerable heterogeneity was observed in this category (I2 = 72%). Sub-group outcomes within the “other outcomes” category suffered from small sample sizes in the included studies. The small number of included studies and relatively small sample sizes within those studies likely impacted other comparisons to a lesser degree, as has been noted in the limitations of other similar studies (Pharoah et al. 2010; Okpokoro et al. 2014; Zhao et al. 2015). Moreover, heterogeneity in how these outcomes were defined and in patients’ underlying comorbid psychiatric and medical conditions may have impacted the findings and contributed to outcome variability. Also, the duration and frequency of CDPI sessions were not significantly different; although, these parameters have been found to have significant effects in other studies (Viana et al. 2013; Okpokoro et al. 2014; Zhao et al. 2015). It should also be noted that the present meta-analysis included only published randomized controlled CDPI trials whereas we did not search for unpublished studies. The associated impact of possible publication bias in favor of successful CDPI programs is likely minimal but should be considered in one’s interpretation of these findings.
These findings support the use of CDPI as a means of reducing the frequency of unwanted clinical and resource utilization outcomes associated with declining mental-health status. Furthermore, incorporating CDPI into schizophrenia treatment may also improve humanistic outcomes such as caregiver emotional burden and patient well-being, while simultaneously reducing risk of relapse and hospital and emergency services utilization. Considering the chronic and heterogenous nature of schizophrenia, further research is warranted to evaluate the optimal composition of CDPI programs particularly with regard to the number of sessions, session frequency, and duration.
References
Awad, A. G., & Voruganti, L. N. P. (2008). The burden of schizophrenia on caregivers. Pharmacoeconomics, 26(2), 149–162. https://doi.org/10.2165/00019053-200826020-00005.
Berglund, N., Vahlne, J. O., & Edman, A. (2003). Family intervention in schizophrenia—impact on family burden and attitude. Social Psychiatry and Psychiatric Epidemiology, 38(3), 116–121. https://doi.org/10.1007/s00127-003-0615-6.
Bradley, G. M., Couchman, G. M., Perlesz, A., Nguyen, A. T., Singh, B., & Riess, C. (2006). Multiple-family group treatment for English- and Vietnamese-speaking families living with schizophrenia. Psychiatric Services, 57(4), 521–530. https://doi.org/10.1176/ps.2006.57.4.521.
Bressi, C., Manenti, S., Frongia, P., Porcellana, M., & Invernizzi, G. (2008). Systemic family therapy in schizophrenia: A randomized clinical trial of effectiveness. Psychotherapy and Psychosomatics, 77(1), 43–49. https://doi.org/10.1159/000110059.
Brundtland, G. H. (2001). From the World Health Organization. Mental health: New understanding, new hope. JAMA, 286(19), 2391.
Carra, G., Montomoli, C., Clerici, M., & Cazzullo, C. L. (2007). Family interventions for schizophrenia in Italy: Randomized controlled trial. European Archives of Psychiatry and Clinical Neuroscience, 257(1), 23–30. https://doi.org/10.1007/s00406-006-0677-z.
Chatterjee, S., Naik, S., John, S., et al. (2014). Effectiveness of a community-based intervention for people with schizophrenia and their caregivers in India (COPSI): A randomised controlled trial. Lancet, 383(9926), 1385–1394. https://doi.org/10.1016/S0140-6736(13)62629-X.
Dai, M. (2007). A study on influence of early comprehensive intervention on prognosis of incipient schizophrenia patients. Chinese Nursing Research, 21(9), 3293–3294.
Dosman, D., & Keating, N. (2005). Cheaper for whom? Costs experienced by formal caregivers in adult family living programs. Journal of Aging & Social Policy, 17(2), 67–83. https://doi.org/10.1300/J031v17n02_05.
Eassom, E., Giacco, D., Dirik, A., & Priebe, S. (2014). Implementing family involvement in the treatment of patients with psychosis: A systematic review of facilitating and hindering factors. British Medical Journal Open, 4(10), e006108. https://doi.org/10.1136/bmjopen-2014-006108.
Giron, M., Fernandez-Yanez, A., Mana-Alvarenga, S., Molina-Habas, A., Nolasco, A., & Gomez-Beneyto, M. (2010). Efficacy and effectiveness of individual family intervention on social and clinical functioning and family burden in severe schizophrenia: A 2-year randomized controlled study. Psychological Medicine, 40(1), 73–84. https://doi.org/10.1017/S0033291709006126.
Glick, I. D., Stekoll, A. H., & Hays, S. (2011). The role of the family and improvement in treatment maintenance, adherence, and outcome for schizophrenia. Journal of Clinical Psychopharmacology, 31(1), 82–85. https://doi.org/10.1097/JCP.0b013e31820597fa.
Grawe, R. W., Falloon, I. R. H., Widen, J. H., & Skogvoll, E. (2006). Two years of continued early treatment for recent-onset schizophrenia: A randomised controlled study. Acta Psychiatrica Scandinavica, 114(5), 328–336. https://doi.org/10.1111/j.1600-0447.2006.00799.x.
Guo, X., Zhai, J., Liu, Z., et al. (2010). Effect of antipsychotic medication alone vs combined with psychosocial intervention on outcomes of early-stage schizophrenia: A randomized, 1-year study. Archives of General Psychiatry, 67(9), 895–904. https://doi.org/10.1001/archgenpsychiatry.2010.105.
Hasan, A. A., Callaghan, P., & Lymn, J. S. (2015). Evaluation of the impact of a psycho-educational intervention for people diagnosed with schizophrenia and their primary caregivers in Jordan: A randomized controlled trial. BMC Psychiatry, 15, 72. https://doi.org/10.1186/s12888-015-0444-7.
Hesse, K., Kriston, L., Mehl, S., et al. (2015). The vicious cycle of family atmosphere, interpersonal self-concepts, and paranoia in schizophrenia—a longitudinal study. Schizophrenia Bulletin, 41(6), 1403–1412. https://doi.org/10.1093/schbul/sbv055.
Kreyenbuhl, J., Nossel, I. R., & Dixon, L. B. (2009). Disengagement from mental health treatment among individuals with schizophrenia and strategies for facilitating connections to care: A review of the literature. Schizophrenia Bulletin, 35(4), 696–703. https://doi.org/10.1093/schbul/sbp046.
Kulhara, P., Chakrabarti, S., Avasthi, A., Sharma, A., & Sharma, S. (2009). Psychoeducational intervention for caregivers of Indian patients with schizophrenia: A randomised-controlled trial. Acta Psychiatrica Scandinavica, 119(6), 472–483. https://doi.org/10.1111/j.1600-0447.2008.01304.x.
McDonell, M. G., Short, R. A., Hazel, N. A., Berry, C. M., & Dyck, D. G. (2006). Multiple-family group treatment of outpatients with schizophrenia: Impact on service utilization. Family Process, 45(3), 359–373.
Nasr, T., & Kausar, R. (2009). Psychoeducation and the family burden in schizophrenia: A randomized controlled trial. Annals of General Psychiatry, 8, 17. https://doi.org/10.1186/1744-859X-8-17.
Okpokoro, U., Adams, C. E., & Sampson, S. (2014). Family intervention (brief) for schizophrenia. The Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD009802.pub2.
Palma-Sevillano, C., Cañete-Crespillo, J., Farriols-Hernando, et al. (2011). Randomised controlled trial of cognitive-motivational therapy program for the initial phase of schizophrenia: A 6-month assessment. The European Journal of Psychiatry, 25, 68–80.
Pharoah, F., Mari, J., Rathbone, J., & Wong, W. (2010). Family intervention for schizophrenia. The Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD000088.pub2.
Secher, R. G., Hjorthoj, C. R., Austin, S. F., et al. (2015). Ten-year follow-up of the OPUS specialized early intervention trial for patients with a first episode of psychosis. Schizophrenia Bulletin, 41(3), 617–626. https://doi.org/10.1093/schbul/sbu155.
Sellwood, W., Wittkowski, A., Tarrier, N., & Barrowclough, C. (2007). Needs-based cognitive-behavioural family intervention for patients suffering from schizophrenia: 5-Year follow-up of a randomized controlled effectiveness trial. Acta Psychiatrica Scandinavica, 116(6), 447–452. https://doi.org/10.1111/j.1600-0447.2007.01097.x.
Sungur, M., Soygur, H., Guner, P., Ustun, B., Cetin, I., & Falloon, I. R. (2011). Identifying an optimal treatment for schizophrenia: A 2-year randomized controlled trial comparing integrated care to a high-quality routine treatment. International Journal of Psychiatry in Clinical Practice, 15(2), 118–127. https://doi.org/10.3109/13651501.2011.554987.
Valencia, M., Fresan, A., Juarez, F., Escamilla, R., & Saracco, R. (2013). The beneficial effects of combining pharmacological and psychosocial treatment on remission and functional outcome in outpatients with schizophrenia. Journal of Psychiatric Research, 47(12), 1886–1892. https://doi.org/10.1016/j.jpsychires.2013.09.006.
Valenstein, M., Ganoczy, D., McCarthy, J. F., Myra Kim, H., Lee, T. A., & Blow, F. C. (2006). Antipsychotic adherence over time among patients receiving treatment for schizophrenia: A retrospective review. The Journal of Clinical Psychiatry, 67(10), 1542–1550.
Viana, M. C., Gruber, M. J., Shahly, V., et al. (2013). Family burden related to mental and physical disorders in the world: Results from the WHO World Mental Health (WMH) surveys. Revista Brasileira De Psiquiatria, 35(2), 115–125.
Zhao, S., Sampson, S., Xia, J., & Jayaram, M. B. (2015). Psychoeducation (brief) for people with serious mental illness. The Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD010823.pub2.
Funding
This study was funded by Janssen Scientific Affairs, LLC, of which EK, CB, and EE are employees. JC is an employee of EPI-Q, Inc., which received consulting fees from Janssen Scientific Affairs, LLC related to the design and implementation of this study. KA, at the time of analysis and manuscript development, was an employee of MyHealios, Inc., which has an ongoing partnership with Janssen Scientific Affairs, LLC to design and adapt a psychosocial intervention employed in Janssen-supported clinical trials. Neither KA nor MyHealios, Inc. received compensation related to the design, implementation, or report of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ashcroft, K., Kim, E., Elefant, E. et al. Meta-Analysis of Caregiver-Directed Psychosocial Interventions for Schizophrenia. Community Ment Health J 54, 983–991 (2018). https://doi.org/10.1007/s10597-018-0289-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10597-018-0289-x