Abstract
In recent years, there has been a progressive trend towards less invasive technologies for detecting metastatic cancer and guiding therapy with the goal of lower morbidity, better outcomes, and superior cosmetic appearance than traditional methods. This mini-review examines three emerging noninvasive hybrid technologies for detecting primary cancer, metastasis and guiding thermal therapy. Real-time thermoacoustic imaging and thermometry potentially provides valuable and critical feedback for guiding focused microwave ablation therapy. Label-free photoacoustic monitoring of cancer cells is a promising clinical diagnostic and theranostic tool for detecting metastatic disease and monitoring the response to therapy. Finally, immunologically targeted gold nanoparticles combined with photoacoustic imaging is able to detect lymph node micrometastasis in mouse models of breast cancer. These emerging techniques have the potential to improve the decision to biopsy, provide more accurate prognosis, and enhance the efficacy of therapy for early and late stage cancers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Studies following breast cancer patients for more than 20 years report that breast conserving therapy (BCT) performed as equally well as radical mastectomy [1, 2]. Although lumpectomy followed by radiation therapy is the BCT standard of care for small tumors, such treatment is still considered aggressive, leading to severe breast asymmetry in 35% of patients and morbidity in another 14%, primarily due to bleeding or infection [3]. Surgery can also lead to life-threatening complications, particularly in patients over 70 years with comorbidities. Locally aggressive higher-stage cancer patients also benefit from BCT following neoadjuvant chemotherapy and tumor down-staging [4]. These patients receive a superior cosmetic appearance and better prognosis when combined with radiation therapy. For later-stage cancers, including those involving metastasis, there is also emerging evidence that surgery and radical mastectomy diminish activity of natural killer cells and cytotoxicity of lymphocytes [5, 6]. These studies further suggest that preserving healthy tissue while destroying the tumor may help protect against recurrence and/or distant metastasis. Despite the reported benefits of BCT, current protocols still require invasive surgery, and there is still a need for less invasive strategies to treat localized breast cancer and preserve as much breast tissue as possible, while minimizing chances of metastasis. Consequently, there has been a progressive trend towards minimally or noninvasive methods with lower morbidity and better cosmetic appearance for treating breast and other types of solid tumor cancers. This report will describe three emerging and less invasive approaches that exploit light, ultrasound, and/or microwaves to guide and treat cancer and detect metastasis.
Focused microwave therapy and thermoacoustic thermometry
Several thermal techniques, including hyperthermia, cryoablation, radiofrequency ablation (RFA), interstitial laser therapy (ILT), and high intensity focused ultrasound (HIFU), are used clinically to treat solid tumor breast cancers with the goal of obtaining efficacy similar to or better than BCT. Compared to surgery and other aggressive treatment options, the advantages of thermal therapies are less scarring, better tissue preservation, superior cosmesis, faster recovery time, and lower healthcare cost [8]. Despite the potential benefits of thermal therapies, each method has its own limitations. RFA and ILT are generally limited to small tumors smaller than 20 mm and do not allow for fine control of the thermal dose. HIFU, for example, is time consuming, especially for large tumors, and requires an expensive and bulky MRI scanner for real-time magnetic resonance thermometry (MRT) to track temperature during ablation therapy. Noninvasive focused microwave therapy (FMT) has been proposed as a superior treatment option that addresses some limitations of other thermal therapies [7]. FMT exploits focused microwave radiation near 1 GHz to thermally ablate solid tumors, which typically have higher water content and stronger absorption than surrounding breast tissue. However, one major drawback of FMT has been its inability to reliably monitor temperature of tissue during heating, leading to inaccurate delivery of the thermal dose to the target, while minimizing exposure to surrounding breast tissue. To address this limitation with FMT, thermoacoustic imaging and thermometry (TAI/TAT) has recently been proposed as feedback during FMT to monitor temperature of the breast during microwave heating. This modality depends on the absorption of a short microwave pulse, transient heating, thermoelastic expansion and generation of ultrasound waves. These waves are detected to form images at the millimeter scale, which depend on both the microwave absorption properties of the tissue [8] and its local temperature [9]. Saraswat et al. (2019) proposed a three-ring, 32-element phased array FMT system integrated with TAI/TAT for guiding treatment of breast cancer (Fig. 1a, b) [10]. Proof-of-concept studies with 4 elements [10, 11] demonstrated and validated real-time TAI/TAT during microwave heating of a tissue-mimicking phantom (Fig. 2). Most recently, this same research team developed a 32-channel phased array for electronic focusing and steering a microwave beam into a chamber filled with an oil/water mixture with dielectric properties similar to breast tissue (Fig. 1c, d). Although the diameter of the microwave (0.915 GHz) focal spot at the center of the chamber was approximately 40 mm, the focus could be further reduced through optimization or choosing a higher microwave frequency. Real-time, volumetric TAI/TAT at 3.0 GHz has been further validated with a resolution of ~ 3 mm [12] in a variety of tissue preparations using localized heating in porcine muscle [13] and bovine udder [14] with a mean error of ~ 3% and ~ 7%, respectively. These studies demonstrate the capability and potential utility of a closed-loop image guided breast cancer therapy system based on noninvasive FMT and TAI/TAT technology.
a Concept of image-guided FMT. Top row: Therapy chamber (left, i) containing a 32-element phased array for electronically focusing and steering a microwave beam at 0.915 GHz into the breast for ablation with power delivered (simulated) localized near a tumor (right). Bottom row: Same chamber with an integrated TAI/TAT system for mapping temperature in real-time in terms a volumetric thermal map (right). ii = waveguide for TAI/TAT delivering 500 ns pulses at 1.2 GHz; iii = US array for detecting thermoacoustic and pulse echo signals for imaging; b depiction of a human torso and breast inside oil-filled image-guided therapy chamber; c photograph of 32 channel FMT chamber (three antenna rings of 12 × 8 × 12)[15]. d Map of a section of a 0.95 GHz microwave beam (power) focused into an oil/water mixture (dielectric = 25) and measured with an electric-field sensor. The beam size in this example (depth = 60 mm) was 4.1 × 3.5 × 4.2 cm. The focal size can be reduced by choosing a higher microwave frequency [15]
Thermoacoustic imaging and thermometry during 40 W microwave heating from a four-element patch array. (left) top: pulse echo image of a cross section of a tissue-mimicking gel (1% Agarose and 0.9% NaCl in diH20). Green circles denote thermocouple for measuring ground-truth temperature. Bottom: comparison between middle thermocouple (T3) and TAT over region of interest defined by red box in ultrasound image. (right) Cross-sectional TAI/TAT images at three times points during 40 W microwave heating of the sample. Mean error between the calculated (TAT) and measured temperature was < 10% [11]. (Color figure online)
Label-free photoacoustic liquid biopsy
Galhanza et al. recently developed the Cytophone platform, a label-free clinical photoacoustic imaging system for detecting circulating tumor cells (CTCs) and distant metastasis [16]. The Cytophone featured transcutaneous delivery of near-infrared laser pulses through the intact skin, producing photoacoustic emissions from strongly absorbing blood vessels and melanin-bearing CTCs in patients with melanoma. The acoustic emissions were recorded in real-time using focused ultrasound transducers. Whereas single, cluster and rolling CTCs were detected in 27 of 28 patients (96.4%) with melanoma, there were no such observations in 19 healthy volunteer control subjects. The Cytophone was also proposed as a theranostic tool by monitoring CTC circulation through the cubital vein before and after continuous laser exposure for one hour (Fig. 3). The authors hypothesized that the laser destruction of CTCs was due to nanobubble induced photomechanical effects on the CTC membranes and intracellular structures [17]. A decrease up to 48-fold of CTCs was observed in melanoma patients, suggesting that most CTCs were destroyed following the prolonged pulsed laser exposure. The Cytophone may prove to be a valuable diagnostic tool for detecting early and late-stage metastasis and a theranostic tool by monitoring CTCs before, during, and after treatment.
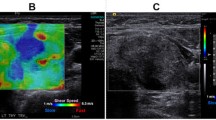
(left) Side-view schematic of the Cytophone. Near-infrared laser pulses (1064 nm, 100–300 µJ) were delivered through the skin of subjects. The photoacoustic emissions from CTCs and red blood cells were detected with cylindrically focused ultrasound transducers and separated based on their waveform. (right) a Photograph of setup with the subject’s arm and Cytophone apparatus; b Pulse echo cross sectional ultrasound image of the cubital vein; PA signal amplitude vs. time before (c) and after (d) one hour laser exposure; spikes indicate CTC detection events above a background threshold. Modified from [16]. (Color figure online)
Immunofunctional photoacoustic imaging of lymph node metastasis
Dumani et al. developed a protocol using glycol-chitosan-coated gold nanoparticles (GC-AuNPs) to detect and image lymph node metastasis in mouse models of breast cancer. The GC-AuNPs were designed to be phagocytosed by immune cells to facilitate uptake into the lymphatic vessels and nodes. Although the nanoparticles normally absorb light near peak wavelength of gold (~ 530 nm), the particles aggregated after entering the cells, which caused a cumulative red shift in their optical absorption properties. The highly specific and targeted imaging approach enabled differentiation of normal-functioning and diseased (metastatic) sentinel lymph nodes 24 h after a subcutaneous injection into the mouse footpad (Fig. 4) [18]. Histology further confirmed that the presence of metastatic cells altered the distribution of GC-AuNP-tagged immune cells. Photoacoustic imaging with the biocompatible nanoparticles developed for this study could be translated to the clinic for detecting micrometastases, guiding the decision to biopsy, and improving the prognosis of metastatic breast cancer with high specificity.
Detection of lymph node metastasis with photoacoustic imaging (PAI, hot colors) and gold nanoparticles. a PAI of sentinel lymph node and afferent lymphatic vessel 24 h after subcutaneous injection of GC-AuNPs in the footpad in a control; b non-metastatic; and c metastatic mouse. The images are superimposed on a B mode pulse echo image displaying anatomical structure; d Nanoparticle-to-tissue ratio for each mouse cohort, indicating that mice with metastatic disease had dramatically lower SNL uptake and function than the other two categories. There was no significant difference between control and non-metastatic mice, demonstrating high sensitivity of the GC-AuNPs (modified from [18]). (Color figure online)
Conclusion
This report described three cutting-edge emerging noninvasive approaches for diagnosing primary and metastatic cancer and guiding therapy. Thermoacoustic thermometry adds crucial feedback to focused microwave heating by accurately quantifying temperature in real-time within a volume of tissue. If successfully demonstrated in the clinic, TAI/TAT-guided FMT would improve outcomes for treating breast cancer by optimizing the thermal dose to the tumor and margins for ablation therapy, while minimizing heat to surrounding regions and preserving as much healthy breast tissue as possible. Additionally, the diagnostic potential of photoacoustic imaging has been discussed, as a means to detect metastasis, using both nanoparticle contrast agents and label-free methods. If this strategy can be extended to the clinic, translational photoacoustic imaging may prove to be a potent modality for gauging function of the lymphatic system and detecting lymph node metastasis with high sensitivity and specificity. This information, in turn, would help guide the decision to biopsy and improve the prognosis for cancer patients.
Abbreviations
- BCT:
-
Breast conservation therapy
- HIFU:
-
High intensity focused ultrasound
- FMT:
-
Focused microwave therapy
- RFA:
-
Radiofrequency ablation
- ILT:
-
Interstitial laser therapy
- TAI/TAT:
-
Thermoacoustic imaging and thermometry
- MRT:
-
Magnetic resonance thermometry
- CTC:
-
Circulating tumor cell
- GC-AuNPs:
-
Glycol-chitosan-coated gold nanoparticles
References
Newman LA, Kuerer HM (2005) Advances in breast conservation therapy. J Clin Oncol 23(8):1685–1697
Carlson RW et al (2009) Breast cancer. Clinical practice guidelines in oncology. J Natl Compr Cancer Netw 7(2):122–192
Littrup PJ et al (2009) Cryotherapy for breast cancer: a feasibility study without excision. J Vasc Interv Radiol 20(10):1329–1341
Singletary SE (2001) Neoadjuvant chemotherapy in the treatment of stage II and III breast cancer. Am J Surg 182(4):341–346
Haen SP et al (2011) More than just tumor destruction: immunomodulation by thermal ablation of cancer. Clin Dev Immunol 2011:160250
Sabel MS (2009) Cryo-immunology: a review of the literature and proposed mechanisms for stimulatory versus suppressive immune responses. Cryobiology 58(1):1–11
Dooley WC et al (2010) Focused microwave thermotherapy for preoperative treatment of invasive breast cancer: a review of clinical studies. Ann Surg Oncol 17(4):1076–1093
Kruger RA et al (2000) Breast cancer in vivo: contrast enhancement with thermoacoustic CT at 434 MHz-feasibility study. Radiology 216(1):279–283
Lou C, Xing D (2010) Temperature monitoring utilising thermoacoustic signals during pulsed microwave thermotherapy: a feasibility study. Int J Hyperthermia 26(4):338–346
Saraswat S et al (2019) Thermoacoustic image-guided focused microwave therapy for enhanced breast cancer treatment. In: 2019 IEEE MTT-S International Microwave Symposium (IMS)
Karunakaran C et al (2019) Real-time thermoacoustic imaging and thermometry during focused microwave heating in multilayer breast phantom. In: 2019 IEEE International Ultrasonics Symposium (IUS)
Karunakaran C, Zhao H, Xin H, Witte RS (2021) Real-time volumetric thermoacoustic imaging and thermometry using a 1.5D ultrasound array. IEEE Trans Ultrason Ferroelectr Freq Control 68:1234–1244
Tamimi EA, Xin H, Witte RS (2020) Real-time 3D thermoacoustic imaging and thermometry using a self-calibration technique. Appl Opt 59(22):G255–G261
Tamimi EA, Xin H, Witte RS (2020) Real-time thermoacoustic imaging and thermometry in bovine udder tissue comparing two calibration methods. In: 2020 IEEE International Ultrasonics Symposium (IUS)
Saraswat S (2020) Thermoacoustic thermometry assisted focused microwave therapy. Masters Thesis, The University of Arizona
Galanzha EI et al (2019) In vivo liquid biopsy using Cytophone platform for photoacoustic detection of circulating tumor cells in patients with melanoma. Sci Transl Med 11(496):eaat5857
Galanzha EI, Zharov VP (2013) Circulating tumor cell detection and capture by photoacoustic flow cytometry in vivo and ex vivo. Cancers 5(4):1691–1738
Dumani DS, Sun IC, Emelianov SY (2019) Ultrasound-guided immunofunctional photoacoustic imaging for diagnosis of lymph node metastases. Nanoscale 11(24):11649–11659
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Presented at the 8th International Cancer Metastasis Congress in San Francisco, CA, USA from October 25–27, 2019 (https://www.cancermetastasis.org). To be published in an upcoming Special Issue of Clinical and Experimental Metastasis: Novel Frontiers in Cancer Metastasis.
Rights and permissions
About this article
Cite this article
Witte, R.S., Tamimi, E.A. Emerging photoacoustic and thermoacoustic imaging technologies for detecting primary and metastatic cancer and guiding therapy. Clin Exp Metastasis 39, 213–217 (2022). https://doi.org/10.1007/s10585-021-10095-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-021-10095-x