Abstract
Breast cancer is the second leading cause of cancer-related deaths among women and 90% of these mortalities can be attributed to progression to metastatic disease. In particular, triple negative breast cancer (TNBC) is extremely aggressive and frequently metastasizes to multiple organs. As TNBCs are categorized by their lack of hormone receptors, these tumors are very heterogeneous and are immune to most targeted therapies. Metabolic changes are observed in the majority of TNBC and a large proportion upregulate enzymes within the serine synthesis pathway, including phosphoserine aminotransferase 1 (PSAT1). In this report, we investigate the role of PSAT1 in migration and invasion potential in a subset of TNBC cell types. We found that the expression of PSAT1 increases with TNBC clinical grade. We also demonstrate that suppression of PSAT1 or phosphoglycerate dehydrogenase (PHGDH) does not negatively impact cell proliferation in TNBC cells that are not dependent on de novo serine synthesis. However, we observed that suppression of PSAT1 specifically alters the F-actin cytoskeletal arrangement and morphology in these TNBC cell lines. In addition, suppression of PSAT1 inhibits motility and migration in these TNBC cell lines, which is not recapitulated upon loss of PHGDH. PSAT1 silencing also reduced the number of lung tumor nodules in a model of experimental metastasis; yet did not decrease anchorage-independent growth. Together, these results suggest that PSAT1 functions to drive migratory potential in promoting metastasis in select TNBC cells independent of its role in serine synthesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the most prevalent cancer diagnosis and the second leading cause of cancer-related deaths among women. Metastatic disease is responsible for over 90% of breast cancer related mortalities [1], which culminates in an overall survival rate of 22% for metastatic patients [2]. Metastasis or advanced recurrent disease affects approximately 30% of patients and is clinically challenging as therapies are often directed at prolonging survival without compromising quality of life [3]. Metastasis can arise from all breast cancer subtypes [4] but triple negative breast cancer (TNBC) is considered the most aggressive as it correlates with poorer overall survival in both early stage and metastatic disease [5]. Separate from hormone receptor positive breast cancers, TNBC is characterized by the lack of estrogen receptor-α (ERα), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) expression [5].
Despite the inherent heterogeneity of TNBC tumors, 70% of TNBCs upregulate the expression of enzymes within the serine synthesis pathway (SSP) [6]. The SSP is a glycolytic shunt that is responsible for converting 3-phosphoglycerate into serine through a series of three reactions. The first reaction, and rate-limiting step, is catalyzed by phosphoglycerate dehydrogenase (PHGDH) and converts 3-phosphoglycerate into 3-phosphohydroxypyruvate. The second enzyme, phosphoserine aminotransferase (PSAT1), couples the conversion of glutamate to α-ketoglutarate with the production of 3-phosphoserine. Phosphoserine phosphatase (PSPH) then dephosphorylates 3-phosphoserine into serine. Most of the previous work involving the SSP and TNBC has focused on a role for PHGDH. Select primary TNBCs and TNBC cell lines have been previously designated as “serine-dependent” or reliant on the cellular production of serine. These cells harbor genetic amplifications of PHGDH or have extremely high PHGDH expression, within which PHGDH silencing causes a significant decrease in proliferation due to loss of alpha-ketoglutarate production through PSAT1 [6]. However, these gene amplifications of PHGDH only account for 6% of primary tumors and 18% of breast cancer cell lines [6]. “Serine synthesis-independent” TNBC cell lines do not harbor genetic amplifications of PHGDH and loss of SSP enzymes yields no anti-proliferative effect in the presence of exogenous serine. Yet, many of these cell types demonstrate elevated expression of the SSP enzymes compared to normal breast tissue, particularly PSAT1, suggesting that these enzymes may have additional functions in TNBC progression [6, 7].
While PSAT1 is not expressed in normal mammary tissue [8], it is elevated in several breast cancer subtypes as well as in several other aggressive malignancies including colon cancer, nasopharyngeal carcinoma, human esophageal squamous cell carcinoma, and non-small cell lung cancer [7, 9,10,11,12,13]. Control of PSAT1 expression is driven by several oncogenic pathways and is differently regulated throughout cell-cycle progression [9, 14,15,16,17,18,19]. Increased PSAT1 expression has been correlated with multiple tumorigenic characteristics, including metastasis and chemoresistance, and is correlated with poorer patient prognosis [9, 11,12,13, 20].
Based on previous reports detailing the requirement for SSP enzymes in “serine synthesis-dependent” TNBC proliferation coupled with PSAT1’s elevated expression in “serine synthesis-independent” TNBC cells, we examined PSAT1’s potential contribution to other TNBC features, particularly in migration and invasion. In this report, we demonstrate that PSAT1 expression increases with TNBC grade and that selective suppression of PSAT1 inhibits the motility and migration of TNBC cells and reduces lung micro-metastases without affecting proliferation. Importantly, loss of PHGDH in “serine synthesis-independent” cells did not phenocopy PSAT1 silencing, suggesting that these effects are specific to PSAT1 in these cell types. Together, these data indicate that PSAT1 plays a role in driving cell migration for the metastatic potential of TNBC.
Materials and methods
Immunohistochemistry
PSAT1 expression was determined in a panel of commercially available tissue microarrays (TMA) that contained de-identified TNBC tumor core sections with provided clinical characteristics, such as grade and histological status of the estrogen and progesterone receptors and HER2 (US Biomax, BR487, BR243, BR1503, and BR1504). TMAs were dewaxed and rehydrated using a series of xylene and ethanol washes. Tissues were then blocked with 5% goat serum and incubated with 1:100 dilution of anti-PSAT1 antibody (ProteinTech) for 16 h at 4°. Sections were subsequently incubated with 1:1000-fold dilution of HRP-conjugated anti-rabbit antibody. PSAT1 was detected using DAB stain (Vector Laboratories), counterstained with hematoxylin, and image was digitally captured using AperioScope digital slide scanner.
Analysis of PSAT1 staining in TNBC sections (ER-, PR-, and HER2-staining as defined by the provided histological analysis accompanying each TMA) was performed using Aperio ImageScope software with the positive pixel count algorithm. Areas of analysis excluded stromal tissue in the tumor samples and was defined to ductal epithelial in the normal breast tissue sections. Comparison of relative PSAT1 levels between normal, grade 1, grade 2, and grade 3 TNBC tissues was determined by dividing the positive pixel count by total pixels (sum of positive and negative) as determined by the software.
Cell culture
MDA-MB-231 and HCC1806 were obtained from ATCC. MDA-MB-231 cells were cultured in IMEM supplemented with 5% FBS and gentamicin and HCC1806 cells were cultured in RPMI-1640 medium supplemented with 10% FBS and gentamicin. All cells were incubated at 37° in 5% CO2.
shRNA and siRNA transfections
PSAT1 siRNA and scrambled negative control siRNA were purchased from Ambion. PHGDH siRNA and non-targeting control pool siRNA were purchased from Dharmacon. PSAT1 shRNA, PHGDH shRNA, and Control shRNA were purchased from Sigma. For transient suppression, siRNAs were transfected into either MDA-MB-231 or HCC1806 cells using RNAiMax Lipofectamine or Polyplus INTERFERin systems according to manufacturer’s protocol. ShRNAs were transfected into cells using the Polyplus jetPRIME reagent according to manufacturer’s protocol and clonal selection for gene silencing was performed using puromycin. The sequences for all siRNA and shRNA species are as follows: PSAT1 RNAi: 5′-CCCUAAACUUGGGAGUUAUtt-3′, negative control RNAi: Silencer Select Negative Control No. 2 cat#4390846, PHGDH RNAi: 5′-CGACAGGUUGCUGAAUGA-3′, non-targeting pool RNAis: 5′-UGGUUUACAUGUCGACUAA-3′, 5′-UGGUUUACAUGUUGUGUA-3′, 5′-UGGUUUACAUGUUUUCUGA-3′, 5′-UGGUUUACAUGUUUUCCUA-3′, PSAT1 shRNA: 5′-CCGGGCACTCAGTGTTGTTAGAGATCTCGAGATCTCTAACAACACTGAGTGCTTTTTG-3′, PHGDH shRNA: 5′- CCGGCTTCGATGAAGGACGGCAAATCTCGAGATTTGCCGTCCTTCATCGAAGTTTTTG-3′, Control shRNA: 5′- CCGGCAACAAGATGAAGAGCACCAACTCGAGTTGGTGCTCTTCATCTTGTTGTTTTT-3′.
Immunoblot assays
Whole-cell lysates were prepared in IP Lysis Buffer (Pierce) containing protease and phosphatase inhibitors. Proteins were separated on 10% SDS-polyacrylamide gels and transferred to PVDF. Membranes were blocked with 5% non-fat dry milk in TBS-T and subsequently probed with 1:1000-fold dilution of anti-PSAT1 (Proteintech, 10501-1-AP) or anti-PHGDH (Sigma HPA021241) antibodies for 16 h at 4°. Washed membranes were then incubated with 1:5000 dilution of HRP-conjugated anti-rabbit or anti-mouse secondary antibodies. Protein detection was done by exposure to ECL Prime chemiluminescent reagent (GE Healthcare). Protein loading was assessed using anti-β-actin antibody (Sigma, A2228).
Cell proliferation
For shRNA silencing, MDA-MB-231 (50,000) cells with or without stable knock-down of PSAT1 or PHGHD were seeded in triplicate in a 12-well (Corning) plate. Cell proliferation was assessed by counting of trypan blue excluded cells 24 and 48-h post-seeding. For siRNA suppression, MDA-MB-231 (50,000) or HCC1806 (30,000) were seeded in 12-well or 24-well (Corning) plate respectively, 24-h post-transfection. Cells were then counted via trypan blue exclusion 24 or 48-h post-seeding.
Wound healing assay
MDA-MB-231 or HCC1806 cells were seeded at 200,000 cells per well in a 12-well (Corning) plate. Cells were either seeded directly (stable shRNA suppression) or 24-hours post siRNA transfection. Scratch in the confluent monolayer was generated with a sterile 200 μL pipette tip. Images were taken at 0 h and 24 h time intervals and % wound healing was quantified using ImageJ.
Migration and invasion assays
For migration assays, MDA-MB-231 and HCC1806 cells were serum starved for 24 h and then plated (25,000 and 50,000 respectively) into Boyden chambers in serum-free medium. Serum-containing medium was placed in each well to serve as the chemoattractant. At 24 h, inserts were fixed with 100% methanol for 10 min and non-migrated cell were removed with a cotton swab. The inserts were then washed with PBS and stained with crystal violet. Images were captured via an EVOS microscope and multiple ×4 fields were analyzed with ImageJ.
For invasion assays, MDA-MB-231 cells were serum starved for a period of 24 h and then plated (50,000) into Corning Biocoat Matrigel Invasion Chambers (Corning) following rehydration according to manufacturer’s protocol. The cells were allowed to invade for 24 h at which point the inserts were fixed with 100% methanol for 10 min and non-invasive cells and remaining matrigel layer were removed via cotton swab. The inserts were then washed with PBS and stained with crystal violet. Images were captured via an EVOS microscope and multiple ×4 fields were analyzed with ImageJ.
Quantitative-real time polymerase-chain reaction
MDA-MB-231 or HCC1806 cells were collected and total RNA was isolated using the RNeasy Mini Kit (Qiagen). One microgram of RNA was converted to cDNA using the High-Capacity RNA-to-cDNA kit (appliedbiosystems) according to the manufacture’s protocol. Samples were then analyzed for qPCR via the TaqMan Fast Advanced (appliedbiosystems) system with human probes for PSAT1 (Hs00795278_mH), PHGDH (Hs00198333_m1), and ACTB (Hs01060665_g1).
Anchorage-independent growth
A bottom layer of 0.6% noble agar in complete medium was prepared in 6 cm dishes. MDA-MB-231 cells were seeded at 50,000 cells per dish in a 0.3% agar solution. Cell colonies were refreshed with 0.25% agar/medium solution every 3–5 days during the 21-day assay. Images were captured via a Nikon digital camera (DXM1200F) attached to a Nikon (SMZ1500) microscope.
Actin cytoskeleton staining
MDA-MB-231 (30,000) or HCC1806 (60,000) cells were plated in Lab-Tek II Chamber slides (154526) either directly or following transfection with siRNA species. Forty-eight hours after plating, cells were fixed with 3.7% formaldehyde solution. The cells were then permeabilized with 0.1% Triton X-100 in PBS before staining with phalloidin (Thermo Fisher) and DAPI (Thermo Fisher) following manufacturer’s protocol. Cellular staining was visualized using an Olympus FV-3000 confocal microscope equipped with Fluoview software (Olympus America Inc.) under ×40 magnification.
Animal model for experimental metastasis
The in vivo study was approved by the University of Louisville’s Institutional Animal Care and Use Committee. The experimental in vivo metastasis model was performed as previously established for MDA-MB-231 cells [21]. Briefly, MDA-MB-231 cells with or without PSAT1 silencing were collected, washed, and resuspended in PBS at a concentration of 1 × 106/mL. One hundred microliters of cell suspension were intravenously injected into the tail vein of athymic nude mice (Charles River), n = 5, shControl; n = 7, shPSAT1. Lung tissue was resected 8 weeks post-injection, formalin fixed, and embedded in paraffin. FFPE lung tissue was sectioned and stained with hematoxylin and eosin to detect MDA-MB-231 foci in the lungs. Images were captured using AperioScope digital slide scanner and micro-metastatic foci were counted from three separate image fields (under ×4 magnification) across individual tissue sections from each animal.
Statistical analysis
Statistical analysis of all studies was performed with Graph Pad Prism software using either analysis of variance (ANOVA) with multiple comparisons test or unpaired t test. Number of replicates for each experimental condition and p values for all results are indicated in their respective figure legends.
Results
PSAT1 expression increases with TNBC grade
In support of the clinical relevance of the serine synthetic pathway in TNBC, we performed immunohistochemistry analysis of breast tissue samples from normal tissue, or at varying grades of TNBC. Similar to previous reports [8], we found that normal breast tissues express low levels of PSAT1 compared to TNBC (Fig. 1). Quantitation of PSAT1 staining revealed a trend towards elevated levels in grade 1 tumor tissue that is significantly increased in higher grades within these TNBC tissues (Fig. 1). These results demonstrate that PSAT1 is expressed in breast tumor tissue, suggesting that PSAT1 has a potential role in the progression of TNBC.
PSAT1 expression increases with TNBC grade. a Formalin-fixed paraffin embedded tissue sections were examined by immunohistological staining for PSAT1. Shown are two independent representative images (×20) from either normal breast tissue or from different grades of TNBC from TMA core sections. b Quantitation of PSAT1 staining demonstrates a significant increase in expression in higher TNBC grade. Relative levels of PSAT1 was determined from multiple independent TMA sections from normal breast tissue (n = 7), or grade 1 (n = 11), grade 2 (n = 14), and grade 3 (n = 14) TNBC. Quantification is demonstrated as relative level (positive/total pixel) of PSAT1 expression and shown are mean ± SEM. *p < 0.01, **p < 0.005, ***p < 0.0001
Suppression of PSAT1 inhibits migration and invasion of select TNBC cell types without affecting cell proliferation
Prior studies have established the SSP as a crucial pathway in cancer progression, including TNBC [6, 20]. However, most of this work has focused on a subset of TNBC designated as “serine-synthesis dependent” in which suppression of any of the SSP enzymes causes a significant proliferative defect. However, there are cell lines in which serine synthesis is dispensable for cell proliferation; yet they still upregulate SSP enzymes when compared to normal breast tissue [6]. This increased expression of SSP enzymes, namely PSAT1, in these serine synthesis-independent cell lines suggests that they may promote tumorigenic properties beyond enhanced proliferation. Based on this, we sought to determine if there was a metastatic role for PSAT1 in two defined serine synthesis-independent TNBC cell models, MDA-MB-231 and HCC1806 [6]. We first found differential expression of PHGDH and PSAT1 in both cell types. While MDA-MB-231 cells predominantly expressed PSAT1 compared to low level of PHGDH, HCC1806 cells exhibited similar levels of both SSP enzymes (Supplementary Fig. 1).
Consistent with previous reports [7], we found that loss of PSAT1, via either stable shRNA or transient siRNA silencing, did not negatively affect cell proliferation (Fig. 2a, b, Supplemental Fig. 2a, b). Alteration in cell morphology, in part due to changes in actin cytoskeleton rearrangement, can directly influence the motile capability of tumor cells. To examine whether loss of PSAT1 affected cytoskeleton structure and cell morphology, we performed phalloidin staining to visualize the F-actin cytoskeleton structure. Upon suppression of PSAT1, MDA-MB-231 cells exhibited changes in both F-actin cytoskeleton arrangement and overall cell morphology compared to control cells (Fig. 2c). In particular, there was a reduction in the spindle-shaped morphology normally observed in these TNBC cells and a disruption in the actin stress fibers (Fig. 2c). These results suggest that PSAT1 may be important for maintenance of cell morphology and may contribute to other tumorigenic properties in the MDA-MB-231 cells, particularly cell motility. To determine the relevance of PSAT1 loss on this cellular function, we examined the migratory ability of MDA-MB-231 cells, by both wound healing and Boyden chamber transwell assays. Both stable and transient suppression of PSAT1 significantly decreased motility of MDA-MB-231 cells by > 50% in both experimental procedures (Fig. 2d, e, Supplemental Fig. 2c, d). We next investigated the invasive potential of these cells using matrigel coated transwells and found that suppression of PSAT1 also significantly inhibited MDA-MB-231 cell invasiveness (Fig. 2f).
Loss of PSAT1 suppresses MDA-MB-231 motility and invasion. a Western blot analysis of PSAT1 expression in MDA-MB-231 cells selected for stable expression of control or PSAT1-specific shRNA. b Cell proliferation in control or PSAT1-shRNA MDA-MB-231 cells. Data are represented as mean ± SD of viable cell counts at 24 and 48 h. c Representative images of cytoskeleton F-actin filaments upon phalloidin staining in both control and PSAT1 shRNA MDA-MB-231 cells. d Representative images of wound healing assays for both control and PSAT1 silencing in MDA-MB-231 cell lines at 0 and 24 h. Quantification is demonstrated as % wound closure (mean ± SD) ****p < 0.0001. e Representative images for migration assays for both control and PSAT1 suppressed cells. Quantification is presented as area stained and shown are mean ± SD **p < 0.01. f Representative images of Matrigel invasion assays with both stable shRNA MDA-MB-231 cell lines. Quantification is reported as area stained and represented as mean ± SD ****p < 0.0001
To determine if these results were unique to these cells or extend to other serine synthesis independent cell systems, we examined the effects of PSAT1 suppression on HCC1806 cells that exhibit comparable PSAT1 and PHGDH expression (Supplemental Fig. 1). Similar to the MDA-MB-231 cells, we observed no proliferative defect upon transient loss of PSAT1 (Fig. 3a, b). In addition, changes in HCC1806 actin stress fibers and cell morphology as seen with phalloidin staining was also comparable to the MDA-MB-231 cells upon PSAT1 suppression, wherein cells exhibited loss of elongated stress fibers (Fig. 3c). Consistent with these findings, the migratory ability of these cells was also significantly inhibited in both the wound healing (Fig. 3d) and Boyden chamber migration assays (Fig. 3e) upon PSAT1 suppression. Taken together, these results suggest that while PSAT1 silencing does not adversely affect the proliferative capacity, PSAT1 loss does significantly inhibit the motility and invasion potential of serine synthesis-independent TNBC cells.
Decreased motility and migration potential of HCC1806 cells upon suppression of PSAT1. a Representative Western blot of PSAT1 levels after transient transfection of negative control or PSAT1 siRNA. b Cell proliferation measured via trypan blue exclusion at 24 and 48 h. Data is shown as mean ± SD of viable cell counts. c Representative images of cytoskeleton F-actin filaments upon phalloidin staining in both negative control and PSAT1 siRNA treated HCC1806 cells. d Representative wound healing assay images. Quantification is presented as % wound closure and shown is mean ± SD **p < 0.01. e Image of cell migration after 24-h. Quantification is presented as area stained and shown is mean ± SD *p < 0.05
Suppression of PHGDH does not phenocopy the loss of PSAT1 on migratory ability
Given the differential levels of PHGDH between these cell lines, this data suggests that the function of PSAT1 in contributing to motility may be separate from its primary role in serine synthesis. To more directly examine this, we tested both MDA-MB-231 (low PHGDH) and HCC1806 (similar PHGDH expression to PSAT1) under both stable and transient suppression of PHGDH within the in vitro motility and migration assays. As PHGDH catalyzes the rate-limiting step in cellular serine production, suppression of this enzyme will underscore the relevance of the SSP for the inhibitory effects we observe. Similar to previous studies, we found no significant effect on proliferation upon loss of PHGDH in the MDA-MB-231 cells (Fig. 4a, b, Supplemental Fig. 3a, b). Unlike our studies with PSAT1 silencing, PHGDH suppression did not affect the cell morphology or the F-actin cytoskeletal structure as observed by phalloidin staining (Supplemental Fig. 3c). We also observed no significant inhibition in either the wound healing (Fig. 4c, Supplemental Fig. 3d) or Boyden chamber migration assays (Fig. 4d, Supplemental Fig. 3e), contrary to our PSAT1 studies.
PHGDH is dispensable for MDA-MB-231 motility. a Representative Western blot analysis demonstrating PHGDH expression in MDA-MB-231 cells stably expressing control or PHGDH specific shRNA. b Cell proliferation at 24 and 48 h with or without PHGDH expression. Data is presented as viable cell counts and shown are mean ± SD for both control and PHGDH shRNA. c Wound healing assays 24 h post-scratch. Data is demonstrated as % wound closure and shown are mean ± SD. d Representative images for Boyden chamber migration assays. Quantification is presented as area stained (mean ± SD)
Alternatively, we also investigated PHGDH function in the HCC1806 cells to demonstrate that these effects are not dependent simply on the dysregulation of the serine synthesis pathway. Similar to MDA-MB-231 cells, suppression of PHGDH did not affect HCC1806 proliferation (Fig. 5a, b), F-actin cytoskeletal arrangement compared to control cells (Fig. 5c), nor inhibit the migratory ability of these cells as observed in wound healing (Fig. 5d) or Boyden chamber migration (Fig. 5e). These results demonstrate that suppression of PHGDH does not phenocopy the effects on cell morphology, motility, and migration that are observed upon PSAT1 silencing. This suggests that promotion of the metastatic characteristics, such as migration and invasion, seen in these serine synthesis-independent TNBC is selective for PSAT1, which may be driven through a function unrelated to its role in de novo serine production.
Loss of PHGDH does not suppress HCC1806 motility and migration. a Western blot analysis for PHGDH expression in HCC1806 cells after transient transfection of control or PHGDH siRNA. b Cell proliferation at 24 or 48 h, which is presented as viable cell counts (mean ± SD). c Representative images of phalloidin stained F-actin filaments upon PHGDH suppression in HCC1806 cells. d Representative images and quantification of wound healing in HCC1806 cells. Data is presented as % wound closure and shown are mean ± SD. e Boyden chamber migration assays of HCC1806 cells with or without PHGDH. Quantification is demonstrated as area stained (mean ± SD)
Suppression of PSAT1 inhibits experimental metastasis
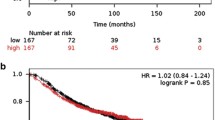
To further investigate the potential role of PSAT1 in TNBC progression, we utilized an established mouse model of experimental metastasis entailing TNBC lung nodule formation after tail-vein injection (Fig. 6a) [21]. Sixty days post-injection, we found a significant decrease in the number of micro-metastatic foci from MDA-MB-231 cells lacking PSAT1 compared to mice injected with control cells (Fig. 6b, c). To ensure that the decrease observed was not due to a loss of anchorage-independent growth, we examined both control and PSAT1 silenced cells for the ability to grow in soft agar. We found that loss of PSAT1 does not affect soft-agar colony formation of these cells (Supplemental Fig. 4), supporting that loss of PSAT1 suppresses the experimental metastasis of TNBC.
PSAT1 silencing inhibits MDA-MB-231 micro-metastases in an experimental metastasis model. a Outline of experimental protocol for the in vivo study. b Representative H&E staining (×4) of lung sections from individual mice receiving no injection or MDA-MB-231 cells with or without stable knock-down of PSAT1. Micro-metastases are indicated by the dark punctate areas of staining. c Micro-metastases were quantified as the sum across three image fields under ×4 magnification from an individual mouse lung section (N = 5, shControl; N = 7, shPSAT1) and presented as metastatic foci (mean ± SD). No micro-metastases were found in no injection control animals. Data analyzed by non-parametric unpaired t test with Mann–Whitney U test, *p = 0.0051
Discussion
In this report, we demonstrate that PSAT1 expression increases in higher grades of TNBC. Through our functional studies employing various suppression approaches in multiple cell systems, our data now highlights PSAT1 as a new driver of migration, invasion, and experimental metastasis through influencing F-actin cytoskeleton rearrangement and cell morphology in serine synthesis independent TNBC. Unlike PHGDH, no genetic amplifications have been observed for PSAT1 [6]; yet elevated levels are presumably the result of oncogenic pathways that promote expression of downstream effectors, such as PSAT1, that are required for TNBC progression and metastasis [9, 19].
Multiple studies have previously demonstrated that activating transcription factor 4 (ATF4) can control PSAT1 expression. ATF4 has been shown to regulate PSAT1 in several different cancer types, including breast cancer [9, 16, 22, 23]. Importantly, in all tumors examined, ATF4 activation increases expression of not only PSAT1 but also enzymes within the entire serine synthesis pathway, including PHGDH and PSPH. As this is not selective for PSAT1 expression, as we have found in the MDA-MB-231 cells, this suggests other regulatory mechanism(s) in TNBC that may be directly controlling PSAT1. Within breast cancer, the transcription factors TAZ/YAP have been shown to have higher activity in basal breast cancer subtype and to selectively induce expression of PSAT1 in TNBC, specifically in the MDA-MB-231 cell line [19]. TAZ expression is activated by the overexpression of the transcription factors Twist and Snail [24]. This increased TAZ/YAP expression/activity has been correlated with high histological grade breast cancer [24] as well as the promotion of oncogenic transformation, enhancing tumorigenic properties, induction of cancer stem cell-like activity and resistance to breast cancer drug therapies [25]. TAZ/YAP have also been linked to increased metastatic capability in breast cancer [26]. In addition, PSAT1 has also been shown to be induced by mTOR and be under the regulation of the PI3K/Akt/mTOR pathway in breast cancer [27]. This pathway has been demonstrated to increase as breast cancer progresses with the highest expression levels correlating with higher grade mammary tumors [28]. The PI3K/Akt/mTOR pathway has also been highly associated with metastasis [28]. Taken together, multiple pro-tumorigenic pathways converge to increase PSAT1 expression that functions to promote the migration and invasion potential of TNBC.
We now show that suppression of PSAT1 in two defined serine synthesis-independent TNBC cell lines does not affect cell proliferation, yet, there is a significant reduction in the cell migration and invasive properties due, in part, to alterations in F-actin cytoskeletal rearrangement and cell morphology. Despite substantial PHGDH expression in a representative cell type (HCC1806), these morphological and migration defects seem to be selective for PSAT1 as PHGDH suppression did not phenocopy loss of PSAT1. Further, PSAT1 contribution to experimental metastatic activity was observed as protein suppression significantly inhibits lung micro-metastasis formation without disrupting anchorage-independent growth of these cells. As the tail-vein injection experimental model is limited in its assessment of the entire metastatic cascade, particularly tumor cell escape from a primary tumor, future examination of effects of PSAT1 loss in metastatic potential from primary orthotopic tumors will be necessary to fully assess its function in TNBC metastasis. Yet, these results suggest that PSAT1 may have an alternate function in contributing to TNBC metastasis that is separate from its role in serine synthesis.
It is important to note that these studies were carried out in TNBC cell types that have been designated as independent of de novo serine synthesis. While expressing SSP enzymes, there is little to no metabolic flux in these cells, thereby necessitating a requirement for external serine for cell proliferation. Conversely, it is well documented that there are TNBC cell lines and patient tumors that are designated as serine synthesis-dependent. This subset exhibits extremely high expression of PHGDH primarily due to genetic amplifications. This drives increased flux through the SSP and allows for growth in serine lacking conditions. Yet, even in serine complete conditions, suppression of PHGDH or PSAT1 causes a significant reduction in cell proliferation in vitro due to disruptions in glutaminolysis and nucleotide production [6, 9]. In addition, suppression of PHGDH, or the use of PHGDH inhibitors, have been shown to have a detrimental effect on the growth of these tumors in vivo [6, 29].
While serine synthesis-dependent tumor cells are sensitive to PHGDH inhibitors, these compounds had no effect on serine synthesis-independent cell types [29] and furthermore did not affect serine flux within this subset [6]. Consistent with these results, suppression of PSAT1 or PHGDH also did not affect the proliferative capacity in the MDA-MB-231 cells in our studies [6, 7]. Conversely, others have also demonstrated that overexpression of PSAT1 in other independent cell types was able to increase proliferation and metastatic capability [9]. Whether these effects were directly due to increased de novo serine synthesis is unclear but supports a role for PSAT1 in promoting cell metastasis. These previous findings coupled with our results demonstrating the inhibitory effects upon suppression of PSAT1 indicate a selective role for PSAT1 and not a result of dysregulation of de novo serine production.
While these results suggest an activity for PSAT1 apart from serine synthesis, its pro-migratory and invasion function(s) in these cell types is unclear. There have been several mechanisms proposed for non-canonical functions of PSAT1. For example, in esophageal cancer, PSAT1 acts upstream of Akt that controls downstream targets of GSK-3β and Snail, which work to promote tumor progression and enhance metastatic characteristics [11]. In non-small cell lung cancer, it has been suggested that PSAT1 inhibits the degradation of cyclin D1, which leads to an alteration in the Rb-E2F pathway [13]. However, despite these potential non-canonical activities of PSAT1, decreased PSAT1 generally resulted in loss of cell proliferation. This is not evident in our systems and suggests another yet unknown function. Alternatively, Yang et al. postulates that TAZ/YAP’s regulation of PSAT1 is driven by a need to generate α-ketoglutarate in order to feed into the TCA. They found that the serine-independent MDA-MB-231 cell line exhibits a high level of TAZ/YAP and is designated as glutamine dependent [19]. This observation from Yang et al. combined with the implications of TAZ/YAP in metastasis indicates that this might be a mechanism in which PSAT1 is contributing to the metastatic characteristics of TNBC. In addition, the observed disruption in actin fibers upon suppression of PSAT1 indicates that PSAT1 may contribute particularly to metastatic potential by maintenance of cytoskeleton structure in promoting cell motility.
Given the extent of PSAT1 expression across TNBC, even within subsets not dependent on de novo serine synthesis, suggests that it may serve an alternate function. These studies support a non-canonical role as loss of PHGDH did not phenocopy PSAT1 suppression. Continued work will be necessary to define whether PSAT1 functions in a similar manner in additional TNBC cell types and the mechanisms by which PSAT1 supports TNBC metastasis. Yet, despite the uncertainty of these mechanism, we believe that PSAT1 is an appealing potential therapeutic target for TNBC patients; particularly in suppressing metastatic spread.
Abbreviations
- TNBC:
-
Triple negative breast cancer
- SSP:
-
Serine synthesis pathway
- PSAT1:
-
Phosphoserine aminotransferase 1
- PHGDH:
-
Phosphoglycerate dehydrogenase
References
Gupta GP, Massague J (2006) Cancer metastasis: building a framework. Cell 127(4):679–695. https://doi.org/10.1016/j.cell.2006.11.001
Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2017) SEER cancer statistics review, 1975–2014. National Cancer Institute, Bethesda
O’Shaughnessy J (2005) Extending survival with chemotherapy in metastatic breast cancer. Oncologist 10(3):20–29
Kimbung S, Loman N, Hedenfalk I (2015) Clinical and molecular complexity of breast cancer metastases. Semin Cancer Biol 35:85–95. https://doi.org/10.1016/j.semcancer.2015.08.009
Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L (2016) Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol 13(11):674–690. https://doi.org/10.1038/nrclinonc.2016.66
Possemato R, Marks KM, Shaul YD, Pacold ME, Kim D, Birsoy K, Sethumadhavan S, Woo HK, Jang HG, Jha AK, Chen WW, Barrett FG, Stransky N, Tsun ZY, Cowley GS, Barretina J, Kalaany NY, Hsu PP, Ottina K, Chan AM, Yuan B, Garraway LA, Root DE, Mino-Kenudson M, Brachtel EF, Driggers EM, Sabatini DM (2011) Functional genomics reveal that the serine synthesis pathway is essential in breast cancer. Nature 476(7360):346–350. https://doi.org/10.1038/nature10350
Samanta D, Park Y, Andrabi SA, Shelton LM, Gilkes DM, Semenza GL (2016) PHGDH expression is required for mitochondrial redox homeostasis, breast cancer stem cell maintenance, and lung metastasis. Cancer Res 76(15):4430–4442. https://doi.org/10.1158/0008-5472.can-16-0530
Uhlen M, Fagerberg L, Hallstrom BM, Lindskog C, Oksvold P, Mardinoglu A, Sivertsson A, Kampf C, Sjostedt E, Asplund A, Olsson I, Edlund K, Lundberg E, Navani S, Szigyarto CA, Odeberg J, Djureinovic D, Takanen JO, Hober S, Alm T, Edqvist PH, Berling H, Tegel H, Mulder J, Rockberg J, Nilsson P, Schwenk JM, Hamsten M, von Feilitzen K, Forsberg M, Persson L, Johansson F, Zwahlen M, von Heijne G, Nielsen J, Ponten F (2015) Proteomics. Tissue-based map of the human proteome. Science 347(6220):1260419. https://doi.org/10.1126/science.1260419
Gao S, Ge A, Xu S, You Z, Ning S, Zhao Y, Pang D (2017) PSAT1 is regulated by ATF4 and enhances cell proliferation via the GSK3beta/beta-catenin/cyclin D1 signaling pathway in ER-negative breast cancer. J Exp Clin Cancer Res 36(1):179. https://doi.org/10.1186/s13046-017-0648-4
Liao KM, Chao TB, Tian YF, Lin CY, Lee SW, Chuang HY, Chan TC, Chen TJ, Hsing CH, Sheu MJ, Li CF (2016) Overexpression of the PSAT1 gene in nasopharyngeal carcinoma is an indicator of poor prognosis. J Cancer 7(9):1088–1094. https://doi.org/10.7150/jca.15258
Liu B, Jia Y, Cao Y, Wu S, Jiang H, Sun X, Ma J, Yin X, Mao A, Shang M (2016) Overexpression of phosphoserine aminotransferase 1 (PSAT1) predicts poor prognosis and associates with tumor progression in human esophageal squamous cell carcinoma. Cell Physiol Biochem 39(1):395–406. https://doi.org/10.1159/000445633
Vie N, Copois V, Bascoul-Mollevi C, Denis V, Bec N, Robert B, Fraslon C, Conseiller E, Molina F, Larroque C, Martineau P, Del Rio M, Gongora C (2008) Overexpression of phosphoserine aminotransferase PSAT1 stimulates cell growth and increases chemoresistance of colon cancer cells. Mol Cancer 7:14. https://doi.org/10.1186/1476-4598-7-14
Yang Y, Wu J, Cai J, He Z, Yuan J, Zhu X, Li Y, Li M, Guan H (2015) PSAT1 regulates cyclin D1 degradation and sustains proliferation of non-small cell lung cancer cells. Int J Cancer 136(4):E39–50. https://doi.org/10.1002/ijc.29150
Baek JY, Jun DY, Dennis TAUB, Kim YH (2003) Characterization of human phosphoserine aminotransferase involved in the phosphorylated pathway of L-serine biosynthesis. Biochem J 373:191–200
Amelio I, Markert EK, Rufini A, Antonov AV, Sayan BS, Tucci P, Agostini M, Mineo TC, Levine AJ, Melino G (2014) p73 regulates serine biosynthesis in cancer. Oncogene 33(42):5039–5046. https://doi.org/10.1038/onc.2013.456
DeNicola GM, Chen PH, Mullarky E, Sudderth JA, Hu Z, Wu D, Tang H, Xie Y, Asara JM, Huffman KE, Wistuba II, Minna JD, DeBerardinis RJ, Cantley LC (2015) NRF2 regulates serine biosynthesis in non-small cell lung cancer. Nat Genet 47(12):1475–1481. https://doi.org/10.1038/ng.3421
Sun L, Song L, Wan Q, Wu G, Li X, Wang Y, Wang J, Liu Z, Zhong X, He X, Shen S, Pan X, Li A, Wang Y, Gao P, Tang H, Zhang H (2015) cMyc-mediated activation of serine biosynthesis pathway is critical for cancer progression under nutrient deprivation conditions. Cell Res 25(4):429–444. https://doi.org/10.1038/cr.2015.33
Svoboda LK, Teh SSK, Sud S, Kerk S, Zebolsky A, Treichel S, Thomas D, Halbrook CJ, Lee HJ, Kremer D, Zhang L, Klossowski S, Bankhead AR, Magnuson B, Ljungman M, Cierpicki T, Grembecka J, Lyssiotis CA, Lawlor ER (2018) Menin regulates the serine biosynthetic pathway in Ewing sarcoma. J Pathol 245(3):324–336. https://doi.org/10.1002/path.5085
Yang CS, Stampouloglou E, Kingston NM, Zhang L, Monti S, Varelas X (2018) Glutamine-utilizing transaminases are a metabolic vulnerability of TAZ/YAP-activated cancer cells. Embo Rep. https://doi.org/10.15252/embr.201643577
Pollari S, Käkönen SM, Edgren H, Wolf M, Kohonen P, Sara H, Guise T, Nees M, Kallioniemi O (2011) Enhanced serine production by bone metastatic breast cancer cells stimulates osteoclastogenesis. Breast Cancer Res Treat 125:421–430. https://doi.org/10.1007/s10549-010-0848-5
Yang S, Zhang JJ, Huang XY (2012) Mouse models for tumor metastasis. Methods Mol Biol 928:221–228. https://doi.org/10.1007/978-1-62703-008-3_17
Riscal R, Schrepfer E, Arena G, Cisse MY, Bellvert F, Heuillet M, Rambow F, Bonneil E, Sabourdy F, Vincent C, Ait-Arsa I, Levade T, Thibaut P, Marine JC, Portais JC, Sarry JE, Le Cam L, Linares LK (2016) Chromatin-bound MDM2 regulates serine metabolism and redox homeostasis independently of p53. Mol Cell 62(6):890–902. https://doi.org/10.1016/j.molcel.2016.04.033
Zhao E, Ding J, Xia Y, Liu M, Ye B, Choi JH, Yan C, Dong Z, Huang S, Zha Y, Yang L, Cui H, Ding HF (2016) KDM4C and ATF4 cooperate in transcriptional control of amino acid metabolism. Cell Rep 14(3):506–519. https://doi.org/10.1016/j.celrep.2015.12.053
Cordenonsi M, Zanconato F, Azzolin L, Forcato M, Rosato A, Frasson C, Inui M, Montagner M, Parenti AR, Poletti A, Daidone MG, Dupont S, Basso G, Bicciato S, Piccolo S (2011) The Hippo transducer TAZ confers cancer stem cell-related traits on breast cancer cells. Cell 147(4):759–772. https://doi.org/10.1016/j.cell.2011.09.048
Hiemer SE, Szymaniak AD, Varelas X (2014) The transcriptional regulators TAZ and YAP direct transforming growth factor beta-induced tumorigenic phenotypes in breast cancer cells. J Biol Chem 289(19):13461–13474. https://doi.org/10.1074/jbc.m113.529115
Zanconato F, Cordenonsi M, Piccolo S (2016) YAP/TAZ at the roots of cancer. Cancer Cell 29(6):783–803. https://doi.org/10.1016/j.ccell.2016.05.005
Coloff JL, Murphy JP, Braun CR, Harris IS, Shelton LM, Kami K, Gygi SP, Selfors LM, Brugge JS (2016) Differential glutamate metabolism in proliferating and quiescent mammary epithelial cells. Cell Metab 23(5):867–880. https://doi.org/10.1016/j.cmet.2016.03.016
Qiao M, Sheng S, Pardee AB (2008) Metastasis and AKT activation. Cell Cycle 7(19):2991–2996. https://doi.org/10.4161/cc.7.19.6784
Pacold ME, Brimacombe KR, Chan SH, Rohde JM, Lewis CA, Swier LJ, Possemato R, Chen WW, Sullivan LB, Fiske BP, Cho S, Freinkman E, Birsoy K, Abu-Remaileh M, Shaul YD, Liu CM, Zhou M, Koh MJ, Chung H, Davidson SM, Luengo A, Wang AQ, Xu X, Yasgar A, Liu L, Rai G, Westover KD, Vander Heiden MG, Shen M, Gray NS, Boxer MB, Sabatini DM (2016) A PHGDH inhibitor reveals coordination of serine synthesis and one-carbon unit fate. Nat Chem Biol 12(6):452–458. https://doi.org/10.1038/nchembio.2070
Acknowledgements
The authors thank Drs. Lee Schmidt, Howard Donninger, and Penn Muluhngwi for their technical assistance with the migration studies. This work was supported by the Kim Hazelwood Glass Gift for Translational Metastatic Breast Cancer Research and funds from the James Graham Brown Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Metcalf, S., Dougherty, S., Kruer, T. et al. Selective loss of phosphoserine aminotransferase 1 (PSAT1) suppresses migration, invasion, and experimental metastasis in triple negative breast cancer. Clin Exp Metastasis 37, 187–197 (2020). https://doi.org/10.1007/s10585-019-10000-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-019-10000-7