Abstract
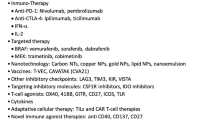
Malignant melanoma is generally chemo- and radio-resistant, and patients with advanced melanoma have a poor prognosis. However, with our increased understanding of the checkpoint immune molecules and genetic alterations of melanoma cells, more effective immunotherapy, such as anti CTLA4 antibody and anti PD-1 antibodies, and targeted drug therapy, such as BRAF inhibitors and MEK inhibitors, have been developed, resulting in improved overall survival and quality of life of patients with advanced melanoma. In addition, emerging technologies to develop prognostic and predictive biomarkers for response to systemic therapy could help clinicians make more accurate assessments of the disease and formulate more effective treatment plans. In this review, current standard systemic therapy options and recently developed novel drugs for advanced melanoma are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Melanoma is the most aggressive type of skin cancer, and the incidence of malignant melanoma has been increasing considerably over the last several decades. It is the fifth and sixth most common cancer among men and women, respectively, in the United States [1]. In 2017, approximately 87,110 new cases and 9730 deaths are estimated to occur in the United States [1]. Although melanoma occurs less frequently than other skin cancers, such as basal cell carcinoma and squamous cell carcinoma, it is responsible for the majority of skin cancer-related deaths [2]. The survival rate is largely associated with the stage of the disease at the time of diagnosis. Patients with early stage melanoma have an excellent chance of cure with surgery alone, whereas those with stage IV melanoma have a 5 year survival rate of 16% with conventional cytotoxic chemotherapy or cytokine therapies [3]. However, with recent advances in immunotherapy and targeted drug therapy, patients with metastatic melanoma now have more effective therapeutic options and are living longer than ever. We discuss here the current standard systemic therapies and the recent development of novel therapies for advanced melanoma. Table 1 summarizes FDA-approved systemic therapy regimens for advanced melanoma.
Cytotoxic chemotherapy
Malignant melanoma is generally resistant to cytotoxic chemotherapy, and the clinical benefit of chemotherapy is modest at best. Dacarbazine was the first drug to be approved by the U.S. Food and Drug Administration (FDA) in 1975 for the management of advanced melanoma. However, the response rate of dacarbazine is less than 15%, and most recent phase III studies which used dacarbazine as a comparison drug frequently showed a response rate of less than 10% according to the RECIST response evaluation criteria [4,5,6,7]. In addition, dacarbazine has not been shown to have survival benefit in this patient population. Other cytotoxic drugs, such as platinums, taxanes and vinka alkaloids, have a similar single agent clinical activity [8]. Combination regimens of cytotoxic chemotherapeutic drugs, including interleukin-2-based biochemotherapy, have higher response rates, but the progression-free survival (PFS) duration is rather short, and no such regimens have been shown to prolong overall survival (OS) [8,9,10,11]. Therefore, cytotoxic chemotherapy is no longer the treatment of choice in the first-line treatment setting, and is often considered as the last choice among the currently available standard therapies.
Interleukin-2
Interleukin-2 (IL-2) is an immunomodulatory cytokine, which activates natural killer cells and cytotoxic T-lymphocytes. A number of phase II studies of high-dose IL-2 demonstrated that a durable clinical response was achievable, and a majority of those who had a complete response had an OS duration longer than 5 years [12, 13]. Because of its ability to induce long-term durable response, high-dose IL-2 was approved by the FDA in 1998. Unfortunately, only a small portion of patients respond to high-dose IL-2 therapy, and only approximately 4% of treated patients have long-term survival [12, 13]. In addition, high dose IL-2 therapy leads to severe toxicity, including significant capillary leak syndrome leading to hypoxia, hypotensive shock and renal failure. Accordingly, high dose IL-2 therapy requires intense cardiac monitoring in the intensive care unit setting or in hospitals specialized in this therapy. Therefore, the use of this treatment has fallen out of favor among most melanoma experts.
Targeted drug therapy
Targeted drug therapy utilizes agents that inhibit the growth or spread of cancer, by interfering with specific target molecules essential for proliferation, invasion and/or survival of cancer cells or tumor-associated vasculature. Interestingly, melanoma has the highest number of mutations among all cancers, likely because a majority of melanomas are induced by mutagenic ultraviolet exposure [14]. The most common mutation is a single substitution mutation in the BRAF gene, which occurs nearly 50% of cutaneous melanomas, followed by mutations in the NRAS (21%) [15]. However, in acral lentiginous and mucosal melanoma, mutations in BRAF and NRAS occur much less often; instead, mutations in the KIT gene play more important role [16]. In uveal melanoma, nearly 80% of tumors have mutations in either the GNAQ or GNA11 gene, and rarely in BRAF and NRAS genes [17, 18]. All of these genetic alterations are kinase-activating mutations, a fact which has implications for the identification of focused and actionable drug targets. In fact, this therapeutic approach has led to successful drug development, exemplified by selective BRAF and MEK inhibitors currently used for the treatment of V600 BRAF mutant-melanoma.
BRAF-mutant melanoma
BRAF inhibitors
BRAF is a serine-threonine kinase protein substrate in the MAP kinase pathway, which plays an important role in proliferation and survival of melanoma cells. The vast majority of mutations in BRAF occur at codon 600, where a single amino acid substitution mutation replaces valine with glutamic acid (V600E). This variant accounts for nearly 80% of all BRAF mutations, followed by a single substitution from valine to lysine at the same codon (V600K), which accounts for ~ 15% [19]. These V600 BRAF mutations lead to constitutive activation of the MAP kinase pathway in melanoma, and inhibiting these mutations effectively leads to inactivation of this signaling pathway, resulting in cell growth arrest. One of the major breakthroughs in treatment of advanced melanoma was the development of selective BRAF inhibitors, namely vemurafenib and dabrafenib. A phase I, dose-escalation trial of vemurafenib demonstrated an overall response rate of 81% in 32 patients with metastatic V600 BRAF mutant-melanoma [20]. In a large, randomized phase III trial of vemurafenib, 675 patients with previously untreated metastatic melanoma harboring a V600E BRAF mutation were treated with either vemurafenib or dacarbazine [4, 21]. There was significant improvement in OS, PFS and response rate in the vemurafenib arm. A hazard ratio (HR) for OS was 0.70 (95% CI 0.57–0.87; p = 0.0008), and median OS duration was 13.6 months for the vemurafenib arm vs 9.7 months for the dacarbazine arm. A HR for PFS was HR 0.38 (95% CI 0.32–0.46; p < 0.0001) with a median PFS duration of 6.9 months in the vemurafenib arm. Response rates were 48 and 5% in the vemurafenib and the dacarbazine arm, respectively. On the basis of the positive results of this phase III study, vemurafenib was approved by the FDA for treatment of advanced V600 BRAF-mutant melanoma in 2011.
Similarly, in a randomized phase III study which compared the clinical benefit of another selective BRAF inhibitor, dabrafenib, to that of dacarbazine, the response rate was higher (50 vs. 6%), and the median PFS duration was longer (5.1 vs. 2.7 months) in patients who received dabrafenib treatment [5]. A HR for PFS, which was the primary endpoint of the study, was 0.30 (95% CI 0.18–0.51; p < 0.0001). This finding led to the approval of dabrafenib by the FDA in this patient population in 2013.
MEK inhibitors
MEK inhibitors have been evaluated in patients with metastatic melanoma harboring a V600 BRAF mutation because the MEK protein is the only known downstream substrate of BRAF kinase in the MAPK signaling transduction pathway. In the early 2000s, a number of MEK inhibitors, such as CI-1040 and PD0325901, were evaluated in patients with metastatic solid tumor. However, these drugs were too toxic or ineffective to be clinically useful [22]. In the late 2000s, trametinib, a specific inhibitor of the MEK1 and MEK2 proteins, was shown in phase I and II studies to have promising clinical activity in patients with V600 BRAF-mutant melanoma [23, 24]. In a randomized phase III study of 322 patients with metastatic V600E or K BRAF-mutant melanoma, trametinib had superior PFS (HR 0.45 [95% CI 0.33–0.63]; p < 0.001) and response rate (22 vs. 8%) over cytotoxic chemotherapy [25]. The median PFS duration was 4.8 months among patients who were treated with trametinib. Interestingly, the clinical activity of trametinib was minimal in patients with V600 BRAF mutant melanoma whose disease had progressed on previous BRAF inhibitor treatment [24]. Although trametinib and selective BRAF inhibitors have not been compared head to head, most clinicians would choose either vemurafenib or dabrafenib over trametinib as a single agent therapy because of the higher response rate and longer median PFS duration observed with the BRAF inhibitors.
Combination of BRAF inhibitor and MEK inhibitor
Despite the high response rates observed with BRAF inhibitors, a vast majority of patients develop resistance to these drugs. Although a number of different mechanisms of resistance have been demonstrated, reactivation of the MAP kinase pathway through development of new mutations in the NRAS and MEK genes, amplification of CRAF, or alternate splicing of BRAF appear to be the most common [26,27,28,29,30]. Preclinical studies demonstrated that addition of a MEK inhibitor to a BRAF inhibitor delays drug resistance to BRAF inhibitor treatment [26,27,28,29,30].
To test this hypothesis, three large, randomized phase III studies (COMBI-D, COMBI-V and co-BRIM) were conducted to evaluate the clinical benefit of a combination of a BRAF inhibitor and a MEK inhibitor compared with a BRAF inhibitor alone; The COMBI-V and COMBI-D trials evaluated a combination of dabrafenib and trametinib [31,32,33], and the co-BRIM trial evaluated a combination of vemurafenib and cobimetinib, another selective MEK1/2 inhibitor. All three studies demonstrated a significant clinical improvement over treatment with a single agent BRAF inhibitor, with respect to OS, PFS and response rate (Table 2).
The overall clinical benefit advantage of these two combination regimens over BRAF inhibitor alone were strikingly similar; HRs for PFS ranged from 0.56 to 0.67, and HRs for OS ranged from 0.69 to 0.71, indicating the clinical advantage of the combination regimens [31,32,33]. Median PFS and OS durations for the combination regimens were 11–12.3 months and 22.3–26 months, respectively. Response rates were 66–69% for the combination treatment vs 45–53% for BRAF inhibitor alone.
In the phase 3 study of dabrafenib and trametinb vs dabrafenib alone (COMBI-D), the most common adverse event was pyrexia (52%) in the combination treatment group, and hyperkeratosis (33%) in the dabrafenib only group [31]. Grade 3 or 4 adverse events occurred in 32% patients in the combination treatment group and 31% patients in the dabrafenib only group [32]. A phase 3 trial of vemurafenib and cobimetinib (coBRIM) showed that the most common grade 3–4 adverse events were γ-glutamyl transferase increase (15%), blood creatine phosphokinase increase (12%), and alanine transaminase increase (11%) [33]. Serious adverse events occurred in 37 and 28% of patients in the combination treatment group and vemurafenib alone group.
With the clear survival advantage and acceptable safety profile, the combinations of BRAF inhibitor and MEK inhibitor have now become the standard for treatment of advanced V600 BRAF mutant-melanoma. In addition to the two combination regimens, another combination of encorafenib (a BRAF inhibitor) and binimetinib (a MEK inhibitor) was shown to have superior clinical benefit over encorafenib alone or vemurafenib alone [34]. Median PFS durations were 14.9, 9.6 and 7.3 months for the combination treatment, encorafenib alone and vemurafenib alone, respectively (HR 0.51 [for the combination treatment in relation to vemurafenib], [95% CI 0.39–0.67]; p < 0.0001). Overall survival was also longer with the combination treatment; Median OS was 33.6 months for the combination vs 16.9 months for vemurafenib (HR 0.61 [95% CI 0.47–0.79]; p < 0.0001). Overall response rates were 64, 52 and 41% for the combination treatment, encorafenib alone and vemurafenib alone, respectively. On the basis of clear clinical advantage of the combination over the BRAF inhibitors alone, this regimen was approved by the FDA for treatment of V600 BRAF-mutant melanoma in June of 2018.
KIT-mutant melanoma
KIT is a receptor tyrosine kinase that activates cellular signaling pathways via PI3K/AKT, the Janus kinase JAK2, and kinases of the Src family. Although KIT mutations are generally rare in melanoma, they occur more frequently in certain types of melanomas, such as mucosal (21%) and acral lentiginous melanomas (11%) [35]. In three phase II clinical trials of imatinib, a potent KIT inhibitor, a total of 118 patient with advanced melanoma containing a KIT mutation were treated, and the results showed response rates of 16–29% and a median PFS duration of 3–3.7 months [36,37,38]. Another potent KIT inhibitor, nilotinib, was also evaluated in a phase II study in 42 treatment-naïve patients with KIT-mutant melanoma; a response rate was 26%, and a median PFS duration was 4.2 months [39]. In all of the clinical trials of KIT inhibitors, greater clinical activity was observed in patients with KIT mutations occurring in exon 9 or 11. Although no KIT inhibitors have been approved by the FDA for the treatment of KIT-mutant melanoma, many oncologists consider imatinib as the treatment of choice for patients whose disease has progressed on checkpoint inhibitor therapy [14].
NRAS-mutant melanoma
NRAS mutations are found in about 21% of all melanomas [15]. The most common NRAS mutations occur at codons 12, 13 and 61. NRAS activates the MAPK pathway and also other signaling pathways such as the PI3K/AKT pathway. NRAS mutations are associated with poorer prognosis in patients with melanoma [40, 41]. Unfortunately, there are no known effective targeted therapies for patients with NRAS mutations to date. Recently, a phase III study of binimetinib, a selective MEK inhibitor, versus dacarbazine was conducted to compare the clinical benefit of the MEK inhibition in this patient population. Four hundred and two patients with advanced NRAS mutant-melanoma were enrolled to receive either binimetinib or dacarbazine in a 2:1 ratio. In this study, patients who were treated with binimetinib had a longer PFS (HR 0.62 [95% CI 0.47–0.80]; p < 0.001), satisfying the primary endpoint of the trial [42]. However, a median PFS in the binimetinib group was only 2.8 months (95% CI 2.8–3.6), and there was no survival advantage. It is unlikely that binimetinib as a monotherapy will have a meaningful clinical impact in patients with NRAS-mutant melanoma, and for this reason, a new drug application for binimetinib was withdrawn in 2017.
Checkpoint inhibitor immunotherapy
Since the 1990s, researchers have identified several important checkpoint molecules in cytotoxic T-lymphocytes and have elucidated their role in suppression of T-cells. The most understood checkpoint molecules are the cytotoxic T lymphocyte antigen-4 (CTLA-4) and programmed cell death-1 (PD-1) receptors, and development of antibodies against these checkpoint receptors has dramatically changed the treatment for advanced melanoma (Table 3).
Anti CTLA-4 antibody therapy
CTLA-4 is a component of the CD28:B7 immunoglobulin family, and it is an important checkpoint molecule, which suppresses T cell activation to prevent autoimmunity and allows tolerance to self-antigens [43]. Ipilimumab, a monoclonal anti CTLA-4 antibody, blocks binding of CTLA-4 to its ligand, B7 protein, in antigen-presenting cells (i.e. dendritic cells), resulting in activation and proliferation of cytotoxic T cells and ultimately leading to antitumor immune response [43]. In a pivotal phase III study, in which 676 patients with unresectable stage III or IV melanoma (HLA-A2 positive) were randomized to receive ipilimumab, gp100 peptide vaccine, or a combination of ipilimumab and gp100 vaccine, patients treated with ipilimumab (or the combination) had superior overall survival and PFS duration as compared to those treated with gp100 vaccine [44]. The median overall survival duration was 10.0 months for patients who received ipilimumab (95% CI 8.5–11.5) in contrast to 6.4 months (95% CI 5.5–8.7) among patients who received gp100 alone (HR for OS, 0.68; p < 0.001) [40]. A 36% reduction in risk of disease progression was observed with ipilimumab treatment alone as compared with gp100 alone (HR 0.64, p < 0.001). This positive survival data led to FDA approval of ipilimumab at 3 mg/kg for the treatment of advanced melanoma in 2011. The clinical benefit of ipilimumab can be durable. A meta-analysis of 1861 melanoma patients treated with ipilimumab in various clinical trials demonstrated that 22% of patients were alive at 3 years, and a vast majority of those who were alive at 3 years were still alive at 5 years and beyond [45].
However, treating physicians and patients must be aware of potentially severe immune-related toxicity associated with ipilimumab treatment. The common immune-related adverse events include dermatitis, colitis, hepatitis, endocrinopathy and neuropathy, and grade 3 or 4 immune-related toxicity occurs in 15–28% of patients treated with ipilimumab [44, 46, 47]. If a patient develops severe immune-related toxicity, it is essential to treat promptly with a high-dose steroid, as death has been reported as a consequence of toxicity, resulting from adverse effects such as Guillain–Barre syndrome and bowel perforation secondary to colitis [48].
Anti-PD-1 antibody therapy
Presence of the PD-1 receptor is essential in immune regulation. PD-1 binds to its ligands, PD-L1 and PD-L2, resulting in suppression of cytotoxic T lymphocytes. Accordingly, anti PD-1 antibodies have shown promising preclinical antitumor activity by interfering with this PD-1 receptor/ligand binding [49,50,51].
Nivolumab is a human IgG4 monoclonal antibody against the PD-1 receptor, and it blocks the binding of PD-1 to its ligands, PD-L1 and PD-L2. In a randomized phase III study, 418 previously untreated patients with metastatic BRAF wild type melanoma were assigned to receive either nivolumab (3 mg/kg every 2 weeks) or chemotherapy [52]. With 16.7 months of follow-up, patient who were treated with nivolumab had a longer OS (HR 0.42 [95% CI 0.25–0.73]; p < 0.001) and PFS (HR 0.43 [95% CI 0.34–0.56]; p < 0.001) than those treated with chemotherapy. Twelve-month OS rates were 72.9 and 42.1% in the nivolumab group and the dacarbazine group, respectively. The overall response rate of nivolumab was 40.0%. In another phase III study, the response rate for nivolumab was 31.7% among 120 melanoma patients whose disease had progressed after anti CTLA-4 antibody therapy, once again higher than found with cytotoxic chemotherapy (10.6%) [6].
Pembrolizumab is another monoclonal anti PD-1 antibody. A randomized phase II clinical trial compared the clinical activity of pembrolizumab (2 or 10 mg/kg every 3 weeks) with that of chemotherapy in patients with ipilimumab-refractory metastatic melanoma [7]. This study showed that patients who received either dose of pembrolizumab had a longer PFS than those who were treated with chemotherapy (HR with 2 mg/kg pembrolizumab 0.57 [95% CI 0.45–0.73]; p < 0.0001). In addition, a higher overall response rate was noted in the pembrolizumab group than the chemotherapy group (21 vs. 4%). In another phase III study of 834 previously untreated patients with advanced melanoma who were randomized to either pembrolizumab (given at 1 of 2 different dosing schedules) or ipilimumab, patients in the pembrolizumab group had longer OS and PFS over ipilimumab [46]. The hazard ratios for OS and PFS were 0.69 (95% CI 0.52–0.90; p = 0.0036) and 0.69 (95% CI 0.52–0.90; p = 0.0036), respectively, favoring pembrolizumab (2 mg/kg every 3 week dosing) over ipilimumab. The two dosing schedules of pembrolizumab, every 2 weeks or every 3 weeks, showed similar results in both PFS and OS.
Anti PD-1 antibody therapies are well tolerated. The safety profiles of nivolumab and pembrolizumab are more favorable than either chemotherapy or ipilimumab [6, 7, 46, 52]. Grade 3 or 4 immune-related toxicity, including colitis, dermatitis, hepatitis and endocrinopathy, occurs in approximately 12% of patients, and less than 7% of patients require treatment discontinuation due to the toxicity [6, 7, 46, 52]. In 2014, both nivolumab and pembrolizumab were approved by the FDA for the treatment of metastatic or unresectable advanced melanoma regardless of BRAF mutation status.
Combination therapy with PD-1 inhibitor and CTLA 4 inhibitor
In preclinical mouse models, the combination of CTLA-4 and PD-1 blockade appeared to lead to synergistic antitumor activity, leading to clinical development of this combination therapy [53, 54]. In a phase I study of the combination of nivolumab and ipilimumab in patients with advanced melanoma, the response rate was 53%, and all patients with a response had tumor reduction of > 80% [55]. This encouraging result promptly led to a randomized phase III study which compared the combination regimen with ipilimumab alone, and also single agent nivolumab with ipilimumab [47]. The study showed that the HR for death with the combination treatment vs ipilimumab alone was 0.55 [98% CI 0.42–0.72] (p < 0.001), indicating a clear OS advantage of the combination regimen. Three-year OS rates were 58 and 34% in the combination group and ipilimumab group, respectively. A median PFS was 11.5 and 2.9 months in the combination treatment group and the ipilimumab group, respectively (HR 0.43 [95% CI 0.35–0.052]; p < 0.001), and a response rate was also higher in the combination treatment arm (58 vs. 19% in the ipilimumab arm) [47]. This study was not designed to directly compare the clinical benefit of the combination regimen and that of nivolumab alone. However, when a descriptive analysis was performed to compare these two treatment arms, there were numerically superior PFS and overall response results with the combination treatment; A HR for risk of progression or death was 0.78 (95% CI 0.64–0.96) (a median PFS of 6.9 months in the nivolumab arm), and an overall response rate for the nivolumab arm was 44%. On the basis of the significant clinical benefit over ipilimumab, the combination of nivolumab and ipilimumab was approved by FDA for the treatment of metastatic melanoma in 2015.
Unfortunately, combination therapy is associated with more severe toxicity. Grade 3 or 4 immune-related adverse events occurred in 59% of patients in the combination group, including increased lipase level (11%), diarrhea (9%), increased alanine aminotransferase level (9%), colitis (8%), and 39% required treatment discontinuation because of the intolerable side effects [47].
Therefore, a treatment decision between single agent anti PD-1 antibody therapy and the combination therapy must be made only after a thorough discussion with the patient regarding both clinical activity and potential severe toxicity.
Talimogene laherparepvec
Talimogene laherparepvec (also called T-VEC or OncoVexGM-CSF) is an oncolytic herpes simplex type 1 virus, which is genetically modified to express granulocyte macrophage colony-stimulating factor (GM-CSF) upon invasion into tumor cells [56]. T-VEC is injected intralesionally to exert the optimal local and systemic immunologic effects. In a phase I/II study of T-VEC, viral replication and GM-CSF expression were observed at the injection sites, confirming its biological effects. Interestingly, tumor regression was observed in the injected lesions as well as in uninjected lesions [57]. In a phase III trial, intralesional T-VEC treatment was compared with subcutaneous injection of recombinant GM-CSF in 436 patients with unresectable or metastatic melanoma who had injectable tumor lesions in the skin or lymph nodes [58]. The results revealed that patients who were treated with T-VEC had a higher durable response rate (16.3 vs. 2.1% of GM-CSF) and overall response rate (26.4 vs. 5.7%). Survival duration in the T-VEC arm was also superior (median OS 23.3 vs. 18.9 months with HR of 0.79 [95% CI 0.62–1.00]; p = 0.051). However, patients with lung or visceral organ metastasis did not benefit from T-VEC treatment. The treatment was well tolerated; fatigue, chills and pyrexia were common (43–50% of the patients), but only 11% of patients who received T-VEC injections experienced grade 3 or 4 treatment-related adverse events, including fatigue, injection site pain, vomiting, and cellulitis. Because of the evidence of durable response rate and the favorable safety profile, T-VEC was approved by the FDA in 2015 for the treatment of melanoma lesions in the skin and lymph nodes, which are not amenable to curative surgical resection.
Systemic therapy for brain metastasis
Historically, melanoma patients with brain metastases have poor outcomes and very limited treatment options. The median survival of patients with brain metastasis is approximately 4 months [59, 60]. Temozolomide had been the systemic therapy of choice for many oncologists for years until recently because of its ability to cross blood brain barrier. However, the clinical response of temozolomoide in the brain is minimal. In a phase II study of temozolomide in patients with brain metastasis, the intracranial response rate was only 7% among 151 treated patients, and a median OS duration was 3.5 months [61].
However, with the development of novel targeted drug therapy and checkpoint inhibitor therapy, there are now more effective therapeutic options. In a phase II study of ipilimumab, 16% of patients (N = 51) with asymptomatic brain metastasis who were not previously treated with steroids had a clinical response [62], and a median OS duration was 7 months. When nivolumab is combined with ipilimumab, a clinical benefit is more obvious. There were two phase II studies examining the clinical activity of combination therapy in melanoma patients with brain metastasis [63], and intracranial response rates ranged from 53 to 56% among the 101 neurologically-asymptomatic patients in the two studies combined. Intracranial complications, such as intracranial hemorrhage or edema, were rarely observed with this regimen.
For patients with V600 BRAF-mutant melanoma with brain metastasis, BRAF inhibitor-based targeted drug therapy is also a great systemic therapeutic option. In a phase II study of dabrafenib, an intracranial response rate was 39.2% among 74 patients with V600E mutant-melanoma, and a median PFS duration was approximately 4 months [64]. More recently, a result of a phase II study of the combination of dabrafenib and trametinib in patients with brain metastasis were published [65]. In this study, among 76 patients with V600E BRAF-mutant asymptomatic brain metastasis, 44 (58%) had an intracranial clinical response, and a median PFS duration was 5.6 months. Similar to the results of the checkpoint inhibitor trials, severe intracranial complications with the combination of dabrafenib and trametinib were rare.
Although these trials have a short follow up duration and overall survival assessment is not available, the results of the combination of nivolumab and ipilimumab, as well as the combination of dabrafenib and trametinib, are very encouraging. Because of the high response rates in the brain, these regimens could be used in conjunction with, or possibly replace, stereotactic radiosurgery as the treatment of choice, especially in patients with concurrent extracranial metastasis.
Adjuvant systemic therapy
Approved by the FDA in 1995, high-dose interferon-alpha-2b had long been the only available treatment option for patients with a high risk of recurrence following surgical lymph node resection/dissection. However, despite early reports of the survival advantage of adjuvant high-dose interferon-alpha treatment over observation in patients with stage III regional nodal metastasis and/or thick primary melanoma (> 4 mm Breslow thickness) [66], a long-term evaluation of the clinical efficacy demonstrated a loss of overall survival benefit of the interferon treatment [67]. In addition, this therapy is associated with significant toxicity, such as flu-like symptoms, severe fatigue and hepatic dysfunction.
In 2011, pegylated interferon-alpha-2b was approved by the FDA on the basis of significant improvement in relapse-free survival over observation in patients with resected stage III melanoma [68]. The reduction in risk of disease recurrence or death was 18% (HR 0.82 [95% CI 0.71–0.96]; p = 0.01). However, overall survival benefit was not observed in patients who were treated with pegylated interferon-alpha-2b compared to those who were observed. Therefore, this treatment has not been widely accepted by medical oncologists and surgeons.
Subsequently, ipilimumab was evaluated for clinical benefit in the adjuvant setting. In a large phase III study of high-dose ipilimumab (10 mg/kg) in patients with stage III melanoma who underwent regional lymph node dissection, 475 patients were treated with ipilimumab, and 476 patients were treated placebo [69]. The treatment schedule of ipilimumab was 10 mg/kg every 3 weeks for 4 doses, followed by once every 3 months for up to 3 years or until disease recurrence or unacceptable toxicity. Recurrence-free survival, the primary endpoint of the trial, was significant longer in the ipilimumab arm (HR 0.76 [95% CI 0.64–0.89]; p < 0.001), and overall survival was also superior (HR 0.72 [95.1% CI 0.58–0.88]; p = 0.001). These positive results led to FDA approval of high-dose ipilimumab as an adjuvant therapy in 2015. Unfortunately, toxicity associated with high-dose ipilimumab is severe; nearly 42% of patients experienced grade 3 or 4 immune-related adverse events, and 1.1% of patients in the ipilimumab arm died due to treatment-induced adverse events.
Most recently, very promising results from a phase III study of nivolumab vs high-dose ipilimumab in an adjuvant setting were published [70]. In a large, randomized, double-blind phase III study, 906 patients with stage IIIB, IIIC and IV melanoma were randomized to receive either nivolumab (3 mg/kg every 2 weeks) or ipilimumab (10 mg/kg every 3 weeks for 4 cycles, followed by 10 mg/kg every 12 weeks) for 1 year following complete lymph node dissection or metastatectomy [70]. Patients in the nivolumab arm had significantly longer recurrence-free survival over those in the ipilimumab arm (HR 0.65 [97.56% CI 0.51–0.83]; p < 0.001), meeting the study’s primary endpoint. A 1-year rate of recurrence-free survival was 70.5% in the nivolumab arm and 60.8% in the ipilimumab arm. The follow-up duration of this study was too short to evaluate the overall survival benefit of nivolumab. As expected, immune-related adverse events were much less frequent with nivolumab treatment; Grade 3 or 4 toxicity occurred in 14.4 and 45.9% of patients who were treated nivolumab and ipilimumab, respectively. Accordingly, a fewer percentage of patients in the nivolumab arm required treatment discontinuation due to the toxicity (9.7 vs. 42.6%). In December of 2017, nivolumab was approved by the FDA for treatment of resected stage III or IV melanoma with high risk for recurrence.
Likewise, pembrolizumab was investigated in an adjuvant setting and showed a significant clinical benefit [71]. A total of 1019 patients with stage IIIA (at least one micrometastasis measuring > 1 mm), IIIB or IIIC melanoma were randomized in a phase III study to either pembrolizumab treatment 200 mg every 3 weeks or placebo for a total of 18 doses after a complete lymph node dissection [71]. Patients who were treated with pembrolizumab had a significantly longer RFS duration (HR 0.57 [98.4% CI 0.43–0.74]; p < 0.001); A RFS rate at 18 months was 71.4% for the pembrolizumab arm and 53.2% for the placebo arm. The clinical benefit was observed regardless of the PD-L1 expression status. Treatment-related grade ≥ 3 adverse events occurred in 14.7% of patients who were treated with pembrolizumab, and 13.0% of patients discontinued treatment due to drug-related toxicity. At the time of this review, the results of the phase III trials of pembrolizumab are under FDA review for potential approval in the treatment of patients with resected melanoma with high-risk for recurrence.
At the same time that the results from the phase III adjuvant nivolumab trial were published, a positive result from another phase III adjuvant study were also published. In this large, double-blind, randomized study, 870 patients with stage IIIA (> 1 mm metastatic tumor load)—IIIC V600E or V600K BRAF-mutant melanoma were treated for 1 year with either a combination of dabrafenib (150 mg twice a day) and trametinib (2 mg a day) or placebo [72]. The primary endpoint was relapse-free survival. At the time of the analysis, patients in the combination treatment arm had significantly longer relapse-free survival compared with those with the placebo arm (HR 0.47; [95% CI 0.39–0.58]; p < 0.001). In addition, 3-year overall survival rate was superior in the treatment group (86 vs. 77%, HR 0.57; [95% CI 0.42–0.79]; p = 0.0006). In April of 2018, the FDA approved the combination of dabrafenib and trametinib for treatment of resected stage III V600 BRAF-mutant melanoma with high risk for recurrence.
In another phase III adjuvant study of a BRAF-targeting drug, 498 patients with stage IIC or III melanoma were randomized to receive either 960 mg vemurafenib twice a day or placebo for 1 year after complete melanoma resection and for a stage III disease, lymph node dissection [73]. The study failed to meet the primary objective of prolongation of disease-free survival (DFS) with vemurafenib treatment in patients with stage IIIC melanoma (cohort 2) (HR 0.80 [95% CI 0.54–1.18]; p = 0.2598), but in patients with stage IIC-IIIB (cohort 1), there was significant improvement in DFS duration in the vemurafenib arm (HR 0.54 [95% CI 0.37–0.78]; p = 0.001). However, because of the study’s original statistical design which prespecified a hierarchical analysis of cohort 2 data prior to cohort 1, the study was deemed negative, and vemurafenib is not a standard treatment as an adjuvant therapy.
Experimental novel therapeutic approaches
Indoleamine 2,3-dioxygenase inhibitor
Indoleamine 2,3-dioxygenase (IDO) is a catalytic enzyme which converts L-tryptophan to N-formylkynurenine. It has been shown to limit T cell function and mediate immune tolerance [74]. Accordingly, inhibition of the IDO enzyme has been shown to synergize the anti-tumor effect of checkpoint inhibitors. In a phase I/II study of the combination of an IDO inhibitor, epacadostat, and nivolumab, 25 of 40 patients (63%) with metastatic melanoma had an objective response. In a phase II study of another IDO inhibitor, indoximod, in combination with pembrolizumab, 31 of 51 patients (61%) with advanced melanoma had a clinical response, including 10 (20%) with a complete response, and a median PFS duration was 12.9 months [75]. Despite the promising results in the early phase clinical trials, however, a phase III study of the combination of pembrolizumab and epacadostat failed to demonstrate improvement in PFS duration over pembrolizumab alone in patients with advanced melanoma in the first-line treatment setting. As a result, a future of IDO inhibitor treatment in advanced melanoma is not clear.
Adoptive T cell therapy
Adoptive T cell therapy (ACT) aims to maximize the cytotoxic immune response against tumor cells via the reintroduction of either patient-derived or genetically engineered tumor infiltrating T cells. Adoptive tumor infiltrating lymphocytes (TIL) transfer therapy, which utilizes autologous tumor reactive T cells harvested from a patient’s own tumor lesion, is administered after lymphodepletion chemotherapy and is followed by high-dose IL-2 therapy. Clinical experience with this approach is encouraging; clinical response rates of nearly 50% have been reported, and a majority of these responses are durable [76, 77]. Unfortunately, TIL isolation and expansion are labor intensive, and only a limited number of academic centers are capable of managing the TIL preparation and administration. Ongoing collaborations between academic institutions and the biopharmaceutical industry will likely make this treatment more widely available.
Combination of BRAF/MEK inhibitor and checkpoint inhibitor
For patients with advanced V600 BRAF mutant-melanoma, combinations of a BRAF inhibitor and a MEK inhibitor generally have higher response rates than checkpoint inhibitor therapy, but it appears that clinical responses may be more durable with checkpoint inhibitor therapy. Therefore, it has been widely speculated whether a combination of targeted drug therapy and checkpoint inhibitor therapy could improve durable response rates and lead to prolonged patient survival.
In addition to inducing constitutive activation of the MAP kinase signaling pathway, a V600 BRAF mutation plays a significant role in immune escape, and inhibition of this mutation can enhance CD8 + T cell-mediated cytotoxicity, especially when T cells are further stimulated with the checkpoint inhibitor [78,79,80]. In a phase I study of atezolizumab (anti PD-L1 antibody) in combination with vemuraenib and cobimetinib, the safety profile of the triple combination was acceptable, and 29 of 34 treated patients (85%) had a clinical response (confirmed and unconfirmed combined) [81]. At this time, there are at least 2 ongoing phase III studies comparing the clinical benefit of a triple combination, BRAF inhibitor, MEK inhibitor and checkpoint inhibitor, to the benefit of a BRAF inhibitor and MEK inhibitor combination alone (Table 4), and the results of these studies are eagerly anticipated.
Molecular biomarkers for melanoma
A number of tumor-based biomarkers have been evaluated and validated as prognostic and predictive biomarkers for melanoma. Examples of widely accepted prognostic biomarkers for primary melanoma which are already included in the AJCC staging system include certain distinct tumor characteristics, such as Breslow thickness, presence of ulceration, mitotic rate and presence of nodal metastasis. Likewise, the presence of somatic mutations in the tumor can be a prognostic biomarker. Patients with melanoma harboring either a V600 BRAF or a NRAS mutation, for example, have a more aggressive disease course and a poor prognosis unless they are treated with effective systemic therapy [41, 82]. In addition, the V600 BRAF mutation is also an excellent predictive biomarker for clinical response to BRAF inhibitors and MEK inhibitors as described above [4, 5, 25]. Recently, there have been great strides made in the discovery of novel predictive or prognostic biomarkers.
Patients with stage I or II melanoma generally have an excellent prognosis, with a 5 year overall survival rate of ≥ 90% [83]. However, it is difficult to foresee who among those patients with early stage melanoma will develop recurrence and die of disease. The quantitative reverse transcription polymerase chain reaction (PCR)-based 31-gene expression profile (GEP) analysis was evaluated as a potential biomarker for high recurrence risk [84,85,86]. In this analysis, RNA is isolated from formalin-fixed paraffin-embedded cutaneous melanoma specimens and converted to complementary DNA (cDNA), with which 31 gene targets are tested. The analysis stratifies the molecular profiles into 2 classes: class I with a low risk for recurrence and class II with a higher risk for recurrence. In retrospective multicenter studies, the 31-gene signature was prognostic in patients with cutaneous melanoma, and metastatic risk was predicted with relatively high accuracy. When multivariate analyses of known prognostic factors, including those currently in the AJCC staging system, were performed, the GEP expression profile was one of the most significant prognostic factors, along with Breslow thickness, mitotic rates and presence of ulceration in patients with stage I or II melanoma [84,85,86]. Similarly, in an analysis of 322 patients with cutaneous melanoma in two prospective registry studies using the 31-gene GEP expression profile, 1.5 year RFS rates were 97 and 77%, 1.5 year DFMS rates were 99 and 89%, and 1.5 year OS rates were 99 and 92% among those with class I and class II molecular profiles, respectively (p < 0.0001 for each) [86]. Although initial limited data suggests that the GEP signature can accurately predicts the risk for recurrence and distant metastasis, the additive value of this analysis in clinical practice is an open question at this time. If long-term follow-up studies with larger numbers of patients demonstrate a similar degree of the positive prognostic stratification, the GEP expression profile may have a significant clinical impact.
Another important recent development is analysis of circulating free tumor-derived DNA (ctDNA) for prognostic and predictive biomarkers for clinical response. ctDNA is released as a result of cell apoptosis or necrosis during the high tumor cell turnover, and can provide genetic information on the tumor in real time. It is less invasive to obtain samples for ctDNA analysis, since this involves a blood draw rather than the tumor biopsy or surgical resection required for tumor genetic sequencing analysis. ctDNA analysis can also detect genetic heterogeneity when there is more than one progressing tumor clone in a patient. In melanoma, plasma ctDNA level has been shown to be associated with a clinical response to BRAF inhibitor therapy and immunotherapy, including anti PD-1 antibody therapies, in small series of retrospective analyses [87,88,89,90]. In addition, ctDNA levels may indicate tumor burden, because a larger tumor volume or a higher number of metastatic foci are likely to result in increased shedding of ctDNA into the blood stream. ctDNA level was found to be more predictive of tumor volume compared to other potential serological biomarkers, such as LDH, S100 calcium-binding protein B (S100B) and melanoma inhibitory activity (MIA) [90,91,92]. Accordingly, ctDNA levels have shown to be correlated with radiographic measures of tumor response to targeted drug therapy [87, 90]. Furthermore, ctDNA analyses can theoretically be used to elucidate mechanisms of resistance to targeted therapy by detecting new genetic mutations which are developed during the course of therapy [90]. Thus far, the clinical utility of ctDNA analysis in patients with metastatic melanoma has not been widely accepted, due to the lack of large, prospective studies. Therefore, prospective clinical trials evaluating ctDNA as a prognostic and predictive biomarker for melanoma are highly desired.
Conclusion
Within the past decade, great advances have been made in the development of novel targeted drug and checkpoint inhibitor treatments for patients with advanced melanoma. As a result, patients with advanced melanoma are now living longer than ever; however, a majority of patients with metastatic or unresectable melanoma still do not survive longer than 5 years. Further, many of the current therapies come with significant toxicity. Therefore, there is still a critical unmet need for more effective and better tolerated therapy regimens which both increase the survival and cure rate and improve the quality of life for these patients. There are many ongoing preclinical and clinical investigations to search for new actionable drug targets, identify suitable predictive biomarkers for therapeutic efficacy, and optimize the sequence or concurrent combination of promising drugs. These research efforts will surely reshape the systemic therapy landscape in melanoma in the coming years.
References
Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67(1):7–30. https://doi.org/10.3322/caac.21387
Howlader N, Noone A, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (2015) SEER cancer statistics review, 1975–2012. National Cancer Institute, Bethesda
Balch CM, Gershenwald JE, Soong SJ, Thompson JF, Atkins MB, Byrd DR, Buzaid AC, Cochran AJ, Coit DG, Ding S, Eggermont AM, Flaherty KT, Gimotty PA, Kirkwood JM, McMasters KM, Mihm MC Jr, Morton DL, Ross MI, Sober AJ, Sondak VK (2009) Final version of 2009 AJCC melanoma staging and classification. J Clin Oncol 27(36):6199–6206. https://doi.org/10.1200/JCO.2009.23.4799
Chapman PB, Hauschild A, Robert C, Haanen JB, Ascierto P, Larkin J, Dummer R, Garbe C, Testori A, Maio M, Hogg D, Lorigan P, Lebbe C, Jouary T, Schadendorf D, Ribas A, O’Day SJ, Sosman JA, Kirkwood JM, Eggermont AM, Dreno B, Nolop K, Li J, Nelson B, Hou J, Lee RJ, Flaherty KT, McArthur GA, Group B-S (2011) Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med 364(26):2507–2516. https://doi.org/10.1056/NEJMoa1103782
Hauschild A, Grob JJ, Demidov LV, Jouary T, Gutzmer R, Millward M, Rutkowski P, Blank CU, Miller WH Jr, Kaempgen E, Martin-Algarra S, Karaszewska B, Mauch C, Chiarion-Sileni V, Martin AM, Swann S, Haney P, Mirakhur B, Guckert ME, Goodman V, Chapman PB (2012) Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet 380(9839):358–365. https://doi.org/10.1016/S0140-6736(12)60868-X
Weber JS, D’Angelo SP, Minor D, Hodi FS, Gutzmer R, Neyns B, Hoeller C, Khushalani NI, Miller WH Jr, Lao CD, Linette GP, Thomas L, Lorigan P, Grossmann KF, Hassel JC, Maio M, Sznol M, Ascierto PA, Mohr P, Chmielowski B, Bryce A, Svane IM, Grob JJ, Krackhardt AM, Horak C, Lambert A, Yang AS, Larkin J (2015) Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 16(4):375–384. https://doi.org/10.1016/S1470-2045(15)70076-8
Ribas A, Puzanov I, Dummer R, Schadendorf D, Hamid O, Robert C, Hodi FS, Schachter J, Pavlick AC, Lewis KD, Cranmer LD, Blank CU, O’Day SJ, Ascierto PA, Salama AK, Margolin KA, Loquai C, Eigentler TK, Gangadhar TC, Carlino MS, Agarwala SS, Moschos SJ, Sosman JA, Goldinger SM, Shapira-Frommer R, Gonzalez R, Kirkwood JM, Wolchok JD, Eggermont A, Li XN, Zhou W, Zernhelt AM, Lis J, Ebbinghaus S, Kang SP, Daud A (2015) Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol 16(8):908–918. https://doi.org/10.1016/S1470-2045(15)00083-2
Bajetta E, Del Vecchio M, Bernard-Marty C, Vitali M, Buzzoni R, Rixe O, Nova P, Aglione S, Taillibert S, Khayat D (2002) Metastatic melanoma: chemotherapy. Semin Oncol 29(5):427–445
Chapman PB, Einhorn LH, Meyers ML, Saxman S, Destro AN, Panageas KS, Begg CB, Agarwala SS, Schuchter LM, Ernstoff MS, Houghton AN, Kirkwood JM (1999) Phase III multicenter randomized trial of the Dartmouth regimen versus dacarbazine in patients with metastatic melanoma. J Clin Oncol 17(9):2745–2751. https://doi.org/10.1200/JCO.1999.17.9.2745
Rosenberg SA, Yang JC, Schwartzentruber DJ, Hwu P, Marincola FM, Topalian SL, Seipp CA, Einhorn JH, White DE, Steinberg SM (1999) Prospective randomized trial of the treatment of patients with metastatic melanoma using chemotherapy with cisplatin, dacarbazine, and tamoxifen alone or in combination with interleukin-2 and interferon alfa-2b. J Clin Oncol 17(3):968–975. https://doi.org/10.1200/JCO.1999.17.3.968
Eton O, Legha SS, Bedikian AY, Lee JJ, Buzaid AC, Hodges C, Ring SE, Papadopoulos NE, Plager C, East MJ, Zhan F, Benjamin RS (2002) Sequential biochemotherapy versus chemotherapy for metastatic melanoma: results from a phase III randomized trial. J Clin Oncol 20(8):2045–2052. https://doi.org/10.1200/JCO.2002.07.044
Atkins MB, Kunkel L, Sznol M, Rosenberg SA (2000) High-dose recombinant interleukin-2 therapy in patients with metastatic melanoma: long-term survival update. Cancer J Sci Am 6(Suppl 1):S11–S14
Atkins MB, Lotze MT, Dutcher JP, Fisher RI, Weiss G, Margolin K, Abrams J, Sznol M, Parkinson D, Hawkins M, Paradise C, Kunkel L, Rosenberg SA (1999) High-dose recombinant interleukin 2 therapy for patients with metastatic melanoma: analysis of 270 patients treated between 1985 and 1993. J Clin Oncol 17(7):2105–2116. https://doi.org/10.1200/JCO.1999.17.7.2105
Hodis E, Watson IR, Kryukov GV, Arold ST, Imielinski M, Theurillat JP, Nickerson E, Auclair D, Li L, Place C, Dicara D, Ramos AH, Lawrence MS, Cibulskis K, Sivachenko A, Voet D, Saksena G, Stransky N, Onofrio RC, Winckler W, Ardlie K, Wagle N, Wargo J, Chong K, Morton DL, Stemke-Hale K, Chen G, Noble M, Meyerson M, Ladbury JE, Davies MA, Gershenwald JE, Wagner SN, Hoon DS, Schadendorf D, Lander ES, Gabriel SB, Getz G, Garraway LA, Chin L (2012) A landscape of driver mutations in melanoma. Cell 150(2):251–263. https://doi.org/10.1016/j.cell.2012.06.024
Tsao H, Zhang X, Fowlkes K, Haluska FG (2000) Relative reciprocity of NRAS and PTEN/MMAC1 alterations in cutaneous melanoma cell lines. Cancer Res 60(7):1800–1804
Curtin JA, Busam K, Pinkel D, Bastian BC (2006) Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol 24(26):4340–4346. https://doi.org/10.1200/JCO.2006.06.2984
Van Raamsdonk CD, Bezrookove V, Green G, Bauer J, Gaugler L, O’Brien JM, Simpson EM, Barsh GS, Bastian BC (2009) Frequent somatic mutations of GNAQ in uveal melanoma and blue naevi. Nature 457(7229):599–602. https://doi.org/10.1038/nature07586
Van Raamsdonk CD, Griewank KG, Crosby MB, Garrido MC, Vemula S, Wiesner T, Obenauf AC, Wackernagel W, Green G, Bouvier N, Sozen MM, Baimukanova G, Roy R, Heguy A, Dolgalev I, Khanin R, Busam K, Speicher MR, O’Brien J, Bastian BC (2010) Mutations in GNA11 in uveal melanoma. N Engl J Med 363(23):2191–2199. https://doi.org/10.1056/NEJMoa1000584
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, Davis N, Dicks E, Ewing R, Floyd Y, Gray K, Hall S, Hawes R, Hughes J, Kosmidou V, Menzies A, Mould C, Parker A, Stevens C, Watt S, Hooper S, Wilson R, Jayatilake H, Gusterson BA, Cooper C, Shipley J, Hargrave D, Pritchard-Jones K, Maitland N, Chenevix-Trench G, Riggins GJ, Bigner DD, Palmieri G, Cossu A, Flanagan A, Nicholson A, Ho JW, Leung SY, Yuen ST, Weber BL, Seigler HF, Darrow TL, Paterson H, Marais R, Marshall CJ, Wooster R, Stratton MR, Futreal PA (2002) Mutations of the BRAF gene in human cancer. Nature 417(6892):949–954. https://doi.org/10.1038/nature00766
Flaherty KT, Puzanov I, Kim KB, Ribas A, McArthur GA, Sosman JA, O’Dwyer PJ, Lee RJ, Grippo JF, Nolop K, Chapman PB (2010) Inhibition of mutated, activated BRAF in metastatic melanoma. N Engl J Med 363(9):809–819. https://doi.org/10.1056/NEJMoa1002011
McArthur GA, Chapman PB, Robert C, Larkin J, Haanen JB, Dummer R, Ribas A, Hogg D, Hamid O, Ascierto PA, Garbe C, Testori A, Maio M, Lorigan P, Lebbe C, Jouary T, Schadendorf D, O’Day SJ, Kirkwood JM, Eggermont AM, Dreno B, Sosman JA, Flaherty KT, Yin M, Caro I, Cheng S, Trunzer K, Hauschild A (2014) Safety and efficacy of vemurafenib in BRAF(V600E) and BRAF(V600K) mutation-positive melanoma (BRIM-3): extended follow-up of a phase 3, randomised, open-label study. Lancet Oncol 15(3):323–332. https://doi.org/10.1016/S1470-2045(14)70012-9
Salama AK, Kim KB (2013) MEK inhibition in the treatment of advanced melanoma. Curr Oncol Rep 15(5):473–482. https://doi.org/10.1007/s11912-013-0336-2
Falchook GS, Lewis KD, Infante JR, Gordon MS, Vogelzang NJ, DeMarini DJ, Sun P, Moy C, Szabo SA, Roadcap LT, Peddareddigari VG, Lebowitz PF, Le NT, Burris HA 3rd, Messersmith WA, O’Dwyer PJ, Kim KB, Flaherty K, Bendell JC, Gonzalez R, Kurzrock R, Fecher LA (2012) Activity of the oral MEK inhibitor trametinib in patients with advanced melanoma: a phase 1 dose-escalation trial. Lancet Oncol 13(8):782–789. https://doi.org/10.1016/S1470-2045(12)70269-3
Kim KB, Kefford R, Pavlick AC, Infante JR, Ribas A, Sosman JA, Fecher LA, Millward M, McArthur GA, Hwu P, Gonzalez R, Ott PA, Long GV, Gardner OS, Ouellet D, Xu Y, DeMarini DJ, Le NT, Patel K, Lewis KD (2013) Phase II study of the MEK1/MEK2 inhibitor Trametinib in patients with metastatic BRAF-mutant cutaneous melanoma previously treated with or without a BRAF inhibitor. J Clin Oncol 31(4):482–489. https://doi.org/10.1200/JCO.2012.43.5966
Flaherty KT, Robert C, Hersey P, Nathan P, Garbe C, Milhem M, Demidov LV, Hassel JC, Rutkowski P, Mohr P, Dummer R, Trefzer U, Larkin JM, Utikal J, Dreno B, Nyakas M, Middleton MR, Becker JC, Casey M, Sherman LJ, Wu FS, Ouellet D, Martin AM, Patel K, Schadendorf D, Group MS (2012) Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med 367(2):107–114. https://doi.org/10.1056/NEJMoa1203421
Nazarian R, Shi H, Wang Q, Kong X, Koya RC, Lee H, Chen Z, Lee MK, Attar N, Sazegar H, Chodon T, Nelson SF, McArthur G, Sosman JA, Ribas A, Lo RS (2010) Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature 468(7326):973–977. https://doi.org/10.1038/nature09626
Emery CM, Vijayendran KG, Zipser MC, Sawyer AM, Niu L, Kim JJ, Hatton C, Chopra R, Oberholzer PA, Karpova MB, MacConaill LE, Zhang J, Gray NS, Sellers WR, Dummer R, Garraway LA (2009) MEK1 mutations confer resistance to MEK and B-RAF inhibition. Proc Natl Acad Sci USA 106(48):20411–20416. https://doi.org/10.1073/pnas.0905833106
Johannessen CM, Boehm JS, Kim SY, Thomas SR, Wardwell L, Johnson LA, Emery CM, Stransky N, Cogdill AP, Barretina J, Caponigro G, Hieronymus H, Murray RR, Salehi-Ashtiani K, Hill DE, Vidal M, Zhao JJ, Yang X, Alkan O, Kim S, Harris JL, Wilson CJ, Myer VE, Finan PM, Root DE, Roberts TM, Golub T, Flaherty KT, Dummer R, Weber BL, Sellers WR, Schlegel R, Wargo JA, Hahn WC, Garraway LA (2010) COT drives resistance to RAF inhibition through MAP kinase pathway reactivation. Nature 468(7326):968–972. https://doi.org/10.1038/nature09627
Poulikakos PI, Persaud Y, Janakiraman M, Kong X, Ng C, Moriceau G, Shi H, Atefi M, Titz B, Gabay MT, Salton M, Dahlman KB, Tadi M, Wargo JA, Flaherty KT, Kelley MC, Misteli T, Chapman PB, Sosman JA, Graeber TG, Ribas A, Lo RS, Rosen N, Solit DB (2011) RAF inhibitor resistance is mediated by dimerization of aberrantly spliced BRAF(V600E). Nature 480(7377):387–390. https://doi.org/10.1038/nature10662
Trunzer K, Pavlick AC, Schuchter L, Gonzalez R, McArthur GA, Hutson TE, Moschos SJ, Flaherty KT, Kim KB, Weber JS, Hersey P, Long GV, Lawrence D, Ott PA, Amaravadi RK, Lewis KD, Puzanov I, Lo RS, Koehler A, Kockx M, Spleiss O, Schell-Steven A, Gilbert HN, Cockey L, Bollag G, Lee RJ, Joe AK, Sosman JA, Ribas A (2013) Pharmacodynamic effects and mechanisms of resistance to vemurafenib in patients with metastatic melanoma. J Clin Oncol 31(14):1767–1774. https://doi.org/10.1200/JCO.2012.44.7888
Long GV, Stroyakovskiy D, Gogas H, Levchenko E, de Braud F, Larkin J, Garbe C, Jouary T, Hauschild A, Grob JJ, Chiarion-Sileni V, Lebbe C, Mandala M, Millward M, Arance A, Bondarenko I, Haanen JB, Hansson J, Utikal J, Ferraresi V, Kovalenko N, Mohr P, Probachai V, Schadendorf D, Nathan P, Robert C, Ribas A, DeMarini DJ, Irani JG, Swann S, Legos JJ, Jin F, Mookerjee B, Flaherty K (2015) Dabrafenib and trametinib versus dabrafenib and placebo for Val600 BRAF-mutant melanoma: a multicentre, double-blind, phase 3 randomised controlled trial. Lancet 386(9992):444–451. https://doi.org/10.1016/S0140-6736(15)60898-4
Robert C, Karaszewska B, Schachter J, Rutkowski P, Mackiewicz A, Stroiakovski D, Lichinitser M, Dummer R, Grange F, Mortier L, Chiarion-Sileni V, Drucis K, Krajsova I, Hauschild A, Lorigan P, Wolter P, Long GV, Flaherty K, Nathan P, Ribas A, Martin AM, Sun P, Crist W, Legos J, Rubin SD, Little SM, Schadendorf D (2015) Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med 372(1):30–39. https://doi.org/10.1056/NEJMoa1412690
Larkin J, Ascierto PA, Dreno B, Atkinson V, Liszkay G, Maio M, Mandala M, Demidov L, Stroyakovskiy D, Thomas L, de la Cruz-Merino L, Dutriaux C, Garbe C, Sovak MA, Chang I, Choong N, Hack SP, McArthur GA, Ribas A (2014) Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. N Engl J Med 371(20):1867–1876. https://doi.org/10.1056/NEJMoa1408868
Dummer R, Ascierto PA, Gogas HJ, Arance A, Mandala M, Liszkay G, Garbe C, Schadendorf D, Krajsova I, Gutzmer R, Chiarion-Sileni V, Dutriaux C, de Groot JWB, Yamazaki N, Loquai C, Moutouh-de Parseval LA, Pickard MD, Sandor V, Robert C, Flaherty KT (2018) Encorafenib plus binimetinib versus vemurafenib or encorafenib in patients with BRAF-mutant melanoma (COLUMBUS): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol 19(5):603–615. https://doi.org/10.1016/S1470-2045(18)30142-6
Garrido MC, Bastian BC (2010) KIT as a therapeutic target in melanoma. J Invest Dermatol 130(1):20–27. https://doi.org/10.1038/jid.2009.334
Carvajal RD, Antonescu CR, Wolchok JD, Chapman PB, Roman RA, Teitcher J, Panageas KS, Busam KJ, Chmielowski B, Lutzky J, Pavlick AC, Fusco A, Cane L, Takebe N, Vemula S, Bouvier N, Bastian BC, Schwartz GK (2011) KIT as a therapeutic target in metastatic melanoma. JAMA 305(22):2327–2334. https://doi.org/10.1001/jama.2011.746
Guo J, Si L, Kong Y, Flaherty KT, Xu X, Zhu Y, Corless CL, Li L, Li H, Sheng X, Cui C, Chi Z, Li S, Han M, Mao L, Lin X, Du N, Zhang X, Li J, Wang B, Qin S (2011) Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol 29(21):2904–2909. https://doi.org/10.1200/JCO.2010.33.9275
Hodi FS, Corless CL, Giobbie-Hurder A, Fletcher JA, Zhu M, Marino-Enriquez A, Friedlander P, Gonzalez R, Weber JS, Gajewski TF, O’Day SJ, Kim KB, Lawrence D, Flaherty KT, Luke JJ, Collichio FA, Ernstoff MS, Heinrich MC, Beadling C, Zukotynski KA, Yap JT, Van den Abbeele AD, Demetri GD, Fisher DE (2013) Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol 31(26):3182–3190. https://doi.org/10.1200/JCO.2012.47.7836
Guo J, Carvajal RD, Dummer R, Hauschild A, Daud A, Bastian BC, Markovic SN, Queirolo P, Arance A, Berking C, Camargo V, Herchenhorn D, Petrella TM, Schadendorf D, Sharfman W, Testori A, Novick S, Hertle S, Nourry C, Chen Q, Hodi FS (2017) Efficacy and safety of nilotinib in patients with KIT-mutated metastatic or inoperable melanoma: final results from the global, single-arm, phase II TEAM trial. Ann Oncol 28(6):1380–1387. https://doi.org/10.1093/annonc/mdx079
Devitt B, Liu W, Salemi R, Wolfe R, Kelly J, Tzen CY, Dobrovic A, McArthur G (2011) Clinical outcome and pathological features associated with NRAS mutation in cutaneous melanoma. Pigment Cell Melanoma Res 24(4):666–672. https://doi.org/10.1111/j.1755-148X.2011.00873.x
Jakob JA, Bassett RL Jr, Ng CS, Curry JL, Joseph RW, Alvarado GC, Rohlfs ML, Richard J, Gershenwald JE, Kim KB, Lazar AJ, Hwu P, Davies MA (2012) NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer 118(16):4014–4023. https://doi.org/10.1002/cncr.26724
Dummer R, Schadendorf D, Ascierto PA, Arance A, Dutriaux C, Di Giacomo AM, Rutkowski P, Del Vecchio M, Gutzmer R, Mandala M, Thomas L, Demidov L, Garbe C, Hogg D, Liszkay G, Queirolo P, Wasserman E, Ford J, Weill M, Sirulnik LA, Jehl V, Bozon V, Long GV, Flaherty K (2017) Binimetinib versus dacarbazine in patients with advanced NRAS-mutant melanoma (NEMO): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 18(4):435–445. https://doi.org/10.1016/S1470-2045(17)30180-8
Peggs KS, Quezada SA, Korman AJ, Allison JP (2006) Principles and use of anti-CTLA4 antibody in human cancer immunotherapy. Curr Opin Immunol 18(2):206–213. https://doi.org/10.1016/j.coi.2006.01.011
Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, Gonzalez R, Robert C, Schadendorf D, Hassel JC, Akerley W, van den Eertwegh AJ, Lutzky J, Lorigan P, Vaubel JM, Linette GP, Hogg D, Ottensmeier CH, Lebbe C, Peschel C, Quirt I, Clark JI, Wolchok JD, Weber JS, Tian J, Yellin MJ, Nichol GM, Hoos A, Urba WJ (2010) Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med 363(8):711–723. https://doi.org/10.1056/NEJMoa1003466
Schadendorf D, Hodi FS, Robert C, Weber JS, Margolin K, Hamid O, Patt D, Chen TT, Berman DM, Wolchok JD (2015) Pooled analysis of long-term survival data from phase II and phase III trials of Ipilimumab in unresectable or metastatic melanoma. J Clin Oncol 33(17):1889–1894. https://doi.org/10.1200/JCO.2014.56.2736
Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, Daud A, Carlino MS, McNeil C, Lotem M, Larkin J, Lorigan P, Neyns B, Blank CU, Hamid O, Mateus C, Shapira-Frommer R, Kosh M, Zhou H, Ibrahim N, Ebbinghaus S, Ribas A, investigators K- (2015) Pembrolizumab versus Ipilimumab in Advanced Melanoma. N Engl J Med 372(26):2521–2532. https://doi.org/10.1056/NEJMoa1503093
Wolchok JD, Chiarion-Sileni V, Gonzalez R, Rutkowski P, Grob JJ, Cowey CL, Lao CD, Wagstaff J, Schadendorf D, Ferrucci PF, Smylie M, Dummer R, Hill A, Hogg D, Haanen J, Carlino MS, Bechter O, Maio M, Marquez-Rodas I, Guidoboni M, McArthur G, Lebbe C, Ascierto PA, Long GV, Cebon J, Sosman J, Postow MA, Callahan MK, Walker D, Rollin L, Bhore R, Hodi FS, Larkin J (2017) Overall survival with combined Nivolumab and Ipilimumab in advanced melanoma. N Engl J Med 377(14):1345–1356. https://doi.org/10.1056/NEJMoa1709684
Fecher LA, Agarwala SS, Hodi FS, Weber JS (2013) Ipilimumab and its toxicities: a multidisciplinary approach. Oncologist 18(6):733–743. https://doi.org/10.1634/theoncologist.2012-0483
Nishimura H, Minato N, Nakano T, Honjo T (1998) Immunological studies on PD-1 deficient mice: implication of PD-1 as a negative regulator for B cell responses. Int Immunol 10(10):1563–1572
Dong H, Zhu G, Tamada K, Chen L (1999) B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med 5(12):1365–1369. https://doi.org/10.1038/70932
Freeman GJ, Long AJ, Iwai Y, Bourque K, Chernova T, Nishimura H, Fitz LJ, Malenkovich N, Okazaki T, Byrne MC, Horton HF, Fouser L, Carter L, Ling V, Bowman MR, Carreno BM, Collins M, Wood CR, Honjo T (2000) Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J Exp Med 192(7):1027–1034
Robert C, Long GV, Brady B, Dutriaux C, Maio M, Mortier L, Hassel JC, Rutkowski P, McNeil C, Kalinka-Warzocha E, Savage KJ, Hernberg MM, Lebbe C, Charles J, Mihalcioiu C, Chiarion-Sileni V, Mauch C, Cognetti F, Arance A, Schmidt H, Schadendorf D, Gogas H, Lundgren-Eriksson L, Horak C, Sharkey B, Waxman IM, Atkinson V, Ascierto PA (2015) Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372(4):320–330. https://doi.org/10.1056/NEJMoa1412082
Curran MA, Montalvo W, Yagita H, Allison JP (2010) PD-1 and CTLA-4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci USA 107(9):4275–4280. https://doi.org/10.1073/pnas.0915174107
Duraiswamy J, Kaluza KM, Freeman GJ, Coukos G (2013) Dual blockade of PD-1 and CTLA-4 combined with tumor vaccine effectively restores T-cell rejection function in tumors. Cancer Res 73(12):3591–3603. https://doi.org/10.1158/0008-5472.CAN-12-4100
Wolchok JD, Kluger H, Callahan MK, Postow MA, Rizvi NA, Lesokhin AM, Segal NH, Ariyan CE, Gordon RA, Reed K, Burke MM, Caldwell A, Kronenberg SA, Agunwamba BU, Zhang X, Lowy I, Inzunza HD, Feely W, Horak CE, Hong Q, Korman AJ, Wigginton JM, Gupta A, Sznol M (2013) Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med 369(2):122–133. https://doi.org/10.1056/NEJMoa1302369
Liu BL, Robinson M, Han ZQ, Branston RH, English C, Reay P, McGrath Y, Thomas SK, Thornton M, Bullock P, Love CA, Coffin RS (2003) ICP34.5 deleted herpes simplex virus with enhanced oncolytic, immune stimulating, and anti-tumour properties. Gene Ther 10(4):292–303. https://doi.org/10.1038/sj.gt.3301885
Hu JC, Coffin RS, Davis CJ, Graham NJ, Groves N, Guest PJ, Harrington KJ, James ND, Love CA, McNeish I, Medley LC, Michael A, Nutting CM, Pandha HS, Shorrock CA, Simpson J, Steiner J, Steven NM, Wright D, Coombes RC (2006) A phase I study of OncoVEXGM-CSF, a second-generation oncolytic herpes simplex virus expressing granulocyte macrophage colony-stimulating factor. Clin Cancer Res 12(22):6737–6747. https://doi.org/10.1158/1078-0432.CCR-06-0759
Andtbacka RH, Kaufman HL, Collichio F, Amatruda T, Senzer N, Chesney J, Delman KA, Spitler LE, Puzanov I, Agarwala SS, Milhem M, Cranmer L, Curti B, Lewis K, Ross M, Guthrie T, Linette GP, Daniels GA, Harrington K, Middleton MR, Miller WH Jr, Zager JS, Ye Y, Yao B, Li A, Doleman S, VanderWalde A, Gansert J, Coffin RS (2015) Talimogene Laherparepvec improves durable response rate in patients with advanced melanoma. J Clin Oncol 33(25):2780–2788. https://doi.org/10.1200/JCO.2014.58.3377
Davies MA, Liu P, McIntyre S, Kim KB, Papadopoulos N, Hwu WJ, Hwu P, Bedikian A (2011) Prognostic factors for survival in melanoma patients with brain metastases. Cancer 117(8):1687–1696. https://doi.org/10.1002/cncr.25634
Fife KM, Colman MH, Stevens GN, Firth IC, Moon D, Shannon KF, Harman R, Petersen-Schaefer K, Zacest AC, Besser M, Milton GW, McCarthy WH, Thompson JF (2004) Determinants of outcome in melanoma patients with cerebral metastases. J Clin Oncol 22(7):1293–1300. https://doi.org/10.1200/JCO.2004.08.140
Agarwala SS, Kirkwood JM, Gore M, Dreno B, Thatcher N, Czarnetski B, Atkins M, Buzaid A, Skarlos D, Rankin EM (2004) Temozolomide for the treatment of brain metastases associated with metastatic melanoma: a phase II study. J Clin Oncol 22(11):2101–2107. https://doi.org/10.1200/JCO.2004.11.044
Margolin K, Ernstoff MS, Hamid O, Lawrence D, McDermott D, Puzanov I, Wolchok JD, Clark JI, Sznol M, Logan TF, Richards J, Michener T, Balogh A, Heller KN, Hodi FS (2012) Ipilimumab in patients with melanoma and brain metastases: an open-label, phase 2 trial. Lancet Oncol 13(5):459–465. https://doi.org/10.1016/S1470-2045(12)70090-6
Tawbi HAH, Forsyth PA, Algazi AP, Hamid O, Hodi FS, Moschos SJ, Khushalani NI, Gonzalez R, Lao CD, Postow MA, Atkins MB, Ernstoff MS, Puzanov I, Kudchadkar RR, Thomas RP, Tarhini AA, Jiang J, Avila A, Demelo S, Margolin KA (2017) Efficacy and safety of nivolumab (NIVO) plus ipilimumab (IPI) in patients with melanoma (MEL) metastatic to the brain: results of the phase II study CheckMate 204. J Clin Oncol 35(15_suppl):9507–9507. https://doi.org/10.1200/JCO.2017.35.15_suppl.9507
Long GV, Uwe T, Davies MA, Kefford RF, Ascierto PA, Chapman PB, Puzanov I, Hauschild A, Robert C, Algazi A, Mortier L, Tawbi H, Wilhelm T, Zimmer L, Switzky J, Swann S, Martin A-M, Guckert M, Goodman V, Streit M, Kirkwood JM, Schadendorf D (2012) Dabrafenib in patients with Val600Glu or Val600Lys BRAF-mutant melanoma metastatic to the brain (BREAK-MB): a multicentre, open-label, phase 2 trial. Lancet Oncol 13(11):1087–1095. https://doi.org/10.1016/S1470-2045(12)70431-X
Davies MA, Saiag P, Robert C, Grob JJ, Flaherty KT, Arance A, Chiarion-Sileni V, Thomas L, Lesimple T, Mortier L, Moschos SJ, Hogg D, Marquez-Rodas I, Del Vecchio M, Lebbe C, Meyer N, Zhang Y, Huang Y, Mookerjee B, Long GV (2017) Dabrafenib plus trametinib in patients with BRAFV600-mutant melanoma brain metastases (COMBI-MB): a multicentre, multicohort, open-label, phase 2 trial. Lancet Oncol 18(7):863–873. https://doi.org/10.1016/S1470-2045(17)30429-1
Kirkwood JM, Strawderman MH, Ernstoff MS, Smith TJ, Borden EC, Blum RH (1996) Interferon alfa-2b adjuvant therapy of high-risk resected cutaneous melanoma: the Eastern Cooperative Oncology Group Trial EST 1684. J Clin Oncol 14(1):7–17. https://doi.org/10.1200/JCO.1996.14.1.7
Kirkwood JM, Manola J, Ibrahim J, Sondak V, Ernstoff MS, Rao U, Eastern Cooperative Oncology G (2004) A pooled analysis of eastern cooperative oncology group and intergroup trials of adjuvant high-dose interferon for melanoma. Clin Cancer Res 10(5):1670–1677
Eggermont AM, Suciu S, Santinami M, Testori A, Kruit WH, Marsden J, Punt CJ, Sales F, Gore M, Mackie R, Kusic Z, Dummer R, Hauschild A, Musat E, Spatz A, Keilholz U, Group EM (2008) Adjuvant therapy with pegylated interferon alfa-2b versus observation alone in resected stage III melanoma: final results of EORTC 18991, a randomised phase III trial. Lancet 372(9633):117–126. https://doi.org/10.1016/S0140-6736(08)61033-8
Eggermont AM, Chiarion-Sileni V, Grob JJ, Dummer R, Wolchok JD, Schmidt H, Hamid O, Robert C, Ascierto PA, Richards JM, Lebbe C, Ferraresi V, Smylie M, Weber JS, Maio M, Bastholt L, Mortier L, Thomas L, Tahir S, Hauschild A, Hassel JC, Hodi FS, Taitt C, de Pril V, de Schaetzen G, Suciu S, Testori A (2016) Prolonged survival in stage III melanoma with Ipilimumab adjuvant therapy. N Engl J Med 375(19):1845–1855. https://doi.org/10.1056/NEJMoa1611299
Weber J, Mandala M, Del Vecchio M, Gogas HJ, Arance AM, Cowey CL, Dalle S, Schenker M, Chiarion-Sileni V, Marquez-Rodas I, Grob JJ, Butler MO, Middleton MR, Maio M, Atkinson V, Queirolo P, Gonzalez R, Kudchadkar RR, Smylie M, Meyer N, Mortier L, Atkins MB, Long GV, Bhatia S, Lebbe C, Rutkowski P, Yokota K, Yamazaki N, Kim TM, de Pril V, Sabater J, Qureshi A, Larkin J, Ascierto PA, CheckMate C (2017) Adjuvant Nivolumab versus Ipilimumab in resected stage III or IV melanoma. N Engl J Med 377(19):1824–1835. https://doi.org/10.1056/NEJMoa1709030
Eggermont AMM, Blank CU, Mandala M, Long GV, Atkinson V, Dalle S, Haydon A, Lichinitser M, Khattak A, Carlino MS, Sandhu S, Larkin J, Puig S, Ascierto PA, Rutkowski P, Schadendorf D, Koornstra R, Hernandez-Aya L, Maio M, van den Eertwegh AJM, Grob JJ, Gutzmer R, Jamal R, Lorigan P, Ibrahim N, Marreaud S, van Akkooi ACJ, Suciu S, Robert C (2018) Adjuvant Pembrolizumab versus Placebo in resected stage III melanoma. N Engl J Med 378(19):1789–1801. https://doi.org/10.1056/NEJMoa1802357
Long GV, Hauschild A, Santinami M, Atkinson V, Mandala M, Chiarion-Sileni V, Larkin J, Nyakas M, Dutriaux C, Haydon A, Robert C, Mortier L, Schachter J, Schadendorf D, Lesimple T, Plummer R, Ji R, Zhang P, Mookerjee B, Legos J, Kefford R, Dummer R, Kirkwood JM (2017) Adjuvant Dabrafenib plus Trametinib in stage III BRAF-mutated melanoma. N Engl J Med. https://doi.org/10.1056/NEJMoa1708539
Lewis K, Maio M, Demidov L, Mandala M, Ascierto PA, Herbert C, Mackiewicz A, Rutkowski P, Guminski A, Goodman G, Simmons B, Ye C, Yan Y, Schadendorf D (2017) BRIM8: a randomized, double-blind, placebo-controlled study of adjuvant vemurafenib in patients (pts) with completely resected, BRAFV600 + melanoma at high risk for recurrence. Ann Oncol 28(suppl_5):LBA7_PR
Munn DH, Mellor AL (2013) Indoleamine 2,3 dioxygenase and metabolic control of immune responses. Trends Immunol 34(3):137–143. https://doi.org/10.1016/j.it.2012.10.001
Zakharia Y (2017) Combined inhibition of the IDO and PD-1 pathways improves the response rate for patients with advanced melanoma. CRI-CIMT-EATI-AACR International Cancer Immunotherapy Conference. Mainz, Germany
Dudley ME, Wunderlich JR, Yang JC, Sherry RM, Topalian SL, Restifo NP, Royal RE, Kammula U, White DE, Mavroukakis SA, Rogers LJ, Gracia GJ, Jones SA, Mangiameli DP, Pelletier MM, Gea-Banacloche J, Robinson MR, Berman DM, Filie AC, Abati A, Rosenberg SA (2005) Adoptive cell transfer therapy following non-myeloablative but lymphodepleting chemotherapy for the treatment of patients with refractory metastatic melanoma. J Clin Oncol 23(10):2346–2357. https://doi.org/10.1200/JCO.2005.00.240
Radvanyi LG, Bernatchez C, Zhang M, Fox PS, Miller P, Chacon J, Wu R, Lizee G, Mahoney S, Alvarado G, Glass M, Johnson VE, McMannis JD, Shpall E, Prieto V, Papadopoulos N, Kim K, Homsi J, Bedikian A, Hwu WJ, Patel S, Ross MI, Lee JE, Gershenwald JE, Lucci A, Royal R, Cormier JN, Davies MA, Mansaray R, Fulbright OJ, Toth C, Ramachandran R, Wardell S, Gonzalez A, Hwu P (2012) Specific lymphocyte subsets predict response to adoptive cell therapy using expanded autologous tumor-infiltrating lymphocytes in metastatic melanoma patients. Clin Cancer Res 18(24):6758–6770. https://doi.org/10.1158/1078-0432.CCR-12-1177
Liu C, Peng W, Xu C, Lou Y, Zhang M, Wargo JA, Chen JQ, Li HS, Watowich SS, Yang Y, Tompers Frederick D, Cooper ZA, Mbofung RM, Whittington M, Flaherty KT, Woodman SE, Davies MA, Radvanyi LG, Overwijk WW, Lizee G, Hwu P (2013) BRAF inhibition increases tumor infiltration by T cells and enhances the antitumor activity of adoptive immunotherapy in mice. Clin Cancer Res 19(2):393–403. https://doi.org/10.1158/1078-0432.CCR-12-1626
Boni A, Cogdill AP, Dang P, Udayakumar D, Njauw CN, Sloss CM, Ferrone CR, Flaherty KT, Lawrence DP, Fisher DE, Tsao H, Wargo JA (2010) Selective BRAFV600E inhibition enhances T-cell recognition of melanoma without affecting lymphocyte function. Cancer Res 70(13):5213–5219. https://doi.org/10.1158/0008-5472.CAN-10-0118
Cooper ZA, Reuben A, Amaria RN, Wargo JA (2014) Evidence of synergy with combined BRAF-targeted therapy and immune checkpoint blockade for metastatic melanoma. Oncoimmunology 3(9):e954–e956. https://doi.org/10.4161/21624011.2014.954956
Sullivan RJ, Gonzalez R, Lewis KD, Hamid O, Infante JR, Patel MR, Hodi FS, Wallin J, Pitcher B, Cha E, Roberts L, Ballinger M, Hwu P (2017) Atezolizumab (A) + cobimetinib (C) + vemurafenib (V) in BRAFV600-mutant metastatic melanoma (mel): updated safety and clinical activity. J Clin Oncol 35:3036
Long GV, Menzies AM, Nagrial AM, Haydu LE, Hamilton AL, Mann GJ, Hughes TM, Thompson JF, Scolyer RA, Kefford RF (2011) Prognostic and clinicopathologic associations of oncogenic BRAF in metastatic melanoma. J Clin Oncol 29(10):1239–1246. https://doi.org/10.1200/JCO.2010.32.4327
Gershenwald JE, Scolyer RA, Hess KR, Sondak VK, Long GV, Ross MI, Lazar AJ, Faries MB, Kirkwood JM, McArthur GA, Haydu LE, Eggermont AMM, Flaherty KT, Balch CM, Thompson JF, for members of the American Joint Committee on Cancer Melanoma Expert P, the International Melanoma D, Discovery P (2017) Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 67(6):472–492. https://doi.org/10.3322/caac.21409
Gerami P, Cook RW, Russell MC, Wilkinson J, Amaria RN, Gonzalez R, Lyle S, Jackson GL, Greisinger AJ, Johnson CE, Oelschlager KM, Stone JF, Maetzold DJ, Ferris LK, Wayne JD, Cooper C, Obregon R, Delman KA, Lawson D (2015) Gene expression profiling for molecular staging of cutaneous melanoma in patients undergoing sentinel lymph node biopsy. J Am Acad Dermatol 72(5):780–785 e783. https://doi.org/10.1016/j.jaad.2015.01.009
Gerami P, Cook RW, Wilkinson J, Russell MC, Dhillon N, Amaria RN, Gonzalez R, Lyle S, Johnson CE, Oelschlager KM, Jackson GL, Greisinger AJ, Maetzold D, Delman KA, Lawson DH, Stone JF (2015) Development of a prognostic genetic signature to predict the metastatic risk associated with cutaneous melanoma. Clin Cancer Res 21(1):175–183. https://doi.org/10.1158/1078-0432.CCR-13-3316
Hsueh EC, DeBloom JR, Lee J, Sussman JJ, Covington KR, Middlebrook B, Johnson C, Cook RW, Slingluff CL Jr, McMasters KM (2017) Interim analysis of survival in a prospective, multi-center registry cohort of cutaneous melanoma tested with a prognostic 31-gene expression profile test. J Hematol Oncol 10(1):152. https://doi.org/10.1186/s13045-017-0520-1
Gray ES, Rizos H, Reid AL, Boyd SC, Pereira MR, Lo J, Tembe V, Freeman J, Lee JH, Scolyer RA, Siew K, Lomma C, Cooper A, Khattak MA, Meniawy TM, Long GV, Carlino MS, Millward M, Ziman M (2015) Circulating tumor DNA to monitor treatment response and detect acquired resistance in patients with metastatic melanoma. Oncotarget 6(39):42008–42018. https://doi.org/10.18632/oncotarget.5788
Ascierto PA, Minor D, Ribas A, Lebbe C, O’Hagan A, Arya N, Guckert M, Schadendorf D, Kefford RF, Grob JJ, Hamid O, Amaravadi R, Simeone E, Wilhelm T, Kim KB, Long GV, Martin AM, Mazumdar J, Goodman VL, Trefzer U (2013) Phase II trial (BREAK-2) of the BRAF inhibitor dabrafenib (GSK2118436) in patients with metastatic melanoma. J Clin Oncol 31(26):3205–3211. https://doi.org/10.1200/JCO.2013.49.8691
Santiago-Walker A, Gagnon R, Mazumdar J, Casey M, Long GV, Schadendorf D, Flaherty K, Kefford R, Hauschild A, Hwu P, Haney P, O’Hagan A, Carver J, Goodman V, Legos J, Martin AM (2016) Correlation of BRAF mutation status in circulating-free DNA and tumor and association with clinical outcome across four BRAFi and MEKi clinical trials. Clin Cancer Res 22(3):567–574. https://doi.org/10.1158/1078-0432.CCR-15-0321
Girotti MR, Gremel G, Lee R, Galvani E, Rothwell D, Viros A, Mandal AK, Lim KH, Saturno G, Furney SJ, Baenke F, Pedersen M, Rogan J, Swan J, Smith M, Fusi A, Oudit D, Dhomen N, Brady G, Lorigan P, Dive C, Marais R (2016) Application of sequencing, liquid biopsies, and patient-derived xenografts for personalized medicine in melanoma. Cancer Discov 6(3):286–299. https://doi.org/10.1158/2159-8290.CD-15-1336
Sanmamed MF, Fernandez-Landazuri S, Rodriguez C, Zarate R, Lozano MD, Zubiri L, Perez-Gracia JL, Martin-Algarra S, Gonzalez A (2015) Quantitative cell-free circulating BRAFV600E mutation analysis by use of droplet digital PCR in the follow-up of patients with melanoma being treated with BRAF inhibitors. Clin Chem 61(1):297–304. https://doi.org/10.1373/clinchem.2014.230235
Chang GA, Tadepalli JS, Shao Y, Zhang Y, Weiss S, Robinson E, Spittle C, Furtado M, Shelton DN, Karlin-Neumann G, Pavlick A, Osman I, Polsky D (2016) Sensitivity of plasma BRAFmutant and NRASmutant cell-free DNA assays to detect metastatic melanoma in patients with low RECIST scores and non-RECIST disease progression. Mol Oncol 10(1):157–165. https://doi.org/10.1016/j.molonc.2015.09.005
Larkin J, Minor D, D'Angelo S, Neyns B, Smylie M, Miller WH, Jr., Gutzmer R, Linette G, Chmielowski B, Lao CD, Lorigan P, Grossmann K, Hassel JC, Sznol M, Daud A, Sosman J, Khushalani N, Schadendorf D, Hoeller C, Walker D, Kong G, Horak C, Weber J (2018) Overall survival in patients with advanced melanoma who received nivolumab versus investigator’s choice chemotherapy in checkmate 037: a randomized, controlled, open-label phase III trial. J Clin Oncol 36(4):383–390. https://doi.org/10.1200/JCO.2016.71.8023
Hamid O, Puzanov I, Dummer R, Schachter J, Daud A, Schadendorf D, Blank C, Cranmer LD, Robert C, Pavlick AC, Gonzalez R, Hodi FS, Ascierto PA, Salama AKS, Margolin KA, Gangadhar TC, Wei Z, Ebbinghaus S, Ibrahim N, Ribas A (2017) Final analysis of a randomised trial comparing pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory advanced melanoma. Eur J Cancer 86:37–45. https://doi.org/10.1016/j.ejca.2017.07.022
Acknowledgements
Editorial assistance to the authors was provided by Ms. Lesley C. Scott-Skye at California Pacific Medical Center Research Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kevin B. Kim has received honoraria from Genentech Inc. Incyte Corp, Novartis Pharmaceuticals, Bristol-Myers Squibb, Array BioPharma for serving as a member of advisory board meeting and honoraria from Bristol-Myers Squibb, Novartis Pharmaceuticals and Merck for serving as a member of speakers bureau.
Rights and permissions
About this article
Cite this article
Swe, T., Kim, K.B. Update on systemic therapy for advanced cutaneous melanoma and recent development of novel drugs. Clin Exp Metastasis 35, 503–520 (2018). https://doi.org/10.1007/s10585-018-9913-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-018-9913-y