Abstract
The standard US diet contributes to greenhouse gas emissions (GHGE) from both the food system, and from the health system through its contribution to non-communicable diseases. To estimate the potential for diet change to reduce GHGE and improve public health, we analyzed the effect of adopting healthier model diets in the USA on the risk of disease, health care costs, and GHGE. We found that adoption of healthier diets reduced the relative risk of coronary heart disease, colorectal cancer, and type 2 diabetes by 20–45%, US health care costs by US$B 77–93 per year, and direct GHGE by 222–826 kg CO2e capita−1 year−1 (69–84 kg from the health care system, 153–742 kg from the food system). Emission reductions were equivalent to 6–23% of the US Climate Action Plan’s target of a 17% reduction in 2005 GHGE by 2020, and 24–134% of California’s target of 1990 GHGE levels by 2020. However, there is potential for investment of health care savings to result in rebound up to and greater than 100%, which would increase net GHGE. Given the urgency of improving public health and of mitigating GHGE over the short term, the potential contribution of diet change, and the options for reducing rebound, deserve more research in support of policy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
There is increasing scientific consensus that significant reductions in anthropogenic greenhouse gas emissions (GHGE) will have to be achieved in the next decade or two to limit global warming to 2 °C to avoid dangerous climate change (Hansen et al. 2013; IPCC 2014; Rogelj et al. 2013; Stocker 2013). Our individual and collective diets, and the food system that creates and supports them, contribute about one third of total emissions globally (Garnett 2011), and changing dietary patterns can reduce GHGE embodied in the diet by up to 50% (Hallström et al. 2015). However, compared with other mitigation strategies, the food system has received relatively little attention (Edenhofer et al. 2014).
Diet change as a mitigation option has the advantage of requiring relatively little investment in new research, technology, or infrastructure, and has important positive externalities, including improved health. However, there are significant economic, social, and cultural challenges to achieving diet change at both individual and policy levels.
Diet change also has the potential to reduce GHGE from the health care system by improving health. The average intake of foods by the US population, the standard American diet (SAD), has become markedly less healthy in recent decades, and in combination with an increasingly sedentary lifestyle, has resulted in an epidemic of non-communicable diseases (NCDs) (Grotto and Zied 2010). About half of all US adults have one or more NCDs, and about two thirds are overweight or obese (USDA and HHS 2015); the prevalence of diabetes was 9% in 2012 (CDC 2012, 2014), the prevalence of cardiovascular disease (including high blood pressure and various forms of coronary heart disease) in the population over 20 years old in 2010 was 35% (Go et al. 2014), and ∼40% of the population is predicted to be diagnosed with cancer during their lifetimes (SEER NCI 2014). NCDs are important contributors to increasing US health care costs, which were almost $3 trillion year−1 in 2014, 18% of the total US GDP (CMS 2016). NCDs can, to a large extent, be prevented by adopting a healthy lifestyle, including healthy diets (WCRF/AICR 2007; WHO/FAO 2003).
The link between diet, health, and climate is a new but growing research field. By using life cycle assessments (LCAs) (ISO 2006a, b), the climate impact of individual foods, meals, and whole diets has been calculated (Scarborough et al. 2014a; Tilman and Clark 2014). Health aspects have been included in LCAs by expressing the climate impact of the food with a functional unit that relates to the nutritional content (Doran-Browne et al. 2015) or by comparing the climate impact of diets with varying nutritional content (Meier and Christen 2012; Saxe et al. 2013; van Dooren et al. 2014; Westhoek et al. 2014). So far, few studies have used epidemiological data to study the relationship between diets’ impact on both GHGE via the food system and on health (Aston et al. 2012; Friel et al. 2009; Scarborough et al. 2012; Springmann et al. 2016; Tilman and Clark 2014). The results from these studies show that dietary change offers substantial potential to simultaneously improve health and reduce GHGE from the food system. However, the potential for rebound (increase in GHGE due to investment of savings from mitigation policies that reduce GHGE) is a major uncertainty that has not been adequately addressed to date (Font Vivanco et al. 2016). This is especially important for health care system savings, since health care dollars are less emissions intensive than the average.
There is no research to date on the combined effect on GHGE from the food and health care systems of the adoption of more healthy diets. Here we report research that addresses this gap. We modeled counterfactual healthy alternative diets (HADs) by adjusting foods in the SAD which are statistically associated with changes in the relative risk for three NCDs. We then estimated the change in direct GHGE from both the food and health care systems. We did not estimate the potential for rebound to take back the reduction in GHGE due to the HADs. Our results provide new insights into the relationship between food, health, and climate that have important policy implications in the development of more sustainable food systems and the mitigation of anthropogenic climate change.
2 Methods
2.1 System boundaries
The spatial boundary of our study was the USA, although we extrapolated LCA data for the food system from other countries when US data were not available, and data for disease risk were from various countries. The reference year for our study was 2013, and we used either data for 2013, extrapolated data to 2013 based on trends, or used data for the closest year when there was no basis for extrapolation. The system boundaries for emissions from the health care system (GHGE-H) were the components of the health care sector associated with the studied NCDs. The system boundaries for emissions from the food system (GHGE-F) were inputs to production at the distal end, including feed and pasture for animals, through retail at the proximal end, because these were the boundaries for the LCA studies we used and included food wasted within these boundaries. Thus, GHGE-F from land use change, and for retail to consumer transport, storage and preparation at the consumer stages, and household food waste disposal were not included, making our estimates conservative. We did not include rebound within the system boundaries. GHGE (in terms of CO2e) comprised the three major greenhouse gases: CO2, N2O, and CH4.
2.2 Overview of methodology
Our method for estimating the effect of dietary change on GHGE comprised six steps (Fig. 1). In step 1, we defined the SAD using data on loss-adjusted food availability at the consumer level, identified foods linked to change in relative risk (RR) for NCDs, and created the HADs by adjusting these foods in the SAD. In step 2, we estimated the changes in disease prevalence with HADs, based on RR estimates found in published meta-analyses. In step 3, we estimated changes in health care expenditures from dietary change, based on changes in disease prevalence from step 2. In step 4, we estimated ΔGHGE-H from dietary change, based on the cost of health care for each NCD from step 3. In step 5, we estimated ΔGHGE-F using LCA data found in the literature. In step 6, we estimated the net total change in GHGE from dietary change, ΔGHGE-T = ΔGHGE-F + ΔGHGE-H.
2.3 Step 1. Developing dietary scenarios
We used the SAD as our reference and compared it with three counterfactual healthy alternative diets (HAD-1, HAD-2, HAD-3) (Table 1). Dietary intake levels in SAD are based on the USDA per capita loss-adjusted food availability data by weight for 2012, the most recent year for which data were available (USDA ERS 2014) (see Online Resource, Section 1.1).
To create the HADs, we adjusted SAD only for foods which met our four criteria: (i) USDA dietary recommendations were consistent with international dietary guidelines and recommendations (USDA and HHS 2010; WCRF/AICR 2007), (ii) there were consistent high quality data correlating the foods with disease, (iii) there were documented GHGE estimates from LCAs, and (iv) there were high quality data on consumption and waste. The changes in HADs were increased consumption of fruits, vegetables, whole grains, and beans and peas, and reduced consumption of refined grains, and red (beef and pork) and processed (preserved by smoking, curing, or salting, or addition of chemical preservatives) meat. There were high quality data linking these foods to from one to three NCDs: coronary heart disease (CHD), colorectal cancer (CRC), and type 2 diabetes (T2D). Creation of the HADs thus involved only a portion of the total SAD.
HAD-1 reflects the USDA dietary recommendations, the “USDA Food Pattern” (USDA and HHS 2010), with processed meat limited to 20% of total red meat. In HAD-2, red meat was further reduced to 25 g of cooked meat day−1, and processed meat was eliminated, and in HAD-3, all red and processed meat was eliminated. The meat removed in the HADs was replaced by increases in beans and peas, based on a framework developed by the USDA for replacing meat protein with plant-based protein (USDA 2010).
2.4 Step 2. Changes in relative risk of disease with changes in diet
We based the selection of diseases to be included on a literature review of the NCBI Pub Med database in March 2014, using as keywords the selected food groups (e.g., “vegetables”) and CHD, hypertension, type 2 diabetes (T2D), and different types of cancer. We selected peer-reviewed meta-analyses of prospective cohort studies, randomized controlled trial studies, and case-control studies, published between 2005 and 2014, that provided RR with 95% confidence intervals (CI) (see Online Resource Section 1.2).
We estimated the health effects of changing the diet from SAD to HADs by calculating a revised RR (RR re ) (Eq. 1) for each food-disease RR (Scarborough et al. 2014b), as reported in the meta-analyses, proportional to the changes of that food in the HADs:
where RR is the original RR obtained from meta-analyses for food f (e.g., processed meat) and disease d (e.g., CHD), x is the level of f in the HAD, y is the level of f in the SAD, and u is the unit increase reported in the meta-analysis identified for disease d.
We then calculated the combined relative risk (RR cd ) of the changes in all of the foods contributing to the RR for each disease by multiplying them:
where RR re1 , RR re2 , RR re3 , and RR ref are the revised RR values for each of the individual foods changed in the diet.
Finally, to construct 95% confidence intervals around the RR estimates for the HADs, we conducted a Monte Carlo simulation (Rubinstein 2007) with 5000 iterations in which the individual RR cd estimates for each disease were allowed to vary randomly according to a lognormal distribution. The result of a Monte Carlo simulation consists of a number of possible outcomes of the calculation, hence giving a representation of the probability of different results depending on the uncertainty and variation in the input data.
2.5 Step 3. Changes in health care costs from changes in disease prevalence
In calculating the reductions in health care costs due to reductions in the RR of the three NCDs for each of the three HADS, we assumed that reduction in these costs in the US economy for each disease were directly proportional to reduction in the RR cd for each disease. We used the most recent and reliable data sources for expenses, and adjusted for inflation (see Online Resource Section 1.3).
2.6 Step 4. Change in GHGE due to changes in health care costs (ΔGHGE-H)
We calculated per capita reduction in GHGE-H for the US population based on established relationships between different types of health care costs and their GHGE in the USA using data from the Carnegie-Mellon IO-LCA (GDI 2014) (see Online Resource Section 1.4). The IO-LCA GHGEs are based on older IPCC estimates of GWP, so we also calculated GHGE by adjusting the GWP for CH4 from 21 to the most recent IPCC estimates (including climate-carbon feedbacks) of 34 for a 100-year time frame (Myhre et al. 2013). While the GWP for N2O changed in the most recent IPCC assessment, the difference was much smaller (from 310 to 298 for the 100-year time frame) and would also have been more difficult to adjust.
2.7 Step 5. Changes in GHGE in the food system (ΔGHGE-F)
We quantified the effect on GHGE-F from changes in diet based on estimates of the GHGE of the specific foods included in the diets, provided from a review of published LCAs (see Online Resource Section 1.5). The literature search was performed in Web of Knowledge (ISI) in April 2014, using as keywords the foods included in the studied diets and LCAs. We also manually searched reference lists from retrieved articles and reviews. GHGE-F data were collected for 28 different food categories and the median, lowest, and highest amount of GHGE-F per kilogram food available at the retail were determined (Tables OR 2, 3, 4). We adjusted the GHGE-F data to match the system boundaries of this study and to reflect the US food system, e.g., by adjusting the proportion of air-transported fruit and hot house-produced vegetables. GHGE-F data were for conventional food production and data on food produced outside of the USA were limited to regions with similar production systems as the USA and to regions that export food to the USA. We adjusted the methane 100-year GWP for beef to the current 34 for the seven source studies for beef, since these comprised the great majority of food system methane emissions for the foods changed to create HADs; six of these used a GWP of 21 and one used 23.
In order to address uncertainty and variability in our GHGE-F results due to differences in production systems, regional conditions, and methods used in different studies (Björklund 2002; Nijdam et al. 2012; Röös and Josefine 2013), we conducted a Monte Carlo simulation (Rubinstein 2007). Because of the limited number and range of estimates in the literature, we used a triangular distribution model for each food category changed in the HADs from the baseline SAD. Each diet iteration involved a summation of the random values within each food category’s distribution. The 5000-iteration Monte Carlo simulation then produced a best estimate and confidence intervals for GHGE-F for each diet.
2.8 Step 6. Net change in GHGE from dietary change (ΔGHGE-T)
The net change in GHGE from dietary change was calculated as the sum of emission reductions in the food (ΔGHGE-F) and the health care systems (ΔGHGE-H).
3 Results and discussion
We found that our HADs resulted in large decreases in GHGE in the health care system, but especially in the food system, and that these were equal to large proportions of US and California climate change mitigation goals. Our estimates are conservative because the HADs included only a selection foods, a selection of associated NCDs, a selection of direct health care GHGE of those conditions, and did not include some important components of food system GHGE (e.g., from land use change and the consumer level). However, the significance of the results is limited by uncertainty, including about the effect of rebound, especially for health care savings, and of longer lives due to HADs.
3.1 Reduction in relative risk of disease and health care costs
The RR cd for CHD, T2D, and CRC for all foods changed in the HADs was reduced by 20–45%, with the largest reduction for CHD, followed by T2D and CRC (Table 2). HAD-1 provided the least reduction in disease prevalence of the HADs (20–40%), while HAD-3, in which all red and processed meat was replaced with legumes, provided the greatest reduction (29–45%).
The potential annual savings in US health care costs with reduction in prevalence of CHD, T2D, and CRC, assuming that the entire US population made a transition from the SAD to the HADs, was $77, $89, and $93 billion year−1 for HAD-1, HAD-2, and HAD-3, or 20–30% of the total expenses for these disease of $220 billion year−1 (CMS 2013).
3.2 Direct reduction in GHGE
Direct reduction in GHGE-H (Table 2) from SAD to the HADs was estimated from the reduction in health care expenses resulting from the reduction in RR (Table 2), with reductions in GHGE-H (kg CO2e capita−1 year−1) from 16 to 18 for CHD, 50–62 for T2D, and 3–4 for CRC. Change in GHGE-F from SAD to the HADs is shown in Table 3. The potential effect of rebound on net GHGE was not estimated.
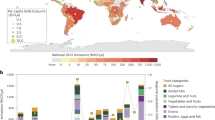
Figure 2 shows the combined reduction in GHGE with a transition from the SAD to the HADs. Adoption of HADs reduced GHG-T by 222–826 kg CO2e capita−1 year−1 (Table OR5). Reductions in GHGE-F dominated reduction potential in all HADs, accounting for 69–90% of total potential reduction. The combined reduction with HAD-2 and HAD-3 was 237 and 373% greater than HAD-1, respectively, due to primarily to the decrease of red and processed meat in the diets.
3.3 Limitations and uncertainty
The results of this study are dependent on the quality of data used for food consumption, food losses, RR, health care expenses, and GHGE. In order to minimize, account for, and illustrate the overall uncertainty in our results, we used validated data of high quality, aimed for high transparency in presenting our methods, and estimated the uncertainty of both GHGE-F and RR of food-related diseases with Monte Carlo simulation.
3.3.1 GHGE-H
A major assumption in our GHGE-H calculations was that the changes in RR are directly related to health care costs. In reality, diet change would only affect disease prevalence over time via reduction in incidence. Our results should therefore be interpreted as theoretical estimates of the disease prevalence attributable to the HADs over time, or as the health care costs associated with a counterfactual scenario where the HADs had always been adopted.
To minimize the risk of double counting health effects when combining RR estimates, we only used RR estimates from meta-analyses that adjusted for influencing confounders, such as other types of food intake, physical activity level, and history of disease. Also, by using whole food-based recommendations (e.g., vegetables), as opposed to nutrient-based recommendations (e.g., protein), we reduced the risk of double counting health effects from nutrients found in various food groups. Despite these efforts, some risk of double counting remains because the RRs are drawn from meta-analyses of mainly prospective cohort studies which have measured usual diet imprecisely, allowing for residual confounding. For increased transparency, we presented the health effects of the HADs both for each dietary factor individually as well as for the combined effect of all dietary changes (Table 2).
There are also some uncertainties in the IO-LCA data used to calculate GHGE-H because it uses an aggregate-based assignment of GHGE for economic activity in a given industry/sector, as opposed to process/product-based assignment. Some components of the LCA, such as pharmaceutical manufacturing, leave out potentially important factors that could add to the GHGE of a given health care expenditure, and some components of our calculations were based on proxy data because GHGE data were not available for all activities. While it is not clear that the health care sector would experience the same rate of decrease in carbon intensity as the overall economy, we did adjust it to match this rate.
Reductions in GHGE-H were underestimated because we did not include many potential diseases (e.g., overweight and obesity, hypertension, stroke, and forms of cancer other than CRC) associated with the foods we did change in HADs, due to lack of adequate RR documentation. In addition, there are also potential diet-disease links for foods we did not change in HADs, e.g., sugar-sweetened beverages. Therefore, the total estimated health care expenses was a small part of the potential contribution of food-related diseases to the total US health care in 2014 of $3 trillion (CMS 2016).
A more fundamental issue in estimating GHGE-H is the increase in life span with reduced risk of NCDs, which would increase the length of time individuals would be generating GHGE. One study of the effect of healthier diets on GHGE globally found that the increased emissions due to longer lives (due to healthier diets) offset only 4–5.8%, and food-related emissions only 0.6–2.2%, of the total food-related emissions reductions in the whole population due to healthier diets (Springmann et al. 2016). Longer life expectancies may also result in increases in additional health care expenses for comorbid conditions. On the other hand, the total health care costs might be reduced if many years of care for T2D, CRC, or CHD were replaced by fewer years of less expensive health care, and higher economic productivity. We did not consider the effect on GHGE of economic adjustments due to changes in demand for different foods (Jensen et al. 2013).
We were not able to estimate the extent of rebound from health care cost savings in terms of the GHGE generated by spending the savings. However, rebound exceeding 100% may be likely because the GHGE intensity of health care dollars is half of that of the rest of the US economy: GHGE from health care is about 10% of US GHGE, while health care is about 20% of the US GDP (Eckelman and Sherman 2016). However, since an estimated 64% of health care expenses in the USA are financed by local, state, and federal government (Himmelstein and Woolhandler 2016), there is potential for government policy to mitigate rebound. More research is needed to better understand the effect of economic savings from healthier diets and other climate mitigation efforts, and to develop policies to direct health care cost savings to investments that would reduce rebound to well below 100% (Font Vivanco et al. 2016).
3.3.2 GHGE-F
A main source of uncertainty in LCA results is the necessity of using data with a range of characteristics from a variety of sources, as we did. This is true both at the global (e.g., Bajželj et al. 2014) and at the regional or national level. Due to lack of data, GHGE data for US foods are typically sourced from other industrial countries (Table OR2) with a range of “climatic conditions, transportation distances, and production methods and therefore are intended to provide a reasonable range of expected values, rather than a definitive result, for each food type” (Heller and Keoleian 2015). Life cycle data on GHGE-F related to the same food item can vary significantly according to different sources due to differences in production systems, regional conditions, and methods used to produce the data (Björklund 2002; Nijdam et al. 2012). Uncertainty was also due to the necessity of using data for a limited selection of foods for each category. For higher precision, regional- or country-level LCA data would be required, which are currently lacking.
We addressed this uncertainty in GHGE-F estimates with a Monte Carlo simulation using a triangular distribution model for each food category as discussed above. This method assumes that uncertainties in GHGE estimates for the food categories are independent of each other, which is a reasonable assumption because most data were from different studies.
GHGE-F estimates were conservative because we did not include land use changes, which can increase emissions from the diet by 10–30% (Röös et al. 2015), although this varies greatly depending on the assessment method used. Potential GHGE-F reductions may also have been underestimated because only a portion of the foods in the SAD was changed in the HADs, while other foods with high emissions (e.g., dairy and other meats) were not. For example, one estimate for the GHGE of dairy in the USA in 2008 was 133.6 Tg CO2e year−1, (using a 100 year GWP for methane of 25) (Thoma et al. 2013), equivalent to 439 kg CO2e capita−1 year−1, which is ∼30% of the GHGE we estimated for SAD. Our results are also likely underestimates to the extent that the EPA underestimates livestock methane emissions in the USA, which could be by almost 50% (Turner et al. 2015), and points to the need for reporting by the livestock industry, the only major sector not required to report GHGE (Halverson 2015).
3.4 Significance
To our knowledge, this is the first study of diet GHGE to: model counterfactual diets by making incremental changes based on recommendations only for foods for which there were high quality RR data for NCDs; estimate reduction in GHGE-H from the health care sector resulting from a change to these diets, in addition to GHGE-F. Our HADs are counterfactual diets illustrating the potential for foods that decrease the RR of NCDs to also decrease GHGE and are meant to illustrate the potential synergies of diet change to contribute simultaneously to improving health and mitigating climate change.
Reductions in GHGE with HAD-1 to HAD-3 represent 1.2–4.4% of the US average per capita GHGE for 2012 (EPA 2014). However, the real significance of the potential of HADs is in comparison with mitigation targets. For example, the range of contributions to mitigation targets potentially achievable for HAD-1 to HAD-3 is 6–23% for the US President’s Climate Action Plan goal of a 17% reduction below US 2005 net GHGE levels by 2020 (Executive Office of the President 2013), and 24–134% for California’s AB 32 goal of reaching 1990 emission levels by 2020 (CARB 2006) (assuming 2020 emissions equal to 2012 emissions) (Table OR6). These estimates do not include the potential for rebound or the effect of increased lifespan.
4 Conclusions
In accordance with several previous studies (Hallström 2015; Scarborough et al. 2014a; Springmann et al. 2016; Tilman and Clark 2014; Westhoek et al. 2014), our results support the hypotheses that healthier eating habits can contribute to large reductions in disease and GHGE in the food system, and that reduction of animal foods, especially red and processed meat, is key.
In addition, we show for the first time that the reduction in health care costs with reduction in NCDs could also directly reduce GHGE. The potential for this direct reduction is likely much greater than our estimates, which were conservative, and limited by the lack of data. However, because of the potential for rebound due to investing the health care savings resulting from diet change, the net reduction in GHGE is uncertain, and rebound could even exceed 100% of the savings, resulting in net increase in GHGE. The extent to which policies for investment of financial savings from reduction in health care costs due to diet change, or other climate change mitigation actions, such as reduced air pollution, could reduce rebound, need to be further investigated. Indeed, the role of rebound in all climate change mitigation strategies, and the potential for policy to reduce it, is relatively unknown (Font Vivanco et al. 2016).
Given the urgency of mitigating GHGE and improving public health over the short term, diet change could play a much more prominent role in national, state, and local climate policies, although there are major psychological, social, and economic challenges to changing diets (Garnett et al. 2015). Because most food choice decisions are the result of unconscious habit, and differ from perceived barriers to climate friendly food choices, and because the public seems largely unaware of a link between diet and climate change (Mäkiniemi and Vainio 2014), there is a role for increased education about the relationships among food choice, climate, and nutrition.
Increased knowledge of the positive synergistic health effects of reducing GHGE via diet change could motivate greater efforts in the future to develop and implement such changes, both at the individual and policy levels. Our results provide new knowledge that could help motivate effective change.
References
Aston LM, Smith JN, Powles JW (2012) Impact of a reduced red and processed meat dietary pattern on disease risks and greenhouse gas emissions in the UK: a modelling study. BMJ Open. doi:10.1136/bmjopen-2012-001072
Bajželj B, Richards KS, Allwood JM, Smith P, Dennis JS, Curmi E, Gilligan CA (2014) Importance of food-demand management for climate mitigation. Nat Clim Chang 4:924–929. doi:10.1038/nclimate2353
Björklund A (2002) A survey of approaches to improve reliability in LCA. Int J LCA 7:64–72
CARB (2006) Assembly Bill 32: Global Warming Solutions Act. http://www.arb.ca.gov/cc/ab32/ab32.htm. Accessed 2012 October 17
CDC (2012) National Diabetes Fact Sheet, 2011 Centers for Disease Control and Prevention. http://www.cdc.gov/diabetes/pubs/factsheet11.htm. Accessed 2014 June 24
CDC (2014) National Diabetes Statistics Report: estimates of diabetes and its burden in the United States. U.S. Department of Health and Human Services; 2014. http://www.cdc.gov/diabetes/pubs/statsreport14.htm. Accessed 2014 June 24
CMS (2013) National Health Expenditure Projections 2012–2022. http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/Proj2012.pdf. Accessed 2014 April 22
CMS (2016) National Health Expenditure Tables. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/Downloads/Tables.zip. Accessed 2016 August 25
Doran-Browne N, Eckard R, Behrendt R, Kingwell R (2015) Nutrient density as a metric for comparing greenhouse gas emissions from food production. Clim Chang 129:73–87. doi:10.1007/s10584-014-1316-8
Eckelman MJ, Sherman J (2016) Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE. doi:10.1371/journal.pone.0157014
Edenhofer O, Pichs-Madruga R, Sokona Y, Farahani E, Kadner S, Seyboth K, Adler A, Baum I, Brunner S, Eickemeier P, Kriemann B, Savolainen J, Schlömer S, Von S, Zwickel T (2014) Climate change 2014: mitigation of climate change. In: Minx JC (ed) Contribution of Working Group III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press, Cambridge, UK
EPA (2014) Inventory of U.S. Greenhouse Gas Emissions and Sinks: 1990–2012. EPA. http://www.epa.gov/climatechange/ghgemissions/usinventoryreport.html. Accessed 2014 June 15
Executive Office of the President (2013) The President’s Climate Action Plan. The White House, Washington DC
Font Vivanco D, Kemp R, Van Der Voet E (2016) How to deal with the rebound effect? A policy-oriented approach. Energ Policy 94:114–125. doi:10.1016/j.enpol.2016.03.054
Friel S et al (2009) Health and climate change 4 public health benefits of strategies to reduce greenhouse-gas emissions: food and agriculture. Lancet 374:2016–2025. doi:10.1016/s0140-6736(09)61753-0
Garnett T (2011) Where are the best opportunities for reducing greenhouse gas emissions in the food system (including the food chain)? Food Policy 36:S23–S32. doi:10.1016/j.foodpol.2010.10.010
Garnett T, Mathewson S, Angelides P, Borthwick F (2015) Policies and actions to shift eating patterns: what works? FCRN; Catham House, Oxford; London
GDI (2014) Economic input–output life cycle assessment. GreenDesign Institute, Carnegie Mellon University. http://www.eiolca.net/index.html. Accessed 2014 January 15
Go AS et al (2014) Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 129:e28–e292. doi:10.1161/01.cir.0000441139.02102.80
Grotto D, Zied E (2010) The standard American diet and its relationship to the health status of Americans. Nutr Clin Pract 25:603–612. doi:10.1177/0884533610386234
Hallström E, Carlsson-Kanyama A, Börjesson P (2015) Environmental impact of dietary change: a systematic review. J Clean Prod 91:1–11
Halverson N (2015) US gives meat producers a pass on climate change emissions. Reveal, from the Center for Investigative Reporting. https://www.revealnews.org/article/us-gives-meat-producers-a-pass-on-climate-change-emissions/. Accessed 2016 May 23
Hansen J et al (2013) Assessing “dangerous climate change”: required reduction of carbon emissions to protect young people, future generations and nature. PLoS ONE 8, e81648. doi:10.1371/journal.pone.0081648
Heller MC, Keoleian GA (2015) Greenhouse gas emission estimates of U.S. dietary choices and food loss. J Ind Ecol 19:391–401. doi:10.1111/jiec.12174
Himmelstein DU, Woolhandler S (2016) The current and projected taxpayer shares of US health costs. Am J Public Health 106:449–452. doi:10.2105/AJPH.2015.302997
IPCC (2014) Climate Change 2014: impacts, adaptation, and vulnerability. The Fifth Assessment Report (AR5). IPCC, Geneva
ISO (2006a) Environmental management. Life cycle assessment—principles and framework. International Standard Organisation, Geneve
ISO (2006b) Environmental management. Life cycle assessment—requirements and guidelines. International Standard Organisation, Geneve
Jensen H et al (2013) The importance of health co-benefits in macroeconomic assessments of UK greenhouse gas emission reduction strategies. Clim Chang 121:223–237. doi:10.1007/s10584-013-0881-6
Mäkiniemi J-P, Vainio A (2014) Barriers to climate-friendly food choices among young adults in Finland. Appetite 74:12–19. doi:10.1016/j.appet.2013.11.016
Meier T, Christen O (2012) Environmental impacts of dietary recommendations and dietary styles: Germany as an example. Environ Sci Technol 47:877–888
Myhre G, Shindell, D, Bréon, F-M, Collins, W et al (2013) Anthropogenic and natural radiative forcing. In: Stocker TF et al (eds) Climate change 2013: the physical science basis contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press, Cambridge, pp 659–740. doi:10.1017/CBO9781107415324.018
Nijdam D, Rood T, Westhoek H (2012) The price of protein: review of land use and carbon footprints from life cycle assessments of animal food products and their substitutes. Food Policy 37:760–770. doi:10.1016/j.foodpol.2012.08.002
Rogelj J, McCollum DL, Reisinger A, Meinshausen M, Riahi K (2013) Probabilistic cost estimates for climate change mitigation. Nature 493:79–83. doi:10.1038/nature11787
Röös E, Josefine N (2013) Uncertainties and variations in the carbon footprint of livestock products. Rapport 063. Department of Energy and Technology, Swedish University of Agricultural Sciences, Uppsala, Sweden
Röös E, Karlsson H, Witthöft C, Sundberg C (2015) Evaluating the sustainability of diets–combining environmental and nutritional aspects. Environ Sci Pol 47:157–166. doi:10.1016/j.envsci.2014.12.001
Rubinstein R, Kroese D (2008) Simulation and the Monte Carlo method. 2nd edn. Wiley, Hoboken
Saxe H, Larsen T, Mogensen L (2013) The global warming potential of two healthy Nordic diets compared with the average Danish diet. Clim Chang 116:249–262. doi:10.1007/s10584-012-0495-4
Scarborough P, Allender S, Clarke D, Wickramasinghe K, Rayner M (2012) Modelling the health impact of environmentally sustainable dietary scenarios in the UK. Eur J Clin Nutr 66:710–715
Scarborough P, Appleby P, Mizdrak A, Briggs AM, Travis R, Bradbury K, Key T (2014a) Dietary greenhouse gas emissions of meat-eaters, fish-eaters, vegetarians and vegans in the UK. Clim Chang 125:179–192. doi:10.1007/s10584-014-1169-1
Scarborough P, Harrington RA, Mizdrak A, Zhou LM, Doherty A (2014b) The preventable risk integrated ModEl and its use to estimate the health impact of public health policy scenarios. Scientifica 2014:21. doi:10.1155/2014/748750
SEER NCI (2014) Cancer Statistics. NCI. http://seer.cancer.gov/. Accessed 2014 April 22
Springmann M, Godfray HCJ, Rayner M, Scarborough P (2016) Analysis and valuation of the health and climate change cobenefits of dietary change. Proc Natl Acad Sci. doi:10.1073/pnas.1523119113
Stocker TF (2013) The closing door of climate targets. Science 339:280–282. doi:10.1126/science.1232468
Thoma G et al. (2013) Greenhouse gas emissions from milk production and consumption in the United States: a cradle-to-grave life cycle assessment circa 2008. International Dairy Journal 31, Supplement 1:S3-S14. doi:10.1016/j.idairyj.2012.08.013
Tilman D, Clark M (2014) Global diets link environmental sustainability and human health. Nature advance online publication doi:10.1038/nature13959
Turner A et al. (2015) Estimating global and North American methane emissions with high spatial resolution using GOSAT satellite data.
USDA (2010) Dietary Guidelines for Americans 2010
USDA, HHS (2010) Dietary Guidelines for Americans, 2010. 7th Edition. Washington, DC, U.S
USDA ERS (2014) Food availability (per capita) data system. http://www.ers.usda.gov/data-products/food-availability-%28per-capita%29-data-system/.aspx -.U3qgyC-LnjE. Accessed 2014 August 14
USDA, HHS (2015) Scientific report of the 2015 Dietary Guidelines Advisory Committee. USDA, HHS, Washington, D.C.
Van Dooren C, Marinussen M, Blonk H, Aiking H, Vellinga P (2014) Exploring dietary guidelines based on ecological and nutritional values: a comparison of six dietary patterns. Food Policy 44:36–46. doi:10.1016/j.foodpol.2013.11.002
WCRF/AICR (2007) Food, nutrition, physical activity, and the prevention of cancer: a global perspective. AICR, Washington DC
Westhoek H et al (2014) Food choices, health and environment: effects of cutting Europe’s meat and dairy intake. Glob Environ Chang 26:196–205, doi:10.1016/j.gloenvcha.2014.02.004
WHO/FAO (2003) Diet, nutrition, and the prevention of chronic disease. Report of 164 a joint WHO/FAO Expert Consultation. Geneva, Switzerland
Acknowledgements
We gratefully acknowledge the valuable comments provided by Daniela Soleri, Pål Börjesson, Annika Carlsson-Kanyama, and two anonymous reviewers for Climatic Change; the help of Nathan Donnelly in the initial stages of research; and the financial support to EH by the Swedish Energy Agency and Royal Swedish Academy of Agriculture and Forestry. A preliminary version of our analysis of GHGE in the health care sector was presented at the Life Cycle Assessment in the Agri-Food Sector conference in 2014.
Author Contributions
Order of authors was determined as follows: corresponding author is the last author, other authors are listed in order of the significance of their contributions. DAC developed and framed the research, and reviewed methods and analyses; EH and QG helped refine the research; EH created the SAD and HADs, calculated food system GHGE, and assembled the RR data; QG, EH, and PS analyzed the RR data; QG assembled and analyzed the health care cost and health care system GHGE data; DAC, EH, and QG wrote the paper; all authors reviewed the paper.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 306 kb)
Rights and permissions
About this article
Cite this article
Hallström, E., Gee, Q., Scarborough, P. et al. A healthier US diet could reduce greenhouse gas emissions from both the food and health care systems. Climatic Change 142, 199–212 (2017). https://doi.org/10.1007/s10584-017-1912-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10584-017-1912-5