Abstract
This randomized control trial used intent-to-treat analyses to compare parent management training—Oregon model (PMTO) (N = 64) to family-based services as usual (SAU) (N = 62) in 3.5–13-year-old children and their families in Denmark. Outcomes were parent report of child internalizing and externalizing problems, parenting efficacy, parenting stress, parent sense of coherence, parent-report of life satisfaction, and parental depressive symptoms. Outcomes were measured at pretreatment, post-treatment, and 18–20 months post-treatment. Results demonstrated that both PMTO and family-based SAU resulted in significant improvements in child externalizing and internalizing problems, parenting efficacy, as well as parent-reported stress and depressive symptoms, life satisfaction, and aspects of sense of cohesion. Effect sizes at post-treatment and follow-up were in the small to moderate range, consistent with prior PMTO evaluations. However, there were no significant differences between PMTO and family-based SAU. Further research on the process and content of family-based SAU is needed to determine how this approach overlaps with and is distinct from PMTO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parent management training—Oregon model (PMTO) [1] is a specific brand of what are generally referred to as behavioral parent training (BPT) interventions [2]. BPT approaches integrate theory, research and practice on family interaction and child behavior [1, 2]. BPT is based on operant conditioning and social learning theory [3], which emphasizes the child’s social environment and reinforcement contingencies that shape both challenging and prosocial behaviors [1, 4]. Challenging parent–child interactions occur in all families; however, in well-functioning families, parents teach children to resolve conflicts using positive means such as humor and negotiation [5, 6]. In less well-functioning families, however, children’s problematic behavior is learned through modeling of parent’s aversive behaviors (e.g., arguing, aggression) as well as negative reinforcement (removal of parental requests to perform undesired behavior) during compliance interactions. Through social learning, operant conditioning and repeated coercive cycles [1, 4], harsh, punitive and aggressive behavior patterns are formed in children, maintained, and over time these behaviors tend to generalize from the family setting to other social settings (e.g., school and peer contexts) [3, 7].
PMTO is an evidence-based psychosocial intervention for the treatment of child behavioral challenges, targeting specific parenting practices to reduce negative coercive cycles between parents and their child. PMTO focuses on teaching parents proactive, non-punitive methods to address, prevent, and reduce challenging behavior in their child. PMTO has a long-standing and robust history as an intervention approach, dating back to the 1960s [8]. Since then, multiple studies, primarily in the United States, have demonstrated the effectiveness of PMTO across two to 18-year-old youth with behavioral disorders (e.g., oppositional defiant and conduct disorder) and antisocial behaviors (e.g., substance abuse, police involvement), using various formats (e.g., individual, groups, telehealth and web-based; [9,10,11,12,13,14]).
With the development of PMTO specifically, and BPT more broadly, there have been increasing efforts over the past two decades to disseminate these approaches internationally. A recent review and meta-analysis [15] found that across 17 studies conducted in 10 countries over five geographical regions, BPT interventions, including PMTO, were effective in reducing child behavior problems. Findings demonstrate that these BPT interventions, developed primarily in the United States and Australia, can be transported to communities that are culturally distinct from where the BPT interventions were initially developed. These findings, while promising, must also be interpreted with other data suggesting that there are attenuated effects of these evidence-based interventions when compared to services as usual (SAU) for children who are clinically referred for treatment [16, 17] and variability of effects across different BPT programs [18]. These data suggest that a closer inspection of randomized effectiveness trials of clinically referred youth comparing specific BPTs (i.e., PMTO) to SAUs in geographically similar regions may be needed.
PMTO has been implemented in the Nordic countries (i.e., Norway, Iceland, Denmark) since the 1990s (see [11] for a discussion) and robust transfer approaches to scale up and sustain PMTO in these countries have been undertaken [19]. To our knowledge, four separate randomized controlled effectiveness trials of PMTO compared with SAU have been conducted in these Nordic countries [20,21,22,23] and one in the Netherlands [24]. The first European randomized controlled trial (RCT) study was conducted in Norway, and included 112 clinically referred children aged four to 12 and their families, who were randomly assigned to either PMTO or SAU [20]. In this study, families assigned to SAU were offered a broad range of treatments, including family therapy, marte meo (i.e., a program that aims to enhance constructive interaction and communication between parent and child), behavior therapy, cognitive therapy, humanistic-existential therapy, and other eclectic approaches to treatment. Results showed that PMTO was more effective than SAU on post-treatment outcome measures relating to externalizing behavior problems, social competence and parental discipline.
A one-year follow-up study of 67% of the sample [25] found differential results based on type of analyses. In an intent-to-treat analysis, two-parent families assigned to PMTO were observed to have less aversive behavior on an observation task than two-parent families assigned to the SAU condition. No significant differences were reported on the other 19 outcomes analyzed. In a treatment-on-the-treated analysis, PMTO resulted in continued effects relative to the SAU condition on teacher-reported total problems, aggression, delinquency, and social skills. In addition, families assigned to PMTO reported greater family cohesion, and observations of aversive behavior were lower in two-parent families assigned to PMTO compared to those assigned to SAU. Overall, the findings suggest that PMTO is beneficial for families at post-treatment and follow-up effects (unsurprisingly) are more evident for families who have at least minimally participated (i.e., attending at least two PMTO sessions) in treatment compared to SAU.
Another randomized trial of group PMTO conducted in Norway utilized a sample of 137 children (3–12 years) who had conduct problems and their parents [22]. Parents in group PMTO reported improvement in child externalizing behavior, social competence, and parental mental health and parenting practices compared to a SAU comparison group, both at the termination of the intervention and six months after the intervention. Group PMTO was also associated with an immediate significant positive effect on parent expectations and teacher-reported social competence, but there was no difference between treatment conditions in these outcomes at the six month follow up. A third randomized trial in Norway [23] evaluated the effectiveness of PMTO among 96 children with behavior problems (ages 3–9 years) and their mothers, all of whom were Pakistani and Somalian immigrants. Compared to the waitlist condition, PMTO was associated with a significant decrease in harsh discipline and an increase in positive parenting. Additionally, PMTO was associated with a reduction in parent reported child conduct problems. However, there were no significant intervention effects on conduct problems or social skills in school as reported by teachers. Similar to findings from Hagen et al. [25], the study unsurprisingly found that the largest effect sizes were found among mothers who attended more than 50% of the PMTO group sessions.
The Icelandic RCT of PMTO included 102 children between the ages of five to 12 with behavior problems and their families [21, 26]. SAU included counseling from a psychologist, counseling from a school counselor, and/or social services that included parenting advice and individual or family psychotherapy. PMTO was found to be more effective than SAU in improving a composite measure of child adjustment, although on single-measure indicators, only social skills improved following PMTO relative to SAU. No effects were found on child-report of depressive symptoms as well as parent- and teacher-report of problem behaviors. Importantly, given that convergent multiple informant constructs, as measured by the composite measure of child adjustment, are more reliable than single-item measures, the results support the main study hypothesis that PMTO would lead to better child outcomes for children relative to SAU. In a separate analysis, Sigmarsdóttir and colleagues [21] found no between-group differences on parenting behavior, although results demonstrated that PMTO appeared to attenuate the detrimental effects of maternal depressive symptoms on maternal parenting behavior in families who were assigned to PMTO. No longer-term follow-up data were reported. Collectively, the findings support the use of PMTO as a treatment for children with behavioral difficulties in Iceland.
While the first four national RCT effectiveness studies conducted in Norway and Iceland were generally supportive of PMTO as compared to SAU [20, 21, 25, 26], a more recent study conducted in The Netherlands was largely unsupportive. In a quasi-randomized effectiveness trial of 146 families with children aged four to 11 years with behavior problems, Thijssen and colleagues [24] examined PMTO and SAU at baseline and after 6, 12, and 18 months of intervention. SAU treatment included family therapy, psychiatric intensive home care, parent therapy, and other services. Results demonstrated that both PMTO and SAU were effective in reducing child externalizing behavior, parental stress, and symptoms of parental psychopathology. Self-reported parenting skills were also improved for both PMTO and SAU families after six months, which were maintained at both 12- and 18-month follow-up assessments. The results of this study found that both PMTO and SAU led to significant improvement for families, but there were no differential effects of PMTO on outcomes.
The collective studies conducted in Nordic countries suggest that PMTO can be effective on a variety of outcomes, but outcomes vary and suggest that PMTO should be further evaluated, particularly when implemented in a new country. Additionally, findings from the Thijssen and colleagues [24] study suggest that the effect size (d = 0.55) of SAU, when compared to effect sizes of SAU in the other trials (d = 0.22–0.43), was higher, despite effect sizes across PMTO being equivalent across studies. Thijssen and colleagues [24] note that the higher effect of SAU found in their study may be in part due to the higher use of cognitive-behavioral techniques in the SAU condition; techniques that are often important components of evidence-based treatment for children with behavioral problems. As such, the SAU condition in the Thijssen and colleagues [24] study may have included components of PMTO, thereby attenuating differences between PMTO and SAU and resulting in the increased effect size of SAU found in that study.
The purpose of this study was to report findings of the most recent randomized clinical effectiveness trial of PMTO in a Nordic country (i.e., Denmark). Specifically, using intent-to-treat analyses, 126 children between three and a half to 13 years of age with behavior problems and their families referred to clinic services were randomized to PMTO or family-based SAU with child behavior, parent efficacy, and parental well-being assessed at baseline, post-treatment and and 18-month follow-up assessments. Importantly, unlike previous studies conducted in Nordic countries, the current study utilizes a specific, and likely most robust SAU comparator—a family-based SAU model. As such, this study evaluates PMTO, a formal, evidence-based, manualized intervention approach to family-based SAU—an informal, evidence-informed, unstructured intervention approach routinely utilized in Denmark for addressing behavioral challenges in youth. In alignment with the majority of studies on PMTO, we hypothesize that PMTO will lead to improvements in child- and parent-level outcomes at immediate post-treatment, with maintenance of effects at follow-up assessment relative to family-based SAU.
Method
Participants
Eligible participants were initially families with children aged four to 12 years, who were referred to municipal treatment because of child behavioral problems (e.g., problem consistent with oppositional defiant disorder and conduct disorder). To increase recruitment rates during the trial, the age range was expanded to include families with children or adolescents between the ages of three and 13 years old and allocation ratios were adjusted in two municipalities in response to a change in municipal capacity. Six children, ages three and a half to four years old, and one 13-year-old child were included in the trial. Families agreeing to participate were randomized either to the PMTO intervention or to the SAU comparison group, which was another municipal treatment option for this study. In total, 123 families with 132 children participated in the study (i.e. nine families participated with two children). The majority of participating children were boys (PMTO = 69%; SAU, 73%), and the youth mean age at baseline was eight years old (PMTO M = 7.9 years old, SD = 2.3; SAU M = 8.1 years old, SD = 2.3). There were no significant differences found in child characteristics or caregiver age between the two intervention groups. There was a small but significant difference in years of education between caregivers in PMTO versus those in SAU, with SAU caregivers having more years of education (See Table 1 for more details). In both intervention groups, the vast majority of respondents were mothers (91%) compared to fathers (9%) and were employed (PMTO, 64%; SAU, 58%).
Procedure
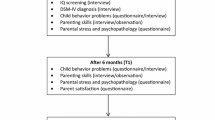
The RCT was a parallel group study conducted in 11 municipalities in Denmark. To be included in the study, municipalities had to offer both PMTO treatment and family treatment to the target group. This criterion ensured that randomization of participants was possible within the participating municipality. Blinded case officers or pre-admission assessment committees in the municipality recruited treatment-referred families to the trial. Families were randomly assigned to either the PMTO intervention or SAU following consent to participate in the study. The research institute used computer generated tables to allocate families to treatments within the municipality. Blocking was used to ensure that comparison groups were generated according to predetermined ratios. Allocation ratios varied between municipality, (i.e., 3:2, 1:1, or 2:3), and were adjusted according to the municipality’s treatment capacity in PMTO and family-based SAU. Families were assessed at three time points: baseline (T0), post-treatment after 7–8 months (T1), and follow-up after 18–20 months (T2). Assessments were conducted by trained interviewers who were not involved in the treatment. Assessments took place in the families’ homes and questionnaires were completed by the primary caregiver. Of the 132 children, 126 (95%) children were assessed at baseline (PMTO n = 64; SAU n = 62); 124 (94%) children were assessed post-treatment (PMTO n = 65; SAU n = 59); and 112 (85%) children were assessed at the follow-up (PMTO n = 61; SAU n = 52). Dropout rates were equally distributed between PMTO and SAU ([Pearson χ2(2) = 0.187; p = 0.91]; see Fig. 1 for a flow chart). All families in this study received treatment between January 2013 and July 2016.
Measures
Some of the below measures had not yet been translated into Danish, and therefore two Danish/English-speaking authors with significant experience with the psychological constructs measured by the below questionnaires separately translated the questionnaires. When there was disagreement in the translation, the final wording was agreed upon together with a third author to ensure the spirit of the measures were retained. Several of these measures were included in a recently completed behavioral parent training study in Denmark [27].
Child Outcomes
The Strengths and Difficulties Questionnaire (SDQ [28]) is a 25-item measure with a 3-point Likert scale that measures general aspects of youth behavior, emotions and peer relationships. The 25 items consist of five subscales measuring emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior. Four of the subscales aggregate into more general broadband scales of internalizing (emotional symptoms and peer relationship) and externalizing (conduct problems and hyperactivity/inattention) problems. The total score ranges from 0 to 40 and each subscale ranges from 0 to 10 with higher scores indicating more problematic issues. The SDQ is widely used for assessing children’s mental health and functioning [29]. Both English and Danish versions have proven to be reliable and valid [30,31,32]. In this sample, Cronbach’s alpha for the parent-reported SDQ total score was 0.68, 0.73, and 0.74 at baseline, post-treatment, and follow-up, respectively.
Parent Outcomes
The parenting sense of competence (PSOC) scale is a 16-item screening instrument evaluating parental skills on two dimensions: parental efficacy and parental satisfaction [33, 34]. Items are scored on a 6-point Likert scale ranging from 1 (“Strongly Disagree”) to 6 (“Strongly Agree”). The instrument was translated into Danish in the context of this study; hence the Danish version applied has not been validated yet. For this paper, parental efficacy scores are reported. In this sample, Cronbach’s alpha was 0.86, 0.82, and 0.80 at baseline, post-treatment, and follow-up, respectively.
The Ladder of Life (LOL) is derived from the Self-Anchoring Striving Scale [35], and was included in the present study to measure parents’ self-evaluation of their current life satisfaction. The items on this measure are presented on the figure of a ladder, which consists of steps with ratings from 0 to 10, with 0 being the lowest rung on the ladder, meaning “The worst possible life,” (indicating a very unsatisfying life) and 10 being the highest rung on the ladder, meaning “The best possible life,” (indicating a very satisfying life). Respondents may be asked their ratings in regards to various time-points in their lives (e.g., “Where on this ladder would you say you are now?”, “Where on this ladder were you two years ago?”, Where on this ladder do you hope to be in six months?”). The scale has demonstrated adequate validity and reliability over the years [36,37,38]. A Danish version of the ladder was included in this study and focused on gathering responses in accordance to the parents’ current life situations.
The Sense of Coherence (SOC; [39]) scale is a reliable, valid, and cross-culturally applicable 13-item screening instrument measured on a 7-point Likert scale ranging from “Seldom or Never” to “Very Often” as viable responses. It produces scores for three subscales assessing: (1) comprehensibility, the ability for people to understand what happens around them; (2) manageability, the extent they are able to manage situations on their own or with the assistance of their social network; and (3) meaningfulness, the ability to find meaning in these situations [40, 41]. These three components, which include cognitive, behavioral, and motivational elements, combine to form a total score encompassing respondents’ general sense of coherence in regards to their own lives. In this study we translated the SOC into Danish and included all 13 items in the assessment of parents. In this sample, Cronbach’s alpha was 0.86, 0.87, and 0.85 at baseline, post-treatment, and follow-up, respectively.
The Parental Stress Scale (PSS; [42]) measures parents’ feelings of stress in relation to child upbringing. The PSS consists of 18 items scored on a 5-point Likert scale, which ranges from “Strongly Disagree,” to “Strongly Agree.” All items were translated into Danish and included in this study. The original English version has proven to be highly reliable and highly related to the general measure of stress [42]. In this sample, Cronbach’s alpha was 0.80, 0.85, and 0.84 at baseline, post-treatment, and follow-up, respectively.
The Major Depression Inventory (MDI; [43]) a widely known and validated instrument used for depression screening in adults [44]. The 10 items are scored on a 6-point scale, ranging from 0, “At No Time” to 5, “All the Time” and assess the frequency of different feelings and experiences related to depression. The original, validated version was collected from caregivers in this study. In this sample, Cronbach’s alpha was 0.88, 0.90, and 0.93 at baseline, post-treatment, and follow-up, respectively.
Intervention
PMTO
Parents met with therapists providing PMTO services for one-hour long sessions on a weekly basis. In Denmark, the meetings generally took place at communal family centers. The length of treatment varied between families, but on average, treatment consisted of 23 individual sessions evenly distributed over the course of seven months [45]. During training, parents were guided through five core parenting practices, including: (1) skill encouragement (i.e., contingent positive reinforcement and teaching techniques); (2) effective discipline (i.e., contingent use of mild sanctions); (3) monitoring (i.e., keeping track of activities); (4) problem-solving (i.e., negotiating disagreements and establishing rules); and (5) positive involvement (i.e., investing time and planning activities; [46]). The five parenting practices and a number of applications were taught in a fixed order, as they are conceptualized to build upon each other. Intervention content was delivered through a number of different modalities, including roleplay, which is one of the essential tools in PMTO treatment. Between sessions, parents carried out defined homework assignments. Telephone contact between the therapist and parents was provided between the sessions to ensure homework completion and enhance engagement and attendance.
PMTO training followed best practices as developed by the PMTO developers (see [19] for details of training conducted across Nordic countries). The PMTO program training structure has some variability in regards to certification requirements. The time to complete certification ranges from 12 to 24 months of training for professionals, during which trainees attend between 11 and 18 days of workshop seminars, treat cases in community agencies utilizing the PMTO intervention, and receive coaching on recorded sessions approximately twice a month. The coaching utilizes videotaped examples from the trainees’ own cases to provide a secure learning environment that emphasizes modeling active teaching strategies, including role-play, problem-solving, and effective questioning processes. Although the trainees work with a reduced caseload throughout the training process, they must implement the intervention with a minimum of at least five families. To be certified, trainees must achieve a mean Fidelity of Implementation Rating System (FIMP; see Treatment Fidelity section below) score of six or above on four sessions covering the following core components: introducing encouragement, troubleshooting encouragement, introducing discipline, and troubleshooting discipline (see [19] for more information).
The FIMP [47] was utilized to assess the PMTO therapists’ adherence to the intervention model in Denmark. Rating was based on observations of nine to 11-min video segments of therapy, where the therapist introduced parents to or coached them in one of two parenting practices from the PMTO model (i.e., skill encouragement or limit setting). To ensure high inter-rater consistency in observations, raters were certified PMTO practitioners with additional FIMP training. The therapists’ delivery was rated on five therapeutic competences, which included: (1) the therapist’s knowledge of social learning theory and PMTO principles and practices; (2) structure and management of sessions; (3) balance between verbal and active teaching tools; (4) range of strategic process skills (e.g., effective questioning, managing resistance, connecting with the family or avoiding negativity); and (5) demonstration of overall development (e.g., promotion and accomplishment of individual satisfaction and growth). Each item was scored on a nine-point scale, where a score of one to three reflected needed additional work, four to six demonstrated acceptable work, and seven to nine reflected good work. A score of six is necessary for PMTO certification. Fidelity ratings for the Danish implementation of PMTO have been published in a separate study [19] which demonstrated that the fidelity ratings collected during the implementation of PMTO in Denmark were considered in the ‘good work’ range.
SAU
SAU was a family-based intervention characterized by informal, evidence-informed practices delivered in a flexible, unstructured format. Therapists were required to have several years of independent clinical experience working within the clinical setting and be willing to treat at least one family using SAY approaches. Supervision for SAU therapists followed procedures within their clinical setting. Generally, this varied across sites. Given that the study aims were to evaluate a PMTO approach (standardized training, supervision and manualized delivery) compared to SAU, the study did not constrain nor attempt to modify SAU processes.
Data Analysis
This study employed an experimental, within-subject analysis. In particular, we estimated the following fixed-effect (FE) regression: Yit = ∑ αtTimet + ∑βtTimet × Treati + ui + εit, where the outcome, Yit, was explained by a time indicator variable (Time = 0, 1, 2), a time-treatment interaction term (Treat = 0 if SAU and Treat = 1 if PMTO), and a child fixed-effect (ui). The parameters, αt, estimated the change over time for the SAU group, and αt + βt estimated the change over time for the PMTO group. Thus, the treatment effects, βt, estimated the additional effect of PMTO compared to SAU (t = 1, 2). We reported Cohen’s d effect sizes (ES) to determine the relative magnitude of each effect by dividing the change with the pretest SD. ES around 0.20 suggest a relatively small effect, ES around 0.50 suggest a medium effect, and ES around 0.80 suggest a relatively large effect [48].
The analysis attempted to account for two challenges in the sample: sample attrition and clustering of respondents. In particular, we applied FE regressions to adjust point estimates and their standard errors for all time-invariant confounders of attrition. Cluster-robust standard errors were estimated to adjust standard errors for clustering at the family level. We applied an adjustment strategy to control for potential attrition bias. In the FE regression, the fixed-effect parameters, ui, absorbed all time-invariant predictors of the outcome, Yit, including potential time-invariant confounders (e.g. gender, baseline age, baseline level of outcome, level of education, constant motivation, time-invariant therapeutic alliance or other time-invariant omitted variables). The FE regression therefore controlled for potential attrition bias via a rigorous adjustment strategy that controls for all time-invariant variables, regardless of whether or not the variable was collected in the data [49]. Consequently, all regressors in the FE model must also vary over time as time-invariant regressors are collinear with ui, so the main effects of treatment (Treati) is excluded from the FE regression. See Wooldridge [50] and StataCorp [51] for an introduction to FE and McNeish and Kelley [49] for a recent comparison of FE and Mixed effects models.
We estimated clustered standard errors to account for potential non-independence of observations. The sample contained repeated outcomes over time for the same child, clustered in a family and in a municipality, suggesting that outcomes (and regression errors, εit) were not independent over i and t. To adjust standard errors, we reported heteroscedastic- and cluster-robust standard errors [52,53,54,55]. The supplementary material provides comparable analyses that employed mixed effects models to control for non-independence of observations.
Results
Child Behavioral Outcomes
Table 2 reports means and standard deviations for all child- and parent-reported outcomes, as well as the main effect of time and the effect of PMTO conditional on the development in the SAU group. Statistically significant improvements over time were found on SDQ total score for the SAU group, both at post-treatment (α1 = − 3.82; p < 0.01; 95% CI = − 5.29 to − 2.36; d = 0.63) and at follow-up (α2 = − 4.51; p < 0.01; 95% CI = − 6.29 to − 2.73; d = − 0.74); and for the PMTO group, both at post-treatment (α1 + β1 = − 3.85; p < 0.01; 95% CI = − 5.36 to − 2.34; d = 0.63) and at follow-up (α2 + β2 = − 5.01; p < 0.01; 95% CI = − 6.58 to − 3.44; d = 0.82). Thus, in both comparison groups, child behavior problems significantly decreased over the treatment period, and continued to decrease from post-treatment to follow-up. The change over time at post-treatment and follow-up can be characterized as medium and large, respectively. There were no significant interaction effects of time and treatment condition, so there were no statistically significant differences between the effectiveness of PMTO and SAU on child behavior, either at post-treatment (β1 = − 0.02; p = 0.98; 95% CI = − 2.12 to 2.07; d = 0.00) or at follow-up (β2 = − 0.50; p = 0.67; 95% CI = − 2.82 to 1.82; d = 0.08).
Similarly, results indicated that in both conditions, there were statistically significant main effects of time on SDQ subscale scores at post-treatment, including the externalizing subscale (α1 = − 1.71; p < 0.01; 95% CI = − 2.61 to − 0.81; d = 0.43), internalizing subscale (α1 = − 2.11; p < 0.01; 95% CI = − 2.99 to − 1.24; d = 0.54), emotional problems subscale, (α1 = − 1.23; p < 0.01; 95% CI = − 1.84 to -0.61; d = 0.55), conduct problems subscale (α1 = − 0.82; p < 0.01; 95% CI = − 1.30 to − 0.35; d = 0.43), hyperactivity subscale (α1 = − 0.89; p < 0.01; 95% CI = − 1.45 to − 0.32; d = 0.34), and peer problems subscale (α1 = − 0.89; p < 0.01; 95% CI = − 1.33 to − 0.45; d = 0.41). The statistically significant main effects of time on SDQ subscale scores persisted at follow-up, including the externalizing subscale (α2 = − 2.39; p < 0.01; 95% CI = − 3.52 to − 1.26; d = − 0.60), internalizing subscale (α2 = − 2.12; p < 0.01; 95% CI = − 2.98 to − 1.26; d = 0.55), emotional problems subscale, (α2 = − 1.17; p < 0.01; 95% CI = − 1,79 to − 0.56; d = 0.47), conduct problems subscale (α2 = − 1.29; p < 0.01; 95% CI = − 1.82 to − 0.77; d = 0.68), hyperactivity subscale (α2 = − 1.09; p < 0.01; 95% CI = − 1.82 to − 0.37; d = 0.42) and peer problems subscale (α2 = − 0.95; p < 0.01; 95% CI = − 1.44 to − 0.45; d = 0.43) when compared to baseline levels. The SDQ prosocial scale was the only SDQ subscale that did not follow this trend. Specifically, while there were significant increases in prosocial behavior at post-treatment for the SAU conditions (α1 = 0.58; p = 0.01; 95% CI = 0.12 to 1.04; d = 0.32), improvements were no longer significant at the follow-up time point (α2 = 0.47; p = 0.07; 95% CI = -0.04 to 0.97; d = 0.26). And contrary for the PMTO condition, while there was no significant improvement at post-treatment (α1 + β1 = 0.33; p = 0.18; 95% CI = -0.16 to 0.82; d = 0.18), there was a marginally significant increase at follow-up (α2 + β2 = 0.54; p = 0.02; 95% CI = 0.08 to 1.01; d = -0.30). The effects of PMTO over time on the remaining SDQ subscales generally followed a similar pattern to that of the SAU condition (see Table 2). There was not an additional effect of PMTO over SAU for any of the SDQ behavior dimensions (p > 0.05 for all βt), demonstrating that the two parent treatment interventions have similar positive effects on child behavior.
Parent Outcomes
Parent Efficacy
As assessed by the PSOC, parent efficacy improved in both conditions at post-treatment (α1 = 2.64; p < 0.01; 95% CI = 0.95 to 4.32; d = 0.42) and at follow-up (α2 = 2.92; p < 0.01; 95% CI = 1.32 to 4.53; d = 0.47). There were again no statistically significant differences in effects over time between the PMTO and SAU groups (β1 = − 0.65; p = 0.55 and β2 = − 1.27; p = 0.23), indicating that PMTO and SAU programs have a similar positive effect on parental efficacy over time.
Parent Well-Being
Results of the parent well-being outcomes generally indicated a similar pattern of improvements over time in both conditions, and no difference in improvements between conditions. There were small to moderate effects of time at post-treatment, and increased effects at follow-up for parental stress as measured by the PSS scale score (α1 = − 2.54; p = 0.01; 95% CI = − 4.49 to − 0.59; d = 0.30; α2 = − 3.77; p < 0.01; 95% CI = − 5.59 to − 1.96; d = 0.45), depressive symptoms as measured by the MDI scale score (α1 = − 2.40; p = 0.04; 95% CI = − 4.66 to − 0.14; d = 0.30; α2 = − 2.79; p = 0.02; 95% CI = − 5.08 to − 0.50; d = − 0.45), and self-evaluation as measured by the LOL scale score (α1 = 1.02; p < 0.01; 95% CI = 0.46 to 1.58; d = 0.52; α2 = 1.40; p < 0.01; 95% CI = 0.87 to 1.93; d = 0.72), and sense of coherence as measured by the SOC total scale score (α1 = 1.81; p = 0.02; 95% CI = 0.23 to 3.40; d = 0.25; α2 = 3.33; p < 0.01; 95% CI = 1.77 to 4.90; d = 0.46). There was not an additional effect of PMTO over SAU for any of these outcomes (p > 0.05 for all βt). Thus, parental stress and depression levels statistically significantly decreased, while parental self-evaluation and total sense of coherence statistically significantly increased, regardless of treatment condition. Analyses of the three SOC subscales revealed statistically insignificant effects on the meaningfulness subscale at both time points (α1 = 0.19; p = 0.58; 95% CI = − 0.47 to 0.84; d = 0.08; α2 = 0.63; p = 0.08; 95% CI = − 0.09 to 1.34; d = 0.26). On the comprehensibility subscale, there was a marginally insignificant effect at post-treatment (α1 = 0.73; p = 0.05; 95% CI = − 0.01 to 1.46; d = 0.22) however, there was a statistically significant effect at follow-up (α2 = 1.40; p < 0.01; 95% CI = 0.65 to 2.15; d = 0.43) in both conditions. Again, there were no statistically significant differences between PMTO and SAU conditions in parent well-being at either time point (p > 0.05 for all βt).
Discussion
The aims of this study were to determine the effectiveness of PMTO, as compared to family-based SAU, in a national, clinic-based RCT on child-level (e.g., behavior and functioning) as well as parent- and family-level (e.g., parental efficacy, stress, depressive symptoms, life satisfaction, and sense of cohesion) outcomes immediately after treatment and at follow-up assessment. We hypothesized, given the documented effects of PMTO [9, 11], that PMTO would result in greater improvements in child behavior and functioning as well as improved parental efficacy, life satisfaction, and sense of cohesion, in addition to reduced stress and depressive symptoms at post-treatment compared with family-based SAU. We further hypothesized that these effects would be evident at the 18–20-month follow-up assessments.
Contrary to our hypothesis, we found that PMTO did not differentially improve outcomes relative to the family-based SAU condition for all child and most parent outcomes at post-treatment and at 18–20-month follow-up assessments. These findings were surprising given that previous studies demonstrated benefits of PMTO [56,57,58], but this may be largely a result of these studies’ comparison to a wait-list rather than active treatment control condition. The findings of this study largely mirror the recent quasi-randomized trial in The Netherlands [24] which found no significant difference between PMTO and SAU on child- and parent-levels outcomes. These findings align with findings from Weisz and colleagues’ [59] meta-analysis comparing evidence-based interventions with SAU, which found that evidence-based interventions result in a small effect size relative to SAU (d = 0.29), which becomes attenuated and is non-significant when focusing on clinically referred samples (such as the current study). While there is mixed-evidence in Europe regarding the effectiveness of PMTO as compared to SAU for long-term outcomes, the present study suggest that PMTO does not produce significantly better outcomes, relative to a family-based SAU, for the treatment of behavioral problems in children.
While there were no significant differences between PMTO and family-based SAU, results demonstrate that both interventions result in significant improvements in a host of child outcomes. In particular, as demonstrated in other studies of PMTO, and BPT generally [27, 60], PMTO and SAU were both found to improve behavioral difficulties (i.e., externalizing difficulties, conduct problems) as well as secondary outcomes (i.e., hyperactivity, emotional problems, and internalizing problems). Intervention effects were also evident at follow-up assessments. Moreover, social behaviors and peer problems were significantly improved at post-treatment and were largely maintained at 18–20-month follow-up assessments; however, improvement found on the prosocial scale of the SDQ at post-treatment was not maintained at follow-up assessment.
Effect size data demonstrate that the combined effect of intervention on outcomes were in the small to moderate range (See Table 2); which aligns with previous studies of PMTO and SAU in Nordic countries. Specifically, the range of outcomes for PMTO and SAU on externalizing problems found in previous studies were between 0.47–0.85 and 0.22–0.55, respectively (see [24]). The within-group effect sizes found for externalizing problems (SDQ Externalizing, Conduct, and Hyperactivity subscales) in the current study ranged from 0.34–0.79 for PMTO and family-based SAU at follow-up (see Table 2)—which is on the higher end of the effect size range found in other studies. This is particularly the case for the SAU condition which suggests that family-based interventions used in the current study were notably effective relative to the alternative SAU treatment conditions used in previous trials—a point we discuss further below in future directions.
Parent outcomes followed a similar pattern as child outcomes. While there was no differential effect on PMTO relative to family-based SAU, both interventions improved parental efficacy, parental stress, depressive symptoms, life satisfaction, and aspects of sense of cohesion at immediate post-treatment, with small to moderate effect sizes. These findings largely were maintained at 18–20-month follow-up, with increased effect sizes at follow-up assessment. These findings align with other studies in the Nordic regions demonstrating effects on parenting behaviors, parental stress, and family cohesion and extend the literature by also demonstrating effects on parental depressive symptoms and life satisfaction. The effect size data suggests a small to moderate effect on these outcomes (see Table 2). Importantly, while not often a central target of treatment, as has been argued by others [2, 60,61,62,63] improving parent-level outcomes may be important in order to attenuate the often-seen development of comorbidity or increased severity of problems in youth related to parental stress and mental health issues. Moreover, the results suggest that efforts at improving family-, parent-, and child-level difficulties translate into higher quality of life outcomes as reported by parents. This is an interesting finding and suggests the potential central role that children’s mental health may have in how parents perceive life satisfaction.
Limitations, Clinical Implications and Future Directions
There are notable limitations in this study. This study was a partnership between treatment developers, researchers, service agency administrators, and front-line therapists. Although aspects of the study were well-aligned with traditional efficacy studies and rigorous (e.g., randomized controlled design, high levels of training and supervision by experts, longitudinal assessment of various key constructs), there were also concerns about demands on therapists and agencies and limited funding that constrained aspects of the study. As an example, we did not collect data on therapists, did not utilize observational data, obtain data from other key informants (e.g., teachers), or ascertain treatment dosage of additional interventions that youth may have been involved in (e.g., medication). Additionally, while they were not involved in treatment, assessors were not blind to conditions. Lastly, we tested multiple hypotheses, which can increase the likelihood of incorrectly rejecting a true null effect (i.e., type-I error). To compensate for this, we applied a Bonferroni correction (pbonferroni = p × h) by multiplying p-values (p) with the number of hypotheses (h). Estimated p-values of the five marginally significant estimates changed from less than 0.05 to above 0.05. All other tests were highly significant, so the Bonferroni correction had a negligible impact on these results. Limitations withstanding, the study has several important implications and offers several directions for future investigation.
PMTO has been studied in Nordic countries through non-randomized [24] and randomized [20, 21, 25, 26] trials and has consistently been associated with improved outcomes across child-, parent-, family-level outcomes, with the results of this study suggesting important effects on life satisfaction/quality of life. The current study further supports the utility of PMTO as an intervention for improving both short-term and longer-term functioning in clinic-referred youth with behavioral challenges and their families. Moreover, this study was the most recent clinical trial and is the first RCT to demonstrate that PMTO does not lead to incrementally better outcomes relative to a SAU condition, which aligns with the results of the recent quasi-RCT from The Netherlands [24], with SAU effect size being greater than what was found in the earliest RCTs [20, 21, 25, 26]. The results from both Thijssen and colleagues [24] and the current study suggest that SAU in general, but family-based SAU in particular, is an effective option for addressing behavioral challenges in children. To our knowledge, this is the first study comparing PMTO to a specific SAU approach. These data suggest that process and content of family-based SAU should be further studied to determine in what ways this approach overlaps with and is distinct from PMTO or other evidence-based manualized approaches to treating children’s behavioral challenges. This type of information may further assist in informing the further development of both family-based SAU and PMTO.
Understanding nuances in treatment response for both PMTO and family-based SAU is important to determine if there is differential effectiveness of these approaches as a function of characteristics of the youth, parent and/or family. As an example, Thijssen and colleagues [24] found that youth with greater initial behavioral problems benefited more from PMTO; Ogden and Hagen [20] found that younger children benefited more from PMTO than older children –a finding not replicated in Sigmarsdóttir et al. [26]. Clearly, identifying moderators to treatment response for both PMTO and family-based SAU offers the potential for more tailored treatment allocation. Finally, while treatment effects may be similar across PMTO and family-based SAU, other key outcomes may differ. As an example, the costs associated with evidence-based, manualized interventions may be lower than found in SAU, given that some studies have found that these evidence-based manualized interventions result in the receipt of fewer ancillary services [2, 64, 65]. Moreover, an understudied but growing area of investigation is the unintended side effects (i.e., adverse events) that may potentially be attributed to receipt of BPT interventions [66]. While effectiveness of an intervention is one consideration for determining the utility of an approach in routine service delivery, these and other factors must also be considered.
Summary
In this study, we sought to evaluate PMTO, which is a formal, evidence-based, manualized intervention approach, in comparison to family-based SAU, which is an informal, evidence-informed, unstructured intervention approach routinely utilized in Denmark for addressing behavioral challenges in youth. Outcomes were parent report of child internalizing and externalizing problems, parenting efficacy, parenting stress, sense of coherence, life satisfaction, and depressive symptoms. Outcomes were measured at pretreatment, post-treatment, and 18–20 months post-treatment.
This RCT is the most recent evaluation of PMTO compared to SAU in Denmark. Our results suggested that both PMTO and family-based SAU resulted in significant improvements in child externalizing and internalizing problems, parenting efficacy, as well as parent-reported stress and depressive symptoms, life satisfaction, and aspects of sense of cohesion. Effect sizes at post-treatment and follow-up were in the small to moderate range, consistent with prior PMTO evaluations. However, there were no significant differences between PMTO and family-based SAU. Findings of the study align with the quasi-RCT conducted by Thijssen and colleagues [22] in that PMTO did not result in greater benefits than SAU, which suggests that family-based treatment for children’s behavioral challenges can have similar benefits. Future studies should examine who is best treated with what type of intervention approach to maximize effective and efficient delivery of interventions for families and costs associated with these various approaches.
References
Patterson GR (2005) The next generation of PMTO models. Behav Ther 35:27–33
Chacko A, Alan C, Uderman J, Cornwell M, Anderson L, Chimiklis A (2015) Training parents of children with ADHD. In: Barkley R (ed) Attention deficit hyperactivity disorder. A handbook for diagnosis and treatment, 4th edn. Guilford Press, New York, pp 513–536
Patterson GR, Chamberlain P, Reid JB (1982) A comparative evaluation of a parent-training program. Behav Ther 13:638–650
Patterson GR (2002) The early development of coercive family process. In: Reid JB, Patterson GR, Snyder J (eds) Antisocial behavior in children and adolescents: developmental theories and models for intervention. American Psychological Association, Washington, DC, pp 25–44
Snyder JJ, Patterson GR (1995) Individual differences in social aggression: a test of a reinforcement model of socialization in the natural environment. Behav Ther 26:371–391
Yew SGK, O’Kearney R (2013) Emotional and behavioural outcomes later in childhood and adolescence for children with specific language impairments: meta-analyses of controlled prospective studies. J Child Psychol Psychiatry 54:516–524
DeBaryshe BD, Patterson GR, Capaldi DM (1993) A performance model for academic achievement in early adolescent boys. Dev Psychol 29:795–804
Patterson GR, Brodsky G (1966) A behavior modification programme for a child with multiple problem behaviors. J Child Psychol Psychiatry 7:277–295
Dishion T, Forgatch M, Chamberlain P, Pelham WE III (2016) The Oregon model of behavior family therapy: from intervention design to promoting large-scale system change. Behav Ther 47:812–837
Forgatch MS, Domenech Rodrıguez MM (2016) Interrupting coercion. The iterative loops among theory, science, and practice. In: Dishion TJ, Snyder JJ (eds) Oxford handbook of coercive relationship dynamics. Oxford University Press, New York, pp 194–214
Forgatch MS, Gewirtz AH (2017) The evolution of the Oregon model of parent management training: an intervention for antisocial behavior in children and adolescents. In: Weisz JR, Kazdin AE (eds) Evidence based psychotherapies for children and adolescents, 3rd edn. Guilford Press, New York, pp 85–102
Forgatch MS, Patterson GR (2010) Parent management training-Oregon model: an intervention for antisocial behavior in children and adolescents. In: Weisz JR, Kazdin AE (eds) Evidence based psychotherapies for children and adolescents, 3rd edn. Guilford Press, New York, pp 159–177
Gewirtz AH, DeGarmo DS, Zamir O (2016) Effects of a military parenting program on parental distress and suicidal ideation: after deployment adaptive parenting tools. Suicide Life Threat Behav 46:S23–S31
Patterson GR, Forgatch MS, DeGarmo DS (2010) Cascading effects following intervention. Dev Psychopathol 22:949–970
Gardner F, Montgomery P, Knerr W (2016) Transporting evidence-based parenting programs for child problem behavior (age 3–10) between countries: systematic review and meta-analysis. J Clin Child Adolesc Psychol 45:749–762
Weisz JR, Kuppens S, Ng MY, Vaughn-Coaxum RA, Ugueto AM, Eckshtain D, Corteselli KA (2019) Are psychotherapies for young people growing stronger? Tracking trends over time for youth anxiety, depression, attention-deficit/hyperactivity disorder, and conduct problems. Perspect Psychol Sci 14:216–237
Weisz JR, Ugueto AM, Cheron DM, Herren J (2013) Evidence-based youth psychotherapy in the mental health ecosystem. J Clin Child Adolesc Psychol 42:274–286
Kaminski JW, Claussen AH (2017) Evidence base update for psychosocial treatments for disruptive behaviors in children. J Clin Child Adolesc Psychol 46:477–499
Sigmarsdóttir M, Forgatch MS, Guðmundsdóttir EV, Thorlacius Ö, Svendsen GT, Tjaden J et al (2019) Implementing an evidence-based intervention for children in Europe: evaluating the full-transfer approach. J Clin Child Adolesc Psychol 48:S312–S325
Ogden T, Hagen KA (2008) Treatment effectiveness of parent management training in Norway: A randomized controlled trial of children with conduct problems. J Consult Clin Psychol 76:607–621
Sigmarsdóttir M, Degarmo DS, Forgatch MS, Guðmundsdóttir EV (2013) Treatment effectiveness of PMTO for children's behavior problems in Iceland: assessing parenting practices in a randomized controlled trial. Scand J Psychol 54:468–476
Kjøbli J, Hukkelberg S, Ogden T (2013) A randomized trial of group parent training: reducing child conduct problems in real-world settings. Behav Res Ther 51:113–121
Bjørknes R, Manger T (2013) Can parent training alter parent practice and reduce conduct problems in ethnic minority children? A randomized controlled trial. Prev Sci 14:52–63
Thijssen J, Vink G, Muris P, de Ruiter C (2017) The effectiveness of parent management training—Oregon model in clinically referred children with externalizing behavior problems in The Netherlands. Child Psychiatry Hum Dev 48:136–150
Hagen KA, Ogden T, Bjørnebekk G (2011) Treatment outcomes and mediators of parent management training: a one-year follow-up of children with conduct problems. J Clin Child Adolesc Psychol 40:165–178
Sigmarsdóttir M, Thorlacius Ö, Guðmundsdóttir EV, DeGarmo DS (2015) Treatment effectiveness of PMTO for children's behavior problems in Iceland: child outcomes in a nationwide randomized controlled trial. Fam Process 54:498–517
Chacko A, Scavenius C (2018) Bending the curve: a community-based behavioral parent training model to address ADHD-related concerns in the voluntary sector in Denmark. J Abnorm Child Psychol 46:505–517
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38:581–586
Smedler AC, Tideman E (2011) At teste børn og unge: om tesmetoder i den psykologiske undersøgelse. Hans Reitzels Forlag
Goodman R, Scott S (1999) Comparing the strengths and difficulties questionnaire and the child behavior checklist: is small beautiful? J Abnorm Child Psychol 27:17–24
Mathai J, Anderson P, Bourne A (2004) Comparing psychiatric diagnoses generated by the strengths and difficulties questionnaire with diagnoses made by clinicians. Aust N Z J Psychiatry 38:639–643
Niclasen J, Teasdale TW, Andersen AMN, Skovgaard AM, Elberling H, Obel C (2012) Psychometric properties of the Danish strength and difficulties questionnaire: the SDQ assessed for more than 70,000 raters in four different cohorts. PLoS ONE 7:1–8
Johnston C, Mash EJ (1989) A measure of parenting satisfaction and efficacy. J Clin Child Psychol 18:167–175
Ohan JL, Leung DW, Johnston C (2000) The parenting sense of competence scale: evidence of a stable factor structure and validity. Can J Behav Sci 32:251–261
Kilpatrick FP, Cantril H (1960) Self-anchoring scaling: A measure of individuals' unique reality worlds. J Individ Psychol 16:158–173
Busseri MA, Merrick H (2016) Subjective trajectories for life satisfaction: a self-discrepancy perspective. Motiv Emot 40:389–403
Diener E, Inglehart R, Tay L (2013) Theory and validity of life satisfaction scales. Soc Indic Res 112:497–527
Lucas RE, Donnellan MB (2012) Estimating the reliability of single-item life satisfaction measures: Results from four national panel studies. Soc Indic Res 105:323–331
Antonovsky A (1993) The structure and properties of the sense of coherence scale. Soc Sci Med 36:725–733
Eriksson M, Lindström B (2005) Validity of Antonovsky’s sense of coherence scale: a systematic review. J Epidemiol Community Health 59:460–466
Feldt T, Lintula H, Suominen S, Koskenvuo M, Vahtera J, Kivimäki M (2007) Structural validity and temporal stability of the 13-item sense of coherence scale: prospective evidence from the population-based HeSSup study. Qual Life Res 16:483–493
Berry JO, Jones WH (1995) The parental stress scale: initial psychometric evidence. J Soc Pers Relat 12:463–472
Bech P, Rasmussen NA, Olsen LR, Noerholm V, Abildgaard W (2001) The sensitivity and specificity of the major depression inventory, using the present state examination as the index of diagnostic validity. J Affect Disord 66:159–164
McDowell I (2010) Measures of self-perceived well-being. J Psychosom Res 69:69–79
Socialstyrelsen (2017) Socialstyrelsen vidioportal [Database]. https://socialstyrelsenbuwebu.videoportal.dk
Forgatch MS, Bullock BM, Patterson GR (2004) From theory to practice: increasing effective parenting through role play. The Oregon model of parent management training (PMTO). In: Steiner H, Chang K, Lock J, Wilson J (eds) Handbook of mental health interventions in children and adolescents: an integrated development approach. Jossey-Bass, New York, pp 782–813
Knutson NM, Forgatch MS, Rains LA, Sigmarsdóttir M (2009) Fidelity of implementation rating system (FIMP): the manual for PMTO™. (revised ed) Eugene, OR, Implementation Sciences International, Inc
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Erlbaum, Hillsdale
McNeish D, Kelley K (2019) Fixed effects models versus mixed effects models for clustered data: reviewing the approaches, disentangling the differences, and making recommendations. Psychol Methods 24:20–35
Wooldridge JM (2013) Fixed effects estimation. Introductory econometrics: a modern approach. 466–474
StataCorp (2019) Stata 16 base reference manual. Stata Press, College Station
Arellano M (2003) Panel data econometrics. Oxford University Press, Oxford, UK
Cameron AC, Miller DL (2015) A practitioner’s guide to cluster-robust inference. J Hum Resour 50:317–372
Cameron AC, Trivedi PK (2005) Microeconometrics: methods and applications. Cambridge University Press, Cambridge
Greene WH (2018) Econometric analysis, 8th edn. New York University, Pearson, NY, Stern School of Business
DeGarmo DS, Forgatch MS (2005) Early development of delinquency within divorced families: evaluating a randomized preventive intervention trial. Dev Sci 8:229–239
Forgatch MS, DeGarmo DS (1999) Parenting through change: an effective prevention program for single mothers. J Consult Clin Psychol 67:711–724
Forgatch MS, DeGarmo DS, Beldavs ZG (2005) An efficacious theory-based intervention for stepfamilies. Behav Ther 36:357–365
Weisz JR, Kuppens S, Eckshtain D, Ugueto AM, Hawley KM, Jensen-Doss A (2013) Performance of evidence-based youth psychotherapies compared with usual clinical care: a multilevel meta-analysis. JAMA Psychiatry 70:750–761
Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S et al (2015) Multiple family group service model for children with disruptive behavior disorders: child outcomes at post-treatment. J Emot Behav Disord 23:67–77
Chacko A, Bedard AC, Marks D, Gopalan G, Feirsen N, Uderman J et al (2018) Sequenced neurocognitive and behavioral parent training for the treatment of ADHD in school-age children. Child Neuropsychol 24:427–450
Chacko A, Fabiano GA, Doctoroff GL, Fortson B (2018) Engaging fathers in effective parenting for preschool children using shared book reading: a randomized controlled trial. J Clin Child Adolesc Psychol 47:79–93
Rajwan E, Chacko A, Wymbs BT, Wymbs FA (2014) Evaluating clinically significant change in mother and child functioning: comparison of traditional and enhanced behavioral parent training. J Abnorm Child Psychol 42:1407–1412
Acri M, Gopalan G, Chacko A, Mckay M (2017) Engaging families into treatment for child behavior disorders: a synthesis of the literature. In: Lochman JE, Matthys W (eds) The Wiley handbook for disruptive and impulse-control disorders. Wiley, Hoboken, NJ, pp 393–409
Gopalan G, Small L, Fuss A, Bowman M, Jackson J, Marcus S et al (2015) Multiple family groups to reduce child disruptive behavior difficulties: moderating effects of child welfare status on child outcomes. Child Abuse Negl 46:207–219
Allan C, Chacko A (2018) Adverse events in behavioral parent training for children with ADHD: an under-appreciated phenomenon. ADHD Rep 26:4–9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Scavenius, C., Chacko, A., Lindberg, M.R. et al. Parent Management Training Oregon Model and Family-Based Services as Usual for Behavioral Problems in Youth: A National Randomized Controlled Trial in Denmark. Child Psychiatry Hum Dev 51, 839–852 (2020). https://doi.org/10.1007/s10578-020-01028-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-020-01028-y