Abstract
Small supernumerary marker chromosomes (sSMCs) are structurally abnormal rare chromosomes, difficult to characterize by karyotyping, and have been associated with minor dysmorphic features, azoospermia, and recurrent miscarriages. However, sSMC with a gonosomal trisomy has never been reported. Spermatocyte spreading and immunostaining were applied to detect meiotic prophase I progression, homologous chromosome pairing, synapsis, and recombination. In all the analyzed spermatocytes of the patient, the extra Y chromosome was not detected while the sSMC was present. The recombination frequency on autosomes was not affected, while the recombination frequencies on XY chromosome was significantly lower in the patient than in the controls. The meiotic prophase I progression was disturbed with significantly increased proportion of zygotene and decreased pachytene spermatocytes in the patients as compared with the controls. These findings highlight the importance of studies on meiotic behaviors in patients with an abnormal chromosomal constitution and provide an important framework for future studies, which may elucidate the impairment caused by sSMC in mammalian meiosis and fertility.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Small supernumerary marker chromosomes (sSMC) are reported in 0.075 % of live full-term infants (Liehr and Weise 2007) and can be defined as structurally abnormal chromosomes that cannot be identified or characterized unambiguously by conventional cytogenetic techniques alone and are (in general) equal in size or smaller than chromosome 20 of the same metaphase spread (Liehr et al. 2004). The smaller markers are reported to be associated with minor dysmorphic features, azoospermia, or recurrent miscarriages (Koc et al. 2009). It is always unexpected to find sSMC during cytogenetic diagnostics. However, sSMCs are most often found either in mentally retarded patients with infertility later on in their life or in fetuses who had invasive prenatal diagnosis of some sort (Liehr and Weise 2007).
The 47, XYY karyotype is found in 0.1 % of the general male population with the extra Y chromosome resulted from paternal non-disjunction during meiosis II or a post-zygotic mitotic error (Robinson and Jacobs 1999). The majority of the 47, XYY men are fertile (Linden et al. 1996), and it has been suggested that the extra Y chromosome is lost prior to meiosis in these cases (Shi and Martin 2001). This hypothesis has been supported by studies on sperm aneuploidy in fertile and infertile 47, XYY men, in which more than 95.6 % sperm were chromosomally normal (Blanco et al. 1997; Chevret et al. 1997; Mennicke et al. 1997; Martin et al. 1999; Rives et al. 2003).
Meiotic recombination plays an essential role in the generation of genetic diversity as well as ensuring the accurate segregation of homologous chromosomes during the first meiotic division (Hassold et al. 2000). Several studies using immunocytogenetic techniques have found that a significant proportion of men with impaired spermatogenesis also have abnormalities in the number of recombination events between the chromosomes (Gonsalves et al. 2004; Ma et al. 2006; Ferguson et al. 2007), whereas the others did not find any abnormalities in meiotic recombination in their studied infertile populations (Codina-Pascual et al. 2005; Topping et al. 2006). It has been reported that an inverse correlation exists between the frequency of sex chromosome recombination and XY disomy in the sperm from both fertile and infertile men (Shi et al. 2001; Ferguson et al. 2007). Thus, abnormalities in meiotic recombination may explain the increase in the incidence of aneuploid sperm in severely infertile men (Ferguson et al. 2007).
Here, we are reporting, for the first time, meiotic chromosome behavior in a patient with a complex karyotype of 48, XYY, +sSMC. Our results indicated that only one Y chromosome was present in spermatocytes of the patient, and the presence of sSMC may interfere with the recombination between the sex chromosomes and meiotic prophase I progression.
Methods
Patient and karyotype analysis
A 40-year-old male was presented to Center for Reproductive Medicine at Drum Tower Hospital affiliated to Nanjing University Medical College, Nanjing, China. Semen analysis was done according to World Health Organization criteria (WHO laboratory manual for the examination of human semen and semen-cervical interaction, 2010). After obtaining informed consent from patient, testicular tissue was sampled for biopsy analysis. Five fertile men (average age 58 ± 16 years) of Han ethnicity, having at least one healthy child, were recruited as normal controls for this study, and similar experiments were performed on them as mentioned for the patient. All the procedures of this study were approved by the institutional review board and ethical committee of the University of Science and Technology of China.
Spermatocyte spreads and immunostaining
Testicular tissues were processed as we described previously (Pan et al. 2012; Jiang et al. 2014). The Rabbit anti-SYCP3 (Abcam, Cambridge, UK), Human anti-CREST (ImmunoVision, Springdale, AR), Mouse anti-MLH1 (BD Pharmingen Biosciences, San Diego, CA), mouse anti-γ-H2AX (Millipore, Billerica, MA), Goat anti-SYCP1 (Santa Cruz Biotechnology, CA, USA), Alexa 555 donkey anti-rabbit (Molecular Probes, Carlsbad, CA), Alexa 488 goat anti-mouse (Molecular Probes, Carlsbad, CA), Alexa 488 donkey anti-mouse (Molecular Probes, Carlsbad, CA) and 1-amino-4-methylcoumarin-3-acetic acid (AMCA) donkey anti-human (Jackson ImmunoResearch, West Grove, PA) were used for the detection of their respective primary antibodies.
The number of centromeres and synaptonemal complexes (SCs) was counted in spermatocytes. Recombination on autosomes as well as on XY bivalents was enumerated for the patient and controls.
Statistical analysis
All the data is presented as mean ± standard deviation (SD). Significance level was set as P < 0.05. Statistical analysis was carried out by using SPSS 13.0 software (SPSS Inc., Chicago, IL). The chi-square test was applied to compare the rate of recombination between the patient and controls. The Mann–Whitney test was applied for the comparison of MLH1 foci per cell between the patient and controls.
Results
Analysis of the semen revealed that the patient was suffering from azoospermia. Karyotyping on G-banded metaphases of peripheral blood lymphocytes revealed a karyotype of 48, XYY, +sSMC in all the 100 studied cells of the patient (Fig. 1).
The extra Y chromosome was not observed in spermatocytes of 48, XYY, +sSMC patient
The number of SCs and centromeres in pachytene spermatocytes with distinguishable autosomes and sex chromosomes was counted in the patient and control individuals. Each cell from the control men showed 24 centromere signals on 22 autosomal SCs and the X and Y chromosomes, while for the patient, 25 centromere signals were observed on 22 autosomal SCs, X, Y, and the small marker chromosome for all the 80 spermatocytes analyzed (Fig. 2a, b). These results indicate that the extra Y chromosome was lost in the spermatocytes of the patient. To confirm that the observed Y chromosome was a univalent but not bivalent formed by complete synapsis of two Ys in the spermatocytes of the patient, these cells were immunostained for SYCP1, a typical central element of SCs. In all the 80 cells analyzed, no SYCP1 signals were observed along the Y chromosome (Fig. 2c, d). Together, our results indicated that the extra Y chromosome was lost from spermatocytes of the 48, XYY, +sSMC patient.
The extra Y chromosome was lost from spermatocytes of the 48, XYY, +sSMC male. Images of a representative pachytene spermatocyte (a and c) immunostained for CREST (blue), SYCP3 (red), MLH1 (green), and SYCP1 (green in c and d). Twenty-five centromere signals were detected and no SYCP1 signals were observed along the X, Y chromosome and sSMC in all the 80 cells with recognizable chromosomes. b and d are enlarged areas shown in a and c, respectively. Arrows indicate the sSMC. Scale bar = 5 μm
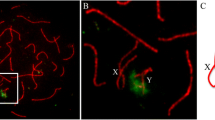
In all the 80 spermatocytes of the patient, the association and recombination between the sex chromosomes were also determined and compared with the control. In the patient, X-Y chromosomes were found to be associated in 83.7 % cells, while in 16.3 % spermatocytes, they were not associated. In control individuals, X and Y were associated in 80.4 % cells and were not associated in 19.5 % cells (Fig. 3), which is not statistically different from the patient (P > 0.05, chi-square test). In the patient, recombination between the sex chromosomes (represented by MLH1 focus) was observed to be present always in the PAR1 region as in controls; however, it occurs in 57.5 % cells, which is significantly lower than that in control individuals (Table 1). These results indicated that the pairing of XY chromosomes was not affected but their recombination was impaired in the patient.
The sex chromosome pairing was normal in the 48, XYY, + sSMC patient. Early pachytene spermatocyte spreads from the control (a–b) and the patient (c–d) were immunostained for SYCP3 (red), MLH1 (green), and CREST (blue). Representative images of early pachytene spermatocytes showing associated (b and d) or not associated (a and c) X and Y chromosomes. White arrows indicate marker chromosome while the yellow arrows indicate pseudoautosomal region (PAR) on X and Y chromosomes. Scale bar = 5 μm
The behavior of the marker chromosome
In the 80 spermatocytes of the patient, the small marker chromosome was always observed (Fig. 2). In 73.7 % of the cells, the small marker chromosome was not associated with any chromosome including sex chromosomes, while in 26.3 % spermatocytes, it was associated either with the X or Y chromosome (Fig. 4). In the latter 26.3 % spermatocytes, the marker chromosome was observed to be associated with X in 52 % and with Y in 48 % of the cells, but no SYCP1 signals were observed along it (data not shown here).
Representative images of spermatocytes showing that sSMC is associated with the sex chromosomes. Spermatocyte spreads were immunostained for CREST (blue), SYCP3 (red), and MLH1 (green). The marker chromosome is associated (26.3 %) (b) or not associated (73.7 %) (a) with the XY chromosomes in all the 80 pachytene spermatocytes analyzed. Arrows indicate sSMC. Scale bar = 5 μm
It has been documented that the chromosomes or chromosome regions that had not experienced synapsis undergo inactivation and are decorated by γ-H2AX signals in spermatocytes (Mahadevaiah et al. 2001; Baarends et al. 2005; Turner et al. 2005). To understand whether the small maker chromosome in the patient also had the similar property, we stained the spermatocytes for the γ-H2AX. In all the 54 spermatocytes with recognizable sSMC, γ-H2AX signals were always observed in the unsynapsed regions of X and Y chromosomes as expected and also in the entire sSMC, no matter whether it was associated with the XY body or not (Supplementary Fig. 1).
To understand whether the meiotic progression in the 48, XYY, +sSMC patient was affected or not, a total of 209 spermatocytes from the patient and 1795 from five controls were analyzed. An increase in zygotene (P < 0.001) and decrease in the pachytene spermatocytes (P < 0.001) were observed in the patient when compared with the controls (Fig. 5d).
Meiotic progression was disturbed in the 48, XYY, +sSMC patient. Spermatocyte spreads were immunostained for SYCP3 (red), MLH1 (green), and CREST (blue). Leptotene (a). Zygotene (b). Pachytene (c). The arrow indicates marker chromosome. N the number of cells analyzed; ***P < 0.001, chi-square test. Scale bar = 5 μm
The recombination on the autosomes was also examined by counting MLH1 foci on all SCs in spermatocytes of the 48, XYY, +sSMC patient and normal controls. As shown in Table 1, almost similar recombination frequencies were observed in the two groups (48.9 in patient vs. 48.0 in control).
Discussion
sSMCs are clinically heterogeneous group; the same holds true for their chromosomal origin and morphology (Liehr et al. 2006; Tsuchiya et al. 2008). sSMC can be derived from any of the 24 human chromosomes and appears as inverted duplicated-, ring-, or centric minute shaped derivative chromosomes (Tsuchiya et al. 2008; Liehr 2009). They are difficult to recognize because of their small size and gradual loss in mitosis (Michalski et al. 1993). In clinical genetics, it is useful to elucidate the phenotypic effects of sSMCs because of their implications in the genetic counselling, especially in cases seeking artificial reproduction assistance (Marle et al. 2014). Presence of sSMC and XYY at the same time is rarely observed, and its origin and effects on spermatogenesis are not yet clear. We have reported a 48, XYY, +sSMC patient and analyzed his meiosis in detail to find the possible sSMC association with meiosis.
The majority of 47, XYY men are reported to be fertile (Linden et al. 1996), and the extra Y chromosome in these patients has been suggested to be lost prior to meiosis (Shi and Martin 2001). This was supported by studies on chromosomal constitution of sperm in 47, XYY. Furthermore, Gabriel-Robez et al. (1996) had observed loss of the extra Y chromosome in all the analyzed pachytene nuclei of a 47, XYY patient with normal sperm count. However, Solari and Valzacchi (1997) reported that a 47, XYY male with extremely low sperm count contained the extra Y in all the pachytene nuclei analyzed. Using immunocytogenetic technique, we observed that only one Y chromosome was present in spermatocytes of the 48, XYY, +sSMC (Fig. 2). Moreover, the patient was normal for the pairing between the X and Y chromosomes (Fig. 3), although their recombination rate was lower in the patient than in normal controls (Table 1).
Homologous chromosome pairing and synapsis are the most typical features of meiosis and ensure that the two DNA molecules from homologous chromosomes happen to come close enough to repair programmed DNA double-strand breaks during meiotic prophase I. Meiotic chromosome pairing and synapsis, because of their accuracy, have been used to detect homology between chromosomes or chromosomal regions in mammals and plants (McKee 2004; Gerton and Hawley 2005). In spermatocytes of our 48, XYY, +sSMC patient, we found that the small marker chromosome was present in all the spermatocytes examined and was randomly associated either with X or Y chromosome but not with autosomes (Fig. 4b), indicating that the sSMC may not be derived from autosomes. It has been reported previously that all unsynapsed material, irrespective of its genetic origin, associates with the XY bivalent as a result of meiotic silencing (Burgoyne et al. 2009; Kurahashi et al. 2012), and this could be one of the possible reasons why sSMC was found associated with sex chromosomes but not with autosomes in our 48, XYY patient. Interestingly, we did not detect any SYCP1 signals in the region where sSMC was associated with X or Y chromosome (Fig. 2). Thus, the chromosomal origin of sSMC in our patient remains unknown. One possible reason for this is that the sSMC was formed from fragments of different chromosomes, and each fragment was too small to synapse with its homologous regions.
In our study, initial stages of meiotic chromosome restructuring were apparently not affected by sSMC as assembly of axial elements appears normal in all tested cells. Except for the sSMC, homologous chromosome recognition and pairing in the patient apparently proceeded as in normal controls. The sSMC was often associated with X or Y chromosome in the patient. A gradual increase in quadrivalent–sex body (SB) association through the meiotic prophase has been described in human reciprocal or Robertsonian translocation carriers (Gabrielrobez et al. 1986; Navarro et al. 1991; Yu et al. 1995; Leng et al. 2009; Jiang et al. 2014). Different hypotheses have been suggested to explain this association and its possible consequences. According to an early model (Lifschyt and Lindsley 1972), the association would interfere in the normal sex chromosome inactivation, reversing this process would allow inappropriate expression of genes located in the X chromosome. Meiotic sex chromosome inactivation (MSCI) is triggered by the phosphorylation of the histone H2AX by the kinase ATR, which is BRCA1 dependent (Turner et al. 2004; Baarends et al. 2005). At the pachytene stage of normal men, γ-H2AX disappears from the completely synapsed autosomes and appears only in the XY body (Sciurano et al. 2006; Sciurano et al. 2007; Leng et al. 2009). In pachytene spermatocytes of our patient, γ-H2AX staining appeared in the chromatin domains of the XY body as well as in the sSMC (Supplementary Fig. 1).
Shi et al. (2001) had reported that reduced XY recombination would result in non-disjunction, leading to 24, XY sperm in 47, XYY patients. To investigate the impact of the sSMC on the progression of meiotic recombination events, we analyzed the patient for the recombination events. We found no significant difference in the number of MLH1 foci on autosomes in the patient compared to normal controls (Table 1). However, the recombination on XY chromosome in the patient was more significantly decreased than in the controls (Table 1). Individual variations have been reported for both patients and controls regarding the mean number of MLH1 foci on autosomes and sex chromosomes in the spermatocytes of both control and patients. Sun et al. (2004) has reported mean frequency of 49.8 ± 4.3 of autosomal recombination foci in a 47-year-old control having 73 % MLH1 foci on XY bivalent. While Codina-Pascual et al. (2005) has studied the meiotic progression in four patients with azoospermia and six patients suffering from oligoasthenozoospermia. They have reported that the mean MLH1 foci per cell were similar in patients (47.3) and controls (48.8) for autosomes. Upon comparison of recombination between sex chromosomes, they had observed decreased mean MLH1 foci (% cells) in patients (59.2 %) as compared to the controls (69.9 %). It was observed that number of MLH1 foci on X-Y chromosome was different in patients suffering from azoospermia (61.7 %) and oligoasthenozoospermia (59.2 %) indicating that MLH1 foci number varies with the underlying type of infertility. Similarly Barlow and Hulten (1998) have reported crossing over analysis at pachytene in a 45-year-old man with proven fertility and have documented that mean number of MLH1 foci were 50.9 on autosomal and 56.5 on sex chromosomes. The results reported in the abovementioned studies are similar to what we have observed in our subject during the present study. Sun et al. (2008) has also reported decreased mean MLH1 foci (% cells) in seven patients with non-obstructive azoospermia (77.7 %) as compared to controls (86.2 %) on sex chromosomes. The mean number of MLH1 foci (% cells) in this study is higher for both patients and controls than the data we have presented, and Sun et al. (2008) has reported that despite having 77.7 % MLH1 foci on sex chromosomes, the patients suffered from reduced meiotic recombination on the XY bivalent confirming that there is no specific range for MLH1 foci per cell for both autosomes as well as sex chromosomes and the number of MLH1 foci varies from person to person.
As the sSMC was observed in all the 80 studied spermatocytes and recombination on XY chromosomes was found to be more significantly decreased in the patient than in the controls, so we studied the association of sSMC with sex chromosomes in order to determine whether there is any association between presence of sSMC and reduced XY recombination. In 73.7 % (N = 59) of the 80 studied spermatocytes, sSMC was not found associated with any chromosome including sex chromosomes, while in 26.3 % spermatocytes, it was associated either with the X or Y chromosome (Fig. 4). In the latter 26.3 % spermatocytes (N = 21), sSMC was observed to be associated with X [in 52 % spermatocytes, N = 11)] and Y [in 48 % spermatocytes (N = 10)] but no SYCP1 signals were observed along them. We further calculated the MLH1 foci in spermatocytes where sSMC was associated with X or Y chromosomes, and we observed that 16 out of 80 (20 % of total) spermatocytes had sSMC associated with X-Y chromosomes and they still had MLH1 foci on them. While five out of 80 (6.2% of total) spermatocytes had sSMC associated with X-Y chromosomes, they had no MLH1 foci on them. These results indicate that the presence of sSMC has not apparently disturbed the recombination between X-Y chromosomes and further studies are recommended to determine the effect of sSMC on the events associated with meiosis.
To evaluate the effect of sSMC in prophase I progression, we quantified the number of spermatocytes in each stage of prophase I of the patient. The presence of a high proportion of cells in zygotene and low pachytene spermatocyte number indicates disturbed meiotic progression (Fig. 5d) which is probably due to change in the testicular environment due to the presence of sSMC but how it has disturbed the meiotic progression is not clear and has not been investigated further because the testicular tissues from the patient were not always available.
In conclusion, we have described a rare example of abnormal chromosome associated with male infertility. We have reported that the extra Y chromosome was not observed in pachytene spermatocytes of 48, XYY patient while the small marker chromosome was present in all studied spermatocytes, and in some of the cells, it was found associated with sex chromosome. These results indicate that the presence of sSMC may lead to a phenotype with significantly disturbed spermatogenesis and infertility but the underlying mechanism is not yet understood. Hence, this work provides an important framework for future studies, which may elucidate the impairment caused by sSMC in mammalian meiosis and fertility.
Abbreviations
- sSMC:
-
Small supernumerary marker chromosome
- SCs:
-
Synaptonemal complexes
- SD:
-
Standard deviation
- DSBs:
-
Double-strand breaks
- SB:
-
Sex body
- MSCI:
-
Meiotic sex chromosome inactivation
References
Baarends WM, Wassenaar E, van der Laan R, Hoogerbrugge J, Sleddens-Linkels E, Hoeijmakers JHJ, de Boer P, Grootegoed JA (2005) Silencing of unpaired chromatin and histone H2A ubiquitination in mammalian meiosis. Mol Cell Biol 25(3):1041–1053
Barlow AL, Hulten MA (1998) Crossing over analysis at pachytene in man. Eur J Hum Genet 6:350–358
Blanco J, Rubio C, Simon C, Egozcue J, Vidal F (1997) Increased incidence of disomic sperm nuclei in a 47, XYY male assessed by fluorescent in situ hybridization (FISH). Hum Genet 99:413–416
Burgoyne PS, Mahadevaiah SK, Turner JMA (2009) The consequences of asynapsis for mammalian meiosis. Nat Rev Genet 10:2017–2216
Chevret E, Rousseaux S, Monteil M, Usson Y, Cozzi J, Pelletier R, Sele B (1997) Meiotic behaviour of sex chromosomes investigated by three-colour FISH on 35142 sperm nuclei from two 47, XYY males. Hum Genet 99:407–412
Codina-Pascual M, Oliver-Bonet M, Navarro J, Campillo M, Garcia F, Egozcue S, Abad C, Egozcue J, Benet J (2005) Synapsis and meiotic recombination analyses: MLH1 focus in the XY pair as an indicator. Hum Reprod 20:2133–2139
Ferguson KA, Wong EC, Chow V, Nigro M, Ma S (2007) Abnormal meiotic recombination in infertile men and its association with sperm aneuploidy. Hum Mol Genet 16:2870–2879
Gabrielrobez O, Ratomponirina C, Dutrillaux B, Carrepigeon F, Rumpler Y (1986) Meiotic association between the XY chromosomes and the autosomal quadrivalent of a reciprocal translocation in 2 infertile men, 46, XY, t(19–22) and 46, XY, t(17–21). Cytogenet Cell Genet 43:154–160
Gabriel-Robez O, Delobel B, Croquette MF, Rigot JM, Djlelati R, Rumpler Y (1996) Synaptic behaviour of sex chromosome in two XYY men. Ann Genet 39:129–132
Gerton JL, Hawley RS (2005) Homologous chromosome interactions in meiosis: diversity amidst conservation. Nat Rev Genet 6:477–487
Gonsalves J, Sun F, Schlegel PN, Turek PJ, Hopps CV, Greene C, Martin RH, Pera RA (2004) Defective recombination in infertile men. Hum Mol Genet 13:2875–2883
Hassold T, Sherman S, Hunt P (2000) Counting cross-overs: characterizing meiotic recombination in mammals. Hum Mol Genet 9:2409–2419
Jiang H, Wang L, Cui Y, Xu Z, Guo T, Cheng D, Xu P, Yu W, Shi Q (2014) Meiotic chromosome behavior in a human male t(8;15) carrier. J Genet Genom 41:177–185
Koc A, Onur SO, Ergun MA, Percin EF (2009) Supernumerary marker chromosome 15 in a male with azoospermia and open bite deformity. Asian J Androl 11:617–622
Kurahashi H, Kogo H, Tsutsumi M, Inagaki H, Ohye T (2012) Failure of homologous synapsis and sex-specific reproduction problems. Front Genet 3:1–11
Leng M, Li G, Zhong L, Hou H, Yu D, Shi Q (2009) Abnormal synapses and recombination in an azoospermic male carrier of a reciprocal translocation t(1;21). Fertil Steril 91(1293):e1217–e1222
Liehr T (2009) Small supernumerary marker chromosomes (sSMCs): a spotlight on some nomenclature problems. J Histochem Cytochem 57:991–993
Liehr T, Weise A (2007) Frequency of small supernumerary marker chromosomes in prenatal, newborn, developmentally retarded and infertility diagnostics. Int J Mol Med 19:719–731
Liehr T, Claussen U, Starke H (2004) Small supernumerary marker chromosomes (sSMC) in humans. Cytogenet Genome Res 107:55–67
Liehr T et al (2006) Small supernumerary marker chromosomes—progress towards a genotype-phenotype correlation. Cytogenet Genome Res 112:23–34
Lifschyt E, Lindsley DL (1972) Role of X-chromosome inactivation during spermatogenesis. Proc Natl Acad Sci U S A 69:182
Linden MG, Bender BG, Robinson A (1996) Intrauterine diagnosis of sex chromosome aneuploidy. Obstet Gynecol 87:468–475
Ma S, Ferguson KA, Arsovska S, Moens P, Chow V (2006) Reduced recombination associated with the production of aneuploid sperm in an infertile man: a case report. Hum Reprod 21:980–985
Mahadevaiah SK, Turner JM, Baudat F, Rogakou EP, de Boer P, Blanco-Rodriguez J, Jasin M, Keeney S, Bonner WM, Burgoyne PS (2001) Recombinational DNA double-strand breaks in mice precede synapsis. Nat Genet 27:271–276
Marle N et al (2014) Molecular characterization of 39 de novo sSMC: contribution to prognosis and genetic counselling, a prospective study. Clin Genet 85:233–244
Martin RH, McInnes B, Rademaker AW (1999) Analysis of aneuploidy for chromosomes 13, 21, X and Y by multicolour fluorescence in situ hybridisation (FISH) in a 47, XYY male. Zygote 7:131–134
McKee BD (2004) Homologous pairing and chromosome dynamics in meiosis and mitosis. Biochim Biophys Acta 1677:165–180
Mennicke K, Diercks P, Schlieker H, Bals-Pratsch M, Al Hasani S, Diedrich K, Schwinger E (1997) Molecular cytogenetic diagnostics in sperm. Int J Androl 20:11–19
Michalski K, Rauer M, Williamson N, Perszyk A, Hoo JJ (1993) Identification, counselling, and outcome of two cases of prenatally diagnosed supernumerary small ring chromosomes. Am J Med Genet 46:88–94
Navarro J, Vidal F, Benet J, Templado C, Marina S, Egozcue J (1991) XY trivalent association and synaptic anomalies in a male carrier of a Robertsonian T(13, 14) translocation. Hum Reprod 6:376–381
Pan ZZ, Yang QL, Ye N, Wang L, Li JH, Yu DX, Cooke HJ, Shi QH (2012) Complex relationship between meiotic recombination frequency and autosomal synaptonemal complex length per cell in normal human males. Am J Med Genet A 158A:581–587
Rives N, Simeon N, Milazzo JP, Barthelemy C, Mace B (2003) Meiotic segregation of sex chromosomes in mosaic and non-mosaic XYY males: case reports and review of the literature. Int J Androl 26:242–249
Robinson DO, Jacobs PA (1999) The origin of the extra Y chromosome in males with a 47, XYY karyotype. Hum Mol Genet 8:2205–2209
Sciurano RB, Rahn MI, Pigozzi MI, Olmedo SB, Solari AJ (2006) An azoospermic man with a double-strand DNA break-processing deficiency in the spermatocyte nuclei: case report. Hum Reprod 21:1194–1203
Sciurano R, Rahn M, Rey-Valzacchi G, Solari AJ (2007) The asynaptic chromatin in spermatocytes of translocation carriers contains the histone variant gamma-H2AX and associates with the XY body. Hum Reprod 22:142–150
Shi Q, Martin RH (2001) Aneuploidy in human spermatozoa: FISH analysis in men with constitutional chromosomal abnormalities, and in infertile men. Reproduction 121:655–666
Shi QH, Spriggs E, Field LL, Ko E, Barclay L, Martin RH (2001) Single sperm typing demonstrates that reduced recombination is associated with the production of aneuploid 24, XY human sperm. Am J Med Genet 99:34–38
Solari AJ, Rey Valzacchi G (1997) The prevalence of a YY synaptonemal complex over XY synapsis in an XYY man with exclusive XYY spermatocytes. Chromosom Res 5:467–474
Sun F, Oliver-Bonet M, Liehr T, Starke H, Ko E, Rademaker A, Navarro J, Benet J, Martin RH (2004) Human male recombination maps for individual chromosomes. Am J Hum Genet 74:521–531
Sun F, Mikhaail-Philips M, Oliver-Bonet M, Ko E, Rademaker A, Turek P, Martin RH (2008) Reduced meiotic recombination on the XY bivalent is correlated with an increased incidence of sex chromosome aneuploidy in men with non-obstructive azoospermia. Mol Hum Reprod 14:399–404
Topping D, Brown P, Judis L, Schwartz S, Seftel A, Thomas A, Hassold T (2006) Synaptic defects at meiosis I and non-obstructive azoospermia. Hum Reprod 21:3171–3177
Tsuchiya KD, Opheim KE, Hannibal MC, Hing AV, Glass IA, Raff ML, Norwood T, Torchia BA (2008) Unexpected structural complexity of supernumerary marker chromosomes characterized by microarray comparative genomic hybridization. Mol Cytogenet 1:7
Turner JM, Aprelikova O, Xu X, Wang R, Kim S, Chandramouli GV, Barrett JC, Burgoyne PS, Deng CX (2004) BRCA1, histone H2AX phosphorylation, and male meiotic sex chromosome inactivation. Curr Biol 14:2135–2142
Turner JM, Mahadevaiah SK, Fernandez-Capetillo O, Nussenzweig A, Xu X, Deng CX, Burgoyne PS (2005) Silencing of unsynapsed meiotic chromosomes in the mouse. Nat Genet 37:41–47
Yu WR, Gabriel-Robez O, Croquette MF, Rigot JM, Rumpler Y (1995) XY-quadrivalent association and sterility in a man carrier of a reciprocal autosomal translocation involving the whole arm of an acrocentric chromosome t(2;15)(q21.3;cen). Andrologia 27:171–174
Acknowledgments
We gratefully acknowledge the patients for the sample donation during this study.
Conflict of interest
All the authors declare that they have no conflict of interest of any sort with anyone.
Funding
This work was supported by the National Basic Research Program (2013CB947900 and 2014CB943101) of China (973), by grants from National Natural Science Foundation of China (31371519, 31301227 and 313111245) and the Knowledge Innovation Program of the Chinese Academy of Sciences (KSCX2-EW-R-07).
Authors’ contributions
L.W. and Q.S. conceived the idea and coordinated the project. Z.X. and C.W. collected the samples. Y.Z. and I.B. organized the data. G.Z. and L.Z. had performed the karyotyping. L.W. analyzed the data. H.J.C., H.J., and F.I. wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: Wendy Bickmore
Liu Wang and Zhipeng Xu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
sSMCs were stained positive for γ-H2AX in spermatocytes. Immunostaining for SYCP3 (red) (A), MLH1 (green) and γ-H2AX (green) (B), CREST (blue) (C) and Merge (D), in a representative mid-pachytene spermatocyte. In all the 54 spermatocytes, in which sSMC was recognizable, γ-H2AX signals were always seen in the sSMC as well as the unsynapsed XY regions. Arrow indicate sSMC. Scale bar = 5 μm. (GIF 44 kb)
Rights and permissions
About this article
Cite this article
Wang, L., Xu, Z., Iqbal, F. et al. Decreased XY recombination and disturbed meiotic prophase I progression in an infertile 48, XYY, +sSMC man. Chromosome Res 23, 267–276 (2015). https://doi.org/10.1007/s10577-015-9465-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10577-015-9465-9