Abstract
Selective mutism (SM) is a relatively rare childhood disorder characterized by a consistent failure to speak in specific settings (e.g., school, social situations) despite speaking normally in other settings (e.g., at home). The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) lists SM among the anxiety disorders. This makes sense as the current review of the literature confirms that anxiety is a prominent symptom in many children suffering from this condition. Further, research on the etiology and treatment of SM also corroborates the conceptualization of SM as an anxiety disorder. At the same time, critical points can be raised regarding the classification of SM as an anxiety disorder. We explore a number of such issues in this review. Recommendations for dealing with this diagnostic conundrum are made for psychologists, psychiatrists, and other mental health workers who face children with SM in clinical practice, and directions for future research are highlighted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Selective mutism (SM) is a psychiatric condition typically occurring during childhood that is characterized by an absence of speech in specific public situations in which the child is expected to speak (e.g., school, social situations), while in other situations (e.g., at home), the child’s production of speech is apparently quite normal. To establish the diagnosis, DSM-5 (APA 2013) specifies that the selective absence of speech should be present for at least 1 month. Many young children are worried when confronted with a totally new situation, such as entering school for the first time, and therefore, the diagnosis is not made during the first month at school. A certain degree of reticence—which can manifest itself as a lack of speech or a failure to speak—can be considered normal from a developmental point-of-view. Further, in DSM-5, the failure to speak is not attributable to a lack of knowledge of, or discomfort with, the spoken language required in the social situation. Moreover, the disturbance is not better explained by a communication disorder (e.g., childhood-onset fluency disorder) and does not occur exclusively during the course of autism spectrum disorder, schizophrenia, or another psychotic disorder. Finally, there should be interference with daily functioning: The absence of speech hinders the child to function well at school or in social interactions (APA 2013).
Available research has indicated that SM is relatively rare. For example, Carlson et al. (1994) mailed a survey to 962 child and adolescent psychiatrists with the request to indicate whether they had ever diagnosed and treated young people with SM. On the basis of responses to this mailing, it was estimated that the prevalence of the condition was less than 1 % (i.e., 0.11 %) as judged by this professional group. Adopting a comparable approach in clinics in Germany and Switzerland, Steinhausen and Juzi (1996) obtained prevalence rates of 0.54 and 0.47 %, respectively. Other studies have relied on school samples by asking teachers to identify mute children in their classrooms. Such a procedure may provide a more accurate estimate of the frequency of SM because it also takes into account children for whom parents do not seek professional help and treatment. Still, studies adopting such an approach have obtained prevalence rates for SM ranging between 0.18 and 1.90 % (Bergman et al. 2002; Elizur and Perednik 2003; Kopp and Gillberg 1997; Kumpulainen et al. 1998), depending on the strictness of the diagnostic criteria that are employed (see Viana et al. 2009). Further, some (but certainly not all) studies have documented that SM is somewhat more prevalent among girls than among boys, with an average ratio of 2:1 (Dummit et al. 1997).
SM is a problem typically occurring in early childhood: The mean age-of-onset varies between 2 and 5 years, but symptoms may become most manifest when children enter school for the first time and the problem persists at least 1 month. Research in which children with SM are followed for a longer time period shows that the disorder has a mean duration of 8 years, after which the key symptom (i.e., total absence of speech in specific situations) normally dissipates if not disappears completely (Remschmidt et al. 2001). This does not mean, however, that children no longer have problems. Studies have demonstrated that children who have previously suffered from SM, later on in their development (even in adulthood), continue to have communication problems, perform less well at school or work, and display higher rates of psychiatric disorders (Remschmidt et al. 2001; Steinhausen et al. 2006).
In the past, this psychiatric condition was known as “voluntary aphasia” (Kussmaul 1877) and later as “elective mutism” (Tramer 1934), labels which both suggest that a child with this condition intentionally chooses not to speak in certain situations or with certain people. With the introduction of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; APA 1994), “elective” was replaced by “selective,” which is more neutral about the child’s motives and puts the emphasis on the fact that the lack of speech only occurs in particular contexts or settings. This is also better in accord with the latest edition of the DSM (i.e., DSM-5; APA 2013) in which SM is listed among the anxiety disorders, suggesting that children with this problem are wary of speaking rather than not wanting to speak in specific situations.
Excellent reviews have appeared in the psychological literature that led up to the decision to classify SM as an anxiety disorder in DSM-5 (Anstedig 1998; Cohan et al. 2006; Sharp et al. 2007; Viana et al. 2009), but the last of these reviews was published more than 5 years ago. Now that its new diagnostic status has been officially formalized, the time has come for an up-to-date review on SM and recent developments. The present article is specifically focused on the link between anxiety and this psychiatric condition. First, studies will be summarized that have explored the involvement of anxiety in SM. Next, an overview is provided of the factors that are thought to be implicated in the origins of SM, with special attention to those variables that may play a role in the etiology of anxiety pathology. Then, the evidence for effective treatment options of SM will be summarized, again looking for commonalities with interventions that have proven to be successful for the anxiety disorders more broadly. Finally, some critical points will be made regarding the current DSM-5 classification of SM as an anxiety disorder, and possible solutions will be offered for dealing with this diagnostic conundrum.
SM and Anxiety
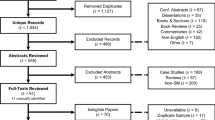
A literature search in Web of Science using (elective mutism/selective mutism in title) AND (anxiety in topic) as the target keywords yielded 110 publications. A close examination of these publications identified 21 relevant research articles on the relation between SM and anxiety. As can be seen in Table 1, a number of papers were descriptive in nature and merely assessed anxiety symptoms or anxiety disorder diagnoses in samples of children with SM. In the study by Steinhausen and Juzi (1996) who analyzed 100 children with this disorder, clinicians noted that the vast majority (66 %) showed comorbid symptoms of anxiety. In an investigation by Ford et al. (1998) that included 153 individuals with SM (101 of whom had the disorder at the time of the study and 52 had SM in the past), a considerably smaller percentage was documented; that is, in only 12 % of the cases, the clinician explicitly reported the presence of anxiety-related problems (e.g., anxiety, panic attacks, social phobia). However, there were several pieces of evidence that suggested the possible involvement of anxiety. To begin with, many of the individuals already reported that they had displayed anxiety-related behaviors such as shyness, withdrawal, and avoidance prior to the onset of their SM. Further, on standardized psychopathology questionnaires such as the Child Behavior Checklist (CBCL; Achenbach 1991), anxiety-related items (e.g., “worries,” “too fearful or anxious,” “fears certain animals, situations or places, other than school,” “shy or timid”) were frequently endorsed. Finally, the speech of these individuals was characterized by a low frequency of words, low volume, and less spontaneity, which strongly resembled that of individuals with a social phobia.
In the study by Cohan et al. (2008), parents of 130 children with SM (aged between 5 and 12 years) completed a set of questionnaires. The Selective Mutism Questionnaire (SMQ; Bergman et al. 2008) was used as an index of SM symptom severity, the Social Anxiety Scale for Children-Revised (SASC-R; La Greca and Stone 1993) was enlisted to assess social anxiety symptoms, and the anxiety problems subscale of the CBCL was used to measure general anxiety symptoms. The results indicated that SM symptom severity was modestly but significantly correlated with social anxiety (r = 0.25) and general anxiety (r = 0.27) symptoms. On first sight, this suggests that social anxiety may not have a strong link with SM. However, it should be kept in mind that most of the SM children included in this study “scored in the clinically significant range for social anxiety” (p. 775), implying that the variation in SASC-R scores was quite restricted, which may have precluded a stronger correlation between SM symptom severity and social anxiety.
Additional support for the link between SM and anxiety, and social anxiety in particular, comes from three descriptive studies that assessed anxiety disorder diagnoses in children with this condition (Black and Uhde 1995; Dummit et al. 1997; Oerbeck et al. 2014). These studies used instruments such as the Diagnostic Interview Schedule for Children (National Institute of Mental Health 1991) and the Schedule for Affective Disorders and Schizophrenia for school-age children (Kaufman et al. 1997) for this purpose and found that almost all children with SM (97 and 100 %, respectively) met DSM-III-R criteria (APA 1987) of social phobia/avoidant disorder. The study by Dummitt et al. (1997) also revealed that nearly half (48 %) of the children with SM had one or more anxiety disorders, notably specific phobias, separation anxiety disorder, and overanxious disorder. Additional research by Edison et al. (2011) and Nowakowski et al. (2011) indicated that 33–50 % of children with SM had at least one comorbid anxiety disorder, although the rate of social phobia was—for some unknown reason—surprisingly low (0–14 %). Nevertheless, on the basis of most descriptive studies, it can be concluded that there is a fairly strong relation between SM and social phobia (see also Andersson and Thomsen 1998; Bergman et al. 2013) and a less strong link between SM and other anxiety disorders.
This conclusion has been further substantiated by the findings of comparative studies in which children with SM are contrasted with non-clinical or clinical control groups (Table 1). The results of this research have shown that children with SM generally display higher levels of anxiety symptoms than non-clinical control children (Bergman et al. 2002; Chavira et al. 2007; Cunningham et al. 2006; Cunningham et al. 2004; Elizur and Perednik 2003; Kristensen 2000) and exhibit comparable levels of anxiety symptoms as children with social phobia or other anxiety disorders (Carbone et al. 2010; Levin-Decanini et al. 2013; Manassis et al. 2003, 2007; McInnes et al. 2004; Vecchio and Kearney 2005), with some studies even indicating that children with SM show more severe social anxiety symptomatology than children with social phobia without SM (Yageneh et al. 2006, 2003; Young et al. 2012). In addition, it should be noted that a number of the comparative or treatment outcome studies also included a diagnostic interview (such as the Anxiety Disorders Interview Schedule for Children; Silverman and Albano 1996) to establish rates of anxiety disorder diagnoses in children with SM between 50 and 100 %, with again social phobia being the most prevalent (Kristensen 2000; Levin-Decanini et al. 2013; Manassis et al. 2003, 2007; Vecchio and Kearney 2005).
Altogether, on the basis of the extant literature, it is evident that anxiety—and social anxiety in particular—is a prominent feature of children with SM. This is in line with the conclusions drawn by Sharp et al. (2007) who noted that SM “tends to co-occur at a high frequency with a number of anxiety-related conditions” (p.576) and “shares many overlapping characteristics with social phobia, including an intense fear associated with social and performance situations in which embarrassment may occur, and the avoidance of these situations” (p.574). These conclusions may help explain why authors like Anstendig (1999)—over 15 years ago—argued for a classification of SM among the anxiety disorders, a plea that has been met in the current edition of the DSM (APA 2013).
The Etiology of SM
The current notion is that SM originates from a variety of genetic, temperamental, environmental, and neurodevelopmental factors (Cohan et al. 2006; Viana et al. 2009). In this section, we will summarize the evidence for each of these etiological pathways and try to integrate them into a comprehensive model. We will also make a comparison with the childhood anxiety disorders literature in order to search for commonalities (as well as differences) in etiological pathways of SM and this type of internalizing psychopathology.
Familial Resemblance and Genetics
Research has documented that SM and associated symptoms occur at a disproportionally high rate within families of children with this condition. For example, in their sample of 45 children with SM, Remschmidt et al. (2001) found that 9 % of the fathers, 18 % of the mothers, and 18 % of the siblings also had a history of SM and that 51 % of the fathers and 44 % of the mothers showed signs of extreme reticence, respectively. Two case–control studies of Kristensen and Torgersen (2001, 2002) investigated personality characteristics and symptomatology in the parents of children with SM and non-clinical control children. Findings consistently indicated that fathers and mothers of SM children displayed higher levels of shyness and social anxiety and also had a stronger preference for solitary activities as compared to the parents of control children. Another relevant investigation was carried out by Chavira et al. (2007) who compared the history of lifetime psychiatric disorders in the parents of 70 children with SM and 62 control children. It was found that generalized social phobia and avoidant personality disorder were more frequently present in the parents of children with SM than in the parents of control children (percentages being 37 vs. 14 %, and 18 vs. 5 %, respectively). All of these results are suggestive of a genetic contribution to the etiology of SM, but of course behavioral genetic and DNA studies are needed to establish the role of heritability more directly (Rice 2008).
Unfortunately, such research is extremely sparse. There are a few case studies of monozygotic twins reporting that both children had the diagnosis of SM (e.g., Segal 2003), but a systematic study comparing the concordance of this condition between monozygotic and dizygotic twins is currently lacking in the literature. However, there is one study that has examined genetic material in relation to SM. Stein et al. (2011) analyzed the DNA of 99 nuclear families that included at least one child with this disorder. Special attention was paid to the contactin-associated protein-like 2-gene (CNTNAP2), which had previously been associated with social problems (including those of children with autism spectrum disorders). The results showed that one of the polymorphisms in CNTNAP2 (rs2710102) was significantly associated with SM. To further explore this finding, a second sample of 1028 young adults was also subjected to a DNA analysis. In addition, these participants completed standardized questionnaires for measuring social anxiety symptoms and socially anxious traits. Again it was found that the polymorphism rs2710102 was related to social anxiety: The presence of the rs2710102 allele was associated with increased odds ratios of 1.33 and 1.40, respectively, for having heightened scores on the measures of social anxiety symptoms and socially anxious traits. Altogether, the results of this study showed that a genetic variation of the CNTNAP2-gene seems to be involved in SM, social anxiety, and socially anxious traits. Interestingly, this also suggests that the overlap between SM and social phobia is also present at the genetic level, which further underscores the link between SM and this anxiety disorder.
Temperament
SM also shares features with the temperament construct of behavioral inhibition, which has been defined as the habitual tendency to show persistent fearfulness and avoidance during confrontations with novel and unfamiliar people, situations, and objects (Kagan 1994). Behavioral inhibition appears to manifest itself in different ways during various stages of children’s development, and interestingly, it has been found that in the preschool years, reticence in the presence of unfamiliar adults and lack of spontaneous speech with unknown persons are among the best indicators of this temperamental construct (Garcia-Coll et al. 1984). Note that these early characteristics of behavioral inhibition closely match the key symptoms of SM and also developmentally correspond with the age-of-onset of the disorder. Further, it is important to note that evidence has accumulated showing that behavioral inhibition in early childhood is associated with higher risk for developing anxiety disorders in later childhood (e.g., Hirshfeld-Becker et al. 2008) and social phobia in particular (Clauss and Blackford 2012; Ollendick and Benoit 2012), which of course points at a common etiological pathway between SM and (social) anxiety.
Although the link between behavioral inhibition and SM seems self-evident, there is actually no direct empirical support for this relationship. However, a number of cross-sectional studies have shown that children with SM display characteristics that seem to be indicative of an inhibited temperament. For example, descriptive research has reported that shyness—which can be viewed as the social variant of behavioral inhibition—is commonly observed in children with SM, with percentages ranging between 68 % (Kumpulainen et al. 1998) and 85 % (Steinhausen and Juzi 1996). This result has been confirmed in the case–control study of Kristensen and Torgersen (2002) who administered the emotionality-activity-sociability (EAS) temperament survey (Buss and Plomin 1984) to the parents of children with SM (with/without a comorbid communication disorder) and the parents of non-referred control children. It was found that both the fathers and the mothers consistently rated children with SM as higher on shyness and lower on sociability than control children. In a similar vein, Ford et al. (1998) noted that children with SM scored high on withdrawal and low on adaptability, indicating that these children do “not respond well to new or novel stimuli” and do “not handle transition and change well” (p. 210). All these findings provide limited but circumstantial evidence for the notion that behavioral inhibition is implicated in SM. However, it is also clear that future studies need to employ prospective designs so that it can be established whether behavioral inhibition serves as a vulnerability factor for the development of SM, just as has been shown for childhood anxiety disorders.
Another aspect of childhood temperament that has also received little research attention is oppositionality. Some children are more difficult to handle not because they are more shy and inhibited but because they do not wish to comply with the rules and conditions set by caregivers (Thomas and Chess 1977). Ford et al.’s (1998) phenomenological investigation indeed revealed that children with SM not only displayed anxiety symptoms but also showed signs of oppositional behavior. That is, these researchers noted that a significant proportion of parents endorsed CBCL items such as “Stubborn, sullen, or irritable” (72 %), “Argues a lot” (58 %), “Disobedient at school” (48 %), “Whining” (46 %), and “Temper tantrums or hot temper” (44 %). A handful of studies have further explored this association by systematically assessing externalizing symptoms in children with SM. The results have been quite mixed. One investigation showed that a small percentage of the children with SM (10 %) met the full criteria for oppositional defiant disorder (Black and Uhde 1995). Other studies have documented heightened externalizing problem scores for children with SM, although average symptom levels remained well within the non-clinical range (Kristensen and Torgersen 2001; Yageneh et al. 2003, 2006). However, there is also research reporting equal or even lower levels of such problems in comparison with clinical and non-clinical control children (Cunningham et al. 2006; Vecchio and Kearney 2005). Therefore, based on the available evidence, it is not likely that oppositionality defines an important etiological pathway to SM, but at the same time, it is clear that some children with this condition will present with (mild) behavior problems (Cohan et al. 2008). It remains to be seen whether these truly reflect comorbidity or merely should be seen as symptomatology occurring in children who are exposed to fearful situations, which are similar explanations that have been put forward for the co-occurrence of anxiety and externalizing disorders (Bubier and Drabick 2009; Drabick et al. 2010; Russo and Beidel 1994).
Environmental Influences
Early theories on the etiology of SM primarily come from a psychodynamic background and either assume that this condition “helps to keep the neurotic family in balance” or “has its origin in childhood trauma” (Hesselman 1983; p. 297). Nowadays, these conceptualizations are less accepted, although a number of early studies have explored their validity. For example, Hayden (1980) examined the link between SM and problematic family functioning and documented considerable pathology in the families of 68 clinically referred children with SM. That is, almost all children (97 %) came from divorced families; moreover, physical as well as sexual abuse (77 and 30 %) was highly prevalent. However, such high rates of family problems have not been reported in other studies (e.g., Black and Uhde 1995; Kumpulainen et al. 1998; Steinhausen and Juzi 1996), and overall findings do not seem to justify the conclusion that the families of children with SM have primarily negative characteristics (Ford et al. 1998). In addition to family-related incidents such as abuse and divorce, other “traumatic” or major life events have been investigated, including hospitalization, moving, and death of a family member (e.g., Black and Uhde 1995; Kopp and Gillberg 1997; Kumpulainen et al. 1998), but convincing evidence of a temporal relationship between these types of psychological trauma and the onset of SM is lacking.
Comparative studies have revealed that apart from SM-like or associated symptoms (e.g., shyness, social anxiety, taciturnity), parents of children with SM and parents of control children do not differ greatly in terms of psychopathology (e.g., Chavira et al. 2007). Furthermore, a recent investigation by Alyanak et al. (2013) demonstrated that the general parental rearing styles in families of children with SM are not different from those observed in families of non-clinical control children (see also Cunningham et al. 2004). At a more behavioral level, however, an observational study by Edison et al. (2011) showed that the parents of children with SM appear to be significantly more controlling and overprotective. More precisely, during a free-play situation and a preparation of a birthday speech, parents of children with SM were rated as granting less autonomy and making more power remarks than parents of clinical and non-clinical control children. Interestingly, additional analyses indicated that child and parent anxiety predicted these parental control attempts, with increased anxiety being associated with higher levels of control. Note that these findings are well in line with what has been found in the childhood anxiety literature (for a review, see McLeod et al. 2007).
Many children with SM do not speak at school (e.g., Bergman et al. 2002; Kumpulainen et al. 1998), which suggests that the condition might be partly due to specific problems occurring within that setting. A first type of problem that is inherently related to school has to do with academic performance. Many educational activities are verbal in nature, and it may well be that children with lower intelligence or learning problems perceive the school program as more difficult and thus are less likely to engage in speech. Support for this notion has been obtained by Kolvin and Fundudis (1981) who found that–although the majority of their sample of children with SM fell within the normal range of intelligence—the average IQ was only 85. In a similar vein, Ford et al. (1998) noted that a substantial proportion of their sample (45.1 %) had been referred to a special education program, mainly for reasons of difficulties with speech and language. This is consistent with findings of other studies indicating that communication disorders (Steinhausen and Juzi 1996 38 %; Kristensen 2000 50 %) and delay in language development (Manassis et al.2007 18–43 %) are common among children with SM. A second type of problem that may occur in school is concerned with poor peer relations. Research has consistently shown that children with SM are considered less socially competent than non-clinical control children. That is, parents and teachers rate these children as less confident during interactions with peers and as having more difficulties with joining the group and establishing friendships (Cunningham et al. 2004, 2006; Levin-Decanini et al. 2013). One study even demonstrated that children with SM strongly resembled children with social phobia in this regard (Carbone et al. 2010). The teachers in the study by Kumpulainen et al. (1998) observed that about 40 % of the children with SM did not actively participate in group activities in class and during the breaks, and a number of these children were rejected by their peers (15 %) or bullied by them (5 %). It is important to keep in mind that the relation between school-related problems and SM is likely to be bidirectional. That is, as argued above, it may well be that children do not speak because of academic and peer problems, but it is equally plausible that such problems arise as a consequence of not speaking at school. Of course, longitudinal studies would be particularly welcome to unravel this cause–effect issue.
Based on a literature review of cases of children with SM, Bradley and Sloman (1975) were the first to note that the incidence of SM seems to be quite high among children of immigrant families. The fairly high occurrence of SM in immigrant families has been confirmed in a number of descriptive studies. For example, in clinically referred samples, Steinhausen and Juzi (1996) found rates of 39 % in Switzerland and 23 % in Germany, while Dummit et al. (1997) and Manassis et al. (2007) documented 22 and 21 % with an immigrant background in the USA and Canada, respectively. In contrast, other studies have obtained considerably lower rates, reporting percentages of no more than 10 % (Black and Uhde 1995; Chavira et al. 2007; Ford et al. 1998). However, prevalence rates in clinical samples may be biased in various ways, and a population-based approach seems preferable to establish whether the incidence of SM is indeed higher among children from immigrant families than among children with an indigenous background. So far, the only study that employed this method was conducted by Elizur and Perednik (2003) who conducted telephone interviews with all preschool teachers of West Jerusalem, Israel, in order to identify children with SM. The results showed that the prevalence of SM among immigrant children was 2.2 %, which was more than four times the rate for native families (0.5 %). Given this evidence, one is inclined to conclude that immigrant children are indeed more prone to develop SM. It remains unclear, however, as to why this would be the case. Nonetheless, several explanations have been put forward, including processes of acculturation, second language acquisition, discrimination, and peer rejection, all of which are often closely tied to immigrant status (Viana et al. 2009). This finding reflects another parallel with the childhood anxiety literature, where similar processes have been put forward to account for the elevated fear and anxiety levels of children in ethnic minority groups (e.g., Beidas et al. 2012).
To summarize, various environmental influences (family dysfunction, traumatic or stressful life events, parental control, negative experiences at school, and immigrant status) seem to be involved in the origins of SM, although it should be evident that research is sparse and the evidence for the contribution of these factors is meager. Nevertheless, it can be noted that similar environmental factors also feature in the literature on the etiology of anxiety disorders more broadly (Muris 2007), again strengthening the idea that there may be a connection between SM and this type of psychopathology.
Neurodevelopmental Factors
With the classification of SM as an anxiety disorder in DSM-5 (APA 2013), it is probable that the marked selectivity of speaking is primarily emotionally determined. However, research has also made it clear that neurodevelopmental factors are involved in a significant proportion of the children with this condition. For example, a heightened prevalence of speech and language problems in children with SM is noted. For example, Kolvin and Fundudis (1981) noted that their sample of 24 selectively mute children on average spoke significantly (i.e., more than 5 months) later than children in the non-clinical control group. Moreover, it was found that 50 % of the children with SM had “immaturity of speech” and/or other speech difficulties. Other researchers have documented that between 11 and 50 % (Ford et al. 1998; Kristensen 2000; Steinhausen and Juzi 1996) of children with SM also fulfill criteria for a communication disorder. For instance, in the investigation of Kristensen (2000), who examined comorbid disorders of SM, it was found that half of the children with this condition were diagnosed with mixed receptive–expressive language disorder (17 %), expressive language disorder (12 %), and/or phonological disorder (43 %). Attempts have also been made to quantify the language skills of children with SM, and this research has generally confirmed the idea that the condition is associated with language deficits (Manassis et al. 2007; Nowakowski et al. 2009; McInnes et al. 2004). An exemplary study was conducted by Manassis et al. (2007) who administered a battery of standardized, nonverbal language tests (e.g., the Peabody Picture Vocabulary Test; Dunn and Dunn 1997) to 6- to 10-year-old children with SM (n = 44) and children with anxiety disorders (n = 28), and non-clinical control children (n = 19) of similar age and intellectual capacity. Results showed that children with SM scored significantly lower on tests of receptive vocabulary skills, phonemic awareness abilities, and grammar as compared to children with anxiety disorder and control children, who displayed comparable scores on the language tests in this study.
Apart from speech/language problems, it has been postulated that children with SM may display deficits in social skills. For example, Carbone et al. (2010) obtained parent- and teacher-reports of social competence and social skills in 44 children with SM, 65 children with mixed anxiety problems, and 49 non-clinical control children. It was found that, according to both parents and teachers, children with SM displayed significantly lower levels of social assertion (e.g., inviting others over or starting conversations) and verbal social skills as compared to mixed anxiety and non-clinical control children. Of course, it is possible that this result merely reflects the nature of SM (i.e., selective use of language), but it could also be the case that these children—because they have deficits in social skills—easily experience anxiety and embarrassment, eventually prompting them to avoid speech.
Several authors have argued that children with SM do not only have speech/language and social skills problems, but also show clear signs of a more general delay in their development (Kolvin and Fundudis 1981; Kristensen 2000, 2002; Steinhausen and Juzi 1996). The work by Kristensen (2000) is noteworthy in this regard. This study showed that children with SM more often displayed pre- and perinatal problems and delays in fine as well as gross motor function as compared to non-clinical control children. Further, when looking at DSM-IV diagnoses, 17 % of these children had developmental coordination disorder, 32 % elimination disorder (i.e., enuresis and/or encopresis), 8 % mild mental retardation, and 7 % autism spectrum disorder (i.e., Asperger disorder), and these prevalence rates were significantly higher than those in the control group. Thus, although less well investigated than language and speech problems, there is evidence that SM is associated with neurodevelopmental immaturity.
At a neurological level, aberrations have been found in some children with SM that may partly explain the selective absence of their speech. During verbal communication, there is a continuous interaction between speech and hearing mechanisms, and various mechanisms are operative to deal with incoming auditory information and to maintain production accuracy. Among these are auditory efferent feedback pathways that play a role during the monitoring and regulation of self-vocalization. One such feedback pathway involves the middle-ear acoustic reflex (MEAR), which refers to the contraction of the middle-ear muscles and serves the masking of one’s own voice during speech. There is clear evidence that the MEAR (and other auditory reflexes) in some children with SM functions less well (Arie et al. 2007; Bar-Haim et al. 2004; Muchnik et al. 2013) and that this results in an abnormal subjective experience of their own voice. Indeed, there have been reports in the literature of children with SM who reported that their “voice sounds funny” (Black and Uhde 1992; Boon 1994). It is unlikely that reduced auditory efferent activities represent a single causal mechanism in SM, but it is conceivable that in combination with (social) anxiety, shyness, and behavioral inhibition, these neurological anomalies may make a contribution to the etiology of this condition. Clearly, this idea requires further scientific evaluation.
Altogether, there seems to be sufficient support for the notion that neurodevelopmental factors such as language and speech problems, a general developmental delay, and neurological anomalies are implicated in the origins of SM. Avoidance of difficulties experienced as a consequence of the neurodevelopmental problems, and avoidance of the associated negative emotions (in particular anxiety) seems to be the most plausible working mechanisms behind this pathway. On first sight, this seems unique for SM and less relevant for other anxiety disorders. Meanwhile, research has indicated that anxiety problems are highly prevalent in children with autism spectrum disorders and/or mental retardation (e.g., Dekker and Koot 2003; Muris et al. 1998; White et al. 2009), which suggests that developmental difficulties are at least to some extent involved in childhood anxiety disorders.
Avoidance as a Maintaining Factor
It has been argued that the “non-speaking behavior” of children with SM essentially should be seen as an emotion regulation strategy (Scott and Beidel 2011). That is, by remaining silent, these children reduce anxiety or other negative emotions in stressful or otherwise challenging situations (e.g., school). An intriguing study conducted by Young et al. (2012) has indeed provided tentative support for such a scenario. Thirty-five children aged between 5 and 12 years with either SM (n = 10), social phobia (n = 11), or no diagnosis (n = 14) participated in two social interaction tasks: (1) a role-play during which the child had to respond to statements and questions posed by a same-aged peer and (2) reading aloud in front of a small audience consisting of an adult and a same-aged peer. Measurements included child and observer ratings of anxiety as well as psychophysiological measures (e.g., electrodermal activity, heart rate). The child self-report ratings did not reveal significant differences in anxiety across the three groups. However, according to behavioral observations, the SM group displayed the highest anxiety levels during the interaction tasks, and these were even significantly higher than those for the social phobia group. Unexpectedly, psychophysiological measures indicated that children in the SM group experienced less arousal than the other children while conducting the social interaction tasks. On the basis of these findings, Young et al. (2012) postulated that the lack of speech in children with SM may reflect “an effective avoidance strategy by which to decrease emotional and physiological distress” (p. 540). Note that a similar mechanism is thought to play a role in the maintenance of anxiety disorders more broadly, where avoidance results in the removal of the unpleasant anxiety symptoms, which in turn further reinforces avoidance behavior (Mowrer 1960).
Overview: Etiology of SM
Altogether, the available evidence indicates that various factors are involved in the etiology of SM, including genetics, temperament, environmental influences, neurodevelopmental variables, and avoidance, although it should be reiterated that the support for some of these etiological factors mainly comes from cross-sectional studies and thus require further prospective exploration. Many of these factors have also been implicated in the origins of anxiety pathology (e.g., Muris 2007), which of course strengthens the conceptualization of SM as an anxiety disorder. Several authors (Cohan et al. 2006; Viana et al. 2009) have proposed that the etiology of SM can be explained within a developmental psychopathology framework (Cicchetti and Cohen 1995; Whiteside and Ollendick 2009). That is, SM does not develop as the result of one deterministic variable, but rather is due to complex interactions among various vulnerability factors, which heighten the probability (risk) that this psychiatric condition will occur (see Fig. 1). In keeping with the principle of equifinality, the constellation of vulnerability factors is different for each individual child with SM. Of course this may also have repercussions for the treatment of this condition, which will be the topic of the next section of this paper.
Treatment of SM
SM is a disabling psychiatric condition, seriously hindering the child in his/her academic and social functioning. Although the key symptom “absence of speech” tends to dissipate over time, it also clear that SM has detrimental consequences for children in later life (Remschmidt et al. 2001; Steinhausen et al. 2006). Therefore, it is very important that effective interventions are available for treating children with SM. The main goal in the treatment of SM is to help children speak in situations where they previously did not speak (Pionek Stone et al. 2002). In general, this can be achieved in two ways: via psychosocial interventions or by means of pharmacotherapy.
Psychosocial Interventions
In their comprehensive review on psychosocial interventions for children with SM, Cohan et al. (2006) documented 23 relevant studies that had been published in scientific journals between 1990 and 2005. They noted that at that time, the most popular intervention was behavioral/cognitive-behavioral in nature. That is, 10 studies evaluated the effects of interventions relying on techniques such as contingency management (i.e., systematic reinforcement of speech behavior), shaping (i.e., training the child to gradually increase the use of speech in specific situations), prompting and fading (i.e., helping the child to speak and slowly removing these prompts so that he/she speaks on his/her own), systematic desensitization (i.e., exposure to increasingly difficult situation while the child is learning to use relaxation to deal with negative emotions), social skills training (i.e., enhancing the social competence of the child by improving verbal and nonverbal skills), and modeling (i.e., the child mimics the effective speech behavior of a model). Other investigations focused on language training (n = 1), family therapy (n = 1), psychodynamic treatment (n = 5), or interventions adopting a multimodal approach (which combines methods from the other approaches; n = 6). The fact that SM is a relatively rare disorder has had a negative impact on the quality of the research. That is, most investigations (n = 17) were case studies or employed a single-case design, and in total only 72 children with SM (aged between 3 and 13 years) were included in these 23 studies. Nevertheless, Cohan et al. concluded that “Although much of this literature is limited by methodological weaknesses, the existing research provides support for the use of behavioral and cognitive-behavioral interventions” (p. 1085; see also Keeton and Crosby Budinger 2012).
Now almost 10 years later, a new literature search in Web of Science using (elective/selective mutism in title) AND (treat* or intervention in topic) as keywords yielded 14 new publications on psychosocial interventions for children with SM. Without exception, all studies focused on the behavioral/cognitive-behavioral approach. Apart from a number of traditional case studies, more controlled research was conducted by Vecchio and Kearney (2009) who employed an alternating treatment design to compare the effects of child-focused exposure-based practice and parent-focused contingency management in nine children with SM. The data showed that treatment resulted in positive end-state functioning (i.e., improvement of speech in public situations) for eight out of nine participants and that effects were better for child-focused exposure-based practice than for parent-focused contingency management.
Another compelling study was carried out by Oerbeck et al. (2014) who randomized 24 children aged 3–9 years either to an intervention consisting of defocused communication (i.e., communicating with the child by creating joint attention using a pleasurable activity rather than focusing on the child) and behavioral techniques (i.e., exposure and stimulus fading) or a waitlist control condition. The main outcome measure was the School Speech Questionnaire (Bergman et al. 2002), which was administered before and after the 3-month intervention/waiting period. Results indicated that speech at school significantly increased in the intervention group, while no change was documented in the waitlist control condition. Interestingly, attempts have been made to develop Web-based and group format versions of cognitive-behavioral treatment for children with SM (Ooi et al. 2012; Sharkey et al. 2008), which certainly deserve further scientific evaluation.
Particularly noteworthy in recent years is the randomized controlled trial conducted by Bergman et al. (2013) evaluating the effects of integrated behavioral therapy (IBT) for SM. The intervention consists of 20 sessions not only involving the child but also the parents and the teacher. Early in treatment, a graded hierarchy of speaking-related situations is created that guides the exposure exercises that the child has to carry out in the clinic, school, and home environment, which is supported by a variety of behavioral techniques (e.g., reinforcement, shaping, modeling). Dependent on the developmental level of the child, cognitive restructuring techniques can be added (e.g., replacing anxious thoughts with coping self-statements; see Table 2 for a more detailed overview of the intervention). Bergman et al. (2013) assigned 21 children aged 4–8 years with SM to either the above-described 20-session IBT program—which was provided during a period of 24 weeks—or a 12-week waitlist control condition. Treatment outcome was evaluated extensively using diagnostic status, a rating of treatment response, parent- and teacher-report of SM symptoms and social anxiety, and a behavioral speech task, with most measures also being administered at a 3-month follow-up to examine the durability of the treatment effects. The results first of all showed that 67 % of the children no longer met the diagnostic criteria of SM after the IBT intervention, while all children in the waitlist condition still fulfilled the criteria at week 12. This finding was confirmed by blind-independent ratings of clinical improvement which indicated that 75 % of children in the IBT condition could be considered as treatment responders compared to 0 % of those who were assigned to the waitlist. Second, on standardized rating scales completed by parents and teachers, it was found that IBT resulted in increased functional speaking, whereas no such improvement in speaking behavior was observed for children in the waitlist condition. On an objective, behavioral index of speech production, children in the IBT condition also outperformed children in the waitlist condition. More precisely, at the end of treatment, these children used more than 3 times the words they initially employed to retell a story that had been presented to them on audiotape, while in the waitlist condition no significant change in the number of words used to tell the story was observed. Third, the 3-month follow-up assessment revealed that these positive changes in children’s speech behavior were maintained. Finally, based on the notion that there is a strong link between SM and social phobia, Bergman et al. (2013) assessed these anxiety symptoms as a secondary outcome measure. It was found that parents, but not teachers, reported significant reductions in social phobia symptomatology following IBT, which were not present in the waitlist control group. Although the design of this study can be criticized because the intervention and waitlist conditions differed in length (24 versus 12 weeks, respectively), the mid-treatment assessments conducted in the intervention condition demonstrated that the superiority of IBT was already clearly present halfway into the treatment. Taken together, these findings provide support for the efficacy of IBT in children with SM.
Pharmacotherapy
Pharmacotherapy has also been proposed as a treatment option for children with SM. Based on the idea that anxiety is a prominent feature of SM, clinicians have predominantly tried to treat the condition with selective serotonin reuptake inhibitors (SSRIs; Kaakeh and Stumpf 2008), which have also proven to be successful in the treatment of children with anxiety disorders (Muris 2012). Fluoxetine has been the most frequently used SSRI for treating children with SM (see Carlson et al. 2008). Its effects have been mainly documented in case reports, but there are two studies that are exceptions to this rule. The first is a small-scale, placebo-controlled, double-blind trial conducted by Black and Uhde (1994) in which 16 young patients with SM aged between 5 and 16 years were treated with placebo medication for 2 weeks. The 15 placebo non-responders were then randomly assigned to a double-blind treatment with fluoxetine or continued placebo for an additional 12 weeks. Significant improvements in clinician, parent, and teacher ratings of SM, anxiety symptoms, and global change were observed in both fluoxetine- and placebo-treated children. However, the parental measures indicated that children treated with fluoxetine were significantly more improved than the placebo-treated controls.
The second investigation on the efficacy of fluoxetine in children with SM is the open trial carried out by Dummit et al. (1996). Twenty-one children aged between 5 and 14 years received a 9-week treatment during which the dose of the drug was gradually increased. Outcome was evaluated by means of clinician ratings of global improvement and social anxiety, and parent- and self-report scales of social problems. It was found that the fluoxetine treatment produced positive effects (as measured by improvement on the Clinical Global Improvement scale) in 76 % of the children, which was also substantiated by consistent reductions of symptoms on various scales.
Although it should be acknowledged that the empirical support is meager, available data suggest that SSRIs (especially fluoxetine) may be a viable treatment option for children with SM, in particular for those who do not respond adequately to psychosocial interventions. These drugs are well tolerated by children, who generally report only a minimal number of mild side effects (e.g., Black and Uhde 1994; Dummit et al. 1996).
Apart from SSRIs, monoamine oxidase (MAO) inhibitors have been occasionally employed to treat children with SM. For example, Golwyn and Sevlie (1999) described the treatment of four children with SM aged 5–7 years who had not recovered after psychosocial treatment or pharmacotherapy with fluoxetine and were then given gradually increasing dosages of phenelzine. All children responded positively to this drug: They started to display spontaneous speech in multiple settings and showed significant reductions in anxiety. SM remained in remission following the termination of the medication treatment, but two of the children needed subsequent treatment with a SSRI because of re-occurring emotional problems. Moreover, moderate side effects (weight gain, low blood pressure, and constipation) were observed in all children, leading the authors to conclude that this medication “should be reserved for cases that do not respond to behavior therapy and fluoxetine or other specific serotonin reuptake inhibitors” (p. 109).
Overview: Treatment of SM
Several conclusions can be drawn from the literature on the treatment of SM. To begin with, it is clear that the research conducted so far is limited in terms of both quantity and quality. Given the rarity of this psychiatric condition, a multicenter approach may be necessary to set up more large-scale treatment outcome studies. Otherwise, a series of cases could be studied within a multiple-baseline design, which can be a particularly powerful method for documenting treatment effects (Kazdin 1982). The available evidence suggests that behavioral/cognitive-behavioral interventions and pharmacotherapy with SSRIs are most effective for treating SM. Note that these treatment approaches are also considered as the treatments-of-choice for children with anxiety disorders (Rapee et al. 2009; Ollendick and King 2012), which of course further strengthen the notion that there is an intimate relationship between SM and anxiety.
However, at least one critical point can be made in this regard. That is, the fact that effective interventions for children with SM mimic those for children with anxiety disorders should not automatically imply that anxiety is the sole target of treatment. As we have noted, other mechanisms are also involved in the development of SM and often require clinical attention (Anstedig 1998). For example, a child with SM who has comorbid communication problems may also need remedial services (logopaedics) to improve speech and language function. Alternatively, a child whose SM is also related to oppositional problems may require a treatment package that includes a parent-management component. This calls for a careful diagnostic evaluation and, if necessary, multimodal treatment of these children in clinical practice.
Discussion: Critical Points Regarding the Current DSM-5 Classification of SM
The current edition of the DSM (i.e., DSM-5) considers SM as an anxiety disorder (APA 2013). As has become clear from this review, there are various reasons to justify this point-of-view. First of all, research shows that anxiety is a prominent feature of SM: Children with this psychiatric condition typically display anxiety-related symptoms and behaviors and often fulfill the diagnostic criteria of a comorbid anxiety disorder. Second, when looking at the etiology of SM, many factors are involved that also play a role in the origins of other childhood anxiety disorders (e.g., behavioral inhibition, parental control, stressful experiences). Third, behavioral and cognitive-behavioral therapies and pharmacotherapy with SSRIs have been found to be most effective for treating children with SM, and precisely, these treatment approaches are also viewed as the most optimal interventions for children with anxiety disorders.
The literature has yielded clear support for a link between SM and anxiety, but there is still debate on the precise nature of this relationship. There is a strong tendency in the literature to consider SM as a special form of social phobia (Bögels et al. 2010), with some authors arguing that the condition should be seen as an extreme symptom of this anxiety disorder (e.g., Black and Uhde 1995) and others proposing that SM is an early childhood variant of social phobia (Bergman et al. 2002). Good arguments can be advanced for both positions. For instance, studies showing that children with SM exhibit even higher levels of social anxiety symptoms than children with social phobia (Yageneh et al. 2003, 2006; Young et al. 2012) of course support the extreme symptom hypothesis, whereas the early age-of-onset of SM in combination with the fact that complete muteness normally tends to disappear with increasing age (Remschmidt et al. 2001) is in favor of the young child variant hypothesis.
By definition, the core problem (absence of speech) of SM occurs in social situations and as such it is not surprising that this condition is closely associated with social phobia. However, it also needs to be emphasized that the overlap between SM and social phobia is not evident in all cases. Various studies indicate that SM is also associated with other anxiety disorders, in particular specific phobias, separation anxiety disorder, and overanxious or generalized anxiety disorder (Black and Uhde 1995; Dummit et al. 1997; Edison et al. 2011), and so it is possible that some children with this condition have a non-socially anxious motive for their lack of speech. For instance, on the basis of observations of interactions in the natural contexts of home and school, Omdal and Galloway (2008) noted that some of these children fully engaged in social interactions by extensively using compensatory body language and gestures, which is of course difficult to reconcile with the traditional clinical picture of an individual with social phobia who fears negative evaluation by others in social situations even when no speaking is required (see also First 2014). Therefore, these authors propose to re-conceptualize SM as a specific phobia of expressive speech. Otherwise, there is evidence indicating that verbal productivity is negatively associated with situational anxiety (e.g., Murray 1971), and so it is conceivable that the silence of children with SM mainly is the result of anxiety elicited by the separation from the parents or by worrisome thoughts triggered by certain aspects of social situations (e.g., school).
DSM-5 eventually adopted the notion that SM is not equivalent to social phobia and classifies the condition as a separate anxiety disorder (APA 2013). Although this certainly is in line with the fact that SM is linked to a broad range of anxiety symptoms, critique can be raised regarding the classification of SM as a distinct anxiety problem. As noted, several authors have pointed out that it may be preferable to regard SM as a specific type of avoidance behavior that can emerge from a variety of reasons (Bögels et al. 2010; Young et al. 2012). A parallel can be drawn with school refusal, which often occurs as a consequence of (social, separation, test) anxiety, but may also have other origins (e.g., learning difficulties, behavioral problems, peer victimization; Kearney 2008). Thus, according to this view (see Scott and Beidel 2011), SM can better be considered as a functional strategy to regulate negative emotions (predominantly anxiety, but also anger, sadness, and shame; e.g., Moldan 2005) and/or a coping mechanism to deal with other difficulties. Full acception of this idea would imply the elimination of SM from diagnostic classification systems such as the DSM, which might have the negative consequence that children suffering from this condition no longer receive the required, specialized clinical attention.
It is also remarkable that SM is the only anxiety disorder listed in DSM-5 that makes no explicit reference to fear or anxiety in its diagnostic criteria (APA 2013). “Fear or anxiety of speaking in specific situations” could have been an appropriate formulation for the key criterion of this condition, but at the same time, this would have increased the urge for adding SM as a specifier to social phobia. By maintaining the more liberal “failure to speak” criterion, it is still possible to assign the diagnosis to children in which (social) anxiety is less prominent. This aligns with the idea that SM is more than just an anxiety disorder, which is also nicely illustrated by a study of Cohan et al. (2008). These researchers performed a latent profile analysis on parent-report measures of social anxiety, behavior problems, and communication delays and identified the three groups of children with SM: exclusively anxious, combined anxious/mildly oppositional, and anxious/communication delayed. Surprisingly, it was found that the exclusively anxious children represented the smallest group (12 %) and that the majority of children were classified into the combined anxious/mildly oppositional and anxious/communication delayed groups (45 and 43 %, respectively). Thus, although anxiety appears to play a role in the majority of cases, other factors are also highly relevant for understanding children with SM (see also Mulligan 2012).
The addition of SM to the anxiety disorders as proposed in DSM-5 will ensure that clinicians are more focused on the anxiety that many of these children suffer from and perhaps will use efficacious interventions for treating this problem (cognitive-behavioral therapy and pharmacotherapy). The downside is, however, that the non-anxiety aspects of the disorder (e.g., oppositionality, language, and other developmental problems) may be neglected and receive less clinical attention. It is highly recommended that psychologists, psychiatrists, and other mental health professionals who face children with SM remain alert to the multifaceted nature of this disorder, and this should be translated into a comprehensive diagnostic assessment that focuses on anxiety and other psychological/psychiatric problems, audiological functioning, and cognitive and speech/language development (e.g., Dow et al. 1995). In line with this, for most children with SM, treatment should not only target the anxiety symptoms that frequently accompany the problem but also address the other difficulties that are also often present (see Dow et al. 1995; e.g., Powell and Dalley 1995; Wright et al. 1995).
We suggest several directions for future research. Now that SM is classified as an anxiety disorder, an instrument should be developed that actually addresses this important, emotional symptom of the disorder. The frequently employed Selective Mutism Questionnaire (Bergman et al. 2008; Letamendi et al. 2008) is not satisfactory in this regard and thus could be revised and then subjected to psychometric validation. Further, an instrument screening for the non-anxiety aspects of SM would also be particularly welcome as it would prime clinicians for the heterogeneous expression of the disorder (e.g., Cohan et al. 2008; Mulligan 2012) and guide them to use the proper assessment and treatment. With regard to the developmental psychopathology of SM, the current review makes it clear that a substantial part of the research on the etiology of SM has been cross-sectional in nature. Hence, the possibility cannot be ruled out that many of the factors that have been put forward and studied as etiological mechanisms are in fact consequences of the disorder. Obviously, the field would profit from research using prospective, longitudinal designs. A final venue for research should focus on the treatment of SM. Cognitive-behavioral therapy (e.g., IBT; Bergman et al. 2013) and SSRIs have proven to be successful in treating children with SM, probably because they are effective in reducing the anxiety associated with the disorder. Future studies need to pay more attention to children who do not respond to these interventions and evaluate treatments that combine cognitive-behavioral and pharmacotherapy or multimodal treatment packages that also address other possible difficulties of these children (e.g., parent-management training, speech therapy). Given the rarity of the disorder, it is advisable that research sites join forces, with the ultimate goal of gaining a better understanding of SM and improving our ability to help children who are suffering from this debilitating disorder.
References
Achenbach, T. M. (1991). Manual for the child behavior checklist/4-18 and 1991 profile. Burlington, VT: University of Vermont, Department of Psychiatry.
Alyanak, B., Kilinçaslan, A., Harmanci, H. S., Demirkaya, S. K., Yurtbay, T., & Vehid, H. E. (2013). Parental adjustment, parenting attitudes, and emotional and behavioral problems in children with selective mutism. Journal of Anxiety Disorders, 27, 9–15.
American Psychiatric Association. (1987). Diagnostic and statistical manual of mental disorders, third edition-revised. Arlington, VA: American Psychiatric Association.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: American Psychiatric Association.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Andersson, C. B., & Thomsen, P. H. (1998). Electively mute children: An analysis of 37 Danish cases. Nordic Journal of Psychiatry, 52, 231–238.
Anstedig, K. D. (1998). Selective mutism: A review of the treatment literature by modality from 1980-1996. Psychotherapy, 35, 381–391.
Anstedig, K. D. (1999). Is selective mutism an anxiety disorder? Rethinking its DSM-IV classification. Journal of Anxiety Disorders, 13, 417–434.
Arie, M., Henkin, Y., Lamy, D., Tetin-Schneider, S., Apter, A., Sadeh, A., & Bar-Haim, Y. (2007). Reduced auditory processing capacity during vocalization in children with selective mutism. Biological Psychiatry, 61, 419–421.
Bar-Yaim, Y., Henkin, Y., Ari-Even Roth, D., Tetin-Schneider, S., Hildesheimer, M., & Muchnik, C. (2004). Reduced auditory efferent activity in childhood selective mutism. Biological Psychiatry, 55, 1061–1068.
Beidas, R. S., Suarez, L., Simpson, D., Read, K., Wei, C., Conolly, S., & Kendall, P. C. (2012). Contextual factors and anxiety in minority and European American youth presenting for treatment across two urban university clinics. Journal of Anxiety Disorders, 26, 544–554.
Bergman, R. L. (2012). Treatment for children with selective mutism: An integrated approach. New York: Oxford University Press.
Bergman, R. L., Gonzalez, A., Piacentini, J., & Keller, M. L. (2013). Integrated behavior therapy for selective mutism: A randomized controlled pilot study. Behaviour Research and Therapy, 51, 680–689.
Bergman, R. L., Keller, M. L., Piacentini, J., & Bergman, A. J. (2008). The development and psychometric properties of the selective mutism questionnaire. Journal of Clinical Child and Adolescent Psychology, 37, 456–464.
Bergman, R. L., Piacentini, J., & McCracken, J. T. (2002). Prevalence and description of selective mutism in a school-based sample. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 938–946.
Black, B., & Uhde, T. W. (1992). Elective mutism as a variant of social phobia. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 1090–1094.
Black, B., & Uhde, T. W. (1994). Treatment of elective mutism with fluoxetine: A double-blind, placebo-controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 33, 1000–1006.
Black, B., & Uhde, T. W. (1995). Psychiatric characteristics of children with selective mutism: A pilot study. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 847–856.
Bögels, S. M., Alden, L., Beidel, D. C., Clark, L. A., Pine, D. S., Stein, M. B., & Voncken, M. (2010). Social anxiety disorder: Questions and answers for the DSM-V. Depression and Anxiety, 27, 168–189.
Boon, F. (1994). The selective mutism controversy (continued). Journal of the American Academy of Child and Adolescent Psychiatry, 33, 283.
Bubier, J. L., & Drabick, D. A. G. (2009). Co-occurring anxiety and disruptive behavior disorders: The roles of anxious symptoms, reactive aggression, and shared risk processes. Clinical Psychology Review, 29, 658–669.
Buss, A. H., & Plomin, R. (1984). Temperament: Early developing personality traits. Hillsdale, NJ: Lawrence Erlbaum.
Carbone, D., Schmidt, L. A., Cunningham, C. E., McHolm, A. E., Edison, S., Pierre, J. S., & Boyle, M. H. (2010). Behavioral and socio-emotional functioning in children with selective mutism: A comparison with anxious and typically developing children across multiple informants. Journal of Abnormal Child Psychology, 38, 1057–1067.
Carlson, J. S., Kratochwill, T. R., & Johnston, H. (1994). Prevalence and treatment of selective mutism in clinical practice: A survey of child and adolescent psychiatrists. Journal of Child and Adolescent Psychopharmacology, 4, 281–291.
Carlson, J. S., Mitchell, A. D., & Segool, N. (2008). The current state of empirical support for the pharmacological treatment of selective mutism. School Psychology Quarterly, 23, 354–372.
Chavira, D. A., Shipon-Blum, E., Hitchcock, C., Cohan, S., & Stein, M. B. (2007). Selective mutism and social anxiety disorder: All in the family? Journal of the American Academy of Child and Adolescent Psychiatry, 46, 1464–1472.
Cicchetti, D., & Cohen, D. J. (1995). Developmental psychopathology. New York: Wiley.
Clauss, J. A., & Blackford, J. U. (2012). Behavioral inhibition and risk for developing social anxiety disorder: A meta-analytic study. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 1066–1075.
Cohan, S. L., Chavira, D. A., Shipon-Blum, E., Hitchcock, C., Roesch, S. C., & Stein, M. B. (2008). Refining the classification of children with selective mutism: A latent profile analysis. Journal of Clinical Child and Adolescent Psychology, 37, 770–784.
Cohan, S. L., Chavira, D. A., & Stein, M. B. (2006a). Psychosocial interventions for children with selective mutism: A critical evaluation of the literature from 1990-2005. Journal of Child Psychology and Psychiatry, 47, 1085–1097.
Cohan, S. L., Price, J. M., & Stein, M. B. (2006b). Suffering in silence: Why a developmental psychopathology perspective on selective mutism is needed. Developmental and Behavioral Pediatrics, 27, 341–355.
Cunningham, C. E., McHolm, A. E., & Boyle, M. H. (2006). Social phobia, anxiety, oppositional behavior, social skills, and self-concept in children with specific selective mutism, generalized selective mutism, and community controls. European Child and Adolescent Psychiatry, 15, 245–255.
Cunningham, C. E., McHolm, A. E., Boyle, M. H., & Patel, S. (2004). Behavioral and emotional adjustment, family functioning, academic performance, and social relationships in children with selective mutism. Journal of Child Psychology and Psychiatry, 45, 1363–1372.
Dekker, M. C., & Koot, H. M. (2003). DSM-IV disorders in children with borderline to moderate intellectual disability. I: Prevalence and impact. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 915–922.
Dow, S. P., Sonies, B. C., Scheib, D., Moss, S. E., & Leonard, H. L. (1995). Practical guidelines for the assessment and treatment of selective mutism. Journal of the American Academy of Child and Adolescent Psychiatry, 34, 836–846.
Drabick, D. A. G., Ollendick, T. H., & Bubier, J. L. (2010). Co-occurrence of ODD and anxiety: Shared risk processes and evidence for a dual-pathway model. Clinical Psychology Science and Practice, 17, 307–318.
Dummit, E. S., Klein, R. G., Tancer, N. K., Asche, B., & Martin, J. (1996). Fluoxetine treatment of children with selective mutism: An open trial. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 615–621.
Dummit, E. S., Klein, R. G., Tancer, N. K., Asche, B., Martin, J., & Fairbanks, J. A. (1997). Systematic assessment of 50 children with selective mutism. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 653–660.
Dunn, L. M., & Dunn, L. M. (1997). Peabody picture vocabulary test III-revised. Circle Pines, MN: American Guidance Services.
Edison, S. C., Evans, M. A., McHolm, A. E., Cunningham, C. E., Nowakowski, M. E., Boyle, M., & Schmidt, L. A. (2011). An investigation of control among parents of selectively mute, anxious, and non-anxious children. Child Psychiatry and Human Development, 42, 270–290.
Elizur, Y., & Perednik, R. (2003). Prevalence and description of selective mutism in immigrant and native families: A controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1451–1459.
First, M. B. (2014). DSM-5 handbook of differential diagnosis. Washington, DC: American Psychiatric Publishing.
Ford, M. A., Sladeczek, I. E., Carlson, J., & Kratochwill, T. R. (1998). Selective mutism: Phenomenological characteristics. School Psychology Quarterly, 13, 192–227.
Garcia-Coll, C., Kagan, J., & Reznick, J. S. (1984). Behavioral inhibition in young children. Child Development, 55, 1005–1019.
Golwyn, D. H., & Sevlie, C. P. (1999). Phenelzine treatment of yin four prepubertal children. Journal of Child and Adolescent Psychopharmacology, 9, 109–113.
Hayden, T. L. (1980). Classification of elective mutism. Journal of the American Academy of Child Psychiatry, 19, 118–133.
Hesselman, S. (1983). Elective mutism in children 1877-1981: A literary summary. Acta Paedopsychiatrica, 49, 297–310.
Hirshfeld-Becker, D. R., Micco, J., Henin, A., Bloomfield, A., Biederman, J., & Rosenbaum, J. (2008). Behavioral inhibition. Depression and Anxiety, 25, 357–367.
Kaakeh, Y., & Stumpf, J. L. (2008). Treatment of selective mutism: Focus on selective serotonin reuptake inhibitors. Pharmacotherapy, 28, 214–224.
Kagan, J. (1994). Galen’s prophecy. Temperament in human nature. Boulder, CO: Westview Press.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for Affective Disorders and Schizophrenia for school-age children–present and life time version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988.
Kazdin, A. E. (1982). Single case research designs: Methods for clinical and applied settings. New York: Oxford University Press.
Kearney, C. A. (2008). School absenteeism and school refusal behavior in youth: A contemporary review. Clinical Psychology Review, 28, 451–471.
Keeton, C., & Crosby Budinger, M. (2012). Social phobia and selective mutism. Child and Adolescent Psychiatric Clinics of North America, 21, 621–641.
Kolvin, I., & Fundudis, T. (1981). Elective mute children: Psychological development and background factors. Journal of Child Psychology and Psychiatry, 22, 219–232.
Kopp, S., & Gillberg, C. (1997). Selective mutism: A population-based study. Journal of Child Psychology and Psychiatry, 38, 257–262.
Kristensen, H. (2000). Selective mutism and comorbidity with developmental disorder/delay, anxiety disorder, and elimination disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 39, 249–256.
Kristensen, H., & Torgersen, S. (2001). MCMI-II personality traits and symptom traits in parents of children with selective mutism: A case-control study. Journal of Abnormal Psychology, 110, 648–652.
Kristensen, H., & Torgersen, S. (2002). A case-control study of EAS child and parental temperaments in selectively mute children with an without a comorbid communication disorder. Nordic Journal of Psychiatry, 56, 347–353.
Kumpulainen, K., Räsänen, E., Raaska, H., & Somppi, V. (1998). Selective mutism among second-graders in elementary school. European Child and Adolescent Psychiatry, 7, 24–29.
Kussmaul, A. (1877). Die störungen der sprache (The disturbances of speech). Basel, Switzerland: Benno Schwabe.
La Greca, A. M., & Stone, W. L. (1993). The social anxiety scale for children-revised: Factor structure and concurrent validity. Journal of Clinical Child Psychology, 22, 17–27.
Letamendi, A. M., Chavira, D. A., Hitchcock, C. A., Roesch, S. C., Shipon-Blum, E., & Stein, M. B. (2008). Selective Mutism Questionnaire: Measurement structure and validity. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 1197–1204.
Levin-Decanini, T., Connolly, S. D., Simpson, D., Suarez, L., & Jacob, S. (2013). Comparison of behavioral profiles for anxiety-related comorbidities including ADHD and selective mutism in children. Depression and Anxiety, 30, 857–864.
Manassis, K., Fung, D., Tannock, R., Sloman, L., Fiksenbaum, L., & McInnes, A. (2003). Characterizing selective mutism: Is it more than social anxiety? Depression and Anxiety, 18, 153–161.
Manassis, K., Tannock, R., Garland, J., Minde, K., McInnes, A., & Clark, S. (2007). The sounds of silence: Language, cognition, and anxiety in selective mutism. Journal of the American Academy of Child and Adolescent Psychiatry, 46, 1187–1195.
McInnes, A., Fung, D., Manassis, K., Fiksenbaum, L., & Tannock, R. (2004). Narrative skills in children with selective mutism: An exploratory study. American Journal of Speech and Language Pathology, 13, 304–315.
McLeod, B. D., Wood, J. J., & Weisz, J. R. (2007). Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review, 27, 155–172.
Moldan, M. B. (2005). Selective mutism and self-regulation. Clinical Social Work Journal, 33, 291–307.
Mowrer, O. H. (1960). Learning theory and behavior. New York: Wiley.
Muchnik, C., Ari-Even Roth, D., Hildesheimer, M., Arie, M., Bar-Haim, Y., & Henkin, Y. (2013). Abnormalities in auditory efferent activities in children with selective mutism. Audiology and Neurotology, 18, 353–361.
Mulligan, C.A. (2012). Selective mutism: Identification of subtypes and influence on treatment. Philadelphia College of Osteopathic Medicine Psychology Dissertations, Paper 210.
Muris, P. (2007). Normal and abnormal fear and anxiety in children and adolescents. Oxford, UK: Elsevier.
Muris, P. (2012). Treatment of childhood anxiety disorders: What is the place for antidepressants? Expert Opinion on Pharmacotherapy, 13, 43–64.
Muris, P., Steerneman, P., Merckelbach, H., Holdrinet, I., & Meesters, C. (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12, 387–393.
Murray, D. C. (1971). Talk, silence, and anxiety. Psychological Bulletin, 75, 244–260.
National Institute of Mental Health. (1991). Diagnostic interview schedule for children. Rockville, MD: National Institute of Mental Health.
Nowakowski, M. E., Cunningham, C. E., McHolm, A. E., Evans, M. A., Edison, S., Pierre, J. S., et al. (2009). Language and academic abilities in children with selective mutism. Infant and Child Development, 18, 271–290.
Nowakowski, M. E., Tasker, S. L., Cunningham, C. E., McHolm, A. E., Edison, S., Pierre, J. S., et al. (2011). Joint attention in parent-child dyads involving children with selective mutism: A comparison between anxious and typically developing children. Child Psychiatry and Human Development, 42, 78–92.
Oerbeck, B., Stein, M. B., Wentzel-Larsen, T., Langrud, Ø., & Kristensen, H. (2014). A randomized controlled trial of a home and school-based intervention for selective mutism: Defocused communication and behavioral techniques. Child and Adolescent Mental Health, 19, 192–198.
Ollendick, T. H., & Benoit, K. (2012). A parent-child interactional model of social anxiety disorder in youth. Clinical Child and Family Psychology Review, 15, 81–91.
Ollendick, T. H., & King, N. J. (2012). Evidence-based treatments for children and adolescents: Issues and controversies. In P. C. Kendall (Ed.), Child and adolescent therapy: Cognitive-behavioral procedures (pp. 499–519). New York: Guilford Publications Inc.
Omdal, H., & Galloway, D. (2008). Could selective mutism be re-conceptualised as a specific phobia of expressive speech? An exploratory post hoc study. Child and Adolescent Mental Health, 13, 74–81.
Ooi, Y. P., Raja, M., Sung, S. C., Fung, D. S. S., & Koh, J. B. K. (2012). Application of a web-based cognitive-behavioural therapy programme for the treatment of selective mutism in Singapore: A case series study. Singapore Medical Journal, 53, 446–450.
Pionek Stone, B., Kratochwill, T. R., Sladezcek, I., & Serlin, R. C. (2002). Treatment of selective mutism: A best-evidence synthesis. School Psychology Quarterly, 17, 168–190.
Powell, S., & Dalley, M. (1995). When to intervene in selective mutism: The multimodal treatment of a case of persistent selective mutism. Psychology in the Schools, 32, 114–123.
Rapee, R. M., Schniering, C. A., & Hudson, J. L. (2009). Anxiety disorders during childhood and adolescence: Origins and treatment. Annual Review of Clinical Psychology, 5, 311–341.
Remschmidt, H., Poller, M., Herpertz-Dahlmann, B., Hennighausen, K., & Gutenbrunner, C. (2001). A follow-up study of 45 patients with elective mutism. European Archives of Psychiatry and Clinical Neuroscience, 251, 284–296.
Rice, T. K. (2008). Familial resemblance and heritability. Advances in Genetics, 60, 35–49.
Russo, M. F., & Beidel, D. C. (1994). Comorbidity of childhood anxiety and externalizing disorders: Prevalence, associated characteristics, and validation issues. Clinical Psychology Review, 14, 199–221.
Scott, S., & Beidel, D. C. (2011). Selective mutism: An update and suggestions for future research. Current Psychiatry Reports, 13, 251–257.
Segal, N. L. (2003). ‘Two’ quiet: Monozygotic female twins with selective mutism. Clinical Child Psychology and Psychiatry, 8, 473–488.
Sharkey, L., McNicholas, F., Barry, E., Begley, M., & Ahern, S. (2008). Group therapy for selective mutism: A parents’ and children’s treatment group. Journal of Behavior Therapy and Experimental Psychiatry, 39, 538–545.
Sharp, W. G., Sherman, C., & Gross, A. M. (2007). Selective mutism and anxiety: A review of the current conceptualization of the disorder. Journal of Anxiety Disorders, 21, 568–579.
Silverman, W. K., & Albano, A. M. (1996). The anxiety disorders interview schedule for children and parents (ADIS-C/P). San Antonio, TX: Psychological Corporation.
Stein, M. B., Yang, B. Z., Chavira, D. A., Hitchcock, C. A., Sung, S. C., Shipon-Blum, E., & Gelernter, J. (2011). A common genetic variant in the neurexin superfamily member CNTNAP2 is associated with increased risk for selective mutism and social anxiety-related traits. Biological Psychiatry, 69, 825–831.
Steinhausen, H. C., & Juzi, C. (1996). Elective mutism: An analysis of 100 cases. Journal of the American Academy of Child and Adolescent Psychiatry, 35, 606–614.
Steinhausen, H. C., Wachter, M., Laimböck, K., & Winkler Metzke, C. (2006). A long-term outcome study of selective mutism in childhood. Journal of Child Psychology and Psychiatry, 47, 751–756.
Thomas, A., & Chess, S. (1977). Temperament and development. New York, NY: Brunner/Mazel.
Tramer, M. (1934). Elektiver Mutismus bei Kindern (Selective mutism in children). Zeitschrift für Kinderpsychiatrie, 1, 30–35.
Vecchio, J. L., & Kearney, C. A. (2005). Selective mutism in children: Comparison to youths with and without anxiety disorders. Journal of Psychopathology and Behavioral Assessment, 27, 31–37.
Vecchio, J. L., & Kearney, C. A. (2009). Treating youths with selective mutism with an alternating design of exposure-based practice and contingency management. Behavior Therapy, 40, 380–392.
Viana, A. G., Beidel, D. C., & Rabian, B. (2009). Selective mutism: A review and integration of the last 15 years. Clinical Psychology Review, 29, 57–67.
White, S. W., Oswald, D., Ollendick, T. H., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29, 216–229.
Whiteside, S. P., & Ollendick, T. H. (2009). Developmental perspectives on anxiety classification. In D. McKay, J. S. Abramowitz, S. Taylor, & G. J. G. Asmundson (Eds.), Current perspectives on the anxiety disorders: Implications for DSM-V and beyond (pp. 303–325). New York: Springer.
Wright, H. H., Cuccaro, M. L., Leonardt, T. V., Kendall, D. F., & Anderson, J. H. (1995). Case study: Fluoxetine in the multimodal treatment of a preschool child with selective mutism. Journal of American Academy of Child and Adolescent Psychiatry, 34, 857–862.
Yeganeh, R., Beidel, D. C., & Turner, S. M. (2006). Selective mutism: More than social anxiety? Depression and Anxiety, 23, 117–123.
Yeganeh, R., Beidel, D. C., Turner, S. M., Pina, A. A., & Silverman, W. K. (2003). Clinical distinctions between selective mutism and social phobia: An investigation of childhood psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry, 42, 1069–1075.
Young, B. J., Bunnell, B. E., & Beidel, D. C. (2012). Evaluation of children with selective mutism and social phobia: A comparison of psychological and psychophysiological arousal. Behavior Modification, 36, 525–544.
Acknowledgments
We thank R. Lindsey Bergman, UCLA Department of Psychiatry and Biobehavioral Science, Los Angeles, USA, for providing us with the table of her intervention for children with selective mutism.
Conflict of interest
The authors have no potential conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Muris, P., Ollendick, T.H. Children Who are Anxious in Silence: A Review on Selective Mutism, the New Anxiety Disorder in DSM-5. Clin Child Fam Psychol Rev 18, 151–169 (2015). https://doi.org/10.1007/s10567-015-0181-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10567-015-0181-y