Abstract
Background
The hypothalamic–pituitary–adrenal (HPA) axis constitutes an important biological component of the stress response commonly studied through the measurement of cortisol. Limited research has examined HPA axis dysregulation in youth exposed to disasters.
Objective
This study examined HPA axis activation in adolescent Hurricane Katrina survivors relative to a non-exposed community comparison group. It was hypothesized that Hurricane Katrina survivors would experience lower basal morning cortisol and greater cortisol suppression with low-dose dexamethasone than the comparison group.
Methods
Fourteen Hurricane Katrina survivors and nine non-exposed community residents were assessed 21 months after the disaster in this observational pilot study with an experimental component. Salivary cortisol was collected at baseline and following low-dose dexamethasone challenge. Posttraumatic stress disorder (PTSD), depressive, and externalizing symptoms were assessed with self-report instruments.
Results
Relative to the community participants, Hurricane Katrina survivors had significantly higher PTSD and depressive symptoms, and, as hypothesized, lower basal morning salivary cortisol. In the full sample, basal morning cortisol was negatively associated with depressive and externalizing symptoms. The hypothesis that low-dose dexamethasone challenge would show more cortisol suppression in Hurricane Katrina survivors than the comparison group was not supported, perhaps reflecting more depressive symptoms in the survivors or due to a floor effect of low cortisol levels.
Conclusions
The results augment the extant literature on youth exposed to disasters by emphasizing the importance of depressive and externalizing symptoms as well as PTSD symptoms in HPA axis functioning. Future research is needed to fully elucidate HPA axis functioning in youth exposed to disasters.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hurricane Katrina, which made landfall on August 29, 2005, resulted in mass evacuation and displacement. Families relocated across the country—some moved to communities where relatives resided, some moved to specific locations in hope of employment, and some traveled to places where they knew no one and never had been. Evacuation, displacement, and relocation can create additional burden for children and families in the context of disasters (Blaze and Shwalb 2009; Lonigan et al. 1994; Milne 1977; Russoniello et al. 2002). A number of conditions have been studied in children exposed to disasters including posttraumatic stress disorder (PTSD) and PTSD symptoms which are the most commonly assessed outcomes in child disaster studies (Silverman and La Greca 2002), depression (Silverman and La Greca 2002), and externalizing reactions (Marsee 2008; Shaw et al. 1995). Depression may increase in importance over time (Goenjian et al. 1995; Silverman and La Greca 2002). In some studies, behavior problems improve in the early aftermath of an event, typically reverting to pre-disaster levels over time (Shaw et al. 1995; Stuber et al. 2005). In addition to emotional and behavioral reactions, biological processes associated with the hypothalamic–pituitary–adrenal (HPA) axis have been examined in child disaster studies through the measurement of cortisol levels (Goenjian et al. 1996, 2003; Pfeffer et al. 2007; Vigil et al. 2009, 2010) and suppression with dexamethasone challenge (Goenjian et al. 1996; Pfeffer et al. 2007), a pharmacological test of the negative feedback mechanism of the HPA axis (de Kloet et al. 2006).
Factors Influencing the Child’s Stress Response
In a seminal paper explicating their Adaptive Calibration Model, Del Giudice et al. (2011) ascribed individual differences in stress responsiveness to adaptive processes across development. The stress response system regulates the development of various life history strategies—the individual’s allocation of time, energy, and resources to various adaptive activities such as growth and learning, competition and risk-taking, and mating. Patterns of activation and responsiveness of the child’s stress response system during early development influence the child’s vulnerability to environmental factors, and later stress responsiveness is influenced by the child’s developmental stage with important “switch points” at developmental transitions (e.g., prenatal, early postnatal, puberty) providing opportunities for refinement in response pathways. Gender has a central role in the child’s stress response with important gender differences in the type of events that stimulate response, in the use of strategies to respond to environmental cues, in the distribution of response patterns, and in correlates of response. Environment factors (e.g., across degrees of safety and danger, stress, and predictability) also influence the calibration of the child’s stress responsiveness including HPA axis activation (Del Giudice et al. 2011).
HPA Axis Functioning and Psychological Symptoms and Conditions
The HPA axis regulates a number of body processes and is central to the individual’s response to stress. The HPA axis has been examined in association with trauma and both internalizing and externalizing behaviors in children. With respect to trauma, Heim et al. (2000) presented conflicting evidence in their review of studies of adults but concluded that PTSD was associated with decreased cortisol and increased suppression with dexamethasone challenge. Studies of traumatized children have found dysregulation of the HPA axis as well but the nature of the dysregulation has not been conclusively established (De Bellis and Zisk 2014). Studies of traumatized children have found lower, higher, and no difference in cortisol concentrations with blunted, enhanced, and no response to challenge tests relative to non-traumatized children (De Bellis and Zisk 2014).
Both internalizing and externalizing behaviors are associated with dysregulation in the HPA axis and changes in cortisol levels in children (Ruttle et al. 2011) with research producing contradictory results. Anxiety and depressive disorders have been found to be associated with elevated cortisol (Nader and Weems 2011). A meta-analysis of HPA axis dysregulation with depression revealed higher basal cortisol levels throughout the day and less suppression with dexamethasone in depressed children and adolescents relative to non-depressed controls (Lopez-Duran et al. 2009). Others have identified a diurnal pattern in the differences in basal cortisol levels between individuals with and without psychological symptoms (Gunnar and Vazquez 2001; Miller et al. 2007). Dysregulation of HPA axis functioning may change when symptoms become chronic. In their study of HPA axis functioning in early adolescents, Ruttle et al. (2011) found that concurrent internalizing behavior in adolescence was associated with higher morning cortisol while youth with more internalizing behaviors during childhood had lower morning cortisol when examined at adolescence.
Research on externalizing problems and HPA axis functioning also has produced discrepant results with some evidence suggesting that age is a factor in the relationship (Alink et al. 2007). A number of studies have documented low basal cortisol in association with antisocial behavior, conduct problems, and disruptive behavior (McBurnett et al. 2000; Pajer et al. 2001; Ruttle et al. 2011; Shirtcliff et al. 2005; Susman 2006) though not all research agrees (Alink et al. 2007; Fairchild et al. 2008; Klimes-Dougan et al. 2001; Shirtcliff and Essex 2008; van Bokhoven et al. 2005). No known studies have examined the relationship between suppression on dexamethasone challenge and externalizing conditions in children.
HPA Axis Functioning in Youth Exposed to Disasters
A limited body of research has examined HPA axis dysregulation in youth exposed to disasters (Goenjian et al. 1996, 2003; Pfeffer et al. 2007; Vigil et al. 2009, 2010). For example, in studies conducted 2 months after Hurricane Katrina, relocated adolescents had relatively lower cortisol levels than non-exposed demographically-matched youth (Vigil et al. 2009, 2010). While there was no relationship between cortisol and depression, aggression was positively correlated with salivary cortisol level (Vigil et al. 2010). Children bereaved by the September 11, 2001, terrorist attacks had higher cortisol levels than non-bereaved children one and one-half years later while bereaved children with PTSD showed significantly lower afternoon cortisol levels and significantly greater cortisol suppression with dexamethasone challenge than bereaved children without PTSD (Pfeffer et al. 2007). Goenjian et al. (1996) compared adolescents from two cities in Armenia at different distances from the epicenter of a massive earthquake 5 years after the disaster. Exposure and PTSD symptoms were associated with lower basal morning salivary cortisol levels and greater suppression with low-dose dexamethasone and there was a positive correlation between reexperiencing symptoms and cortisol suppression. In another study of adolescent survivors 6.5 years after the same earthquake, severity of PTSD and depression symptoms, but not exposure, was negatively correlated with basal morning cortisol levels (Goenjian et al. 2003).
Summary
The HPA axis constitutes an important biological component of an individual’s stress response system which is influenced by a number of factors including development, gender, and environmental circumstances and conditions. HPA axis functioning is commonly studied through the measurement of cortisol and has been examined in association with trauma and internalizing and externalizing behaviors. Studies of traumatized children have uncovered HPA axis dysregulation but the nature of the dysregulation remains unclear. The limited research in this area in youth exposed to disasters has focused attention on this important biological component of stress without conclusively establishing the relationship of HPA axis dysregulation and PTSD symptoms, depression, or externalizing behaviors.
The Current Study
This report describes an observational pilot study with an experimental component comparing displaced adolescent Hurricane Katrina survivors who relocated to Oklahoma with a comparison sample from the community where the survivors relocated. The study, conducted on average 21 months after the disaster, examined the association of basal cortisol levels and of cortisol suppression on dexamethasone challenge with depression and externalizing problems as well as PTSD symptoms. Research on HPA axis dysregulation and trauma has produced inconsistent results related to a number of factors such as age/development, gender, time since exposure, and timing of measurement. Based on child disaster studies conducted years after exposure, it was hypothesized that Hurricane Katrina survivors would experience lower basal morning cortisol and greater suppression with low-dose dexamethasone than the comparison group.
Methods
Participants
A pilot sample of adolescents who had relocated to Oklahoma after Hurricane Katrina was recruited for study between March 19, 2007, and January 28, 2008, 19–29 months (mean = 21.3 months; SD = 2.8) after the disaster. These participants and a comparison group of adolescents from Oklahoma who had no direct exposure to Hurricane Katrina were recruited through direct outreach, flyers posted in relief agencies (e.g., the American Red Cross, Catholic Charities, the Mental Health Association, local churches, public schools, community mental health centers), newspaper and radio advertisement, and word of mouth in the urban Oklahoma community where the survivor and comparison participants were residing. All participants were physically healthy and not taking psychotropic or other medications that might confound biological assessments. Informed consent was obtained from all participants. Participants received $100 for their effort in this 2-day psychometric and biological assessment. Taxi fare was paid for travel to and from assessment sessions for participants who did not have transportation.
Materials and Procedure
Support for this research was provided by the Oklahoma Center for the Advancement of Science and Technology. All authors disclose no relationships that may be perceived as a conflict of interest. The study was approved by the Institutional Review Board of the University of Oklahoma Health Sciences Center in Oklahoma City.
This observational pilot study included an experimental component assessing cortisol and dexamethasone suppression as well as psychometrics. On Day 1, after completing consent forms, basal morning salivary cortisol specimens were collected at 8:00 a.m. from all participants before psychometric assessments to preclude the possibility that administering psychometric assessment batteries first might induce biological responses that could affect cortisol measurement. All participants were sent home with a low dose of dexamethasone (0.5 mg) with instructions for oral administration at 11:00 p.m. on Day 1. A reminder call was made that evening. Day 2 cortisol specimens were obtained at 8:00 a.m. and 4:00 p.m. Participants were instructed to abstain from caffeine and nicotine intake before cortisol sampling and to rinse their mouth with water and avoid eating or drinking 15 min before all salivary samples were collected on Day 1 and Day 2. No participants reported adverse reactions to dexamethasone. All assessments were conducted in the university-based laboratory of one of the investigators (PT).
Cortisol Assays
Specimens for measuring salivary cortisol were obtained in Salivette tubes and were assayed in duplicate using salivary cortisol kits provided by Salimetrics, LLC. Specimens were centrifuged for 2 min and stored at −20 °C, with salivary cortisol levels later measured by radioimmunoassay methods (Salimetrics, LLC; State College, PA). Three salivary cortisol measurements constituted the outcome variables of this study: Day 1 8:00 a.m. (basal), Day 2 8:00 a.m., and Day 2 4:00 p.m. levels of salivary cortisol. The morning salivary cortisol response to a low dose of dexamethasone suppression was analyzed by computing a rate of suppression according to the formula: 100 × (basal Day 1 morning − post dexamethasone Day 2 morning)/basal Day 1 morning.
Psychometric Assessments
Participants were interviewed to determine their trauma exposure. They also provided individual written self-report information related to PTSD symptoms, depression, and externalizing behaviors. The study did not include reports from participants’ parents or teachers.
Exposure to lifetime trauma and current PTSD symptoms were assessed using the UCLA PTSD Reaction Index (RI) (Steinberg et al. 2004). Participants were asked to think about a bad thing that happened to them and to quantify current PTSD RI items describing their reaction to this event. The reliability statistics (Cronbach’s alpha) in this study sample were 0.74, 0.75, and 0.89 for reexperiencing, avoidance/numbing, and hyperarousal subscales respectively. PTSD caseness was defined using the clinical cut-off score of 38 on the PTSD RI scale (Steinberg et al. 2004).
The Children’s Depression Inventory (CDI) (Kovacs 1985), a 27-item questionnaire, was used to measure current depression symptoms. The reliability (Cronbach’s alpha) of the instrument in this study sample was 0.86. A score of 12 was used as the cut-off for clinical depression. Depression status was defined as not depressed (CDI < 12) or depressed (CDI ≥ 12) (Kovacs 1992).
Externalizing symptomatology was measured with the 15-item rule-breaking behavior and the 17-item aggressive behavior subscales of the Youth Self-Report (YSR) (Achenbach and Rescorla 2001). The scores of both subscales were added to obtain an Externalizing Problems score. The rule-breaking behavior and the aggressive behavior subscales had good reliability in this study sample with Cronbach’s alpha of 0.84 and 0.80, respectively. Based on scoring for these subscales, the clinical cut-off for externalizing problems was 19 for boys and 20 for girls (Achenbach 2001).
Statistical Analysis
The values of cortisol levels were log-transformed to meet the normality assumption of multivariate model residuals. Independent t tests were used to compare the means of log-transformed cortisol levels in hurricane survivors and the comparison group. As the other continuous variables (age and psychological symptom scores) were only used as independent variables in the modeling of cortisol levels, they were not transformed but were analyzed with nonparametric tests instead. Since the variances of PTSD RI and CDI scores of survivors and the comparison group were significantly different, the Fligner–Policello (F–P) robust rank test (Fligner and Policello 1981) was preferred over the Wilcoxon’s rank sums test to compare the mean ranks of these variables. In contrast to the Wilcoxon’s rank sums test, the F–P test does not require the variances in both samples to be equal. For consistency, the F–P test also was used to compare the Externalizing Problems score of the survivor and comparison groups. The effect size of the independent t test was calculated as d = m d /s, where m d is the mean difference between the two groups, and s is the standard deviation of the difference. For the F–P test, the effect size was computed as r = z/sqrt(n), where z is the F–P statistic and n is the study sample size (Fritz et al. 2012). Bivariate correlations were estimated with Spearman correlation coefficients. A piecewise linear model was fitted to determine whether the overtime trajectory of salivary cortisol of adolescents exposed to Hurricane Katrina was significantly different from that of the comparison group. A knot (i.e., the place where the pieces of the model join) was placed at 24 h post baseline (i.e., Day 2 at 8:00 a.m.) as this was the time of the first measurement of salivary cortisol after the dexamethasone challenge. Salivary cortisol levels were log-transformed to meet the model assumption of normality. Hence, the basic piecewise model with time and exposure to Hurricane Katrina as covariates can be written as:
where i = 1,…,23 is the participant index; j = 1, 2, 3 is the salivary cortisol measurement index; Exposure i = 1 if the participant had been exposed to Hurricane Katrina, and Exposure i = 0 if the participant was in the comparison group. The covariance matrix of the repeated measures was assumed unstructured. The model was subsequently adjusted for participants’ age, sex, and psychological symptoms (PTSD RI total, CDI, and YSR Externalizing Problems scores). The model parameters were estimated using restricted maximum likelihood.
Statistical significance was set at α = 0.05. All the reported p values are two-sided. F–P tests were performed with the R package NSM (Schneider et al. 2013). All the other statistical analyses were conducted using SAS 9.2 (SAS Institute, Cary, NC).
Results
Fourteen African-American adolescents who had been directly exposed to Hurricane Katrina (survivor group) and nine African-American youth from an urban community in Oklahoma who had no direct exposure to the hurricane (comparison group) participated in the study. Eleven (78.6 %) survivors were in the disaster-stricken area when the hurricane hit their community witnessing the storm, flooding, and/or the destruction of their neighborhoods and homes. The other three (21.4 %) survivors had evacuated the area within a few days before the hurricane made landfall. Two (14.3 %) survivors, who were directly exposed to the storm, had been separated from their family. All of the survivors had been displaced because of the hurricane and all of their families had relocated to Oklahoma. The age of survivors ranged from 12 to 17 years with an average of 14.5 years (SD = 1.8), while youth in the comparison group were between 13 and 16 years of age with an average of 14.8 years (SD = 1.2). Seven (50.0 %) survivors and 5 (55.6 %) non-exposed adolescents were female. There was no significant difference in age (F–P: p = 0.7308) or sex (Fisher’s exact test: p = 1.0) between the survivors and the comparison group.
Psychological Symptoms
Two of the community participants reported exposure to traumatic events. One had been physically assaulted 2 weeks before the assessment (PTSD RI total score = 22) and one had been attacked by a dog and exposed to a house fire approximately 1 year before the current study (PTSD RI total score = 2). Neither participant scored in the clinical range on the PTSD RI.
Hurricane Katrina survivors had higher scores than the comparison group on the PTSD RI avoidance/numbing (F–P: p = 0.0154; Table 1) and hyperarousal (F–P: p = 0.0396; Table 1) subscales as well as higher total PTSD RI scores (F–P: p = 0.0498; Table 1). There was no significant difference between the groups on the PTSD RI reexperiencing subscale (F–P: p = 0.1138; Table 1). Two survivors and none of the comparison participants scored above the clinical cut-off of 38 on the PTSD RI scale but the difference was not statistically significant (Fisher’s exact test: p = 0.4935).
Current depression symptom scores, measured with the CDI, were significantly higher in Hurricane Katrina survivors than the comparison group (F–P: p = 0.019; Table 1). Six (42.9 %) survivors scored above the clinical cut-off of 12 on the CDI, while none of the comparison group participants scored above the cut-off (Fisher’s exact test: p = 0.0481).
The Externalizing Problems score was higher in Hurricane Katrina survivors than the comparison group although the difference was not statistically significant (F–P: p = 0.4268; Table 1). Four (28.6 %) of the survivors, and only one (11.1 %) of the comparison participants, scored above the clinical cut-off for externalizing problems, but the difference was not statistically significant (Fisher’s exact test: p = 0.3602).
Bivariate analyses revealed statistically significant pairwise correlations among the three PTSD symptom subscales (reexperiencing, avoidance/numbing, and hyperarousal) and also between depressive symptoms and hyperarousal symptoms. Aggressive behavior was positively correlated with avoidance/numbing, hyperarousal, and depressive symptoms; however these associations marginally missed statistical significance at the 0.05 level (p = 0.0572, 0.0796 and 0.0821, respectively; Table 2). Likewise, the positive association between avoidance/numbing and depressive symptoms narrowly missed significance (p = 0.0721; Table 2).
Salivary Cortisol
Log-transformed basal morning (Day 1 a.m.) salivary cortisol levels were, on average, lower in Hurricane Katrina survivors than in the comparison participants (p = 0.0107; Table 1). There was no significant association between sex and any of the log-transformed measured levels of salivary cortisol (t-tests: p = 0.2106 for Day 1 a.m.; p = 0.4787 for Day 2 a.m.; and p = 0.7262 for Day 2 p.m. salivary cortisol levels). Likewise, age was not significantly correlated with any of the log-transformed cortisol values (Spearman correlation r = 0.01; p = 0.9531 for Day 1 a.m.; r = 0.14; p = 0.5191 for Day 2 a.m.; and r = 0.01; p = 0.9714 for Day 2 p.m.).
CDI and Externalizing Problems scores were each significantly and negatively correlated with Day 1 basal morning salivary cortisol levels, but not with Day 2 a.m. or Day 2 p.m. salivary cortisol levels (Table 3).
There was no significant difference between the groups in log-transformed salivary cortisol levels after the administration of 0.5 mg dexamethasone (p = 0.1344 and p = 0.2855 for Day 2 a.m. and Day 2 p.m. salivary cortisol levels, respectively; Table 1), and the cortisol suppression rate in the groups was not significantly different (p = 0.8773; Table 1).
The multivariate model using log-units of salivary cortisol as the outcome and adjusting for age, sex, exposure to Hurricane Katrina, and PTSD symptoms confirmed the significant negative association between basal morning salivary cortisol and both depressive symptoms (β = −0.06; p = 0.0041; Table 4) and externalizing problems (β = −0.07; p = 0.0003; Table 4). PTSD symptoms and exposure to Hurricane Katrina were not significantly associated with salivary cortisol, however (Table 4).
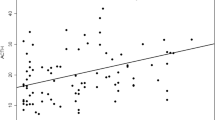
There was a significant decrease in salivary cortisol in both groups after the administration of 0.5 mg dexamethasone, but the rates of decrease in the two groups were not significantly different. Indeed the effects of the interaction terms between hurricane exposure and time were not significant (Fig. 1; Table 4).
The results of the dexamethasone suppression test were further analyzed by comparing the rates of cortisol suppression of participants in the highest quartile (salivary cortisol ≥ 0.518 μg/dl; n = 6; Table 5) of basal morning cortisol to those of participants in the lowest quartile (salivary cortisol ≤ 0.230 μg/dl; n = 6; Table 5) of basal morning cortisol. The difference was statistically significant (F–P: p = 0.0433), with the mean rate of suppression being higher in participants in the highest quartile of basal cortisol [86.5 (SD = 22.5) vs. 60.2 (SD = 24.6)]. All six participants in the lowest quartile of basal cortisol were Hurricane Katrina survivors, while only one participant in the highest-quartile group had been exposed to the hurricane. Depressive symptoms were significantly higher in the lowest-quartile group, in which four participants scored in the clinical range of depression, compared to the highest-quartile group, in which only one participant, a survivor, scored above the clinical cut-off (F–P: p = 0.0260). The Externalizing Problems score was higher in the lowest-quartile group compared to the highest-quartile group, but the difference between the two quartile groups marginally missed significance (F–P: p = 0.0563).
Discussion
This pilot study comparing relocated adolescent Hurricane Katrina survivors and non-exposed youth from the community where the survivors were currently residing revealed significantly greater total PTSD, avoidance/numbing, and hyperarousal symptoms and significantly greater depression symptoms in survivors than the comparison group. Externalizing problems were higher in survivors relative to the comparison group, but the difference was not statistically significant, perhaps due to the small sample size. With respect to the clinical relevance of the psychological outcomes, significantly more survivors than comparison participants scored above the clinical cut-off for depression but not for PTSD or externalizing problems.
This study adds to a growing literature examining HPA axis activation in child and adolescent disaster survivors (Goenjian et al. 1996, 2003; Pfeffer et al. 2007; Vigil et al. 2009, 2010). Consistent with previous child disaster research (Goenjian et al. 1996, 2003; Vigil et al. 2009, 2010), and as hypothesized, Hurricane Katrina survivors in the current study had lower basal salivary cortisol levels than the comparison group. Although marginally missing statistical significance, the results of the current study are consistent with the findings in adolescent earthquake survivors of negative correlations between basal morning cortisol and reexperiencing (Goenjian et al. 1996), avoidance/numbing, hyperarousal, and total PTSD symptoms (Goenjian et al. 2003) years after the event. In the current study, a multivariate regression model adjusting for participants’ demographics revealed that cortisol levels were negatively associated with depression and externalizing problems, but not with PTSD symptoms or hurricane exposure. Contrary to the study hypothesis, the mean cortisol suppression rate after dexamethasone was not significantly different between the survivor and comparison groups.
Development, gender, and environmental conditions influence HPA axis activity in traumatized youth (Nader and Weems 2011). Other potential factors include the type or nature of the trauma, controllability and severity of the trauma, time since trauma exposure, duration of the trauma, and the emotions (e.g., shame) and psychiatric sequelae (e.g., PTSD) elicited by the trauma as well as methodological issues in cortisol assessment (De Bellis and Zisk 2014; Miller et al. 2007; Nader and Weems 2011). Of these, time since trauma exposure has received considerable attention in child and adolescent samples (Bevans et al. 2008, 2009; De Bellis 2001; Ruttle et al. 2011; Weems and Carrión 2007).
Time Since Trauma Exposure
The time interval between exposure to the stressor and assessment may have influenced the results of the current study. De Bellis (2001) speculated that after an initial normal increase in cortisol post trauma, as time passes, HPA axis functioning changes in the direction of lower cortisol levels over time. It is not entirely clear how to interpret this down regulation. It may represent the body’s attempt to compensate for elevated levels and return to normal (Miller et al. 2007). It also is possible that this time since exposure represents chronicity of the stressor or a period of accumulating stressors. In their meta-analysis, Miller et al. (2007) concluded that lower concentrations of morning cortisol and more pronounced suppression of cortisol following dexamethasone challenge were associated with exposure to chronic stress. Down regulation of the HPA axis may reflect more serious dysregulation with more severe consequences than hyperactivation (Badanes et al. 2011). Alternatively, the phase of hypocortisolism may support recovery and compensate for the physiological and immune effects of the extended period of elevated cortisol (Del Giudice et al. 2011).
In their study of maltreated children, Doom et al. (2014) implicated other aspects of HPA axis functioning, as well as timing, in the development of psychopathology. Finding that maltreated children with higher initial cortisol levels evidenced lower levels over time, these authors suggested that higher initial cortisol levels may be associated with HPA axis blunting. The study by Doom et al. (2014) also found greater variability in initial 4:00 p.m. cortisol level and in the cortisol secretion pattern over the study period in maltreated children relative to a non-maltreated comparison group. This greater variability may constitute a risk for illness and psychopathology. Furthermore, in their study, maltreatment and greater variability in cortisol levels were each associated with more behavior problems (Doom et al. 2014).
Child and adolescent disaster cortisol studies have been conducted months (Vigil et al. 2009, 2010) to years (Goenjian et al. 1996, 2003; Pfeffer et al. 2007) after event exposure. As cortisol levels were generally measured after a relatively long time interval from the disaster, it is possible that the observed low cortisol levels reflect HPA axis down regulation following a phase of hyperactivation after exposure to the disaster. The studies by Vigil’s team (2009, 2010) are of interest with respect to timing of assessment as they were conducted only 2 months after disaster exposure, a relatively short time period. Unfortunately, it is unclear what time of the day cortisol levels were lower in Hurricane Katrina survivors relative to the non-exposed comparisons, a factor that may be important in that team’s results. In their meta-analysis, Miller et al. (2007) found that people with chronic stress had lower morning cortisol levels but higher afternoon/evening cortisol levels relative to individuals without chronic stress.
Depression and Externalizing Problems
The current study augments the sparse literature establishing low cortisol in association with depression in disaster-exposed adolescents when assessed years post event (Goenjian et al. 2003). The results also are consistent with the study by Ruttle et al. (2011) which revealed that internalizing behaviors in childhood predicted lower morning cortisol when the children reached adolescence and that while stress exposure is associated with hypercortisolism initially, prolonged exposure to stress and elevated cortisol may lead to hypocortisolism over time.
The results related to externalizing problems also are consistent with the literature documenting low basal cortisol in association with antisocial behavior, conduct problems, and disruptive behavior (McBurnett et al. 2000; Pajer et al. 2001; Ruttle et al. 2011; Shirtcliff et al. 2005; Susman 2006), but not with the study by Vigil et al. (2010) conducted 2 months after Hurricane Katrina which found a positive correlation between aggression and salivary cortisol level and no significant correlation of cortisol with depression, anxiety, self-esteem, or distress. In the current study, conducted 21 months after Hurricane Katrina, behavior difficulties were associated with lower levels of cortisol. This difference in findings may reflect differences in timing since trauma exposure or other confounding factors for as noted above, the literature on HPA axis functioning and externalizing behaviors is evolving with contradictory findings yet to be reconciled.
Not only were both depression and externalizing problems associated with lower levels of basal cortisol in the current study, exposure to Hurricane Katrina and PTSD symptom scores were no longer significantly associated with basal salivary cortisol after adjusting for these covariates. Not measured in the current study, chronic and accumulated stress may affect cortisol levels and HPA axis functioning and may be particularly important in the context of natural disasters, which may disproportionately affect the most vulnerable (Masten and Narayan 2012). Thus, failure to consider conditions like depression and externalizing problems as well as accumulated stress may lead to erroneous interpretations of findings on HPA axis functioning in disaster survivor youth.
Dexamethasone Challenge
The normal response to dexamethasone challenge is a decrease in cortisol secretion with non-suppression (Lopez-Duran et al. 2009) and enhanced suppression (de Kloet et al. 2006) indicating dysregulation of the HPA axis negative feedback mechanism. While the literature suggests increased suppression of cortisol with dexamethasone challenge in traumatized adults (Heim et al. 2000), a study comparing adolescents with and without PTSD and non-traumatized controls found no difference in cortisol suppression among the three groups (Lipschitz et al. 2003). Similarly, the adolescent Hurricane Katrina survivors and the comparison group in the current study did not differ in cortisol suppression rates or in post-dexamethasone cortisol levels. More extensive analyses of the dexamethasone results in the current study revealed that participants with the highest level of basal morning cortisol, only one of whom was a Hurricane Katrina survivor, had significantly greater cortisol suppression after dexamethasone administration than participants with the lowest level of basal morning cortisol, all of whom were hurricane survivors. Depressive symptoms were significantly higher in the lowest-quartile group relative to the highest-quartile group with four participants in the lowest-quartile group and only one in the highest-quartile group scoring in the clinical range of depression. Similarly, although there was considerable variability in findings among the studies they examined, Lopez-Duran et al. (2009) found less suppression with dexamethasone challenge in depressed youth than in non-depressed youth. Thus, the failure to support the current study’s hypothesis that survivors would exhibit greater suppression with dexamethasone than the comparison group may reflect differences in depression between the survivor and comparison groups. It also is possible that the lack of suppression in the participants in the lowest-quartile group was due to a floor effect, that is, their cortisol levels were so low that they could not be further suppressed.
Limitations
One major limitation in this pilot study was the small size of the study sample. Differences in Hurricane Katrina survivor and comparison youth assessed as part of this study may have reached significance if a larger sample had been used. The small sample size may have precluded the detection of significant associations between salivary cortisol levels and the other covariates. In addition, the exclusion of youth taking psychotropic or other medications that would affect biological measures may have eliminated more symptomatic Hurricane Katrina survivors who may have experienced greater HPA axis dysregulation.
The current study sample was exclusively African American; hence, the results may not generalize to other ethnicities. Little research on ethnic differences in HPA axis functioning in youth has been conducted. DeSantis et al. (2007) found lower wakeup cortisol levels in African-American adolescents compared to their Caucasian counterparts, and higher bedtime cortisol levels in Hispanic and African-American adolescents relative to Caucasian adolescents, after adjusting for demographics, parental socioeconomic status, stress, depression, hours of sleep, and recent cigarette smoking, but were unable to determine if the results were based on genetic differences or social conditions. Dulin-Keita et al. (2012) found a “neighborhood” effect on basal morning serum cortisol in African-American—but not European-American—children using an index combining measures of parental unemployment, poverty, households headed by single mothers, and vacant housing. A related factor, socioeconomic status, was not measured or controlled for in the current study.
Both gender and age affect HPA axis functioning (Nader and Weems 2011) though these effects were not evident in the current study perhaps due to the small sample size. Age is of particular concern in this sample given that the participants spanned developmental stages from early puberty to late adolescence. Cortisol dysregulation appears to be a function of numerous other individual and stressor factors not measured in the current study. Individual factors include genetic vulnerability, previous stress experiences, personality style, psychiatric status, and coping (Heim et al. 2000; Miller et al. 2007). Factors related to the stressor include the nature and duration of threat or trauma exposure; severity, intensity, and controllability of the stressor; and time since exposure (Bevans et al. 2008; Heim et al. 2000; Miller et al. 2007). More specific aspects of the survivors’ exposure experiences might have influenced the results as might have other life stressors and trauma (before and after the disaster). Moreover, the onset and duration of PTSD symptoms, depression, and externalizing problems and the presence of chronic and accumulated stress were not measured in the current study.
The use of only one cortisol assay per participant before the dexamethasone challenge was another limitation in this study. Single-point measures are problematic because of the large transient fluctuations in cortisol (Yehuda 2001). Because of diurnal variability in cortisol levels, Weems and Carrión (2009) emphasized the importance of studying diurnal changes in cortisol rather than daily cortisol levels or levels at particular times of the day when attempting to characterize HPA axis dysregulation in association with PTSD symptoms. Thus, the comparison of mean cortisol levels may be less informative than measures of diurnal patterns and may add to the confusion in interpreting results across cortisol studies. Additional measures across the day in the current sample would have allowed the comparison of diurnal patterns of cortisol levels in the two study groups. The meta-analysis by Miller et al. (2007) found a flatter diurnal pattern of cortisol level in individuals exposed to chronic stress compared to those without chronic stress, an issue only touched upon in the child disaster literature (Goenjian et al. 1996; Pfeffer et al. 2007). In addition, early and longitudinal assessment of this sample would have allowed the plotting of a trajectory of the participants’ responses over time.
It remains unclear if changes in HPA axis functioning create a risk for, constitute a marker of, or reflect the consequences of adverse trauma reactions (Saltzman et al. 2005). Moreover, natural disasters disproportionately affect poor and disadvantaged communities (Cutter and Finch 2008) where vulnerable children and families are likely to reside. Thus, both psychological and biological reactions recorded in the aftermath of an event may reflect pre-disaster social conditions, including chronic stress and an accumulation of adversities, rather than the disaster itself. The literature supports the role of pre-existing conditions, other trauma, and stressful life events in psychological outcomes of disaster exposure in youth (Masten and Narayan 2012; Silverman and La Greca 2002). Disentangling biological stress reactions from these social conditions is a challenging task virtually impossible to achieve with cross-sectional research. Future research using longitudinal design to investigate changes in HPA axis functioning that may occur in disaster-exposed youth may be able to address cause-and-effect relationships. Studies of biological responses to trauma might also explore whether trauma-related HPA axis changes have an adaptive role.
Conclusions
A major incremental contribution of this pilot study is to emphasize the potential role of depression and externalizing problems in HPA axis functioning in an adolescent disaster sample 21 months post event. In this sample, neither disaster exposure nor PTSD symptoms accounted for low basal cortisol when depression and behavior problems were considered, underscoring the importance of a comprehensive assessment in understanding the factors that influence HPA axis functioning. Thus, longitudinal research is needed using representative samples large enough to control for multiple influences—including age, gender, time since disaster exposure, cumulative stressors, and various emotional reactions—to fully elucidate the effects of trauma on HPA axis functioning in youth exposed to disasters and to clarify the importance of HPA axis dysregulation in the long-term mental health of disaster-exposed youth.
References
Achenbach, T. M. (2001). YSR profile for boys & girls—Syndrome scales. [Measurement instrument, Achenbach System of Empirically Based Assessment (ASEBA)]. Burlington: University of Vermont, Research Center for Children, Youth, & Families.
Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, & Families.
Alink, L. R. A., van Ijzendoorn, M. H., Bakermans-Kranenburg, M. J., Mesman, J., Juffer, F., & Koot, H. M. (2007). Cortisol and externalizing behavior in children and adolescents: Mixed meta-analytic evidence for the inverse relation of basal cortisol and cortisol reactivity with externalizing behavior. Developmental Psychobiology, 50(5), 427–450. doi:10.1002/dev.20300.
Badanes, L. S., Watamura, S. E., & Hankin, B. L. (2011). Hypocortisolism as a potential marker of allostatic load in children: Associations with family risk and internalizing disorders. Development and Psychopathology, 23(3), 881–896. doi:10.1017/S095457941100037X.
Bevans, K., Cerbone, A., & Overstreet, S. (2008). Relations between recurrent trauma exposure and recent life stress and salivary cortisol among children. Development and Psychopatholology, 20(1), 257–272. doi:10.1017/S0954579408000126.
Bevans, K., Cerbone, A. B., & Overstreet, S. (2009). The interactive effects of elevated mid-afternoon cortisol and trauma history on PTSD symptoms in children: A preliminary study. Psychoneuroendocrinology, 34(10), 1582–1585. doi:10.1016/j.psyneuen.2009.04.010.
Blaze, J. T., & Shwalb, D. W. (2009). Resource loss and relocation: A follow-up study of adolescents two years after Hurricane Katrina. Psychological Trauma: Theory, Research, Practice, and Policy, 1(4), 312–322. doi:10.1037/a0017834.
Cutter, S. L., & Finch, C. (2008). Temporal and spatial changes in social vulnerability to natural hazards. Proceedings of the National Academy of Sciences, 105(7), 2301–2306. doi:10.1073/pnas.0710375105.
De Bellis, M. D. (2001). Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology, 13(3), 539–564. doi:10.1017/s0954579401003078.
De Bellis, M. D., & Zisk, A. (2014). The biological effects of childhood trauma. Child and Adolescent Psychiatric Clinics of North America, 23(2), 185–222. doi:10.1016/j.chc.2014.01.002.
de Kloet, C. S., Vermetten, E., Geuze, E., Kavelaars, A., Heijnen, C. J., & Westenberg, H. G. M. (2006). Assessment of HPA-axis function in posttraumatic stress disorder: Pharmacological and non-pharmacological challenge tests, a review. Journal of Psychiatric Research, 40(6), 550–567. doi:10.1016/j.jpsychires.2005.08.002.
Del Giudice, M., Ellis, B. J., & Shirtcliff, E. A. (2011). The Adaptive Calibration Model of stress responsivity. Neuroscience and Biobehavioral Reviews, 35(7), 1562–1592. doi:10.1016/j.neubiorev.2010.11.007.
DeSantis, A. S., Adam, E. K., Doane, L. D., Mineka, S., Zinbarg, R. E., & Craske, M. G. (2007). Racial/ethnic differences in cortisol diurnal rhythms in a community sample of adolescents. Journal of Adolescent Health, 41(1), 3–13. doi:10.1016/j.jadohealth.2007.03.006.
Doom, J. R., Cicchetti, D., & Rogosch, F. A. (2014). Longitudinal patterns of cortisol regulation differ in maltreated and nonmaltreated children. Journal of the American Academy of Child and Adolescent Psychiatry, 53(11), 1206–1215. doi:10.1016/j.jaac.2014.08.006.
Dulin-Keita, A., Casazza, K., Fernandez, J. R., Goran, M. I., & Gower, B. (2012). Do neighbourhoods matter? Neighbourhood disorder and long-term trends in serum cortisol levels. Journal of Epidemiology and Community Health, 66(1), 24–29. doi:10.1136/jech.2009.092676.
Fairchild, G., van Goozen, S. H. M., Stollery, S. J., Brown, J., Gardiner, J., Herbert, J., & Goodyer, I. M. (2008). Cortisol diurnal rhythm and stress reactivity in male adolescents with early-onset or adolescence-onset conduct disorder. Biological Psychiatry, 64(7), 599–606. doi:10.1016/j.biopsych.2008.05.022.
Fligner, M. A., & Policello, G. E, I. I. (1981). Robust rank procedures for the Behrens-Fisher problem. Journal of the American Statistical Association, 76(373), 162–168. doi:10.2307/2287062.
Fritz, C. O., Morris, P. E., & Richler, J. J. (2012). Effect size estimates: current use, calculations, and interpretation. Journal of Experimental Psychology: General, 141(1), 2–18. doi:10.1037/a0024338.
Goenjian, A. K., Pynoos, R. S., Steinberg, A. M., Endres, D., Abraham, K., Geffner, M. E., & Fairbanks, L. A. (2003). Hypothalamic-pituitary-adrenal activity among Armenian adolescents with PTSD symptoms. Journal of Traumatic Stress, 16(4), 319–323. doi:10.1023/A:1024453632458.
Goenjian, A. K., Pynoos, R. S., Steinberg, A. M., Najarian, L. M., Asarnow, J. R., Karayan, I., et al. (1995). Psychiatric comorbidity in children after the 1988 earthquake in Armenia. Journal of the American Academy of Child and Adolescent Psychiatry, 34(9), 1174–1184. doi:10.1097/00004583-199509000-00015.
Goenjian, A. K., Yehuda, R., Pynoos, R. S., Steinberg, A. M., Tashjian, M., Yang, R. K., et al. (1996). Basal cortisol, dexamethasone suppression of cortisol, and MHPG in adolescents after the 1988 earthquake in Armenia. American Journal of Psychiatry, 153(7), 929–934.
Gunnar, M. R., & Vazquez, D. M. (2001). Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Development and Psychopathology, 13(3), 515–538. doi:10.1017/s0954579401003066.
Heim, C., Ehlert, U., & Hellhammer, D. H. (2000). The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology, 25(1), 1–35. doi:10.1016/S0306-4530(99)00035-9.
Klimes-Dougan, B., Hastings, P. D., Granger, D. A., Usher, B. A., & Zahn-Waxler, C. (2001). Adrenocortical activity in at-risk and normally developing adolescents: Individual differences in salivary cortisol basal levels, diurnal variation, and responses to social challenges. Development and Psychopathology, 13(3), 695–719. doi:10.1017/s0954579401003157.
Kovacs, M. (1985). The Children’s Depression Inventory (CDI). Psychopharmacology Bulletin, 21(4), 995–998. doi:10.1037/t00788-000.
Kovacs, M. (1992). The Children’s Depression Inventory (CDI) manual. North Tonawanda: Multi-Health Systems.
Lipschitz, D. S., Rasmusson, A. M., Yehuda, R., Wang, S., Anyan, W., Gueoguieva, R., et al. (2003). Salivary cortisol responses to dexamethasone in adolescents with posttraumatic stress disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 42(11), 1310–1317. doi:10.1097/01.chi.0000084832.67701.0d.
Lonigan, C. J., Shannon, M. P., Taylor, C. M., Finch, A. J, Jr, & Sallee, F. R. (1994). Children exposed to disaster: II. Risk factors for the development of post-traumatic symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry, 33(1), 94–105. doi:10.1097/00004583-199401000-00013.
Lopez-Duran, N. L., Kovacs, M., & George, C. J. (2009). Hypothalamic–pituitary–adrenal axis dysregulation in depressed children and adolescents: A meta-analysis. Psychoneuroendocrinology, 34(9), 1272–1283. doi:10.1016/j.psyneuen.2009.03.016.
Marsee, M. A. (2008). Reactive aggression and posttraumatic stress in adolescents affected by Hurricane Katrina. Journal of Clinical Child & Adolescent Psychology, 37(3), 519–529. doi:10.1080/15374410802148152.
Masten, A. S., & Narayan, A. J. (2012). Child development in the context of disaster, war, and terrorism: Pathways of risk and resilience. Annual Review of Psychology, 63, 227–257. doi:10.1146/annurev-psych-120710-100356.
McBurnett, K., Lahey, B. B., Rathouz, P. J., & Loeber, R. (2000). Low salivary cortisol and persistent aggression in boys referred for disruptive behavior. Archives of General Psychiatry, 57(1), 38–43. doi:10.1001/archpsyc.57.1.38.
Miller, G. E., Chen, E., & Zhou, E. S. (2007). If it goes up, must it come down? Chronic stress and the hypothalamic–pituitary–adrenocortical axis in humans. Psychological Bulletin, 133(1), 25–45. doi:10.1037/0033-2909.133.1.25.
Milne, G. (1977). Cyclone tracy: II. The effects on Darwin children. Australian Psychologist, 12(1), 55–62. doi:10.1080/00050067708255860.
Nader, K., & Weems, C. F. (2011). Understanding and assessing cortisol levels in children and adolescents. Journal of Child & Adolescent Trauma, 4(4), 318–338. doi:10.1080/19361521.2011.624059.
Pajer, K., Gardner, W., Rubin, R. T., Perel, J., & Neal, S. (2001). Decreased cortisol levels in adolescent girls with conduct disorder. Archives of General Psychiatry, 58(3), 297–302. doi:10.1001/archpsyc.58.3.297.
Pfeffer, C. R., Altemus, M., Heo, M., & Jiang, H. (2007). Salivary cortisol and psychopathology in children bereaved by the September 11, 2001 terror attacks. Biological Psychiatry, 61(8), 957–965. doi:10.1016/j.biopsych.2006.07.037.
Russoniello, C. V., Skalko, T. K., O’Brien, K., McGhee, S. A., Bingham-Alexander, D., & Beatley, J. (2002). Childhood posttraumatic stress disorder and efforts to cope after Hurricane Floyd. Behavioral Medicine, 28(2), 61–71. doi:10.1080/08964280209596399.
Ruttle, P. L., Shirtcliff, E. A., Serbin, L. A., Fisher, D. B., Stack, D. M., & Schwartzman, A. E. (2011). Disentangling psychobiological mechanisms underlying internalizing and externalizing behaviors in youth: Longitudinal and concurrent associations with cortisol. Hormones and Behavior, 59(1), 123–132. doi:10.1016/j.yhbeh.2010.10.015.
Saltzman, K. M., Holden, G. W., & Holahan, C. J. (2005). The psychobiology of children exposed to marital violence. Journal of Clinical Child and Adolescent Psychology, 34(1), 129–139. doi:10.1207/s15374424jccp3401_12.
Schneider, G., Chicken, E., & Becvarik, R. (2013). NSM3: An R package to accompany Hollander, Wolfe, and Chicken—Nonparametric statistical methods (3rd ed., R package version 1.1). Retrieved from http://cran.r-project.org/web/packages/NSM3/index.html
Shaw, J. A., Applegate, B., Tanner, S., Perez, D., Rothe, E., Campo-Bowen, A. E., & Lahey, B. L. (1995). Psychological effects of Hurricane Andrew on an elementary school population. Journal of the American Academy of Child and Adolescent Psychiatry, 34(9), 1185–1192. doi:10.1097/00004583-199509000-00016.
Shirtcliff, E. A., & Essex, M. J. (2008). Concurrent and longitudinal associations of basal and diurnal cortisol with mental health symptoms in early adolescence. Developmental Psychobiology, 50(7), 690–703. doi:10.1002/dev.20336.
Shirtcliff, E. A., Granger, D. A., Booth, A., & Johnson, D. (2005). Low salivary cortisol levels and externalizing behavior problems in youth. Development and Psychopathology, 17(1), 167–184. doi:10.1017/s0954579405050091.
Silverman, W. K., & La Greca, A. M. (2002). Children experiencing disasters: Definitions, reactions, and predictors of outcomes. In A. M. La Greca, W. K. Silverman, E. M. Vernberg, & M. C. Roberts (Eds.), Helping children cope with disasters and terrorism (pp. 11–33). Washington, DC: American Psychological Association. doi:10.1037/10454-001.
Steinberg, A. M., Brymer, M. J., Decker, K. B., & Pynoos, R. S. (2004). The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports, 6(2), 96–100. doi:10.1007/s11920-004-0048-2.
Stuber, J., Galea, S., Pfefferbaum, B., Vandivere, S., Moore, K., & Fairbrother, G. (2005). Behavior problems in New York City’s children after the September 11, 2001, terrorist attacks. American Journal of Orthopsychiatry, 75(2), 190–200. doi:10.1037/0002-9432.75.2.190.
Susman, E. J. (2006). Psychobiology of persistent antisocial behavior: Stress, early vulnerabilities, and attenuation hypothesis. Neuroscience and Biobehavioral Reviews, 30(3), 376–389. doi:10.1016/j.neubiorev.2005.08.002.
van Bokhoven, I., Van Goozen, S. H. M., van Engeland, H., Schaal, B., Arseneault, L., Séguin, J. R., et al. (2005). Salivary cortisol and aggression in a population-based longitudinal study of adolescent males. Journal of Neural Transmission, 112(8), 1083–1096. doi:10.1007/s00702-004-0253-5.
Vigil, J. M., Carle, A. C., Geary, D. C., Granger, D. A., Flinn, M. V., & Pendleton, P. (2009). Maternal correlates of children’s stress functioning following a major natural disaster. Journal of Child & Adolescent Trauma, 2(4), 287–296. doi:10.1007/s00702-004-0253-5.
Vigil, J. M., Granger, D. A., Geary, D. C., & Flinn, M. V. (2010). Sex differences in salivary cortisol, alpha-amylase, and psychological functioning following Hurricane Katrina. Child Development, 81(4), 1228–1240. doi:10.1111/j.1467-8624.2010.01464.x.
Weems, C. F., & Carrión, V. G. (2007). The association between PTSD symptoms and salivary cortisol in youth: The role of time since the trauma. Journal of Traumatic Stress, 20(5), 903–907. doi:10.1002/jts.20251.
Weems, C. F., & Carrión, V. G. (2009). Brief report: Diurnal salivary cortisol in youth—clarifying the nature of posttraumatic stress dysregulation. Journal of Pediatric Psychology, 34(4), 389–395. doi:10.1093/jpepsy/jsn087.
Yehuda, R. (2001). Biology of posttraumatic stress disorder. Journal of Clinical Psychiatry, 62(Suppl 17), 41–46.
Acknowledgments
Support for this research was provided, in part, by the Oklahoma Center for the Advancement of Science and Technology.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Points of view in this document are those of the authors and do not necessarily represent the official position of the University of Oklahoma Health Sciences Center or the Oklahoma Center for the Advancement of Science and Technology.
Rights and permissions
About this article
Cite this article
Pfefferbaum, B., Tucker, P. & Nitiéma, P. Adolescent Survivors of Hurricane Katrina: A Pilot Study of Hypothalamic–Pituitary–Adrenal Axis Functioning. Child Youth Care Forum 44, 527–547 (2015). https://doi.org/10.1007/s10566-014-9297-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10566-014-9297-3