Abstract
Microbiological contamination of retrieved tissues has become an issue of key importance and is a critical aspect of allograft safety, especially in the case of multi-tissue donations, which frequently become contaminated during retrieval and handling. We analysed contamination in 11,129 tissues with a longitudinal contamination profile for each individual tissue. Specifically, 10,035 musculoskeletal tissues and 1094 cardiovascular tissues were retrieved from a total of 763 multi-tissue donors, of whom 105 heart-beating organ donors and 658 deceased tissue donors. Of the 1955 tissues found to be contaminated after the first decontamination step, 1401 tissues (72%) were contaminated by the same species as the one(s) isolated at retrieval (Time1) and 554 (28%) by different species. Among the 113 tissues testing positive after the 2nd decontamination (Time3), 36 tissues (32%) were contaminated by the same species detected at Timel while the contaminating species differed from Time1 in 77 tissues (68%). The higher the number of contaminating species per tissue the higher the percentage of tissues in which contamination changed over time compared to Time1. The analysis revealed a 28% incidence of new species in tissues already testing positive after retrieval and of 3.5% of tissues becoming positive after admission to the tissue bank. Of these, coagulase-negative Staphylococcus accounted for over 70% of new contaminations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
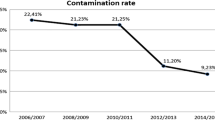
Bacterial contamination is one of the primary problems to be addressed at Tissue Banks (TB) to ensure allograft safety. After retrieval, the contamination rate can be as high as 80% for cardiovascular (CVT) and up to 50% for musculoskeletal tissues (MST) (Paolin et al. 2017a), thus prompting the adoption of stringent decontamination protocols. Decontamination of allografts with antibiotics was first described in 1969 (Barratt-Boyes and Roche 1969), but to date the regimens used by banks differ in terms of antimicrobials used, temperature and duration of treatment. Some protocols have as a result, proven to be less satisfactory than others, despite being validated (Heng et al. 2013). Sterilization is performed using gamma irradiation or ethylene oxide, but high doses of gamma irradiation can alter the biomechanical properties of allografts (Gibbon et al. 1991) and ethylene oxide can cause immune response (Jackson et al. 1990). One study was recently performed to determine the bacterial infections at highest risk of transmission via substances of human origin (Domanović et al. 2017), but few investigations have addressed the origin of contaminating bacteria in allografts. Tissue contaminations are reported to be correlated with donor type, cadaver time, warm ischaemic time, and size of the retrieval team (Van Kats et al. 2010; Paolin et al. 2017b). Among the causes of death, trauma increases the risk of contamination and the likelihood of the contaminants being highly pathogenic bacteria (Deijkers et al. 1997; Paolin et al. 2017b). Among the primary sources of contamination, skin commensals are acknowledged to be the bacteria most frequently isolated in cadaver donor tissues (Martinez et al. 1985). Although the factors contributing to allograft contamination post retrieval are well known, very few papers in the literature consider the appearance of tissue contamination after tissue bank admission. Two papers described cases of negative tissues becoming positive at the following stages of analysis (Jashari et al. 2007; Fan et al. 2012), while another study reported that Microbiology Laboratories (ML), where microbiological cultures are conducted, may be another underestimated source of contamination (Mermel et al. 1994). Said paper presented four cases of contamination from Comamonas Acidovorans in bone tissues tested prior to implantation. These tissues were then found to be false positives and the contamination attributed to the water bath sonicator used at the ML to prepare tissue samples.
We conducted a longitudinal analysis of the bacterial species isolated in microbiological cultures performed, over the course of four years, on 11,129 tissues processed at Treviso Tissue Bank Foundation (FBTV), to collected data of tissues testing positive at more than one control and we observed if these tissues were always contaminated by the same microorganism. Moreover, we examined the types of bacteria detected in tissues found positive after testing negative at the previous microbiological analysis.
Materials and methods
Data collection
Tissues were retrieved, processed and stored by FBTV and bacterial contamination was analyzed in 11,129 consecutive tissues (10,035 MST and 1094 CVT). After obtaining signed informed consent, tissues were retrieved from a total of 763 donors of whom 105 were heart-beating donors (HBD) and therefore also organ donors, and 658 were non-heart-beating donors (NHBD). The tissues were harvested in the operating theatre, by our retrieval team of physicians and technicians, from HBD after organ retrieval and from NHBD within 24 h of cardiac arrest. Prior to tissue retrieval, the skin was surgically scrubbed with chlorhexidine solution, shaved and treated with a second application of chlorhexidine and povidone. Tissues unsuitable for clinical use on account of morphological abnormalities were not included in the analysis nor were tissues collected from donors testing positive for one of the relevant serological markers. After retrieval, the tissues were rinsed in isotonic sterile solution, transferred to antibiotic solution described in the “Decontamination method” section, and transported at + 4 °C.
Decontamination method
The tissues were processed in biohazard class-II laminar airflow cabinets in a class B environment facility as defined according to EU GMP Annex 1. Two decontamination steps were carried out for each tissue: the first immediately after retrieval and the second after processing. The antibiotic cocktail was composed of Ceftazidime 240 μg/ml (Fresenius-Kabi), Lincomycin 120 μg/ml, Polymyxin B 100 μg/ml (Biochrom) and Vancomycin 50 μg/ml (Hospira) in RPMI medium. The decontamination steps were performed at + 4 °C for 24–48 h; tissues testing positive after the second decontamination step were discarded.
Microbiological analysis
Bacteriological examinations for aerobic and anaerobic bacteria and fungi/yeasts were performed three times for each tissue i.e. at the time of retrieval (Time1) and after each of the two decontamination steps (Time2 and Time3) (Fig. 1). Tissues were rinsed with maximum 500 ml isotonic sterile saline after retrieval and after each decontamination step. Samples of the rinsing solution of each tissue were collected (8 ml), without filtering, for microbiological analysis. All procedures were carried out at room temperature. To detect microbial growth, samples were inoculated and incubated in BD BACTEC™ culture vials (BD Becton, Dickinson and Company, New Jersey), according to the manufacturer’s instructions. Samples were then processed under a biohazard class-II laminar flow hood and all bacteria identified using the standard biochemical procedure. Samples were also cultured in a Lowenstein–Jensen medium to isolate mycobacteria. Microbiological cultures and analyses were carried out by an accredited in-hospital ML and interpreted by a microbiologist with specific expertise.
Results
Overall contamination profile of MST and CVT
Table 1 shows the contamination profile of MST and CVT at each time point.
Out of 11,129 analyzed tissues, 6130 were found to be positive at Time1 (55%) while 4999 proved negative (45%). Of the 6130 tissues testing positive at Time1, 113 remained positive across the time points (Group 1), 1842 (Group 2) proved negative after the second decontamination, and 4175 (Group 3) tested negative after the first decontamination. Out of 4999 tissues found negative at Time1, 4607 remained negative across the time points examined (Group 4), 381 became positive at Time2 only (Group 5), 4 tissues tested positive at Time2 and Time3 (Group 6), and 7 tissues proved positive at Time3 only (Group 7).
Longitudinal profile of bacteria in tissues contaminated at Time1
Table 2 shows the trend and type of contaminations in tissues testing positive at Time1.
Out of the 6130 tissues contaminated at Time1, 5207 were contaminated by a single species (85%), 741 by 2 species (12%), 182 by more than 2 species (3%).
Out of 1955 tissues found to be contaminated at Time2, 1401 (72%) were contaminated by the same species while the contaminating species in 554 tissues (28%) differed from Time1. Out of 113 tissues found positive at Time3, 36 tissues (32%) were contaminated by the same species detected at Time1 while the contaminating species in 77 tissues (68%) differed from Time1. The higher the number of contaminating species per tissue the higher the percentage of tissues in which contamination changed over time compared to Time1, as demonstrated in Table 2. In fact, tissues contaminated by more than one species at Time1, were found to be contaminated by different species at higher rate at the following stages of analysis. Table 3 details the longitudinal change in contamination at Time2 and Time3 of tissues testing positive at Time1. In MST, the same contaminants were isolated at both Time2 and Time3 in 1151 out of 1540 tissues (75% of the total), with no significant difference between HBD and NHBD. In CVT, the percentage of the same contaminants fell instead to 38%, with only 200 out of a total of 528 CVT being contaminated by the same species at both Time2 and Time3.
Species detected in tissues previously testing negative
Tables 4, 5 and 6 report the culture results for the tissues of Groups 5, 6, 7 respectively.
In Group 5, NHBD tissues were significantly more contaminated than HBD tissues and the most commonly isolated species were Gram-positive. Tissues were mainly contaminated by skin commensals (coagulase-negative Staphylococcus [CNS], Micrococcus luteus,), followed by species of the respiratory tract (Streptococcus mitis, Streptococcus spp, Staphylococcus aureus), air (Bacillus spp, Bacillus licheniformis), and gastrointestinal tract (Peptostreptococcus spp, Peptostreptococcus anerobius, Enterococcus spp, Clostridium spp). (Table 4)
Tissues belonging to Groups 6 and 7 were contaminated by Gram-positive species, retrieved almost entirely from NHBD. The bacterial species detected were skin commensals (CNS), respiratory and gastrointestinal tract contaminants (Granulicatella adiacens, Clostridium sordelli), and sporogenous bacteria (Tables 5, 6).
Discussion
Retrospective analysis of our tissue cohort clearly revealed that the species contaminating the individual tissues were not always the same in cases remaining positive across various time points, and that several tissues testing negative at Time1 or after decontamination became positive at later controls. Among the tissues testing positive at Time1 and remaining positive at later controls (Groups 1 and 2), the isolated species were, in the majority of cases, the same at the various time points, above all in tissues contaminated by a single microorganism. This was most evident in MST, while the microbiological profile varied more widely at the different time points in tissues contaminated by more than one species, particularly in CVT from NHBD, as detailed in Table 3. Of the 392 tissues that became positive after Time1 (Groups 5, 6 and 7), only 4 (Group 6) were positive at two later steps. An analysis of Time1 data and a discussion of the possible causes of tissue contamination at the time of retrieval have been provided in a previous work (Paolin et al. 2017a). The present study aims instead to highlight the variability of the flora isolated from tissues remaining positive at the various time points, and moreover, the presence of several tissues with an initial negative outcome became positive later. Findings indicate that the contaminations isolated at Time1 (Paolin et al. 2017b) and in previously uncontaminated tissues (Groups 5, 6 and 7) were due almost exclusively to Gram-positive microorganisms. CNS accounted for over 70% of these contaminations, in line with the previous literature on tissue contamination (Veen et al. 1994; Deijkers et al. 1997; Vehmeyer et al. 2002; Ibrahim et al. 2004; Tabaku et al. 2004; Ireland and Spelman 2005; Atique and Khalil 2014). The remaining contaminations were from microorganisms colonising the gastrointestinal and respiratory tracts, and the humid environment. More contaminations were found in NHBD and in CVT (Van Kats et al. 2010; Martinez et al. 1985; Koneman and Davis 1974; Ireland and Spelman 2005). Only a few comparable studies have been described in the literature. Jashari and colleagues, for example, reported the appearance of contamination in some initially sterile allografts. The contaminants were again skin commensals (CNS, Propionibacterium acnes), soil microorganisms (Arthrobacter), Gram-positive cocci, i.e. moderately aerobic, pleomorphic and, in some instances, moderately anaerobic microbes (Jashari et al. 2007). Fan and colleagues reported that the microorganism most frequently isolated in a cohort of cardiovascular tissues uncontaminated at the start of processing but positive after decontamination, was the skin commensal Propionibacterium acnes (Fan et al. 2012). This prompts the question of which factors contribute to new contamination of tissues after bank admission. Potential sources of contamination include TB and ML at which tissues are repeatedly handled during processing, sampling and assaying. The first decontamination did not effectively eradicate the pathogens in the tissues in our sample considering that one-third of them were still positive at Time2. However, 28% of these tissues were contaminated by pathogens not present at Time1 and this finding was more marked in CVT. Conversely, Group 5 and 6 tissues became positive after the first decontamination and those belonging to Group 7 after the second. Contamination can be analysed on the basis of what is known about the origins and transmission routes of bacteria and fungi. By combining this with our knowledge of hygiene and handling at the TB and ML, we can then focus on specific patterns with a view to improving procedures and thus the quality and safety of tissues for recipients. When tissues are admitted to a TB they enter a highly sterile environment with a separate clean room, a sterile cabinet equipped with downflow, filters, screens and air barriers; staff are dressed in sterile clothing to unpack, inspect and process tissues without interruption and in the absence of other people and movement. Continuous controls are made during and after tissue processing. During the year several microbiological controls of the laboratory and operators are carried out, specifically in one year we perform more than 6000 analysis including active air tests, contact plates, settle plate in process, gloves and clothing. The results reveal that less than 0.2% controls are positive and the Staphylococcus species are the most frequent contaminants. Therefore the isolation of air species and skin commensals in tissues can be related to the TB laboratory and operators but a strict correlation cannot be stated. To determine the origin of contamination, more needs to be known about bacteria and ways to group them by properties and habitats. Bacteria must be divided into gram positive (Gram+) and gram negative (Gram−) based on their Gram-staining response. This tells us about their origins: Gram+ have a thick cell wall resistant to dryness and exist on the skin; Gram- have a thin lipid layer with pores that need humidity and colonise the gastrointestinal tract and humid environments. It is helpful to identify bacterial spore formers (Gram+ Clostridia and Bacillus) because spores are highly resistant to dryness, antibiotics and chemical substances and travel rapidly through air. The skin is dry, acidic, cool and derived from nutrients, making it an inhospitable environment for most bacteria, except its own colonisation with Gram+ bacteria, which varies greatly by skin site (Wilson 2005). By far the greatest cause of contamination at the TB is by Staphylococci, but not Staphylococcus aureus. Other common skin bacteria are Corynebacteria and Propionibacteria, but little contamination tends to be encountered from these because they grow slowly or are anaerobic, and need specific culture techniques for longer periods which most labs do not practice (Van Kats et al. 2010). Streptococci along with CNS, Micrococcus luteus, and Bacillus spp are the most common contaminants in MST retrieved from NHBD, which were almost the only tissues contaminated in Group 5. Streptococci can also originate from people talking and coughing, which ought not to affect TBs since staff perform all work wearing a mouth mask and in a safety cabinet with a hood and downflow. One possible source could be microbiology technicians, who do not wear mouth masks or, in many cases, gloves, and work on open workbenches. Air contains mainly spores and cocci. Much contamination from dust and the spores of spore-forming microbes as Bacillus spp can be found at hospital laboratories located in or near to building sites (Barrie et al. 1992; Whyte et al. 1982). Clostridium is a spore-forming bacteria with many species and a commensal of the intestinal tract. If Clostridium is isolated despite retrieval having been performed without perforation, within 12–24 h post mortem, and in the absence of donor bacteraemia, then the Clostridium spores must originate from an exogenous source, such as ML environment.
Another possible explanation for the microbiological variability in our cohort over time is the low sensitivity and/or specificity of the culture method for some pathogens. Plausibly, therefore, some species are not isolated due either to longer growth times than the ones routinely used for incubation, or to the presence of antibiotic cocktail residues. In both cases, however, this would cause an increase in false negatives rather than false positives. Furthermore, we validated the microbiological analysis method before using it in practice. Lastly, the majority of microorganisms identified in allografts are skin commensals (Martinez et al. 1985; Veen et al. 1994; Deijkers et al. 1997; Vehmeyer et al. 2002; Ibrahim et al. 2004; Tabaku et al. 2004; Ireland and Spelman 2005; Atique and Khalil 2014), which can be easily identified by our culture methods, even at low loads.
Conclusions
Despite the application of stringent procedures, particularly during tissue processing in classified environments, additional contaminations by new species and contamination of sterile tissues are not a rare occurrence. Moreover, many potential additional contaminations can be associated with later tissue handling in other, less protected environments. These observations should prompt all workers involved to adopt even more rigorous safety indicators with a view to drastically reducing the final number of positive samples and therefore of discarded tissues. Finding positive tissues at the end of processing and after antibiotic decontamination is not, however, an infrequent outcome in many TBs and can in some cases result in a high percentage of tissues being discarded, particularly CVTs.
References
Atique FB, Khalil MM (2014) The bacterial contamination of allogeneic bone and emergence of multidrug-resistant bacteria in tissue bank. Biomed Res Int 2014:430581
Barratt-Boyes BG, Roche AH (1969) A review of aortic valve homografts over a six and one-half year period. Ann Surg 170(3):483–492
Barrie D, Wilson JA, Hoffman PN, Kramer JM (1992) Bacillus cereus meningitis in two neurosurgical patients: an investigation into the source of the organism. J Infect 25(3):291–297
Deijkers RL, Bloem RM, Petit PL, Brand R, Vehmeyer SB, Veen MR (1997) Contamination of bone allografts: analysis of incidence and predisposing factors. J Bone Joint Surg Br 79(1):161–166
Domanović D, Cassini A, Bekeredjian-Ding I, Bokhorst A, Bouwknegt M, Facco G, Galea G, Grossi P, Jashari R, Jungbauer C, Marcelis J, Raluca-Siska I, Andersson-Vonrosen I, Suk JE (2017) Prioritizing of bacterial infections transmitted through substances of human origin in Europe. Transfusion 57(5):1311–1317
Fan YD, Van Hoeck B, Holovska V, Jashari R (2012) Evaluation of decontamination process of heart valve and artery tissues in European Homograft Bank (EHB): a retrospective study of 1,055 cases. Cell Tissue Bank 13(2):297–304
Gibbons MJ, Butler DL, Grood ES, Bylski-Austrow DI, Levy MS, Noyes FR (1991) Effects of gamma irradiation on the initial mechanical and material properties of goat bone-patellar tendon-bone allografts. J Orthop Res 9(2):209–218
Heng WL, Albrecht H, Chiappini P, Lim YP, Manning L (2013) International heart valve bank survey: a review of processing practices and activity outcomes. J Transpl 2013:163150
Ibrahim T, Stafford H, Esler CN, Power RA (2004) Cadaveric allograft microbiology. Int Orthop 28(5):315–318
Ireland L, Spelman D (2005) Bacterial contamination of tissue allografts-experiences of the donor tissue bank of Victoria. Cell Tissue Bank 6(3):181–189
Jackson DW, Windler GE, Simon TM (1990) Intraarticular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med 18(1):1–10
Jashari R, Tabaku M, Van Hoeck B, Cochéz C, Callant M, Vanderkelen A (2007) Decontamination of heart valve and arterial allografts in the European Homograft Bank (EHB): comparison of two different antibiotic cocktails in low temperature conditions. Cell Tissue Bank 8(4):247–255
Koneman EW, Davis MA (1974) Postmortem bacteriology. 3. Clinical significance of microorganisms recovered at autopsy. Am J Clin Pathol 61(1):28–40
Martinez OV, Malinin TI, Valla PH, Flores A (1985) Postmortem bacteriology of cadaver tissue donors: an evaluation of blood cultures as an index of tissue sterility. Diagn Microbiol Infect Dis 3(3):193–200
Mermel LA, Josephson SL, Giorgio C (1994) A pseudoepidemic involving bone allografts. Infect Control Hosp Epidemiol 15(12):757–758
Paolin A, Trojan D, Petit P, Coato P, Rigoli R (2017a) Evaluation of allograft contamination and decontamination at the Treviso Tissue Bank Foundation: a retrospective study of 11,129 tissues. PLoS ONE 12(3):e0173154
Paolin A, Romualdi C, Romagnoli L, Trojan D (2017b) Analysis of potential factors affecting allografts contamination at retrieval. Cell Tissue Bank 18(4):539–545
Tabaku M, Jashari R, Carton HF, Du Verger A, Van Hoeck B, Vanderkelen A (2004) Processing of cardiovascular allografts: effectiveness of European Homograft Bank (EHB) antimicrobial treatment (cool decontamination protocol with low concentration of antibiotics). Cell Tissue Bank 5(4):261–266
Van Kats JP, van Tricht C, van Dijk A, van der Schans M, van den Bogaerdt A, Petit PL, Bogers AJ (2010) Microbiological examination of donated human cardiac tissue in heart valve banking. Eur J Cardiothorac Surg 37(1):163–169
Veen MR, Bloem RM, Petit PL (1994) Sensitivity and negative predictive value of swab cultures in musculoskeletal allograft procurement. Clin Orthop Relat Res 300:259–263
Vehmeyer S, Wolkenfelt J, Deijkers R, Petit P, Brand R, Bloem R (2002) Bacterial contamination in postmortem bone donors. Acta Orthop Scand 73(6):678–683
Whyte W, Hodgson R, Tinkler J (1982) The importance of airborne bacterial contamination of wounds. J Hosp Infect 3(2):123–135
Wilson M (2005) Microbial inhabitants of humans. Cambridge University Press, Cambridge
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors. The nature of the survey exempted it from ethics committee review: i.e. the analysis was performed on tissue rinsing solutions collected after the two decontamination steps.
Rights and permissions
About this article
Cite this article
Paolin, A., Montagner, G., Petit, P. et al. Contamination profile in allografts retrieved from multitissue donors: longitudinal analysis. Cell Tissue Bank 19, 809–817 (2018). https://doi.org/10.1007/s10561-018-9739-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-018-9739-5