Abstract
Autologous chondrocyte implantation (ACI) and osteochondral autograft transplantation (OAT or mosaicplasty) are two effective surgeries for the treatment of large cartilage defects for more than two decades. But there are always some controversies about which one has the better outcomes for the patients. The purpose of this meta-analysis is to compare the outcomes of these two surgeries and give an advice to the clinical practices. The literature search was performed on multiple electronic databases with specific included criteria. After the assessments, five Randomized controlled trials (level II) were included and two of them were in the same cohort. The continuous data of outcomes were categorized into ranked ones (excellent, good, fair and poor) for comparisons. In the six comparisons of excellent or good results and poor results, the outcomes of ACI were significantly better than OAT in only one comparison (RR 2.57, 95 % CI 1.09–6.07, P = 0.03) while others had no significant differences. We may reach a primary conclusion that there is no significant different outcome between ACI and OAT in a short-term follow-up but it may indicate that the patients with OAT may be more likely to have worse condition than that with ACI for a long-term period.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Articular hyaline cartilage is an avascular tissue which covers the surface of the bone in a joint for low-friction motion and weight-bearing capacity. It is usually less than 3 mm and likely to suffer from trauma or degeneration (Smith et al. 2005; Chiang and Jiang 2009). The joints with cartilage defects usually have the symptoms of pain, articular effusion and crepitus that are hard to relief. For the lack of access to abundant nutrients or circulating progenitor cells, articular cartilage has a poor self-repair capacity after injury and these defects are easy to progress into osteoarthritis with pain and instability (Huey et al. 2012). Thus the cartilage defects often require surgical intervention for a better function.
The surgical interventions in knee can be classified as reparative and reconstructive surgeries. The reparative surgery includes microfracture, drilling and abrasion arthropasty and the reconstructive surgery comprises allograft transplantation, osteochondral autograft transplantation (OAT) and autologous chondrocyte implantation (ACI) (Stroh et al. 2011). According to the results of clinical trials and review articles, reparative surgery is more effective on the smaller defects (<100 mm2) than reconstructive surgery while in large defects (>100 mm2), reconstructive surgery performs better (Perera et al. 2012; Smith et al. 2005). Osteochondral autograft transplantation and autologous chondrocyte implantation are two popular methods in the treatment of large cartilage defects.
Osteochondral autograft transplantation, also known as osteochondral cylinder transplantation or mosaicplasty, is a technique that was described in 1990s (Matsusue et al. 1993; Hangody and Karpati 1994). It uses the osteochondral grafts taken from lighter-load-bearing areas of patient’s own joint to fill the focal defects (Hangody et al. 1998). Autologous chondrocyte implantation is put forward in the same period (Brittberg et al. 1994) but it is a totally different technique from osteochondral autograft transplantation. It needs to get the chondrocytes from the patient’s joint and expand them in vitro for the reimplantation (Chilelli et al. 2014). However, for the treatment of large cartilage defects, it still remains controversial that which method has better outcomes. So this meta-analysis mainly aimed to compare the efficacy of osteochondral autograft transplantation with autologous chondrocyte implantation in the treatment of large cartilage defects of knee.
Materials and methods
Search strategy
The literature search was performed on November 5, 2014 through the electronic databases: PubMed (1966 to November 2014), OVID (1974 to November 2014), The Cochrane Library (Issue 10 of 12, October 2014) and SinoMed (1978 to November 2014). The search terms and Boolean operators used were as follow: [(osteochondral autograft transplantation or osteochondral autologous transplantation or mosaicplasty or osteochondral cylinder transplantation) and (autologous chondrocyte implantation or autologous chondrocyte transplantation or matrix-assisted chondrocyte implantation)]. No language or article type restrictions were included in search strategy. The eligibility criteria are presented in Table 1.
Study selection and data collection
After excluding the duplicates, two reviewers independently screened the titles and abstracts of the initial studies to determine if each article might meet the eligibility criteria. Studies which definitely failed to meet the eligibility criteria were excluded. The rest studies were screened the full text without the authors, institutions, journal of publications and results. The studies which had disagreement in either assessment were screened by the third reviewer to determine whether the studies were included or not.
Each included randomized controlled trials were assessed by two reviewers according the assessment of study quality from randomization, allocation concealment, blinding, drop-out and outcomes. For each eligible study, information was extracted as follows: first author’s name, year and country of publication, study design, follow-up period, setting, mean age and defect size of patients and postoperative functional assessment. We attempted to contact the authors through emails for the data that was not presented on the paper.
Statistical analysis
The extracted information from each study was turned into dichotomous data to describe the postoperative outcomes. The data was expressed as risk ratios (RR) and 95 % confidence intervals (CIs) and was combined by the method of Mantel and Haenszel to test significance and homogeneity. The statistical heterogeneity was evaluated by χ2 test and I2 statistics. The pooled effect was calculated in fixed-effect model when there was no significant heterogeneity (P > 0.10 and I2 < 50 %), or random-effects model was used.
Results
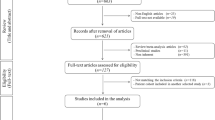
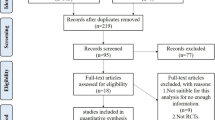
Study selection (Fig. 1)
The initial literature research identified 850 potential relevant studies with 108 duplicates. After the screen of title, abstract and full text according to the eligibility criteria, 5 studies were included: Bentley et al. (2003, 2012), Dozin et al. (2005), Horas et al. (2003), Lim et al. (2012) (Table 2). The Kappa value was 0.828 for the title and abstract screening and 0.876 for the full-text screening. Two reviewers had a controversy on Dozin et al. (2005) which was included after discussion. All the studies were randomized controlled trials with evidence level II (evidence level as declared by the journal in which the study was published). Two studies were in the same cohort with different follow-up periods (Bentley et al. 2003, 2012).
Study characteristics
Bentley et al. (2003) had a total of 100 patients and 96 had osteochondral defects on medial/lateral femoral condyle or patella. The clinical results were graded as excellent (>80), good (55–79), fair (30–54) or poor (<30) by the assessment of modified Cincinatti rating system at 12 months. This study also used arthroscopy to assess the results according to the International Cartilage Research Society (ICRS) grading system in 60 patients. There were no lost in follow-up patients.
Bentley et al. (2012) used the same cohort with Bentley et al. (2003) and 6 patients were lost (5 ACI patients and 1 OAT patient). This study reported the 5-year failure rate (failure was defined as the poor result by the assessment of modified Cincinatti rating system) and 63 patients were taken arthroscope to evaluate the outcomes.
Dozin et al. (2005) was a multicenter trial of 5 orthopedic units with 47 patients registered and 3 quitted. The results were presented on the basis of Lysholm Knee Scoring Scale (LKSS). There was a poor follow-up at 12 months with 18 out of 44 (41 %) so that the outcomes of 37 patients was categorized into four classes: LKSS < 60, LKSS = 69–90, LKSS > 90 and subjective improvement.
Horas et al. (2003) included 40 patients with the lesion on the medial/lateral femoral condyle. Seven of twenty patients with ACI and four of twenty patients with OAT had arthroplasty or spongiolization previously. The postoperative results were presented as enumeration data by Lysholm, Tegner and Meyers scores and ranked data by chief complaint. No participants were lost to follow-up.
Lim et al. (2012) investigated 30 knees with microfracture, 22 with OAT and 18 with ACI which were compared postoperatively by Lysholm score, Tegner score, Hospital for Special Surgery score, modified Outerbridge cartilage grades using MRI and International Cartilage Research Society (ICRS) grading system using arthroscopy. MRI was taken on 36 of 40 (90 %) while arthroscopy was used on 32 of 40 (80 %) and the results was ranked as excellent (1), good (2), fair (3), poor (4).
Meta-analysis
The outcome measurements of these studies were different from each other and there are no satisfied responses from the authors by emails, so we categorized the results into the grades as excellent, good, fair and poor results (Table 3 and Table 4). Four studies (Bentley et al. 2003; Dozin et al. 2005; Horas et al. 2003; Lim et al. 2012) were included first for the comparison of the excellent or good results (Table 3 presented the outcome assessments used in the comparisons) and Fig. 2 showed that the P value was 0.06 and there was no significant overall results. Figure 3 displayed the results that Dozin et al. (2005) was excluded for the poor follow-up and dissatisfied outcome assessments and the total RR was 0.85 with a 95 % confidence interval of (0.73, 1.00). In these two comparisons, neither ACI nor OAT had more satisfied outcomes in about one-year period. Then, we included five studies (Bentley et al. 2003, 2012; Dozin et al. 2005; Horas et al. 2003; Lim et al. 2012) for the comparison of postoperative poor results between these two therapies (Table 4 presented the outcome assessments used in the comparisons). Bentley et al. (2003, 2012) were not used in one comparison for they came from the same cohort with different follow-up periods. Figures 4 and 5 which included Bentley et al. (2003) with/without Dozin et al. (2005) showed no significant results and the P values were 0.12 and 0.19. Lastly, we used Bentley et al. (2012) which had a five-year follow-up to replace Bentley et al. (2003) (1-year follow-up) (Figs. 6, 7) and there was a significant overall effect with Dozin et al. (2005) excluded. In Fig. 7, the overall RR was 2.57 with a 95 % confidence interval of (1.09, 6.07) and it revealed OAT had poorer outcomes than ACI in statistics.
Comparison of excellent or good results (without Dozin et al. 2005)
Comparison of poor results (with Bentley et al. 2003)
Comparison of poor results (with Bentley et al. 2012)
Discussion
OAT and ACI are two effective surgeries for the treatment of large cartilage defects that usually bigger than 100 mm2 (Perera et al. 2012).
In surgical techniques, OAT needs multiple cylindrical autogenous osteochondral plugs which are usually taken from the less weight-bearing joint area as a mosaic to fill the lesions for a resurfaced area. Therefore it is usually used in the defect that is less than 400 mm2 for the limitation of autograft and may have some complications years after the cylindrical cutting devices. It also has some limitations such as the absence of fill among the mosaics and different orientations of the surfaces of plugs (Bedi et al. 2010; Robert 2011; Bekkers et al. 2009). In the arthroscopical and histological results, smooth surface with hyaline or hyaline-like cartilage could be seen in the most of OAT cases but some patients had a circular gap between the transplanted and surrounding resident cartilage (Bentley et al. 2003, Horas et al. 2003).
ACI has a more complicated procedure than OAT since ACI needs at least two operations. Firstly, the joint should be evaluated by arthroscopy to assess the injury. It also needs full-thickness cartilage biopsy for chondrocyte culturing and expansion (Smith et al. 2005). Obviously, the injury of preparation for the surgery is much less than that of OAT but ACI needs more time and higher cost. Because of the chondrocyte culturing, ACI usually used for the defects over 400 mm2 (Bekkers et al. 2009). There are various kinds of technique for implantation, such as periosteum-covered ACI, collagen-covered ACI, matrix-induced ACI and ACI within a 3D scaffold (Harris et al. 2011; Brittberg 2010; Marlovits et al. 2006). In the included studies, three used the surgical techniques of periosteum-covered ACI while the rest two (Bentley et al. 2003, 2012) used ACI covered with porcine collagen membrane or periosteum. In the most cases of ACI, fibrous repair tissues or fibrocartilage and monodirectional collagen bundles were grown with the surfaces rippled or rough and some had overgrown the level of the surrounding cartilage. Only did a few patients have the results with hyaline or hyaline-like cartilage (Horas et al. 2003; Bentley et al. 2003; Roberts et al. 2009; Huey et al. 2012).
In recent years, there have been several systematic reviews discussing the outcomes of these surgeries, but as little researches and high heterogeneity, no powerful conclusion was drawn (Goyal et al. 2014; Bekkers et al. 2009; Vasiliadis and Wasiak 2010). In this meta-analysis, there were five randomized controlled trials about OAT and ACI included with two of them in one cohort and we included one more study than the previous reviews (Bentley et al. 2012). For these five studies, various outcome assessments (Lysholm score, Meyers score, Tegner activity score, Hospital for Special Surgery score, International Knee Documentation Committee Scale, mofied Outerbridge cartilage grades using MRI, International Cartilage Repair Society repair grade using arthroscopy) and statistic data (quantitative data and quantitative data) were used and no available unified criteria and data remained. We attempted to communicate with the authors for the details of data but there were no positive responses. Consequently, we utilized the ranked data extracted from the original articles. Bentley et al. (2003) used the assessments of modified Cincinatti rating system in 100 patients (100 %) and International Cartilage Research Society (ICRS) in 60 patients (60 %). As a result we prefer the former one for the comparison. Same condition was found in Bentley et al. (2012) where 94 patients (94 %) assessed by Cincinatti rating system while only 63 patients (63 %) by ICRS. In Lim et al. (2012), the available outcomes were presented by MRI (36 of 40, 90 %) and arthroscopy (32 of 40, 80 %) but we considered the results of arthroscopy were more precise and credible. Dozin et al. (2005) and Horas et al. (2003) had no more available choices in ranked data for comparison. In the quality assessment of all the studies included, we found that Dozin et al. (2005) was a multicenter trial with different operators and technique, poor follow-up, dissatisfied outcome assessments and smaller mean defect size (192.5 mm2). So we did the meta-analysis without Dozin et al. (2005) to reduce its interference.
The pooled outcomes of each study were graded as excellent, good, fair and poor. In the comparison of the results with the follow-up of 1–2 years, whether good or poor, there was no significant difference between OAT and ACI. However, when we replaced Bentley et al. (2003) with Bentley et al. (2012) which had a longer follow-up, we could see the significant result that OAT was poorer. So in the short-term, we may not distinguish which one has the better outcomes. Both of these two techniques can cover the large cartilage defects and relief the symptom obviously but as time goes on, the disadvantages shows. In OAT, the injuries for autografts, absence of fill and differences in orientation may influence the outcomes in the future and patients can not afford another OAT operation. In contrast of OAT, ACI has huge potential to be renovated into a more effective technique with the development of tissue engineering and can be taken repeatedly on one patient.
In the six comparisons of the excellent or good results and the poor results, we may reach a primary conclusion that there is no significant different outcomes between ACI and OAT in a short-term follow-up but it may indicate that the patients with OAT may be more likely to have worse conditions than that with ACI for a long-term period.
Obviously, there were some limitations in this study. For this meta-analysis, although all the included studies were RCTs, the qualities of them were not satisfied (level II) and these results might have placebo effects. Moreover, the outcome measurements of the studies were different from each other and we had to categorize the quantitative data into crude grades for comparisons. Different selections of patients, operative technique and rehabilitation program might also cause the heterogeneity. The heterogeneity made it difficult to reach a conclusion that was strong enough, so more high-quality randomized controlled trials and other clinical trials are needed urgently with unified criteria, surgical techniques and long-term follow-up.
References
Bedi A, Feeley BT, Williams RR (2010) Management of articular cartilage defects of the knee. J Bone Joint Surg Am 92:994–1009
Bekkers J, Inklaar M, Saris DB (2009) Treatment selection in articular cartilage lesions of the knee: a systematic review. Am J Sports Med 37:148S–155S
Bentley G, Biant LC, Carrington RW, Akmal M, Goldberg A, Williams AM, Skinner JA, Pringle J (2003) A prospective, randomised comparison of autologous chondrocyte implantation versus mosaicplasty for osteochondral defects in the knee. J Bone Joint Surg Br 85-B:223–230
Bentley G, Biant LC, Vijayan S, Macmull S, Skinner JA, Carrington RW (2012) Minimum ten-year results of a prospective randomised study of autologous chondrocyte implantation versus mosaicplasty for symptomatic articular cartilage lesions of the knee. J Bone Joint Surg Br 94-B:504–509
Brittberg M (2010) Cell carriers as the next generation of cell therapy for cartilage repair: a review of the matrix-induced autologous chondrocyte implantation procedure. Am J Sports Med 38:1259–1271
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Chiang H, Jiang C (2009) Repair of articular cartilage defects: review and perspectives. J Formos Med Assoc 108:87–101
Chilelli BJ, Mastrocola MR, Gomoll AH (2014) Autologous chondrocyte implantation: surgical technique and outcomes. Oper Tech Orthop 24:246–252
Dozin B, Malpeli M, Cancedda R, Bruzzi P, Calcagno S, Molfetta L, Priano F, Kon E, Marcacci M (2005) Comparative evaluation of autologous chondrocyte implantation and mosaicplasty: a multicentered randomized clinical trial. Clin J Sport Med 15:220–226
Goyal D, Keyhani S, Goyal A, Lee EH, Hui JHP, Vaziri AS (2014) Evidence-based status of osteochondral cylinder transfer techniques: a systematic review of level I and II studies. Arthroscopy 30:497–505
Hangody L, Karpati Z (1994) New possibilities in the management of severe circumscribed cartilage damage in the knee. Magy Traumatol Ortop Kezseb Plasztikai Seb 37:237–243
Hangody L, Kish G, Karpati Z, Udvarhelyi I, Szigeti I, Bely M (1998) Mosaicplasty for the treatment of articular cartilage defects: application in clinical practice. Orthopedics 21:751–756
Harris JD, Siston RA, Brophy RH, Lattermann C, Carey JL, Flanigan DC (2011) Failures, re-operations, and complications after autologous chondrocyte implantation—a systematic review. Osteoarthr Cartil 19:779–791
Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R (2003) Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint A prospective, comparative trial. J Bone Joint Surg Am 85-A:185–192
Huey DJ, Hu JC, Athanasiou KA (2012) Unlike bone, cartilage regeneration remains elusive. Science 338:917–921
Lim H, Bae J, Song S, Park Y, Kim S (2012) Current treatments of isolated articular cartilage lesions of the knee achieve similar outcomes. Clin Orthop Relat Res 470:2261–2267
Marlovits S, Zeller P, Singer P, Resinger C, Vecsei V (2006) Cartilage repair: generations of autologous chondrocyte transplantation. Eur J Radiol 57:24–31
Matsusue Y, Yamamuro T, Hama H (1993) Arthroscopic multiple osteochondral transplantation to the chondral defect in the knee associated with anterior cruciate ligament disruption. Arthroscopy 9:318–321
Perera JR, Gikas PD, Bentley G (2012) The present state of treatments for articular cartilage defects in the knee. Ann R Coll Surg Engl 94:381–387
Robert H (2011) Chondral repair of the knee joint using mosaicplasty. Orthop Traumatol Surg Res 97:418–429
Roberts S, Menage J, Sandell LJ, Evans EH, Richardson JB (2009) Immunohistochemical study of collagen types I and II and procollagen IIA in human cartilage repair tissue following autologous chondrocyte implantation. Knee 16:398–404
Smith GD, Knutsen G, Richardson JB (2005) A clinical review of cartilage repair techniques. J Bone Joint Surg Br 87:445–449
Stroh A, Johnson A, Mont M (2011) Surgical implants and technologies for cartilage repair and preservation of the knee. Expert Rev Med Devices 8:339–356
Vasiliadis HS, Wasiak J (2010) Autologous chondrocyte implantation for full thickness articular cartilage defects of the knee. Cochrane Database Syst Rev 10:CD003323
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (No. 81472079).
Author information
Authors and Affiliations
Corresponding author
Additional information
Zeng Li and Tianyi Zhu have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Li, Z., Zhu, T. & Fan, W. Osteochondral autograft transplantation or autologous chondrocyte implantation for large cartilage defects of the knee: a meta-analysis. Cell Tissue Bank 17, 59–67 (2016). https://doi.org/10.1007/s10561-015-9515-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10561-015-9515-8