Abstract
Purpose
Pharmacodynamic drug-drug interactions (PD DDIs) may influence the safety of non-vitamin K antagonist oral anticoagulants (NOACs), but the extent to which PD DDIs increase bleeding risks, remains unclear. Therefore, the impact of PD DDIs on bleeding outcomes in NOAC-treated patients with atrial fibrillation (AF) was investigated.
Methods
Using Belgian nationwide data, NOAC-treated AF patients were included between 2013–2019. Concomitant use of PD interacting drugs when initiating NOAC treatment was identified.
Results
Among 193,072 patients, PD DDIs were identified in 114,122 (59.1%) subjects. After multivariable adjustment, concomitant use of PD interacting drugs was associated with significantly higher risks of major or clinically-relevant non-major bleeding (adjusted hazard ratio (aHR) 1.19, 95% confidence interval (CI) (1.13–1.24)), gastrointestinal (aHR 1.12, 95%CI (1.03–1.22)), urogenital (aHR 1.21, 95%CI (1.09–1.35)) and other bleeding (aHR 1.28, 95%CI (1.20–1.36)), compared to NOAC-treated AF patients without PD interacting drug use. Increased bleeding risks were most pronounced with P2Y12 inhibitors (aHR 1.62, 95%CI (1.48–1.77)) and corticosteroids (aHR 1.53, 95%CI (1.42–1.66)), followed by selective serotonin or serotonin and norepinephrine reuptake inhibitors (SSRI/SNRI, aHR 1.26, 95%CI (1.17–1.35)), low-dose aspirin (aHR 1.14, 95%CI (1.08–1.20)) and non-steroidal anti-inflammatory drugs (NSAID, aHR 1.10, 95%CI (1.01–1.21)). Significantly higher intracranial bleeding risks in NOAC users were observed with SSRI/SNRIs (aHR 1.50, 95%CI (1.25–1.81)) and corticosteroids (aHR 1.49, 95%CI (1.21–1.84)).
Conclusion
Concomitant use of PD interacting drugs, especially P2Y12 inhibitors and corticosteroids, was associated with higher major, gastrointestinal, urogenital, and other bleeding risks in NOAC-treated AF patients. Remarkably, higher intracranial bleeding risks were observed with SSRI/SNRIs and corticosteroids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-vitamin K antagonist oral anticoagulants (NOACs) are the preferred option for stroke prevention in patients with atrial fibrillation (AF), given their fixed dosing regimen without the need for INR monitoring, fast onset of action, and lower intracranial bleeding risk than vitamin K antagonists (VKAs) [1, 2]. Several randomized and observational studies have indeed demonstrated that NOACs are effective and safe alternatives to VKAs [3,4,5,6,7,8], albeit not consistently in real-world observational studies [9,10,11]. Compared to VKAs, fewer pharmacokinetic drug-drug interactions (DDIs) have been observed with NOACs [1, 2]. However, as highlighted in the European Heart Rhythm Association (EHRA) Practical Guide on NOAC use in AF patients, pharmacodynamic (PD) DDIs with NOACs may also be relevant, which occur when the pharmacological effect of one drug is altered by that of another drug in a combination regimen [1]. Consequently, careful consideration is required when combining antiplatelets, non-steroidal anti-inflammatory drugs (NSAIDs), systemic corticosteroids, or selective serotonin or serotonin and norepinephrine reuptake inhibitors (SSRI/SNRIs) with NOACs. The benefit of concomitant use should be thoroughly balanced against the risk in each clinical situation, as significantly higher bleeding risks have been reported, especially when combining NOACs and antiplatelets in patients with AF and coronary artery disease (CAD) [12,13,14,15,16,17,18,19,20]. When concomitant use is necessary and other risk factors for bleeding are present (e.g., frailty), a reduced NOAC dose may be considered, as suggested by the EHRA Practical Guide [1], although sufficient randomized data to support this approach are lacking.
However, the extent to which bleeding risks may increase with PD interacting drugs such as NSAIDs, corticosteroids and SSRI/SNRIs in NOAC users is less established. Moreover, previous studies were often limited by small sample sizes, short follow-up durations, limited exposure assessment (e.g., not accounting for the initiation or discontinuation of interacting drugs during follow-up) or investigation of subjects with specific comorbidities (e.g., CAD) or undergoing specific interventions (e.g., percutaneous coronary intervention (PCI)).
Therefore, we aimed to investigate the impact of drugs involved in PD DDIs on bleeding outcomes in NOAC-treated AF patients. Differences between specific PD interacting drug classes and in location-specific bleeding risks were explored.
Methods
Source population
Details on the study methodology have been reported before [7, 21]. In brief, two nationwide databases provided the source population, namely the InterMutualistic Agency (IMA) database and Minimal Hospital Dataset (MHD). The IMA centralizes all claims data from Belgian health insurance funds on reimbursed ambulatory and hospital care, including demographic characteristics (e.g., age, sex), medical procedures and drug prescription claims (e.g., dispensing date, Anatomical Therapeutic Chemical (ATC) classification code, package size…), and represents all legal residents in Belgium [22]. The MHD aggregates hospital discharge diagnoses of every hospital admission (hospitalizations, day-care stays and emergency room contacts), coded in International Classification of Diseases (ICD) codes (ICD-9 up to 2014, ICD-10 from 2015 onwards) [23]. Every case of the study population was identified in both databases. This study was approved by the Belgian Commission for the Protection of Privacy (approval code IVC/KSZG/20/344) [24]. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline was followed (eTable 1) [25].
Study population
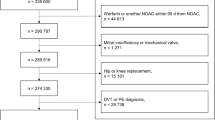
Subjects ≥ 45 years old with ≥ 1 year coverage by Belgian health insurance funds were included on the first date of filling a NOAC prescription (= index date) from 1 January 2013 to 1 January 2019 (eFig. 1). Dabigatran (approved in Belgium since August 2012), rivaroxaban (approved since September 2012), apixaban (approved since September 2013) and edoxaban (approved since October 2016) users were included. Only NOAC-naïve subjects were considered, excluding patients with an oral anticoagulant prescription filled ≤ 1 year before the index date. Subjects were not required to have an ICD-coded hospital discharge diagnosis of AF to be included, as this would create selection bias due to limiting the study population to hospitalized AF subjects and excluding AF subjects treated exclusively in primary or ambulatory care [7, 26].
Persons were also excluded in case of (1) total hip or knee replacement, or diagnosis of deep vein thrombosis or pulmonary embolism ≤ 6 months before the index date, (2) mechanical prosthetic heart valve or moderate/severe mitral stenosis, (3) end-stage renal disease (chronic kidney disease stage V and/or dialysis), (4) ≥ 2 prescription claims of different NOAC types or doses on the index date, or (5) use of NOAC doses not approved for stroke prevention in AF (e.g., rivaroxaban 10 mg) (eTable 2).
Drugs involved in pharmacodynamic drug-drug interactions
As described in the EHRA Practical Guide [1], antiplatelets (including low-dose aspirin ≤ 160 mg daily and P2Y12 inhibitors), systemic NSAIDs (including high-dose aspirin > 160 mg daily), systemic corticosteroids and SSRI/SNRIs were considered as drugs involved in PD interactions with NOACs, and were identified with ATC-coded prescription claims in ambulatory and hospital care up to 6 months before the index date (eTable 3) [1, 12]. Patients were categorized by whether or not a PD interacting drug was concomitantly used at the time of NOAC initiation. Criteria for concomitant use were determined as 1) the interacting drug was concurrently started on the index date, or 2) the treatment period of an interacting drug included the index date (overlapping drug supply), in line with previous research [12, 27,28,29,30,31,32,33,34].
Outcomes
The primary outcome of interest was major or clinically relevant non-major bleeding (MB/CRNMB). Secondary outcomes included major bleeding, CRNMB, intracranial bleeding, gastrointestinal bleeding, urogenital bleeding, and bleeding at other sites (e.g., retroperitoneal). Major bleeding was defined as a bleeding event requiring hospitalization in a critical area or organ (e.g., intracranial), fatal bleeding or bleeding event with a medical procedure code for blood transfusion ≤ 10 days after admission, which is adapted from the International Society on Thrombosis and Haemostasis definition due to a lack of data on haemoglobin levels or number of blood transfusion units [7, 35]. CRNMB was defined as a bleeding event requiring hospitalization that did not classify for major bleeding. Outcomes were identified using ICD-coded hospital discharge diagnoses and medical procedure codes (eTable 4) [21].
Follow-up
Subjects were followed from NOAC initiation until the first occurrence of the investigated outcome, discontinuation (> 60-day gap of drug supply, which accounts for delays in refilling, minor non-adherence and residual drug effects) or switch of NOAC treatment, death, emigration or end of the study period (1 January 2019), whichever came first (on-treatment analysis) [21]. To account for changes in interacting drug use after NOAC initiation, patients who used PD interacting drugs at baseline were censored on the date they discontinued treatment, or patients who were not treated with PD interacting drugs at baseline were censored on the day during follow-up that they initiated one, as done before [12, 30,31,32].
Covariates
Baseline characteristics were assessed on the index date and included age, sex, NOAC type and dose, comorbidities, medication history and clinical risk scores. Comorbidities were identified ≤ 1 year before the index date with specific ICD-coded diagnoses, medical procedure codes and/or medication prescription claims (eTable 2). Medication history was identified with recent medication prescription claims ≤ 6 months before the index date. The CHA2DS2-VASc score, modified HAS-BLED score (without the ‘labile INR’ criterion) and age-adjusted Charlson Comorbidity Index (CCI) were calculated [1, 36].
Statistical analyses
Mean and standard deviation, and counts and percentages were presented for continuous and categorical variables, respectively. Crude event rates were calculated as the total number of events per 100 person-years at risk. Bleeding outcomes were investigated between AF patients initiating NOAC treatment with versus without concomitant use of PD interacting drugs. Moreover, outcomes were examined between patients concurrently treated with low-dose aspirin, P2Y12 inhibitors, NSAIDs, corticosteroids or SSRI/SNRIs, and patients without use of any PD interacting drug (reference group) in pairwise comparisons (not mutually exclusive, as some patients used multiple interacting drugs). To minimize confounding by indication and improve comparability, 1:1 propensity score matching (PSM) was performed using nearest neighbor matching without replacement and a caliper of 0.05 [33]. Propensity scores were calculated with logistic regression models including the 37 confounding covariates described in Table 1, namely age, sex, NOAC type (dabigatran, rivaroxaban, apixaban or edoxaban) and dose (standard or reduced dose), comorbidities, medication history including the most frequently used pharmacokinetically-interacting drugs, and clinical risk scores, stratified by calendar year. Covariate balance before and after matching was checked using standardized mean differences with a ≥ 0.1 threshold to indicate imbalance. Cox proportional hazard regression models were used to calculate adjusted hazard ratios (aHRs) with 95% confidence intervals (CIs). Unbalanced variables were incorporated in the Cox regression model. The proportional hazard assumption was assessed using scaled Schoenfeld residuals. A two-sided p-value of < 0.05 was considered statistically significant. All analyses were performed in R (R version 3.6.0).
Subgroup analyses
As exploratory subgroup analyses, outcomes were examined stratified by the number of PD interacting drugs used per patient (1, 2 or ≥ 3 drugs), by individual NOAC types and by NOAC doses, using 1:1 PSM for each pairwise comparison.
Sensitivity analysis
Several sensitivity analyses were performed to check the robustness of results. First, a more stringent definition of concomitant treatment was used which excluded subjects who may have discontinued the PD interacting drug just before or at the time of NOAC initiation (e.g., low-dose aspirin, NSAIDs). Therefore, at least one additional prescription claim for the PD interacting drug after NOAC initiation was required to be considered as concomitant use, as done before [12, 14]. Second, a > 30-day and > 90-day supply gap was used to consider discontinuation of NOAC or PD interacting drug treatment. Third, analyses were repeated using stabilized inverse probability of treatment weighting (IPTW). Lastly, to verify the AF population and reduce misclassification bias, only subjects with an ICD-coded hospital discharge diagnosis of AF before or up to 90 days after the index date were investigated [26].
Results
Baseline characteristics
Among 193,072 included NOAC-treated AF patients, 114,122 (59.1%) concomitantly used a PD interacting drug at the time of NOAC initiation (Table 1, eFig. 2). Antiplatelets were the most frequently used drug class involved in PD DDIs with NOACs (48.1%), followed by SSRI/SNRIs (10.0%), corticosteroids (8.4%) and NSAIDs (6.5%), whereas low-dose aspirin (45.1%), methylprednisolone (7.8%), clopidogrel (5.8%), escitalopram (4.0%) and diclofenac (1.8%) were the most commonly used individual drugs (eTable 5). Before matching, subjects concomitantly using PD interacting drugs were older (77.1 ± 9.8 versus 75.2 ± 10.5 years), had higher CHA2DS2-VASc (3.9 ± 1.8 versus 3.0 ± 1.6) and HAS-BLED scores (2.9 ± 1.1 versus 1.9 ± 1.1), had more cardiovascular comorbidities and used more drugs concomitantly (7.9 ± 4.2 versus 4.8 ± 3.3) than patients without concomitant use of PD interacting drugs (Table 1). After matching, covariate balance was achieved in each pairwise comparison, except for the number of concomitantly used drugs, CCI and some comorbidities (e.g., CAD) when investigating the impact of NSAIDs, which were incorporated in the Cox regression models (Table 1, eTable 6, eFig. 3).
Pharmacodynamic drug-drug interactions
AF patients with and without PD DDIs had a mean follow-up of 1.1 ± 1.3 years (125,705 person-years) and 1.3 ± 1.4 years (103,056 person-years), respectively. Before adjustment, event rates of MB/CRNMB ranged from 6.3/100 person-years among patients without use of PD interacting drugs, to 9.7, 9.8, 11.6, 17.8 and 21.1/100 person-years among patients concomitantly using low-dose aspirin, NSAIDs, SSRI/SNRIs, P2Y12 inhibitors and corticosteroids, respectively (Table 2).
After multivariable adjustment, concomitant use of PD interacting drugs was associated with significantly higher risks of MB/CRNMB (aHR 1.19, 95%CI (1.13–1.24)), major bleeding (aHR 1.15, 95%CI (1.08–1.23)), CRNMB (aHR 1.25, 95%CI (1.17–1.33)), gastrointestinal bleeding (aHR 1.12, 95%CI (1.03–1.22)), urogenital bleeding (aHR 1.21, 95%CI (1.09–1.35)) and bleeding at other sites (aHR 1.28, 95%CI (1.20–1.36)) in NOAC-treated AF patients, while the risk of intracranial bleeding (aHR 1.08, 95%CI (0.96–1.22)) was not significantly increased (Fig. 1, eTable 7).
Adjusted hazard ratios with 95% confidence intervals of outcomes compared between NOAC-treated AF patients with versus without concomitant use of PD interacting drugs. The number of subjects at risk and event rates per 100 person-years after 1:1 PSM are illustrated. aHR: adjusted hazard ratio; CI: confidence interval; CRNMB: clinically relevant non-major bleeding; DDI: drug-drug interaction; GI: gastrointestinal; MB: major bleeding; NOAC: non-vitamin K antagonist oral anticoagulant; NSAID: non-steroidal anti-inflammatory drug; PD: pharmacodynamic; PSM: propensity score matching; SNRI: serotonin and norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; vs: versus
Compared to subjects without use of PD interacting drugs, the significantly higher risk of MB/CRNMB was most pronounced among subjects concomitantly using P2Y12 inhibitors (aHR 1.62, 95%CI (1.48–1.77)) and corticosteroids (aHR 1.53, 95%CI (1.42–1.66)), followed by SSRI/SNRIs (aHR 1.26, 95%CI (1.17–1.35)), low-dose aspirin (aHR 1.14, 95%CI (1.08–1.20)) and NSAIDs (aHR 1.10, 95%CI (1.01–1.21)).
Trends in location-specific bleeding of specific drugs classes involved in PD DDIs with NOACs are illustrated in Fig. 1. Remarkably, significantly higher risks of intracranial bleeding were observed with SSRI/SNRIs (aHR 1.50, 95%CI (1.25–1.81)) and corticosteroids (aHR 1.49, 95%CI (1.21–1.84)), while the risk of gastrointestinal bleeding was not significantly increased with NSAIDs (aHR 1.13, 95%CI (0.95–1.33)).
Subgroup analyses
Compared to subjects without use of PD interacting drugs, the increased risk of MB/CRNMB was more pronounced among subjects concomitantly using 2 (n = 25,835; unadjusted event rate 14.8/100 person-years; aHR 1.44, 95%CI (1.34–1.55)) or ≥ 3 pharmacodynamically-interacting drugs (n = 5770; unadjusted event rate 19.8/100 person-years; aHR 1.57, 95%CI (1.39–1.78)) than 1 drug (n = 82,517; unadjusted event rate 8.6/100 person-years; aHR 1.12, 95%CI (1.07–1.18)) (Fig. 2, eTable 8). Moreover, analyses stratified by NOAC type and dose are illustrated in Fig. 2, and trends were consistent (eTable 9–10).
The risk of MB/CRNMB compared between NOAC-treated AF patients with versus without concomitant use of PD interacting drugs after 1:1 PSM, stratified by the number of interacting drugs, NOAC types and NOAC doses. The number of subjects at risk and event rates per 100 person-years after 1:1 PSM are illustrated. aHR: adjusted hazard ratio; CI: confidence interval; CRNMB: clinically relevant non-major bleeding; DDI: drug-drug interaction; MB: major bleeding; No.: number; NOAC: non-vitamin K antagonist oral anticoagulant; PD: pharmacodynamic; PSM: propensity score matching
Sensitivity analysis
When applying a more stringent definition of concomitant treatment, requiring at least one additional prescription claim for the PD interacting drug after NOAC initiation (n = 67,767; corresponding with 35.1% of the overall cohort or 59.4% of subjects with PD DDIs at the time of NOAC initiation), the increased risk of MB/CRNMB with versus without use of PD interacting drugs was more pronounced (aHR 1.47, 95%CI (1.40–1.55)), especially with low-dose aspirin (n = 49,531; aHR 1.65, 95%CI (1.55–1.74)) (eTable 11, eFig. 4). Likewise, significantly increased risks of gastrointestinal bleeding were observed with every PD interacting drug class, including NSAIDs (aHR 1.37, 95%CI (1.09–1.36)). Moreover, results were generally consistent when using a > 30- and > 90-day supply gap to identify treatment discontinuation (eTable 12, eFig. 5), when using IPTW (eTable 13, eFig. 6), or when restricting the study population to subjects with an ICD-coded hospital discharge diagnosis of AF (n = 103,723) (eTable 14, eFig. 7).
Discussion
In this nationwide cohort study, we have demonstrated that concomitant use of PD interacting drugs, identified in 59% of patients initiating NOAC treatment, was associated with increased risks of major, gastrointestinal, urogenital, and other bleeding. The increase in bleeding risk was most pronounced with concomitant use of P2Y12 inhibitors and corticosteroids, followed by SSRI/SNRIs, low-dose aspirin and NSAIDs. Remarkably, significantly higher intracranial bleeding risks were observed among NOAC users concurrently treated with SSRI/SNRIs and corticosteroids, which highlights the need for future research to replicate these exploratory findings.
Pharmacodynamic interactions frequently occur among AF patients initiating NOAC treatment [12,13,14,15, 37]. In line with prior research [28, 31], we observed a 19% higher bleeding risk when NOACs were combined with PD interacting drugs and this bleeding risk further increased in patients concurrently using 2 or ≥ 3 interacting drugs (44% and 57% higher risk, respectively). Therefore, potential benefits of combining these drugs should be carefully balanced against their potential impact on the bleeding risk, whereas discontinuation or switch of PD interacting drugs may be preferred, if possible [1]. Exemplary, 41% of patients concomitantly using PD interacting drugs at the time of NOAC initiation did not fill a new prescription of the interacting drug after NOAC initiation, which may indicate adequate discontinuation or switch of treatment. Nevertheless, as 59% of patients did renew their prescription after NOAC initiation and bleeding risks were even more pronounced in this subgroup (47% higher risk compared to 19% overall), there is still room for improvement. Therefore, continued efforts targeting both healthcare professionals (physicians and pharmacists) and patients to increase the awareness of increased bleeding risks when combining NOACs with PD interacting drugs may be needed. Physicians should check whether the PD interacting drug can be discontinued or switched, in line with guideline recommendations [1, 38], and pharmacists should screen for such interactions and contact the prescribing physician when they occur [39]. If discontinuation is not possible, NOACs should be appropriately dosed, modifiable bleeding risk factors should be addressed (e.g., uncontrolled hypertension), and patients should be informed of the increased risk of bleeding [1, 39]. Close monitoring by earlier and more frequent follow-up of patients during concomitant use of NOACs and PD interacting drugs is advisable [1, 37, 39].
AF and (atherosclerotic) vascular disease frequently coincide, posing a therapeutic dilemma for physicians to balance benefits and risks of anticoagulants and antiplatelets [12, 13, 38]. Since low-dose aspirin and P2Y12 inhibitors inhibit platelet aggregation and primary haemostasis, whereas NOACs inhibit the coagulation pathway and secondary haemostasis, the combination of NOACs with antiplatelets has consistently been associated with increased risks of bleeding [12,13,14,15,16, 27, 28], especially triple therapy (NOAC, P2Y12 inhibitor and aspirin) [13, 17,18,19,20, 27], which was also observed among VKA users [40, 41]. Likewise, the combination of NOACs with aspirin in AF patients with stable CAD has been associated with increased bleeding risks, without significantly reducing atherothrombotic risks [12, 16, 42]. In the present study, a 14% and 62% significantly higher risk of bleeding was observed among NOAC users concurrently treated with low-dose aspirin and P2Y12 inhibitors, respectively. Although the increased risk of bleeding may appear less pronounced with concomitant use of low-dose aspirin than P2Y12 inhibitors, bleeding risks may have been attenuated by subjects discontinuing aspirin at the time of NOAC initiation. Exemplary, 21–47% of patients on aspirin at baseline included in the ARISTOTLE and ROCKET-AF trial discontinued aspirin after enrolment [12, 14]. In our study, still 57% of baseline aspirin users filled at least one additional prescription of low-dose aspirin after NOAC initiation and the increased bleeding risks were substantially more pronounced in this subgroup (65% higher risk). Therefore, non-indicated antiplatelet use should be avoided [1, 12, 27, 38]. According to current guideline recommendations, aspirin should not be combined with NOACs in most AF patients with vascular disease, except for short-term triple therapy up to 1 week after PCI (or ≤ 1 month after an acute coronary syndrome (ACS) with PCI if high atherothrombotic and low bleeding risk) [1, 12, 38]. Likewise, prolonged association of NOACs with P2Y12 inhibitors after PCI (> 6 months after elective PCI, > 12 months after ACS with PCI) should also be avoided in the majority of AF patients with vascular disease [1, 12, 38].
NSAIDs are used for pain relief and inflammatory diseases (e.g., rheumatoid arthritis), and inhibit cyclooxygenase (COX) enzymes, reducing the synthesis of thromboxane A2, prostacyclin and prostaglandins [30, 43]. Consequently, higher bleeding risks have been observed when combining NSAIDS with NOACs [30, 34, 44] or VKAs [30, 45, 46], in line with the 10% higher risk illustrated in the present study. However, we could not demonstrate a significantly higher risk of gastrointestinal bleeding, which adds to the conflicting evidence seen in prior studies [30, 34, 44]. This may be due to the high proportion of concomitant PPI use (47% after matching), selective prescribing of NSAIDs to NOAC users without an increased risk of gastrointestinal bleeding, and attenuated bleeding risks driven by subjects using NSAIDs intermittently during a short period of time for acute pain relief or subjects discontinuing NSAIDs at the time of NOAC initiation [30]. Exemplary, when specifically investigating subjects who renewed an NSAID prescription after NOAC initiation, a 37% significantly higher risk of gastrointestinal bleeding was observed. Therefore, NSAIDs should be avoided for pain relief, or used for as short a time as possible in NOAC users [1, 38].
Systemic corticosteroids are used for several medical conditions (e.g., chronic lung disease, cancer, inflammatory diseases, organ transplant…). However, due to the inhibition of prostaglandin synthesis, they are also known to increase the risk of gastrointestinal bleeding [47]. Indeed, concomitant use of corticosteroids with NOACs was associated with a 53% and 49% significantly increased risk of MB/CRNMB and gastrointestinal bleeding, respectively. To the best of our knowledge, only one observational study has explored the impact of corticosteroids in association with NOACs on safety outcomes, demonstrating a doubled risk of gastrointestinal bleeding [29]. Remarkably, intracranial, urogenital and other bleeding risks were also significantly increased among NOAC users concurrently treated with corticosteroids, although these findings may reflect a higher vulnerability of AF patients using systemic corticosteroids and should therefore be interpreted with caution.
SSRI/SNRIs, used for depression and anxiety, also interfere with platelet aggregation due to the inhibition of serotonin reuptake in platelets [32, 33, 48]. Indeed, increased risks of bleeding have been observed when combining SSRIs with VKAs [32, 45, 49] or NOACs [28, 34, 50], albeit not consistently with NOACs [32, 33]. Remarkably, concomitant use of SSRI/SNRIs with NOACs was associated with a 50% significantly increased risk of intracranial bleeding in this study. Higher intracranial bleeding risks with SSRIs have also been observed in AF patients treated with VKAs [49, 51] or NOACs [34, 50], as well as in non-anticoagulated patients without AF [48, 51]. Therefore, caution should be warranted and a reduced NOAC dose may be considered in case of other risk factors for bleeding based on recommendations of the EHRA Practical Guide [1]. Future studies are urgently needed to replicate these findings, to assess whether other antidepressants may be preferred in NOAC-treated AF patients with depression or anxiety, and to assess the effectiveness and safety of using an off-label reduced NOAC dose in case of PD interacting drug use and other bleeding risk factors.
Several studies have also demonstrated an increased risk of bleeding among VKA-treated AF patients with versus without concomitant use of PD interacting drugs [30, 32, 40, 41, 45, 46, 49]. To the best of our knowledge, dedicated trials investigating the benefit-risk profile of NOACs compared to VKAs in patients concurrently treated with PD interacting drugs, to assess whether PD DDIs of NOACs are more, less or equally severe as PD DDIs of VKAs, are currently lacking. However, no significant interaction between PD interacting drug use and randomized treatment (the investigated NOAC or warfarin) on bleeding outcomes was observed in post-hoc analyses of phase 3 randomized controlled trials [13,14,15, 30, 33, 44].
Strengths and limitations
Strengths of this nationwide cohort study include the large sample size, long-term follow-up, use of an on-treatment analysis that accounted for changes in interacting drug use during follow-up to reduce exposure misclassification, and adjustment for multiple confounders using PSM.
Several limitations should be acknowledged. First, assessment of PD DDIs was based on dispensing data, not on the patients’ actual intake or physicians’ prescriptions, and may have been overestimated (due to the assumption that every dispensed pill is taken). Exemplary, discontinuation of the interacting drug at the time of NOAC initiation or before the calculated last day of supply, or short-term intermittent use, could not be identified. Nevertheless, results were consistent (e.g., with SSRI/SNRI) or even more pronounced (e.g., with low-dose aspirin) when only investigating patients with ≥ 1 additional prescription for the same PD interacting drug after NOAC initiation. Likewise, trends were consistent using different supply gaps to define discontinuation. Second, certain NSAIDs (aspirin 325–1000 mg, ibuprofen 200–400 mg and naproxen 220 mg) were available over-the-counter, and therefore dispensing data of these drugs were not systematically recorded in the nationwide database. Third, due to the observational design using healthcare databases, coding errors and misclassification bias may be present. However, by identifying comorbidities based on ICD, medical procedure codes and/or medication prescription claims assessed in ambulatory and hospital care, missing data and misclassification of characteristics were reduced. Fourth, although PSM improved comparability and reduced confounding by (contra)indication, unmatched individuals were discarded from the analysis, reducing the effective sample size and increasing the risk of selection bias [52]. Nevertheless, results were consistent using IPTW, which included every individual. Fifth, despite thorough adjustment for 37 confounders, there is a risk of unmeasured confounding due to missing lifestyle characteristics (e.g., body weight, smoking) and laboratory values (e.g., renal function), and selective prescribing of PD interacting drugs to sicker AF patients at increased risk of bleeding. Outcomes may have been influenced by the severity of underlying comorbidities (e.g., ACS versus stable CAD), peri-procedural complications (e.g., after PCI), recent hospitalisations (e.g., intravenous corticosteroid use for acute exacerbation of chronic lung disease), polypharmacy, reduced drug adherence, and inappropriate drug dosing (including off-label NOAC dosing, which could not be assessed due to the lack of data on body weight and renal function) [21, 37]. Our results should therefore be interpreted with caution and considered as hypothesis-generating. Lastly, although persons with competing treatment indications were excluded, subjects were not required to have an ICD-coded hospital discharge diagnosis of AF to be included, as this would have limited the study population to hospitalized AF subjects and excluded AF subjects treated exclusively in primary or ambulatory care [7, 26]. Nevertheless, trends were consistent when specifically investigating subjects with an ICD-coded diagnosis of AF ≤ 1 year before or ≤ 90 days after the index date.
Conclusion
In conclusion, concomitant use of PD interacting drugs with NOACs was associated with higher major, gastrointestinal, urogenital, and other bleeding risks compared to NOAC-treated AF patients without PD interacting drug use, which was most pronounced with P2Y12 inhibitors and corticosteroids, followed by SSRI/SNRIs, low-dose aspirin and NSAIDs. Remarkably, significantly higher intracranial bleeding risks were observed when SSRI/SNRIs or corticosteroids were combined with NOACs, compared to patients without PD interacting drug use, highlighting the need for future research.
Material and/or Code availability
Requests for the data underlying this article should be directed to the administrators of the InterMutualistic Agency (IMA) database or Minimal Hospital Dataset and is subject to approval.
References
Steffel J, Collins R, Antz M, et al. 2021 European heart rhythm association practical guide on the use of non-vitamin k antagonist oral anticoagulants in patients with atrial fibrillation. Europace : Eur Pacing, Arrhythmias, Card Electrophysiol: J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol. 2021;23(10):1612–76.
Grymonprez M, Simoens C, Steurbaut S, De Backer TL, Lahousse L. Worldwide trends in oral anticoagulant use in patients with atrial fibrillation from 2010 to 2018: a systematic review and meta-analysis. Europace : Eur Pacing, Arrhythmias, Card Electrophysiol: J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol. 2022;24(6):887–98.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–51.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–104.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–92.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–91.
Grymonprez M, De Backer TL, Bertels X, Steurbaut S, Lahousse L. Long-term comparative effectiveness and safety of dabigatran, rivaroxaban, apixaban and edoxaban in patients with atrial fibrillation: A nationwide cohort study. Front Pharmacol. 2023;14:1125576.
Chan YH, See LC, Tu HT, et al. Efficacy and safety of apixaban, dabigatran, rivaroxaban, and warfarin in asians with nonvalvular atrial fibrillation. J Am Heart Assoc. 2018;7(8):e008150. https://doi.org/10.1161/JAHA.117.008150.
Paschke LM, Klimke K, Altiner A, von Stillfried D, Schulz M. Comparing stroke prevention therapy of direct oral anticoagulants and vitamin K antagonists in patients with atrial fibrillation: a nationwide retrospective observational study. BMC Med. 2020;18(1):254.
Warkentin L, Hueber S, Deiters B, Klohn F, Kühlein T. Vitamin-K-antagonist phenprocoumon versus low-dose direct oral anticoagulants (DOACs) in patients with atrial fibrillation: a real-world analysis of German claims data. Thromb J. 2022;20(1):31.
Ujeyl M, Koster I, Wille H, et al. Comparative risks of bleeding, ischemic stroke and mortality with direct oral anticoagulants versus phenprocoumon in patients with atrial fibrillation. Eur J Clin Pharmacol. 2018;74(10):1317–25.
Alexander JH, Lopes RD, Thomas L, et al. Apixaban vs. warfarin with concomitant aspirin in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2014;35(4):224–32.
Dans AL, Connolly SJ, Wallentin L, et al. Concomitant use of antiplatelet therapy with dabigatran or warfarin in the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) trial. Circulation. 2013;127(5):634–40.
Shah R, Hellkamp A, Lokhnygina Y, et al. Use of concomitant aspirin in patients with atrial fibrillation: findings from the ROCKET AF trial. Am Heart J. 2016;179:77–86.
Xu H, Ruff CT, Giugliano RP, et al. Concomitant use of single antiplatelet therapy with edoxaban or warfarin in patients with atrial fibrillation: analysis from the ENGAGE AF-TIMI48 Trial. J Am Heart Assoc. 2016;5(2):e002587. https://doi.org/10.1161/JAHA.115.002587.
Yasuda S, Kaikita K, Akao M, et al. Antithrombotic therapy for atrial fibrillation with stable coronary disease. N Engl J Med. 2019;381(12):1103–13.
Dewilde WJ, Oirbans T, Verheugt FW, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet (London, England). 2013;381(9872):1107–15.
Lopes RD, Heizer G, Aronson R, et al. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019;380(16):1509–24.
Cannon CP, Bhatt DL, Oldgren J, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017;377(16):1513–24.
Gibson CM, Mehran R, Bode C, et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016;375(25):2423–34.
Grymonprez M, Capiau A, Steurbaut S, et al. Adherence and persistence to oral anticoagulants in patients with atrial fibrillation: A Belgian nationwide cohort study. Front Cardiovasc Med. 2022;9:994085.
InterMutualistic Agency (IMA/AIM). Available from: https://ima-aim.be/. Accessed 25 November 2021.
The Minimal Hospital Dataset. Available from: https://www.health.belgium.be/en/node/23607. Accessed 25 November 2021.
The Sectoral Committee of Social Security and Health, Section Health ('Informatieveiligheidscomité'). Available from: https://www.ehealth.fgov.be/ehealthplatform/nl/informatieveiligheidscomite. Accessed 25 November 2021.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet (London, England). 2007;370(9596):1453–7.
Hellfritzsch M, Pottegård A, Haastrup SB, Rasmussen L, Grove EL. Cohort selection in register-based studies of direct oral anticoagulant users with atrial fibrillation: an inevitable trade-off between selection bias and misclassification. Basic Clin Pharmacol Toxicol. 2020;127(1):3–5.
van Rein N, Heide-Jorgensen U, Lijfering WM, Dekkers OM, Sorensen HT, Cannegieter SC. Major bleeding rates in atrial fibrillation patients on single, dual, or triple antithrombotic therapy. Circulation. 2019;139(6):775–86.
Zhang Y, Souverein PC, Gardarsdottir H, van den Ham HA, van der Zee AHM, de Boer A. Risk of major bleeding among users of direct oral anticoagulants combined with interacting drugs: a population-based nested case-control study. Br J Clin Pharmacol. 2020;86(6):1150–64.
Holt A, Blanche P, Zareini B, et al. Gastrointestinal bleeding risk following concomitant treatment with oral glucocorticoids in patients on non-vitamin K oral anticoagulants. Heart. 2022;108(8):626–32.
Dalgaard F, Mulder H, Wojdyla DM, et al. Patients with atrial fibrillation taking nonsteroidal anti-inflammatory drugs and oral anticoagulants in the ARISTOTLE Trial. Circulation. 2020;141(1):10–20.
Holm J, Mannheimer B, Malmström RE, Eliasson E, Lindh JD. Bleeding and thromboembolism due to drug-drug interactions with non-vitamin K antagonist oral anticoagulants-a Swedish, register-based cohort study in atrial fibrillation outpatients. Eur J Clin Pharmacol. 2021;77(3):409–19.
Komen JJ, Hjemdahl P, Mantel-Teeuwisse AK, Klungel OH, Wettermark B, Forslund T. Concomitant anticoagulant and antidepressant therapy in atrial fibrillation patients and risk of stroke and bleeding. Clin Pharmacol Ther. 2020;107(1):287–94.
Quinn GR, Hellkamp AS, Hankey GJ, et al. Selective serotonin reuptake inhibitors and bleeding risk in anticoagulated patients with atrial fibrillation: an analysis from the ROCKET AF Trial. J Am Heart Assoc. 2018;7(15):e008755.
Lee MT, Park KY, Kim MS, You SH, Kang YJ, Jung SY. Concomitant use of NSAIDs or SSRIs with NOACs requires monitoring for bleeding. Yonsei Med J. 2020;61(9):741–9.
Kaatz S, Ahmad D, Spyropoulos AC, Schulman S. Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost:JTH. 2015;13(11):2119–26.
Quan H, Li B, Couris CM, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82.
Grymonprez M, Petrovic M, De Backer TL, Steurbaut S, Lahousse L. The impact of polypharmacy on the effectiveness and safety of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Thromb Haemost. 2023. https://doi.org/10.1055/s-0043-1769735.
Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498.
Capiau A, Mehuys E, De Bolle L, Van Tongelen I, De Backer T, Boussery K. Drug-drug interactions with direct oral anticoagulants: development of a consensus list for ambulatory care. Int J Clin Pharm. 2023;45(2):364–74.
Dentali F, Douketis JD, Lim W, Crowther M. Combined aspirin-oral anticoagulant therapy compared with oral anticoagulant therapy alone among patients at risk for cardiovascular disease: a meta-analysis of randomized trials. Arch Intern Med. 2007;167(2):117–24.
Andreotti F, Testa L, Biondi-Zoccai GG, Crea F. Aspirin plus warfarin compared to aspirin alone after acute coronary syndromes: an updated and comprehensive meta-analysis of 25,307 patients. Eur Heart J. 2006;27(5):519–26.
Lamberts M, Gislason GH, Lip GY, et al. Antiplatelet therapy for stable coronary artery disease in atrial fibrillation patients taking an oral anticoagulant: a nationwide cohort study. Circulation. 2014;129(15):1577–85.
Vane JR, Botting RM. Mechanism of action of nonsteroidal anti-inflammatory drugs. Am J Med. 1998;104(3a):2S-8S (discussion 21S-2S).
Kent AP, Brueckmann M, Fraessdorf M, et al. Concomitant oral anticoagulant and nonsteroidal anti-inflammatory drug therapy in patients with atrial fibrillation. J Am Coll Cardiol. 2018;72(3):255–67.
Schalekamp T, Klungel OH, Souverein PC, de Boer A. Increased bleeding risk with concurrent use of selective serotonin reuptake inhibitors and coumarins. Arch Intern Med. 2008;168(2):180–5.
Lamberts M, Lip GY, Hansen ML, et al. Relation of nonsteroidal anti-inflammatory drugs to serious bleeding and thromboembolism risk in patients with atrial fibrillation receiving antithrombotic therapy: a nationwide cohort study. Ann Intern Med. 2014;161(10):690–8.
Narum S, Westergren T, Klemp M. Corticosteroids and risk of gastrointestinal bleeding: a systematic review and meta-analysis. BMJ Open. 2014;4(5):e004587.
Shin D, Oh YH, Eom CS, Park SM. Use of selective serotonin reuptake inhibitors and risk of stroke: a systematic review and meta-analysis. J Neurol. 2014;261(4):686–95.
Quinn GR, Singer DE, Chang Y, et al. Effect of selective serotonin reuptake inhibitors on bleeding risk in patients with atrial fibrillation taking warfarin. Am J Cardiol. 2014;114(4):583–6.
Chang KH, Chen CM, Wang CL, et al. Major bleeding risk in patients with non-valvular atrial fibrillation concurrently taking direct oral anticoagulants and antidepressants. Front Aging Neurosci. 2022;14:791285.
Hackam DG, Mrkobrada M. Selective serotonin reuptake inhibitors and brain hemorrhage: a meta-analysis. Neurology. 2012;79(18):1862–5.
Allan V, Ramagopalan SV, Mardekian J, et al. Propensity score matching and inverse probability of treatment weighting to address confounding by indication in comparative effectiveness research of oral anticoagulants. J Comp Eff Res. 2020;9(9):603–14.
Acknowledgements
We would like to thank the administrators, data managers, statisticians and other staff of the InterMutualistic Agency (IMA) and Minimal Hospital Dataset (MHD) for providing the data, especially Birgit Gielen (IMA), David Jaminé (IMA), Iris Grant (IMA), Montse Urbina (IMA), Dirk De Kesel (IMA), Sarah Bel (IMA), Jérôme Paque (IMA), Remi Vandereyd (IMA), Xavier Rygaert (IMA), Delfien Verhelst (MHD), Karin Smets (MHD) and Francis Windey (MHD). Moreover, we would like to thank eHealth for the deterministic linkage of both databases. Lastly, we would like to thank Stephan Devriese (Belgian Health Care Knowledge Centre, KCE) for performing the small cell risk analysis.
Funding
This work was supported by the Research Foundation Flanders (FWO) [Grant number 11C0820N to Maxim Grymonprez].
Author information
Authors and Affiliations
Contributions
MG and LL contributed to the concept and design of the study. MG performed the statistical analysis, interpretation and writing under the supervision of LL. AC, SS, KB, AC, EM, AS, MP, TDB and LL revised the manuscript critically. All authors contributed to the article and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This study was approved by the IMA and MHD database administrators and by the ‘Sectoral Committee of Social Security and Health, Section Health’, a subcommittee of the Belgian Commission for the Protection of Privacy (approval code IVC/KSZG/20/344), waiving the need for individual informed consents [24].
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Competing Interests
Outside this manuscript, TDB has served as a chairperson during a lecture for Bayer and Daiichi Sankyo and participated in an expert meeting for Pfizer. Outside this manuscript, LL has been consulted as expert for AstraZeneca. Outside this manuscript, MP and SS have given a lecture sponsored by BMS, LL a lecture sponsored by Chiesi, and SS, LL and MG lectures sponsored by IPSA vzw, a non-profit organization facilitating lifelong learning for pharmacists. No author has received any fees personally.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Grymonprez, M., Capiau, A., Steurbaut, S. et al. Pharmacodynamic Drug-Drug Interactions and Bleeding Outcomes in Patients with Atrial Fibrillation Using Non-Vitamin K Antagonist Oral Anticoagulants: a Nationwide Cohort Study. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07521-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07521-5