Abstract
Background
The optimal dosing strategy of four-factor prothrombin complex concentrate (4F-PCC) for vitamin K antagonists (VKAs) reversal is unknown.
Methods
We conducted systematic search on the PubMed, SCOPUS, and Embase databases from inception to December 2020 for clinical studies that compared the fixed-dose versus variable-dose of 4-PCC for VKAs reversal with at least one reported clinical outcome. The treatment effects were expressed as relative ratios (RR) with 95% confidence intervals (CIs) and pooled by a random-effects model.
Results
Ten studies, including 988 patients, were included. Fixed-dose 4-PCC was associated with lower rate of mortality (RR= 0.65, 95% CI 0.47 to 0.9, p= 0.009), comparable rate of thromboembolic event (TEE) (RR= 1.10, 95%CI 0.44 to 2.80, p= 0.826), and lower goal INR reached (RR= 0.87, 95%CI 0.78 to 0.96, p= 0.007). Less 4-PCC cumulative dose, shorter duration of order-to-needle time, similar hospital length of stay, the comparable time required for INR reversal, higher post-4-PCC INR, and a higher need for additional dose were observed in fixed-dose.
Conclusions
The use of a fixed-dose of 4-PCC may be considered an effective and safe dosing strategy for VKAs reversal in various clinical situations. However, further well-designed, controlled studies should be conducted focusing on clinical outcomes to determine the optimal dose of 4-PCC for VKAs reversal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin K antagonists (VKAs) are widely prescribed effective anticoagulants for the prevention and treatment of various thromboembolic events [1] and mainly act via inhibition of the vitamin K-dependent clotting factors synthesis [2]. Although direct oral anticoagulants have been introduced as alternatives, there are still some conditions in that VKAs remained the agent of choice [3], but the VKAs-related bleeding complications should not be neglected [4], as the rate of warfarin-induced major bleeding was reported to be 10 to 16% [5]. The risk of warfarin-associated intracerebral hemorrhage (ICH) may reach 1 to 2% per year, and this risk increases up to 4.2% in older patients [6, 7] The risk of major bleeding in the patient receiving warfarin who undergo urgent surgery was also as high as 21.6% [8]. Consequently, if indicated, these patients require prompt and effective reversal of VKA associated coagulopathy [9]. Vitamin K is used mainly in combination with other reversal agents, such as prothrombin complex concentrates (PCC) [9, 10] and fresh frozen plasma (FFP) [11] for VKAs reversal. Generally, 4-factor PCC (4-PCC) is preferred over FFP [12] and 3-factor PCC (3-PCC) [13] for urgent reversal of VKA due to better safety and efficacy.
4-PCC contains the human coagulation factors, including factors II, VII, IX, and X [13]. Although the safety and efficacy of 4-PCC have been well established for VKA reversal [12], optimal dosing strategy remains uncertain. Therefore, several studies have been conducted to determine the optimal dose of 4-PCC for VKAs reversal [14]. The recommended dosing regimen of package insert is a variable-dose regimen based on body weight and pre-treatment INR ranging from 25 to 50 units of factor IX per kg [15]. Based on this dosing, the efficacy of 4-PCC is not optimal, and adequate hemostasis is reported only in up to 71% of patients [16].
The most recent 2020 American College of Cardiology (ACC) Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants recommended reversal of VKAs with 4-PCC using either package insert recommendations or low, fixed-dose strategy [17]. Several advantages of fixed-dose strategy have been proposed, including faster 4-PCC administration [18], no need for dose calculation [19], hypothetically decreased risk of thromboembolic event (TEE) [14, 20], and lower cost [21]. Conversely, the variable-dose may be associated with a higher rate of goal INR reached, especially in the patient with a high baseline INR [18]; however, the TEE rate may be increased in concordance with the PCC dose [22]. Therefore, several studies have evaluated the clinical outcomes of the fixed-dose versus variable-dose strategy of 4-PCC; nevertheless, the results were inconsistent [14]. To address these dicrapancies, we did a systematic review and meta-analysis of clinical studies to investigate the efficacy and safety of fixed-dose 4-PCCs compared to the variable, weight/INR-based dosing strategy for VKAs reversal in patients who present with major bleeding or a need for urgent surgery or invasive procedure.
Methods
Search Strategy
This systematic review and meta-analysis were performed in concordance with the PRISMA [Preferred Reporting Items for Systematic Review and Meta-analysis] guidelines [23]. A comprehensive systematic search was carried out in PubMed, SCOPUS, Embase, and Gray literature by two independent reviewers (KM and SY) from inception until December 2020 without any time or language restrictions by using the following keywords: “warfarin OR vitamin K antagonists OR VKA OR VKAs OR coumarin OR coumadin OR phenprocoumon OR acenocoumarol” AND “4-factor prothrombin complex concentrate OR prothrombin complex concentrate OR 4-PCC OR PCC.” Relevant studies were hand-searched within their references.
Study Selection and Inclusion Criteria
Two reviewers (KM and SY) independently performed study selection using prespecified inclusion and exclusion criteria. Studies were included if they met the following criteria: (1) randomized controlled trials (RCTs) and prospective or retrospective observational studies, (2) publications that were carried out on adult patients who presented with VKAs-related major bleeding, or those who required urgent VKAs reversal for surgery or an invasive procedure, (3) studies which compared fixed-dose (based on indication; regardless of the patient's weight and presenting INR) and variable-dose of 4-PCC (package insert-based recommendation; INR/weight-based dosing) (4) those with at least one reported relevant efficacy and safety outcome. Any disagreements regarding the inclusion of each study were resolved by a third researcher (AH). Reviews, comments, abstracts, letters, conference papers, case reports, duplicates, and unpublished articles were excluded from consideration in this study.
Data Extraction
Two researchers (SY, MA) extracted the data using a standardized data record form, and the whole team resolved any disagreements in this step. The following information was retrieved: name of the first author, publication year, study location, subjects’ demographic data (age, sex, weight, etc.), study design, number of participants, VKAs indications, site of bleeding, the administered dose of 4-PCC, reversal-related efficacy and safety outcomes (number or mean ± SD of measured outcomes).
Outcomes
The various efficacy and safety outcomes were extracted and evaluated as outcome measures. The primary outcomes including the mortality rate during a follow-up period of each study, rate of 4-PCC related arterial and venous thrombotic events, and the number of goal INR reached that defined as patients who reached goal INR as specified by each study. The secondary outcomes including the number of patients required administration of the supplemental dose of 4-PCC in addition to the initial dose, the total and weight-based administered dose of the 4-PCC, the mean time required for INR reversal, post 4-PCC administration mean INR (after 15–30 min or other close times as defined by the included studies), order-to-needle time (the time between the ordering of 4-PCC to start of infusion), and the total length of hospital stay.
Assessment of Study Quality
The methodological quality of the included studies was evaluated independently by two reviewers, and any disagreements were resolved by consensus. The Newcastle-Ottawa Scales (NOS) [24] and Jadad scale [25] were used for quality assessment of cohort and RCTs studies, respectively. The NOS assesses the quality of nonrandomized/observational cohort studies based on eight items that are categorized into three groups: (a) the selection of the study groups (0–4 points), (b) the comparability of the groups (0–2 points), and (c) the and study outcomes (0–3 points). The NOS scores of 7 or higher were considered high-quality studies, and scores of 5 to 6 denoted moderate qualities [26]. In the Jadad scale, papers were evaluated based on randomization, blinding, and inclusion of participants. Based on this scale, studies with a score of 3 or more were considered high-quality trials [25].
Data Synthesis and Statistical Analysis
To evaluate the pooled effects of various dosing strategies (fixed-dose vs. variable-dose of 4-PCCs) on categorical and continuous outcomes, a meta-analysis was carried out using the relative risk (RR), weighted mean differences (WMD), and their 95% confidence intervals (CI), respectively, by random-effects model [27, 28]. Heterogeneity across included studies was determined using Cochrane’s Q test and the I2 statistic. [29]. I2 above 50% and Cochrane’s Q test with p < 0.1 was considered the existence of significant heterogeneity. In some instance, we performed a priori subgroup analysis according to indication for VKAs reversal (all indication together, non-ICH patients and only ICH patients), mean baseline INR of the included patient (INR ≥ 4 vs. INR < 4), and weight of the patient (weight ≥ 80 kg vs. weight <80 kg). The potential non-linear effects for the dose of 4-PCC were examined using fractional polynomial modeling. Egger’s regression test and visual examination of the funnel plot were applied to measure publication bias. All statistical analyses were performed using STATA 15.0 statistical software (Stata Corporation, College Station, TX, USA).
Results
Study Selection
The flowchart of literature the search and selection process of studies is presented in Fig. 1. From the literature search, we identified 2386 articles. After removing duplicates, 1496 articles were screened by title and abstract. Overall, 72 articles were found potentially relevant for detailed full-text evaluation. Finally, the literature search yielded ten [18, 21, 30,31,32,33,34,35,36,37] eligible articles for the current meta-analysis
Study Characteristics
The characteristics of the included studies are summarized in Table 1. Six and four studies were conducted in the USA [21, 30,31,32,33,34] and the Netherlands [18, 35,36,37], respectively. Studies were published between 2006 and 2020. Among these, nine studies were prospective or retrospective cohort studies [18, 21, 30,31,32,33,34,35,36], and one of them was RCT [37]. All of the studies were performed to compare fixed-dose versus variable-dose of 4-PCC for reversal of VKAs in different clinical settings, including intracranial hemorrhage (ICH), extra-cranial hemorrhage (ECH), and emergent surgical procedures. The Cofact and Kcentra 4-PCC products were used in four [18, 35,36,37] and five [21, 30,31,32, 34] studies, respectively. One study did not mention the brand name of the administered 4-PCC [33]. Two studies included only ICH patients [33, 36], while ICH patients were excluded from two studies [18, 35]. The mean ± SD age of the participants was 75.2 ± 3.9 years. Data of 988 patients (442 patients in the fixed-dose and 546 patients in the variable-dose group) were pooled for this analysis. The results of the quality assessment of eligible cohort studies are also presented in Table 1. The cohort studies demonstrated high quality with NOS scores ranging from 7 to 9. The Jadad score of one included RCT was equal to 3 points, considered high quality.
Results of the Meta-Analysis
Primary Outcome: Mortality, TEE, and Goal INR Reached
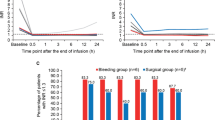
Mortality was reported in nine studies. As shown in Fig. 2, the risk of mortality was significantly lower in the fixed-dose group (50 of 395 [12.6%]) than the variable-dose group (98 of 500, [19.6%]; RR= 0.65, 95% CI, 0.47 to 0.9; p= 0.009). Heterogeneity among the studies was negligible (p-heterogeneity= 0.802, I2= 0.0). Subgroup analysis based on indication of reversal and site of bleeding showed the lower mortality rate in fixed-dose compared to variable-dose in all reversal indications (RR= 0.56, 95% CI 0.35 to 0.9, p= 0.019) and non-ICH patients (RR= 0.55, 95% CI 0.32 to 0.95, p= 0.032); however, in patients with ICH, the difference in mortality rate was not significant (RR= 1.22, 95% CI 0.6 to 2.46, p= 0.580). In subgroup analysis of data based on weight of included population, lower rate of mortality was seen in both groups weight <80 kg (RR= 0.66, 95% CI 0.41 to 0.9, p= 0.013) and weight ≥ 80 kg (RR= 0.75, 95% CI 0.42 to 1.33, p= 0.319), although this was not significant in later group. The mortality rate was significantly lower in the fixed-dose versus the variable-dose strategy among patients with baseline INR > 4 (RR= 0.55, 95% CI 0.33 to 0.99, p= 0.026), but this difference was not significant among patient with baseline INR < 4 (RR= 0.72, 95% CI 0.48 to 1.08, p= 0.114) (Table 2).
Forest plot of the mortality in patients receiving fixed-dose 4-PCC comparing with variable-dose strategy, a overall analysis, b sub-group analysis based on weight, c sub-group analysis based on reversal indication, d sub-group analysis based on pre-PCC administration INR (total sample size; fixed-dose = 395, variable-dose = 500). ICH: intracerebral hemorrhage, RR; relative risk, CI: confidence intervals
TEE rate was reported in 10 studies. Similar TEE rate was seen between the two dosing strategies (fixed-dose 9 of 442 patients [2.03%] vs. variable-dose 8 of 546 patients [1.47%]; RR= 1.10, 95% CI 0.44, 2.80, p= 0.826) in overall analysis, as shown in Fig. 3. No heterogeneity was observed among studies which reported TEE rate (p-heterogeneity= 0.881, I2= 0.0%). A similar rate of thromboembolic events was also seen in fixed-dose compared to variable-dose in subgroups analysis based on VKA reversal indication, weight, and baseline INR (Table 2).
Forest plot of the thromboembolic events in patients receiving fixed-dose 4-PCC comparing with variable-dose strategy, a overall analysis, b sub-group analysis based on weight, c sub-group analysis based on reversal indication, d sub-group analysis based on pre-PCC administration INR (total sample size; fixed-dose = 442, variable-dose = 546). ICH: intracerebral hemorrhage, RR; relative risk, CI: confidence intervals
The number of goal INR reached, or hemostasis reversal, was assessed as an efficacy outcome in all ten included studies. As shown in Fig. 4, the rate of goal INR reached was significantly lower in the fixed-dose group (311 of 442 [70.36%]) than the variable-dose group (444 of 546, [81.32%]; RR= 0.87, 95% CI; 0.78, 0.96, p= 0.007) with substantial heterogeneity (p-heterogeneity= 0.023, I2= 53.2). In subgroup analysis based on 4-PCC indication, the number of goal INR reached was not statistically significant between the two groups (Table 2). Similar goal INR reached was observed in subgroup analysis of patient with weight ≥ 80 kg (RR= 0.95, 95% CI 0.85, 1.07, p= 0.385), whereas among patient with weight < 80, lower INR reversal was observed in fixed-dose (RR= 0.79, 95% CI 0.66 to 0.96, p= 0.016). The goal INR reached was significantly lower in fixed-dose than variable-dose in patients with baseline INR ≥ 4 (RR= 0.78, 95% CI 0.61 to 1.02, p= 0.006), while this result was not significant for patients with baseline INR < 4 (RR= 0.91, 95% CI 0.82 to 1.00, p= 0.055) (Table 2).
Forest plot of the number of goal INR reached in patients receiving fixed-dose 4-PCC comparing with variable-dose strategy, a overall analysis, b sub-group analysis based on weight, c sub-group analysis based on reversal indication, d sub-group analysis based on pre-PCC administration INR (total sample size; fixed-dose = 442, variable-dose = 546). ICH: intracerebral hemorrhage, RR; relative risk, CI: confidence intervals
Secondary Outcomes
Higher number of patients required administration of additional dose of 4-PCC in fixed-dose (41 of 389 [10.5%]) than variable-dose group (15 of 474, [3.2%]; RR= 2.38, 95% CI 1.33 to 4.24, p= 0.003) in nine studies (Supplemental Fig. 1). Non-significant heterogeneity was seen among studies (p-heterogeneity = 0.478, I2= 0.0%). In subgroup analysis based on reversal indication, requirement for additional doses of 4-PCC was not statically significant in ICH (p= 0.345) and non-ICH patients (p= 0.762). The number of additional 4-PCC dose requirement was similar in subgroup patient with weight ≥ 80 kg (p= 0.910), baseline INR ≥ 4 (p= 0.067), and baseline INR < 4 (p= 0.112) as shown in Table 2. The number of patient who received concurrent vitamin K did not differ between two groups (RR= 0.99, 95% CI 0.93 to 1.06, p= 0.849).
The overall results of all ten studies revealed a significantly lower total administered cumulative dose of 4-PCC in fixed-dose (mean 1360.4 unit) in comparison to variable-dose (mean 2028.9 unit) (WMD= −629.45 unit, 95% CI −790.31 to −468.59 unit, p <0.001) (Supplemental Fig. 2). Considerable heterogeneity was also observed between studies (p-heterogeneity <0.001, I2= 82.9%). A similar finding was observed in all subgroup analyses (Table 3). Likewise, in overall and subgroup analysis of unit per kilogram of administered 4-PCC dose, total administered unit/kg 4-PCC dose (mean 16.39 unit/kg in fixed and mean 24.7 unit/kg in variable-dose) was significantly lower in fixed-dose (WMD = −7.83 unit/kg, 95% CI −9.71 to −5.96 unit/kg, p <0.001) (p-heterogeneity ˂0.001, I2=78.8%) (Supplemental Fig. 3), as shown in Table 3.
Combined results indicated that there was no significant difference in the required time for goal INR achievement between fixed-dose (mean 190.67 min) and variable-dose (mean 205.87 min) of 4-PCC (WMD = −23.22 min, 95% CI −92.19 to 45.75 min, p= 0.509) (Supplemental Fig. 4) in the analysis of three studies. There was substantial heterogeneity among pooled studies (p-heterogeneity= 0.03, I2= 70.6%). The post 4-PCC administration INR was higher in fixed-dose (mean 1.48) group compared to variable-dose (mean 1.34) among all 10 studies (WMD = 0.15, 95% CI 0.04 to 0.45, p= 0.005) with considerable heterogeneity (p-heterogeneity <0.001, I2 = 79.0%) (Supplemental Fig. 5). On the other hand, the mean post-PCC INR was not significantly different in the subgroup of patients with baseline INR ≥ 4 (p = 0.069) and weight ≥ 80 (p = 0.068) (Table 3).
The order to needle time was significantly lower in fixed-dose (mean 68 min) compared to variable-dose (mean 87.75 min; WMD= −22.50 min, 95% CI −31.88 to −13.12 min, p <0.001) with negligible heterogeneity (p-heterogeneity= 0.517, I2= 0.0%) (Supplemental Fig. 6) (Table 3).
The duration of hospital stay between fixed-dose (mean 8.15 days) and variable-dose group (mean 6.71 days) was not significantly different in the analysis of four studies (WMD= 1.64 days, 95% CI −0.38, 3.66 days, p= 0.112) (Supplemental Fig. 7). No heterogeneity was seen (p-heterogeneity= 0.713, I2=0.0%) (Table 3).
Non-linear Dose-Response Between the Dose of 4-PCC and Primary Outcomes
The non-linear dose-response relationship analysis between 4-PCC administered dose and primary outcomes was conducted, and no specific association was found between 4-PCC administered dose and rate of mortality, rate of a thromboembolic event, and number of goal INR achieved (Fig. 5)
Publication Bias
In this study, we used Egger’s weighted regression test and visual examination of the funnel plot to measure publication bias. The Egger’s regression test was not significant for measured outcomes, including mortality (p= 0.332), thromboembolic event (p= 0.557), number of goal INR achieved (p= 0.097), number of need for additional 4-PCC dose (p= 0.719), total 4-PCC administered dose (p= 0.066 for total unit dose and p= 0.068 for unit/kg dose), required time for INR reversal (p= 0.516), post 4-PCC administration mean INR (p= 0.095), and the mean door-to-needle time (p= 0.364). Visual inspection of funnel plot illustrated no evidence of publication bias among primary outcomes (Fig. 5).
Discussion
Main Findings
The overarching aim of this systematic review and meta-analysis of eligible studies was to compare the fixed-dose versus variable-dose of 4-PCC in VKAs reversal. We found ten studies in which 988 patients received 4-PCC in two dosing strategies (fixed-dose and variable-dose based on the package insert and INR/weight of the patients) for reversal of VKAs in cases of major hemorrhage or urgent surgery. To the best of our knowledge, this is the first meta-analysis to compare the efficacy and safety outcomes of fixed-dose versus variable-dose strategy of 4-PCC for VKAs reversal.
The lower mortality rate was observed in fixed-dose 4-PCC compared to variable-dose strategy in our meta-analysis. A similar result was noticed in some subgroup analyses, including the patient with baseline INR ≥ 4. The comparable mortality rate was seen in both dosing strategies in the analysis of two studies in which only ICH patients were included. Nonetheless, these findings should be evaluated in further studies. Additionally, the risk of TEE in overall and subgroup analysis of two dosing groups did not differ significantly. Although the use of variable-dose 4-PCC is associated with the lower mean value of post 4-PCC INR and the higher likelihood of achieving hemostasis (reached to goal INR after a defined period time, generally after 15–30 min), the time needed to reach goal INR was similar between two groups.
On the other hand, the need for an additional 4-PCC dose was higher in overall analysis in the fixed-dose strategy group, but this was not statistically significant in the subgroup of the patient with INR ≥ 4 or weight ≥ 80 kg or ICH patients. Despite this finding, it should be kept in mind that the total administered dose of 4-PCC based on total IU, and IU/kg was significantly lower in the fixed-dose versus variable-dose. Furthermore, a lower order-to-needle time in the fixed-dose group was reported. Indeed, the required time for preparation, ordering, and start of infusion of 4-PCC was lower in the fixed-dose group. The overall search strategy, results, and conclusion of our systematic review and meta-analysis are presented in Fig. 6.
The efficacy and safety of fixed-dose strategies have been discussed in various clinical studies and review articles. In some studies, no difference was reported in the clinical outcomes between the two dosing strategies [21, 32], while in other studies, lower number of goal INR reached with comparable mortality rate was seen in fixed-dose 4-PCC compared to variable-dose [36, 37]. Varga et al. [38] retrospectively reviewed data of 103 patients who received PCCs for warfarin reversal. They found that 1000 IU fixed-dose strategy was associated with satisfactory clinical response (control of bleeding without requiring additional measures) in 84% of patients. In another retrospective study, Klein et al. [39] reported that 1500 IU 4-PCC successfully reversed median INR in 92% (36 participants) of 39 patients who presented with VKA-related bleeding. No associated thromboembolic event was seen in this report. A systematic review was conducted by Khorsand et al. [14] in 2015 to review the efficacy and clinical outcomes of the all used PCC dosing strategies for VKAs reversal. The fixed-dose strategy was used in only seven studies in this systematic review; however, most of them were not a comparative study. Meanwhile, the authorsy concluded that relatively satisfactory results are obtained with the use of various PCC dosing strategies. Furthermore, lower administered PCC doses were used in the fixed-dose strategy.
Altogether, our study revealed that 4-PCC fixed-dose strategy1000–1500 IU of 4-PCC is a safe, effective, and time-saving strategy for the patients with VKAs-related major bleeding or undergoing the procedure. In contrast, the optimal 4-PCC dosing strategy in patients with VKAs-related ICH is more challenging. ACC guidelines recommended using either INR/weight-based variable dosing or fixed-dose 1500 IU in ICH patients [17]. In our pooled data of ICH patients, no significant difference in the major outcomes (e.g., mortality, hemostasis reversal, etc.) was seen in fixed-dose versus variable-dose. Two studies included only ICH patients, and six studies included ICH patients in their participants. As the mean dose of the 4-PCC in the fixed-dose group in the pooled data of the studies in which ICH patients were included was 1440.5 units, it can be concluded that the recommended dose of 1500 IU 4-PCC in ACC guideline may be suitable in ICH patient. However, the use of fixed-dose in ICH patients should be evaluated in further studies. Use of the upper range of dose or adding a re-dose option (e.g., if INR goal not achieved or in patients with obesity or significantly elevated INR > 7.5 or in ICH patients) is the more prudent strategy and may be considered in selected patients. Besides, in dose-response analysis between primary outcomes and administered 4-PCC dose, no significant correlation was seen. The non-significant growing trend in mortality rate in 4-PCC dose above 1500 IU may be due to the fact that the number of death was numerically greater in the variable-dose group in which higher doses were given.
In conclusion, our results suggest that fixed-dose 4-PCC strategy may be considered for VKAs reversal in the different clinical settings; however, this finding should be interpreted with caution. The conduction of more extensive clinical studies focusing on the efficacy and safety outcomes and the optimal dosing strategy of 4-PCC for the VKAs reversal in the different clinical settings, especially ICH patients, is needed. The PROPER3 study [40], RCT trial that evaluating fixed-dose 4-PCC versus variable-dose for VKA reversal, is currently ongoing and will hopefully provide further information on the efficacy and safety of these dosing regimens.
Strengths and Limitations
The current meta-analysis has some strengths. All of the included studies were comparative and have been performed to compare the fixed-dose to variable-dose of 4-PCC. A variety range of patients, including ICH, ECH, and those in need of urgent procedures, were included. Low publication bias and none to moderate risk of heterogeneity among included studies were observed in findings evaluations. Moreover, we assessed both clinically relevant efficacy and safety outcomes. Subgroup analysis based on the particular situations that may act as a confounding factor was also performed. As with all meta-analysis, there are several limitations to be taken into consideration. Most of the included studies in our analysis were retrospective/prospective cohort designs which mostly did not adjust their results for differences among groups. Additionally, for some outcomes, the cohort studies conflicted with one included RCT. The limitation of dose-response analysis due to the risk of potential aggregation bias, especially in weight-based dosing groups, should be considered. Another limitation of our study was related to the unifying definition of some measured outcomes. For example, our included studies had not used a universal and same INR cutoff for goal INR reached in their studies.
Conclusion and Relevance
To summarize, the use of fixed-dose of 4-PCC in VKAs-related coagulopathy may be associated with the lower mortality rate, less total 4-PCC administered, and the faster start of 4-PCC infusion. The thrombotic events rate, duration of hospital stays, and the time needed to reach goal INR were similar between the two groups. In contrast, the variable-dose has been associated with the more hemostatic reversal. Altogether, the fixed-dose strategy of 4-PCC may be considered for urgent reversal of VKAs, but further well-designed, controlled studies should be conducted focusing on clinical outcomes to determine the optimal dose of 4-PCC for VKAs reversal.
Data Availability
All data generated or analyzed during this study were included in the article.
References
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, et al. Evidence-based management of anticoagulant therapy: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e152S–84S.
De Caterina R, et al. Vitamin K antagonists in heart disease: current status and perspectives (Section III). Position paper of the ESC working group on thrombosis--task force on anticoagulants in heart disease. Thromb Haemost. 2013;110(6):1087–107.
Pirmohamed M. Warfarin: the end or the end of one size fits all therapy? J Personal Med. 2018;8(3):22.
Roetker NS, Lutsey PL, Zakai NA, Alonso A, Adam TJ, MacLehose R. All-cause mortality risk with direct oral anticoagulants and warfarin in the primary treatment of venous thromboembolism. Thromb Haemost. 2018;118(9):1637–45.
Wysowski DK, Nourjah P, Swartz L. Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch Intern Med. 2007;167(13):1414–9.
Bleeding during antithrombotic therapy in patients with atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators. Arch Intern Med. 1996;156(4):409–16.
Hart RG, Tonarelli SB, Pearce LA. Avoiding central nervous system bleeding during antithrombotic therapy: recent data and ideas. Stroke. 2005;36(7):1588–93.
Healey JS, Eikelboom J, Douketis J, Wallentin L, Oldgren J, Yang S, et al. Periprocedural bleeding and thromboembolic events with dabigatran compared with warfarin: results from the Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) randomized trial. Circulation. 2012;126(3):343–8.
Frontera JA, Lewin III JJ, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, et al. Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care. 2016;24(1):6–46.
Polito NB, Kanouse E, Jones CMC, McCann M, Refaai MA, Acquisto NM. Effect of vitamin K administration on rate of warfarin reversal. Transfusion. 2019;59(4):1202–8.
Goldstein JN, Rosand J, Schwamm LH. Warfarin reversal in anticoagulant-associated intracerebral hemorrhage. Neurocrit Care. 2008;9(2):277–83.
Hill R, Han TS, Lubomirova I, Math N, Bentley P, Sharma P. Prothrombin complex concentrates are superior to fresh frozen plasma for emergency reversal of vitamin K antagonists: a meta-analysis in 2606 subjects. Drugs. 2019;79(14):1557–65.
Voils SA, Holder MC, Premraj S, Catlin JR, Allen BR. Comparative effectiveness of 3- versus 4-factor prothrombin complex concentrate for emergent warfarin reversal. Thromb Res. 2015;136(3):595–8.
Khorsand N, Kooistra HAM, van Hest RM, Veeger NJGM, Meijer K. A systematic review of prothrombin complex concentrate dosing strategies to reverse vitamin K antagonist therapy. Thromb Res. 2015;135(1):9–19.
Schwebach AA, Waybright RA, Johnson TJ. Fixed-dose four-factor prothrombin complex concentrate for vitamin K antagonist reversal: does one dose fit all? Pharmacotherapy. 2019;39(5):599–608.
Sarode R, Milling TJ Jr, Refaai MA, Mangione A, Schneider A, Durn BL, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation. 2013;128(11):1234–43.
Tomaselli GF, Mahaffey KW, Cuker A, Dobesh PP, Doherty JU, Eikelboom JW, et al. 2020 ACC Expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2020;76(5):594–622.
Khorsand N, Veeger NJGM, van Hest RM, Ypma PF, Heidt J, Meijer K. An observational, prospective, two-cohort comparison of a fixed versus variable dosing strategy of prothrombin complex concentrate to counteract vitamin K antagonists in 240 bleeding emergencies. Haematologica. 2012;97(10):1501–6.
Appleby N, Groarke E, Crowley M, Wahab FA, McCann AM, Egan L, et al. Reversal of warfarin anticoagulation using prothrombin complex concentrate at 25 IU kg(-1) : results of the RAPID study. Transfus Med. 2017;27(1):66–71.
Makhoul T, Kelly G, Kersten B, Nadler M, Zammit CG, Jones CMC, et al. Incidence of thromboembolic events following administration of four-factor prothrombin complex concentrate (4F-PCC) for oral anticoagulation reversal. Thromb Res. 2020;194:158–64.
Dietrich SK, Mixon M, Holowatyj M, Werth JC, Delgado SA, Mascolo NE, et al. Multi-centered evaluation of a novel fixed-dose four-factor prothrombin complex concentrate protocol for warfarin reversal. Am J Emerg Med. 2020;38(10):2096–100.
Dager WE. Using prothrombin complex concentrates to rapidly reverse oral anticoagulant effects. Ann Pharmacother. 2011;45(7-8):1016–20.
Moher D, Liberati A, Tetzlaff J, Altman DG, for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5.
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12.
Wells GA, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford. 2000.
Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird's methodology to perform multivariate random effects meta-analyses. Stat Med. 2010;29(12):1282–97.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Bitonti MT, Rumbarger RL, Absher RK, Curran LM. Prospective evaluation of a fixed-dose 4-factor prothrombin complex concentrate protocol for urgent vitamin K antagonist reversal. J Emerg Med. 2020;58(2):324–9.
Gilbert BW, Morton L, Huffman JB, Roemer K, Potter A, Cassidy CD, et al. Modified version of the American College of Cardiology's recommendation for low-dose prothrombin complex concentrate is effective for warfarin reversal. Am J Emerg Med. 2020;38(4):806–9.
Dietrich SK, et al. Comparison of 3 different prothrombin complex concentrate regimens for emergent warfarin reversal: PCCWaR study. Ann Pharmacother. 2020;11:1060028020978568.
Scott R, Kersten B, Basior J, Nadler M. Evaluation of fixed-dose four-factor prothrombin complex concentrate for emergent warfarin reversal in patients with intracranial hemorrhage. J Emerg Med. 2018;54(6):861–6.
Elsamadisi P, Cepeda MAG, Yankama T, Wong A, Tran Q, Eche IM. Weight-based dosing versus a fixed-dose regimen of 4-factor prothrombin complex concentrate in obese patients requiring vitamin K antagonist reversal. Am J Cardiovasc Drugs. 2020.
Khorsand N, Veeger NJGM, Muller M, Overdiek JWPM, Huisman W, van Hest RM, et al. Fixed versus variable dose of prothrombin complex concentrate for counteracting vitamin K antagonist therapy. Transfus Med. 2011;21(2):116–23.
Abdoellakhan RA, Miah IP, Khorsand N, Meijer K, Jellema K. Fixed versus variable dosing of prothrombin complex concentrate in vitamin K antagonist-related intracranial hemorrhage: a retrospective analysis. Neurocrit Care. 2017;26(1):64–9.
van Aart L, Eijkhout HW, Kamphuis JS, Dam M, Schattenkerk ME, Schouten TJ, et al. Individualized dosing regimen for prothrombin complex concentrate more effective than standard treatment in the reversal of oral anticoagulant therapy: an open, prospective randomized controlled trial. Thromb Res. 2006;118(3):313–20.
Varga C, al-Touri S, Papadoukakis S, Caplan S, Kahn S, Blostein M. The effectiveness and safety of fixed low-dose prothrombin complex concentrates in patients requiring urgent reversal of warfarin (CME). Transfusion. 2013;53(7):1451–8.
Klein L, Peters J, Miner J, Gorlin J. Evaluation of fixed dose 4-factor prothrombin complex concentrate for emergent warfarin reversal. Am J Emerg Med. 2015;33(9):1213–8.
Abdoellakhan RA, Khorsand N, van Hest RM, Veeger N, ter Avest E, Ypma PF, et al. Randomised controlled trial protocol to evaluate a fixed dose prothrombin complex concentrate against the variable dose in vitamin K antagonist related bleeding (PROPER3). BMJ Open. 2018;8(3):e020764.
Acknowledgements
We would like to thank Dr. Jamal Rahmani for the appropriate conduction of systematic reviews and meta-analysis.
Author information
Authors and Affiliations
Contributions
All authors were responsible for the study conception and design. KM, SY, and MA contributed to database searching, data extraction, assessment of study quality, data analysis and interpretation, and drafting of the manuscript. AT and KM critically evaluated and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to Participate
Not applicable.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 8334 kb)
Rights and permissions
About this article
Cite this article
Mohammadi, K., Yaribash, S., Sani, M.A. et al. Efficacy and Safety of the Fixed-Dose Versus Variable-Dose of 4-PCC for Vitamin K Antagonist Reversal: A Comprehensive Systematic Review and Meta-Analysis. Cardiovasc Drugs Ther 36, 533–546 (2022). https://doi.org/10.1007/s10557-021-07192-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07192-0