Abstract
Cardiovascular complications, including heart failure, hypertension, ischemic syndromes and venous thromboembolism, have been identified in patients treated with anti-cancer drugs. Oxidative stress, mitochondrial dysfunction and DNA synthesis inhibition are considered to be responsible for the cardiotoxicity induced by these agents. Protein quality control (PQC) has 3 major components, including the endoplasmic reticulum (ER), the ubiquitin-proteasome system (UPS) and the autophagy-lysosome system, and participates in protein folding and degradation to maintain protein homeostasis. We have demonstrated that PQC dysfunction is a new causal mechanism for the development of cardiac hypertrophy and failure. Increasing evidence shows that anti-cancer drugs, such as tyrosine kinase inhibitors, proteasome inhibitors, anthracyclines and autophagy inhibitors, cause PQC dysfunction. Here, we provide an overview of the potential role of PQC dysfunction in the development of cardiovascular complications induced by anti-cancer drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because of the progress made in the development of anti-cancer drugs that prolong the lifespans of patients with cancer, cardiovascular complications, such as heart failure, hypertension, ischemic syndromes and venous thromboembolism, have become more prominent in patients undergoing cancer therapy. Thus, the prevention of these complications is newly emerging unmet medical need that must be solved [1].
Protein quality control (PQC) has 3 major components, including the endoplasmic reticulum (ER), the ubiquitin-proteasome system (UPS) and the autophagy-lysosome system, and participates in protein folding and degradation to maintain protein homeostasis. When the functions of these 3 components are disturbed, unfolded or misfolded proteins can accumulate in the cells, which can lead to cell apoptosis [2]. We and others have recently demonstrated that PQC dysfunction is involved in the development of atherosclerosis and cardiac hypertrophy/failure as well as diabetes and neurodegenerative disorders [3–10]. Anti-cancer drugs induce cardiovascular complications via several mechanisms, such as oxidative stress, mitochondrial dysfunction and DNA synthesis inhibition, any of which can potentially cause PQC dysfunction [11, 12]. Furthermore, anti-cancer drugs such as tyrosine kinase inhibitors, proteasome inhibitors, anthracyclines and autophagy inhibitors directly cause PQC dysfunction and, consequently, cardiovascular complications [5, 8, 13, 14]. We provide an overview of 3 major components of PQC and discuss their potential roles in the cardiovascular complications induced by anti-cancer drugs.
The 3 Components of PQC
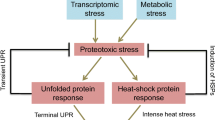
The ER
The ER is the largest membrane-bound organelle in the cell and is the main site of protein folding, lipid synthesis and cellular calcium storage [15]. Certain stimuli, including oxidative stress, ischemia, increased protein synthesis and gene mutations, result in the accumulation of unfolded or misfolded proteins in the ER, a condition referred to as ER stress [16]. When the ER stress is mild, unfolded protein responses (UPRs) are induced to maintain ER homeostasis. Three ER transmembrane sensors, activating transcription factor 6 (ATF6), inositol-requiring enzyme 1 (IRE1), and PKR-like ER kinase (PERK), detect the accumulation of unfolded and misfolded proteins and activate UPR pathways (Fig. 1a). ER stress causes ATF6 translocation from the ER to the Golgi body where it is cleaved by site-1 protease (S1P) and S2P. Subsequently, cleaved ATF6 enters into the nucleus and induces the expression of UPR target genes, including X-box binding protein 1 (XBP1) and 78-kDa glucose-regulated protein (GRP78). Moreover, ER stress leads to IRE1 dimerization and trans-autophosphorylation which mediates the splicing of the mRNA of XBP1. The spliced XBP1 induces the expression of ER stress-related genes, such as the ER chaperone GRP78, thereby reducing ER stress. PERK is also activated by ER stress and activated PERK phosphorylates eukaryotic translation initiation factor (eIF) 2-alpha, which in turn inhibits global protein synthesis, reduces protein loading to the ER and ameliorates ER stress [17] (Fig. 1a).
UPR and ER stress-initiated apoptosis signaling pathways. a Stimuli, such as oxidative stress and Ca2+ disturbance, induce ER stress and cause the accumulation of unfolded or misfolded proteins in the ER. When ER stress is mild, UPR is activated. ATF6, an ER transmembrane sensor, is cleaved at the Golgi and the cleaved ATF6 then translocates to the nucleus and increases the expression of XBP1 and the ER chaperone GRP78. IRE1 activation results in the increases of XBP1 splicing, leading to the induction of the ER chaperone GRP78. PERK activation inhibits protein translation. These UPR pathways cooperatively reduce ER stress. b Severe or prolonged ER stress activates three ER stress-initiated apoptotic signaling pathways: caspase-12, JNK and CHOP. Caspase-12 is cleaved by calpain, caspase-7 and IRE-TRAF2 to induce cell apoptosis. IRE-TRAF2 also activates JNK, resulting in cell apoptosis. CHOP is induced by the PERK-ATF4 signal pathway, which decreases the Bcl2/Bax ratio to induce cell apoptosis
However, when ER stress is severe or prolonged, ER stress-initiated apoptotic signaling pathways, including caspase-12, c-JUN NH2-terminal kinase (JNK), and CCAAT-enhancer-binding protein (C/EBP) homologous protein (CHOP), are activated (Fig. 1b). Caspase-12, which is an apoptotic molecule that locates to the outside of ER membrane, can be activated and cleaved by IRE1-TNF receptor-associated factor 2 (TRAF2), calpain and caspase-7 under severe or prolonged ER stress. Cleaved caspase-12 then activates a downstream apoptotic signaling pathway, resulting in cell apoptosis. JNK phosphorylation is also activated by IRE-TRAF2 in response to ER stress. CHOP expression is induced by ER stress via the PERK-ATF4 pathway. CHOP decreases the anti-apoptotic factor/pro-apoptotic factor ratio (Bcl2/Bax), which leads to cell apoptosis [3, 18]. (Fig. 1b).
We have demonstrated that ER stress is induced in human failing hearts [10]. Furthermore, we also showed that CHOP expression increased in the transition from cardiac hypertrophy to failure due to pressure overload [10] and the ablation of CHOP attenuated the development of heart failure through the decrease in Bcl2/Bax ratio [3]. Interestingly, CHOP expression increased in human vulnerable plaques [4] and the ablation of CHOP attenuates the extent of atherosclerosis in a mouse model [19]. These findings demonstrate that ER stress is important in the development of cardiovascular diseases.
The UPS
Newly synthesized proteins are folded and transported to their sites of activity [17, 20]. However, if the proteins cannot be folded correctly, then they are degraded by UPS to maintain cell homeostasis. Proteins targeted for degradation are ubiquitinated by three enzymes: ubiquitin-activating enzyme (E1), ubiquitin-conjugating enzyme (E2) and ubiquitin ligase (E3). In mammals, the proteasome is the primary protein degradation machinery and consists of one 20S core subunit and two 19S regulatory cap subunits. 19S recognizes the ubiquitinated proteins and transfers them into the catalytic 20S core subunit of the proteasome where the target proteins are degraded [21] (Fig. 2). Because the UPS is the primary selective degradation system in cells, UPS dysfunction is involved in the pathogenesis of numerous human diseases, including cancer, immune-related diseases, cardiovascular diseases and neurodegenerative diseases [22]. Furthermore, increased ubiquitinated proteins were confirmed in hearts of patients with cardiomyopathy [23]. In hearts failing due to pressure overload, cardiomyocyte apoptosis was observed along with depression of proteasome activities and a decrease in the anti-apopototic/ pro-apoptotic protein ratio [5]. Moreover, genetically inhibited and enhanced proteasome activity had detrimental and protective effects in ischemia-reperfusion injury, respectively [24, 25]. These findings indicate that the UPS plays an important role in the development of cardiac diseases.
The Autophagy-Lysosome System
Autophagy is an intracellular degradation system [26]. Targeted cytoplasmic constituents, including proteins, organelles and foreign pathogens, are separated and enclosed within double-membrane vesicles known as the autophagosome. Autophagy-related gene (Atg) 5 and Beclin-1 are required for the initiation and elongation of the autophagosome, respectively [27].The autophagosome then fuses with a lysosome which maintains an acid environment and contains a variety of acid hydrolases to degrade the contents [26] (Fig. 3). The autophagy-lysosome system has a fundamental role in maintaining cellular homeostasis under normal and pathological conditions, such as cancer, neurodegeneration and microbial infection [28]. Increased autophagosome formation in response to stress signals and/or impaired autophagosome clearance due to lysosome inhibition can cause autophagosome accumulation, which has been observed in many diseases, including Alzheimer’s disease, diabetes, atherosclerosis and heart failure [29].
The autophagy-lysosome system. Unfolded or misfolded proteins, damaged organelles and foreign pathogens are isolated and enclosed by double-membrane vesicles known as autophagosomes. These vesicles then fuse with lysosomes, forming autolysosomes. Finally, the contents are degraded by acid hydrolases in the autolysosome
The genetic deletion of Atg5, an essential protein for autophagosome initiation, leads to cardiac dysfunction with increased disorganized sarcomere structure and mitochondrial aggregation in the heart after treatment with pressure overload. These results indicate that the normal function of autophagy is important for maintaining cardiac function against hemodynamic stress [30]. Autophagy activation has also been shown to enhance myocardial injury in response to I/R [31]. Despite the complex role of autophagy in cardiac diseases, increasing evidence suggests that the suppression of autophagy below physiological levels or the induction of autophagy beyond physiological levels causes PQC dysfunction in cardiomyocytes, leading to cardiac dysfunction [30, 32].
PQC Dysfunction and the Cardiovascular Complications Induced by Anti-Cancer Drugs
Because of the substantial advancements in cancer therapy in recent decades, the number of cancer survivors is increasing [33]. Additionally, cardiovascular complications have become a leading cause of morbidity and mortality among these patients [34]. Anti-cancer drugs cause cardiovascular complications via distinct mechanisms, including oxidative stress and mitochondrial dysfunction [35]. 5-fluorouracil can induce oxidative stress by increasing intracellular ROS [36]. Mitoxantrone can induce mitochondrial dysfunction by inhibiting ATP-synthase expression and activity [37]. Although there is no evidence available currently, it is likely that oxidative stress and mitochondrial dysfunction by these anti-cancer drugs may also induce PQC dysfunction. Further investigation will be required to clarify the evidence of PQC dysfunction and the contribution of PQC dysfunction to the development of cardiovascular diseases induced by these anti-cancer drugs.
In addition to these mechanisms, we and others have demonstrated that anti-cancer drugs, such as imatinib and doxorubicin, can directly affect the components of PQC and, consequently, also contribute to the cardiovascular complications induced by these drugs [8, 13]. Here, we provide an overview of the potential role of PQC dysfunction in the development of cardiovascular complications induced by anti-cancer drugs.
Tyrosine Kinase (TK) Inhibitors
TKs are key regulators of normal cellular processes and play a critical role in the progression of many types of cancer. Therefore, TK inhibitors have been developed for cancer therapy [38, 39]. However, several TK inhibitors, such as imatinib and dasatinib, induce cardiac dysfunction in patients receiving them [12].
Imatinib is a specific inhibitor of Abelson oncogene 1 (c-Abl) kinase, a member of the TK enzyme family [40]. Because c-Abl binds to ErbB2 and functions as a protective factor in cardiomyocytes, the inhibition of c-Abl via imatinib can cause significant cardiotoxicity [40–42]. Imatinib is widely used to treat chronic myelogenous leukemia, gastrointestinal stromal tumors and numerous other malignancies [43]. Severe congestive heart failure has been reported in patients treated with imatinib, although its incidence is modest (0.5–1.7%) [13, 44]. The inhibition of c-Abl kinase by imatinib leads to ER enlargement, the activation of an ER transmembrane sensor protein, IRE1, and causes cardiomyocyte apoptosis via JNK activation. Although the potential mechanisms by which c-Abl induces ER stress remains unclear, the gene transfer of an imatinib-resistant mutant of c-Abl largely rescues cardiomyocytes from imatinib-induced death associated with ER stress reduction [13]. In contrast, another study has shown that imatinib induces cardiomyocyte dysfunction by inducing ER stress and inhibiting the fusion of autophagosome and lysosome, regardless of c-Abl inhibition [45]. Although a discrepancy exists between these studies, the cardiac toxicity induced by imatinib is clearly attributable to ER stress or autophagy dysfunction (Fig. 4). Therefore, reducing ER stress and/or autophagy dysfunction might become a new means for cardiac protection in patients receiving imatinib. Moreover, dasatinib, a derivative drug of imatinib, has also been reported to cause cardiac dysfunction [46]. Although the underlying mechanism has not been clarified, PQC dysfunction has the possibility to play a role in dasatinib-induced cardiac dysfunction as imatinib, because its structure is similar to that of imatinib.
Imatinib-induced cardiomyopathy. Imatinib activates IRE1 by inhibiting c-Abl and induces cardiomyocyte apoptosis through the JNK signaling pathway. In addition, imatinib can accumulate in lysosomes and inhibit the fusion of autophagosomes and lysosomes, which increases ROS production. These two mechanisms could be responsible for cardiomyocyte apoptosis induced by imatinib
Proteasome Inhibitors
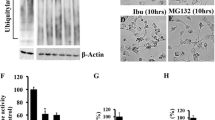
Proteasome inhibitors hinder the degradation of unfolded or misfolded proteins, thereby causing the accumulation of these proteins. They induce cancer cell apoptosis by increasing the pro-apoptotic/anti-apoptotic factor ratio [47]. Many types of tumor cells are more sensitive to proteasome inhibitors than non-tumorigenic cells, because tumor cells have higher proteasome activity and nuclear ubiquitin-conjugated proteins than normal cells [47, 48]. However, the UPS also plays a fundamental role in maintaining cellular homeostasis in cardiomyocytes. We and others have demonstrated that proteasome inhibition induces the death of cultured cardiomyocytes through the induction of ER stress and the accumulation of pro-apoptotic proteins, such p53 and Bax [5, 7].
Bortezomib, an inhibitor of the 20S proteasome, has been clinically used to treat multiple myeloma (MM) and mantle cell lymphoma [49]. MM cells produce an abnormal amount of antibodies and may, thus, potentially place a load on the ER. MM cells are susceptible to bortezomib-induced apoptosis [50], because bortezomib inhibits the activity of proteasome and causes unfolded or misfolded protein accumulation to induce ER stress-initiated apoptosis [51]. In addition, bortezomib can post-translationally regulate the protein levels of key molecules, and many molecules, such as Kruppel-like factor 9, I-κB and the Bcl2 family members, have been involved in the growth suppression and the apoptosis of cancer cells [48, 52]. Bortezomib also impacts the cardiovascular system [53]. Previous studies have demonstrated that bortezomib activates the calcineurin-nuclear factor of activated T-cells (NFAT) pathway by decreasing the degradation of calcineurin A, leading to left ventricular dilatation, hypertrophy and cardiac dysfunction [54]. We have reported that MG132, which is another proteasome inhibitor, directly inhibited unfolded or misfolded protein degradation and caused ER stress in cardiomyocytes, inducing cardiomyocyte apoptosis via the CHOP-dependent pathway. The overexpression of ER chaperone GRP78 attenuated cardiomyocyte death induced by proteasome inhibition, indicating that ER stress-initiated cardiomyocyte apoptosis plays an important role in the bortezomib-induced cardiac dysfunction [7]. These findings indicate that bortezomib causes the ER stress and increases the accumulation of hypertrophic and pro-apoptotic proteins, both of which are involved in the development of cardiac dysfunction (Fig. 5). Moreover, proteasome inhibition increased the accumulation of pro-apoptotic proteins, such p53 and Bax, which caused cardiomyocyte apoptosis and contributed to the cardiac dysfunction induced by pressure overload [5]. In addition, carfilzomib has also been reported to induce cardiac dysfunction [55]. Therefore, the use of proteasome inhibitors should take into account the cardiotoxicity in patients receiving them.
Bortezomib-induced cardiomyopathy. Bortezomib-induced proteasome inhibition decreases pro-apoptotic protein degradation, resulting in cardiomyocyte apoptosis. Bortezomib-induced proteasome inhibition causes unfolded or misfolded protein accumulation, which induces the ER stress-initiated apoptotic signal CHOP and cardiomyocyte apoptosis. Bortezomib-induced proteasome inhibition increases the amount of calcineurin A by suppressing its degradation, and increased calcineurin A participates in the pathogenesis of cardiac hypertrophy and dysfunction
Doxorubicin
Doxorubicin, a member of the anthracycline family, is widely used in cancer therapy. However, its clinical application is limited by its cardiotoxicity. Doxorubicin has been shown to causes oxidative stress, sarcomere damage, topoisomerase inhibition and mitochondrial dysfunction, which lead to cardiomyocytes damage and death [56]. Doxorubicin has been observed to disturb Ca2+ homeostasis by inhibiting the expression of SERCA2 and, consequently, leads to Ca2+ depletion in the ER [57]. Because Ca2+ is essential for proper protein folding and transport, the ER Ca2+ depletion induced by doxorubicin can induce ER stress and PQC dysfunction. Furthermore, doxorubicin increases the expression of E3 ligase and proteasome activity in cardiomyocytes, leading to the enhanced degradation of anti-apoptotic factors and cell apoptosis [58]. A recent study shows that doxorubicin inhibits autophagy in cardiomyocytes and that the accumulation of autolysosomes leads to increased ROS production and cardiac injury [59] (Fig. 6).
Doxorubicin-induced cardiomyopathy. Although doxorubicin induces ER stress by generating ROS and inhibiting SERCA2, doxorubicin cannot induce the expression of ER chaperone GRP78 that protects the cardiomyocyte, which further augments ER stress and cardiomyocyte apoptosis via caspase-12-dependent pathways. The cardiac specific overexpression of GRP78 or supplementation with 4-PBA, a chemical ER chaperone, can rescue doxorubicin-induced cardiomyocyte death. Moreover, doxorubicin activates proteasome activity and increases the degradation of anti-apoptotic factors, leading to cardiomyocyte apoptosis. Doxorubicin also induces cardiomyocyte apoptosis by inhibiting autophagy function and increasing ROS generation. Taken together, doxorubicin potentially affects all 3 components of PQC
In addition, we have demonstrated that doxorubicin induces ER stress by activating the transcription factor ATF6 in cardiomyocytes [8]. However, doxorubicin suppresses the expression of the genes downstream of ATF6 and does not induce the ER chaperone GRP78 (Fig. 6). Because GRP78 plays a protective role in the response to ER stress, the failure of GRP78 induction augments doxorubicin-induced cardiotoxicity. As a result, doxorubicin induces cardiomyocyte apoptosis by activating caspase-12, an ER stress-initiated apoptotic signaling pathway. Because ER chaperones can promote protein folding and reduce ER stress, the cardiac-specific overexpression of GRP78 and administration of 4-phenylbutyrate (4-PBA), a chemical ER chaperone to mimic the function of GRP78 [60], suppresses caspase-12 activation and reduces cardiomyocyte apoptosis, alleviating doxorubicin-induced cardiac dysfunction [8] (Fig. 6). Moreover, 4-PBA has been clinically used to treat urea cycle disorders [61]. Thus, 4-PBA could be applied in the context of PQC dysfunction to treat the cardiac complications induced by anti-cancer drugs. These findings demonstrate that the dysfunction of 3 components of PQC is involved in doxorubicin-induced cardiotoxicity and that the alleviation of PQC dysfunction may attenuate cardiac dysfunction in patients receiving doxorubicin.
Autophagy Inhibitors
Autophagy removes unfolded or misfolded proteins, protein aggregates and damaged organelles through lysosomal degradation [62]. Because autophagy is a mechanism associated with the degradation of unfolded or misfolded proteins, its dysfunction can cause the accumulation of unfolded or misfolded proteins, resulting in ER stress. Previous studies reported that the inhibition of autophagy by pharmacological agents or the knockdown of autophagy-related gene Beclin-1 increased the ER stress levels and apoptotic cell death [63].
Chloroquine has long been used to treat or prevent malaria [64]. However, recent studies have suggested that the use of chloroquine in combination with other chemotherapeutic agents may enhance therapeutic effects [65, 66]. One possible mechanism for the anti-cancer effect of chloroquine is related to its enhancement of the membrane permeabilization of lysosommes [14]. Chloroquine can enter the lysosome and becomes protonated because of the low pH within the lysosome. The accumulation of the protonated form of chloroquine within the lysosome leads to less acidic conditions and, thereby, decreased acid hydrolase activity and lysosomal function [14]. Lysosome dysfunction can suppress the fusion of the autophagosome and lysosome with increased ROS production, leading to cardiac injury and dysfunction [59] (Fig. 7). Clinical trials of chloroquine have been conducted for glioblastoma and metastatic melanoma treatment [67, 68]. However, the use of chloroquine can induce cardiac dysfunction and its discontinuation dramatically improved cardiac function [69]. Furthermore, chloroquine caused cardiomyocyte apoptosis and cardiac dysfunction via ROS generation in a rat model of pressure overload hypertrophy [70]. Therefore, we need careful monitoring of cardiac dysfunction when patients are receiving chloroquine.
Chloroquine-induced cardiomyopathy. Chloroquine can enter the lysosome to enhance the membrane permeabilization of the lysosome. In the lysosome, accumulated chloroquine increases the pH, thereby decreasing acid hydrolase activity and lysosomal function. Lysosomal dysfunction suppresses the fusion of autophagosome and lysosome, leading to cardiomyocyte apoptosis
Conclusions
Although many challenges have been addressed, cardiovascular complications remain a major problem for cancer survivors [71, 72]. Anti-cancer drugs can induce PQC dysfunction directly by targeting the component of PQC and indirectly by oxidative stress, mitochondrial dysfunction and the inhibition of DNA synthesis (Table 1). Although further investigations are required to clarify the potential role of PQC dysfunction in the development of cardiovascular complications induced by anti-cancer drugs, the targeted alleviation of PQC dysfunction in cardiovascular system or cancer-specific delivery of PQC-disturbing anti-cancer drugs may be a promising novel approach to prevent the cardiovascular complications in patients receiving cancer therapy.
References
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53:2231–47.
Wang ZV, Hill JA. Protein quality control and metabolism: bidirectional control in the heart. Cell Metab. 2015;21:215–26.
Fu HY, Okada K, Liao Y, et al. Ablation of C/EBP homologous protein attenuates endoplasmic reticulum-mediated apoptosis and cardiac dysfunction induced by pressure overload. Circulation. 2010;122:361–9.
Myoishi M, Hao H, Minamino T, et al. Increased endoplasmic reticulum stress in atherosclerotic plaques associated with acute coronary syndrome. Circulation. 2007;116:1226–33.
Tsukamoto O, Minamino T, Okada K, et al. Depression of proteasome activities during the progression of cardiac dysfunction in pressure-overloaded heart of mice. Biochem Biophys Res Commun. 2006;340:1125–33.
Minamino T, Komuro I, Kitakaze M. Endoplasmic reticulum stress as a therapeutic target in cardiovascular disease. Circ Res. 2010;107:1071–82.
Fu HY, Minamino T, Tsukamoto O, et al. Overexpression of endoplasmic reticulum-resident chaperone attenuates cardiomyocyte death induced by proteasome inhibition. Cardiovasc Res. 2008;79:600–10.
Fu HY, Sanada S, Matsuzaki T, et al. Chemical endoplasmic reticulum chaperone alleviates doxorubicin-induced cardiac dysfunction. Circ Res. 2016;118:798–809.
Balchin D, Hayer-Hartl M, Hartl FU. In vivo aspects of protein folding and quality control. Science. 2016;353:aac4354.
Okada K, Minamino T, Tsukamoto Y, et al. Prolonged endoplasmic reticulum stress in hypertrophic and failing heart after aortic constriction: possible contribution of endoplasmic reticulum stress to cardiac myocyte apoptosis. Circulation. 2004;110:705–12.
Cross MJ, Berridge BR, Clements PJ, et al. Physiological, pharmacological and toxicological considerations of drug-induced structural cardiac injury. Br J Pharmacol. 2015;172:957–74.
Mellor HR, Bell AR, Valentin JP, Roberts RR. Cardiotoxicity associated with targeting kinase pathways in cancer. Toxicol Sci. 2011;120:14–32.
Kerkelä R, Grazette L, Yacobi R, et al. Cardiotoxicity of the cancer therapeutic agent imatinib mesylate. Nat Med. 2006;12:908–16.
Yoon YH, Cho KS, Hwang JJ, Lee SJ, Choi JA, Koh JY. Induction of lysosomal dilatation, arrested autophagy, and cell death by chloroquine in cultured ARPE-19 cells. Invest Ophthalmol Vis Sci. 2010;51:6030–7.
Dobson CM. Protein folding and misfolding. Nature. 2003;426:884–90.
Hetz C. The unfolded protein response: controlling cell fate decisions under ER stress and beyond. Nat Rev Mol Cell Biol. 2012;13:89–102.
Walter P, Ron D. The unfolded protein response: from stress pathway to homeostatic regulation. Science. 2011;334:1081–6.
Tabas I, Ron D. Integrating the mechanisms of apoptosis induced by endoplasmic reticulum stress. Nat Cell Biol. 2011;13:184–90.
Thorp E, Li G, Seimon TA, Kuriakose G, Ron D, Tabas I. Reduced apoptosis and plaque necrosis in advanced atherosclerotic lesions of Apoe−/− and Ldlr−/− mice lacking CHOP. Cell Metab. 2009;9:474–81.
Tsukamoto O, Minamino T, Kitakaze M. Functional alterations of cardiac proteasomes under physiological and pathological conditions. Cardiovasc Res. 2010;85:339–46.
Weissman AM, Shabek N, Ciechanover A. The predator becomes the prey: regulating the ubiquitin system by ubiquitylation and degradation. Nat Rev Mol Cell Biol. 2011;12:605–20.
Wang X, Li S. Protein mislocalization: mechanisms, functions and clinical applications in cancer. Biochim Biophys Acta. 1846;2014:13–25.
Powell SR, Herrmann J, Lerman A, Patterson C, Wang X. The ubiquitin-proteasome system and cardiovascular disease. Prog Mol Biol Transl Sci. 2012;109:295–346.
Tian Z, Zheng H, Li J, Li Y, Su H, Wang X. Genetically induced moderate inhibition of the proteasome in cardiomyocytes exacerbates myocardial ischemia-reperfusion injury in mice. Circ Res. 2012;111:532–42.
Li J, Horak KM, Su H, Sanbe A, Robbins J, Wang X. Enhancement of proteasomal function protects against cardiac proteinopathy and ischemia/reperfusion injury in mice. J Clin Invest. 2011;121:3689–700.
Mizushima N. Autophagy: process and function. Genes Dev. 2007;21:2861–73.
Mizushima N. The pleiotropic role of autophagy: from protein metabolism to bactericide. Cell Death Differ. 2005;12(Suppl 2):1535–41.
Yang Z, Klionsky DJ. Eaten alive: a history of macroautophagy. Nat Cell Biol. 2010;12:814–22.
Levine B, Kroemer G. Autophagy in the pathogenesis of disease. Cell. 2008;132:27–42.
Nakai A, Yamaguchi O, Takeda T, et al. The role of autophagy in cardiomyocytes in the basal state and in response to hemodynamic stress. Nat Med. 2007;13:619–24.
Hariharan N, Zhai P, Sadoshima J. Oxidative stress stimulates autophagic flux during ischemia/reperfusion. Antioxid Redox Signal. 2011;14:2179–90.
Matsui Y, Takagi H, Qu X, et al. Distinct roles of autophagy in the heart during ischemia and reperfusion: roles of AMP-activated protein kinase and Beclin 1 in mediating autophagy. Circ Res. 2007;100:914–22.
Siegel R, Naishadham D, Jemal A, et al. CA Cancer J Clin. 2012;62:10–29.
Lenneman CG, Sawyer DB. Cardio-oncology: an update on cardiotoxicity of cancer-related treatment. Circ Res. 2016;118:1008–20.
Albini A, Pennesi G, Donatelli F, Cammarota R, De Flora S, Noonan DM. Cardiotoxicity of anticancer drugs: the need for cardio-oncology and cardio-oncological prevention. J Natl Cancer Inst. 2010;102:14–25.
Lamberti M, Porto S, Marra M, et al. 5-fluorouracil induces apoptosis in rat cardiocytes through intracellular oxidative stress. J Exp Clin Cancer Res. 2012;31:60.
Rossato LG, Costa VM, Vilas-Boas V, et al. Therapeutic concentrations of mitoxantrone elicit energetic imbalance in H9c2 cells as an earlier event. Cardiovasc Toxicol. 2013;13:413–25.
Gschwind A, Fischer OM, Ullrich A. The discovery of receptor tyrosine kinases: targets for cancer therapy. Nat Rev Cancer. 2004;4:361–70.
Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9:28–39.
Goldman JM, Melo JV. Chronic myeloid leukemia--advances in biology and new approaches to treatment. N Engl J Med. 2003;349:1451–64.
Belmonte F, Das S, Sysa-Shah P, et al. ErbB2 overexpression upregulates antioxidant enzymes, reduces basal levels of reactive oxygen species, and protects against doxorubicin cardiotoxicity. Am J Physiol Heart Circ Physiol. 2015;309:H1271–80.
Saad SY, Alkharfy KM, Arafah MM. Cardiotoxic effects of arsenic trioxide/imatinib mesilate combination in rats. J Pharm Pharmacol. 2006;58:567–73.
Stegmeier F, Warmuth M, Sellers WR, Dorsch M. Targeted cancer therapies in the twenty-first century: lessons from imatinib. Clin Pharmacol Ther. 2010;87:543–52.
Chen ZI, Ai DI. Cardiotoxicity associated with targeted cancer therapies. Mol Clin Oncol. 2016;4:675–81.
Hu W, Lu S, McAlpine I, et al. Mechanistic investigation of imatinib-induced cardiac toxicity and the involvement of c-Abl kinase. Toxicol Sci. 2012;129:188–99.
Shah NP, Wallis N, Farber HW, et al. Clinical features of pulmonary arterial hypertension in patients receiving dasatinib. Am J Hematol. 2015;90:1060–4.
Adams J. The proteasome: a suitable antineoplastic target. Nat Rev Cancer. 2004;4:349–60.
Li B, Dou QP. Bax degradation by the ubiquitin/proteasome-dependent pathway: involvement in tumor survival and progression. Proc Natl Acad Sci U S A. 2000;97:3850–5.
Dou QP, Zonder JA. Overview of proteasome inhibitor-based anti-cancer therapies: perspective on bortezomib and second generation proteasome inhibitors versus future generation inhibitors of ubiquitin-proteasome system. Curr Cancer Drug Targets. 2014;14:517–36.
Hideshima T, Richardson P, Chauhan D, et al. The proteasome inhibitor PS-341 inhibits growth, induces apoptosis, and overcomes drug resistance in human multiple myeloma cells. Cancer Res. 2001;61:3071–6.
Ri M. Endoplasmic-reticulum stress pathway-associated mechanisms of action of proteasome inhibitors in multiple myeloma. Int J Hematol. 2016;104:273–80.
Oda E, Ohki R, Murasawa H, et al. Noxa, a BH3-only member of the Bcl-2 family and candidate mediator of p53-induced apoptosis. Science. 2000;288:1053–8.
Enrico O, Gabriele B, Nadia C, et al. Unexpected cardiotoxicity in haematological bortezomib treated patients. Br J Haematol. 2007;138:396–7.
Tang M, Li J, Huang W, et al. Proteasome functional insufficiency activates the calcineurin-NFAT pathway in cardiomyocytes and promotes maladaptive remodelling of stressed mouse hearts. Cardiovasc Res. 2010;88:424–33.
Rosenthal A, Luthi J, Belohlavek M, et al. Carfilzomib and the cardiorenal system in myeloma: an endothelial effect? Blood Cancer J. 2016;6:e384.
Sawyer DB, Peng X, Chen B, Pentassuglia L, Lim CC. Mechanisms of anthracycline cardiac injury: can we identify strategies for cardioprotection? Prog Cardiovasc Dis. 2010;53:105–13.
Arai M, Yoguchi A, Takizawa T, et al. Mechanism of doxorubicin-induced inhibition of sarcoplasmic reticulum Ca(2+)-ATPase gene transcription. Circ Res. 2000;86:8–14.
An J, Li P, Li J, Dietz R, Donath S. ARC is a critical cardiomyocyte survival switch in doxorubicin cardiotoxicity. J Mol Med (Berl). 2009;87:401–10.
Li DL, Wang ZV, Ding G, et al. Doxorubicin blocks cardiomyocyte autophagic flux by inhibiting lysosome acidification. Circulation. 2016;133:1668–87.
Kubota K, Niinuma Y, Kaneko M, et al. Suppressive effects of 4-phenylbutyrate on the aggregation of Pael receptors and endoplasmic reticulum stress. J Neurochem. 2006;97:1259–68.
Guha M. Urea cycle disorder drug approved. Nat Biotechnol. 2013;31:274.
Rubinsztein DC. The roles of intracellular protein-degradation pathways in neurodegeneration. Nature. 2006;443:780–6.
Ding WX, Ni HM, Gao W, et al. Differential effects of endoplasmic reticulum stress-induced autophagy on cell survival. J Biol Chem. 2007;282:4702–10.
Price RN, von Seidlein L, Valecha N, Nosten F, Baird JK, White NJ. Global extent of chloroquine-resistant plasmodium vivax: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:982–91.
Amaravadi RK, Lippincott-Schwartz J, Yin XM, et al. Principles and current strategies for targeting autophagy for cancer treatment. Clin Cancer Res. 2011;17:654–66.
Kimura T, Takabatake Y, Takahashi A, Isaka Y. Chloroquine in cancer therapy: a double-edged sword of autophagy. Cancer Res. 2013;73:3–7.
Rosenfeld MR, Ye X, Supko JG, et al. A phase I/II trial of hydroxychloroquine in conjunction with radiation therapy and concurrent and adjuvant temozolomide in patients with newly diagnosed glioblastoma multiforme. Autophagy. 2014;10:1359–68.
Rangwala R, Leone R, Chang YC, et al. Phase I trial of hydroxychloroquine with dose-intense temozolomide in patients with advanced solid tumors and melanoma. Autophagy. 2014;10:1369–79.
Bae SM, Jung HO, Ihm SM, et al. Hydroxychloroquine-induced cardiomyopathy that presented as pulmonary hypertension: a newly noted complication. Cardiology. 2012;123:197–200.
Chaanine AH, Gordon RE, Nonnenmacher M, Kohlbrenner E, Benard L, Hajjar RJ. High-dose chloroquine is metabolically cardiotoxic by inducing lysosomes and mitochondria dysfunction in a rat model of pressure overload hypertrophy. Physiol Rep. 2015.
Bloom MW, Hamo CE, Cardinale D, et al. Cancer therapy-related cardiac dysfunction and heart failure: part 1: definitions, pathophysiology, risk factors, and imaging. Circ Heart Fail. 2016;9:e002661.
Hamo CE, Bloom MW, Cardinale D, et al. Cancer therapy-related cardiac dysfunction and heart failure: part 2: prevention, treatment, guidelines, and future directions. Circ Heart Fail. 2016;9:e002843.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No disclosure.
Conflict of Interest
YS and TM received research grant from Takeda Pharmaceutical Company Limited., Novartis Pharma K. K., Pfizer Japan Inc., Kyowa Hakko Kirin Co., Ltd., and Ono Pharmaceutical CO., Ltd. FH, MM, NA and MH have no disclosures.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Fu, H.Y., Mukai, M., Awata, N. et al. Protein Quality Control Dysfunction in Cardiovascular Complications Induced by Anti-Cancer Drugs. Cardiovasc Drugs Ther 31, 109–117 (2017). https://doi.org/10.1007/s10557-016-6709-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-016-6709-7