Abstract
Pancreatic cancer (PC) is assumed to be an intimidating and deadly malignancy due to being the leading cause of cancer-led mortality, predominantly affecting males of older age. The overall (5 years) survival rate of PC is less than 9% and is anticipated to be aggravated in the future due to the lack of molecular acquaintance and diagnostic tools for its early detection. Multiple factors are involved in the course of PC development, including genetics, cigarette smoking, alcohol, family history, and aberrant epigenetic signatures of the epigenome. In this review, we will mainly focus on the genetic mutations and epigenetic signature of PC. Multiple tumor suppressor and oncogene mutations are involved in PC initiation, including K-RAS, p53, CDKN2A, and SMAD4. The mutational frequency of these genes ranges from 50 to 98% in PC. The nature of mutation diagnosis is mostly homozygous deletion, point mutation, and aberrant methylation. In addition to genetic modification, epigenetic alterations particularly aberrant hypermethylation and hypomethylation also predispose patients to PC. Hypermethylation is mostly involved in the downregulation of tumor suppressor genes and leads to PC, while multiple genes also represent a hypomethylation status in PC. Several renewable drugs and detection tools have been developed to cope with this aggressive malady, but all are futile, and surgical resection remains the only choice for prolonged survival if diagnosed before metastasis. However, the available therapeutic development is insufficient to cure PC. Therefore, novel approaches are a prerequisite to elucidating the genetic and epigenetic mechanisms underlying PC progression for healthier lifelong survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Pancreatic cancer (PC) is considered the most devastating and deadliest among all cancer types due to a lack of investigative approaches, masked anatomical positions, and deadly characteristics. PC is recognized as the seventh most occurring cancer in the world, while in the USA, PC is placed in the third position due to its leading cancer mortality [1]. According to the American Cancer Society 2019, approximately 56,770 (3%) new cases of PC came under observation, of which 29,940 were male and 26,830 were female. The mortalities are also estimated to include 45,750 patients, of whom 23,800 were males and 21,950 were females, surpassing those of breast cancer (3490 cases). Moreover, based on estimated values, by 2030, PC will be regarded as the second leading cause of cancer-related mortality [1,2,3]. The incidence and mortality rate of PC have remained constant over the last four decades, while no substantial improvement has been made. Among all the major cancers, PC has the highest rate of mortality. Approximately 91% of pancreatic cancer patients of all stages die within 5 years of diagnosis, while only 9% of patients have the chance to survive over 5 years. There are very limited options available for PC treatment, but none of them is effective in prolonging the chance of survival and quality of life. Treatment seldom results in a complete cure, and only < 20% of PC patients are considered for surgery because of metastasis [2].
The incidence ratio of pancreatic cancer is much higher in developed countries, and a significant burden of pancreatic cancer frequency is tolerated by Europe only. Accuracy of data could be achieved by the application of more accurate diagnostic procedures and prognostic approaches in developed countries [4]. In 2008, Europe carried only approximately one-ninth of the world population, but its incidence of pancreatic cancer was approximately one-quarter of the total [5]. The accuracy of data regarding the incidence and mortality rate of PC in Europe is indispensable for evaluating the load of cancer and the outcomes of prophylactic measures and planning and for budgeting for the diagnosis and treatment of PC at local and national levels [6]. At present, due to the limited availability of PC treatment choices, the only possible curative approach for PC is surgical removal of the pancreas, which can extend the survival chance of patients to over 5 years from diagnosis [6, 7]. Conversely, due to the progression and occurrence of metastasis before diagnosis, resection of the tumor is not considered or supported in 80 to 90% of patients [6] because of the uncertainty of the long-term endurance of PC patients [7]. However, some new therapeutic approaches have recently been evaluated, and it is anticipated that chemotherapy may have a positive and effective impact on the overall survival extension of PC patients if suggested after the surgical resection of pancreatic tumors before metastasis occurs [8].
Although pancreatic cancer is a complex malady with multiple factors involved in its initiation and progression, family history [9] and cigarette smoking are the dominant factors [10]. The two most common types of pancreatic cancer are pancreatic adenocarcinoma and pancreatic neuroendocrine tumor (PanNET). Pancreatic adenocarcinoma accounts for 85% of cases and originates from the exocrine part of the pancreas, while PanNET has less than a 5% chance of occurrence, but its tissue specificity is the endocrine part of the pancreas [11]. The prognosis of pancreatic adenocarcinoma is abysmal, and even if diagnosed, the survival chance of 1 year is only 24%, while 9% of patients have a survival chance over 5 years [12]. Pancreatic cancer is categorized into four types based on the clinical representation of the tumor stage. Type I is a nonmetastatic and resectable tumor. If no metastasis occurs and tumors grow up to 2 cm, it is regarded as IA, and if it is more than 2 cm in size but does not exceed 4 cm, it is labeled IB. Type II is locally metastatic and resectable, with tumors of more than 4 cm metastasized to the nearby tissue. Type III is metastatic regionally and nonresectable. The tumor grows into the surrounding tissue, including lymph nodes, nerves, and blood vessels, but not into the distal parts of the body. Type IV involves systemic metastasis, in which cancer evenly spreads throughout the body. All endocrine or exocrine pancreatic cancers have a poor prognosis, even at very late stages of progression, which are stages III and IV, compared to PanNETs because of a lack of symptoms and, if not treated with surgical resection, may influence the survival chance of patients [13,14,15] (Table 1).
Nevertheless, during tumor progression, some nonspecific manifestations have been observed, including weight loss, abdominal pain, light-colored stools, fatigue, and jaundice [16]. All currently available diagnostic procedures are highly nonspecific and unable to diagnose pancreatic cancer at its initial phase [13]. Chemotherapy and surgical resection can be used as therapeutic choices to improve the quality of life and somewhat extend life expectancy; however, a cure for the advance stage is still indefinite [17].
2 PDAC stroma and immune landscape
2.1 PDAC stroma
The microenvironment of PDAC is composed of condensed desmoplastic stroma and cancer-associated fibroblasts (CAFs). CAF cells are characterized as an important cellular population of the stroma. Certainly, the reactions that occur in the stroma are responsible for 50 to 80% of the tumor volume [18]. The role of CAFs in the induction of immunosuppression and PDAC progression has been discussed extensively. However, it has also been reported in various studies that desmoplasia contributes to the promotion of tumor growth, biological aggressiveness, and immune suppression [19,20,21]. Two different studies in a mouse model with PDAC confirmed that targeting the stroma of PC leads to aggressive, while in undifferentiated PC, it displays a protective role [22, 23]. Based on the gene expression analysis results collected from formalin-fixed pancreatic cancer patient samples, the Puleo group devised a new classification system [24]. They confirmed the existing classification based on tumor components, such as classical and basal, and reported four new components of the PDAC stroma, including activated, structurally vascularized, immune, and inflammatory components, representing the PDAC microenvironment heterogeneity [25]. Moffitt and colleagues endorsed these results and further explained that the activated stroma (consisting of an increased fibroblast level) and basal-like tumor subtypes both represent worse prognoses and low immune infiltration compared to other subtypes [24]. All these data reveal a complicated interplay between stromal fibroblasts, tumor cells, and immune cell infiltration, leading to tumor-suppressing or tumor-promoting functions upon specific pathway abrogation or activation.
2.2 PDAC immune landscape
Pancreatic ductal adenocarcinoma has a nonimmunogenic tumor microenvironment consisting of immune cells, fibroblasts, an extracellular matrix, stellate cells, and many other immune-suppressive molecules. The tumor microenvironment of PADCs possesses dense fibrotic stroma with low tumor perfusion, which protects them from antitumor therapeutic agents such as chemotherapy and other approaches that show successful outcomes in other types of cancer [26]. The interaction between the tumor cells and the immune system can be designated in three different phases: the first is the elimination phase, the second is the equilibrium phase, and the third is the escape phase. These phases start working when the immune system recognizes the transformed cells and eliminates them in the early elimination phase. On the other hand, the tumor cells that escaped from the early elimination phase alter their genomic status from a tumor microenvironment that promotes the progression of early lesions. In the last phase, tumor cells signal other immunosuppressor cells, including tumor-associated macrophages (TAMs), marrow-derived suppressor cells (MDSCs), and regulatory T cells (also known as “Treg cells”), which assist in the establishment of an immunosuppressive tumor microenvironment, evading host immune surveillance [27].
The PDAC tumor microenvironment displays a unique and nonimmunogenic surrounding with large amount of immunosuppressive cell infiltration, including Treg MDSCs and high infiltrations of carcinoma-associated fibroblast cells (CAFs), which results in an enhanced fibrotic response due to collagen deposition [28, 29]. The PDAC stroma is very dense and composed of pancreatic stellate cells, an extracellular matrix (ECM), myofibroblasts, fibroblasts, growth factors, cytokines, and a variety of immune cells that predispose patients to promoted initiation, metastasis, and proliferation of tumors via intricate interactions [30]. Pancreatic stellate cells are present in the surrounding vicinity of pancreatic glands and synthesize a variety of proteins, including matrix metalloproteinase (MMP), matrix proteins, and matrix metalloproteinase inhibitors, which regulate extracellular matrix turnover [31]. Multiple factors are involved in the activation of PSCs, including oxidant stress, proinflammatory cytokines, hyperglycemia, hypoxia, and enlarged interstitial pressure [32]. PSCs activated via various factors further promote pancreatic cancer cell growth, proliferation, and invasion potential while ceasing apoptosis [33, 34].
Fibroblasts that are activated in the TME are known as CAFs and are predominantly found in the PDAC stroma, with multiple subtypes having diverse functionalities. The heterogeneity in subgroups makes it very challenging to target fibroblasts in the regulation of the TME [35]. Inflammatory CAFs and myofibroblast CAFs are the two CAFs most commonly found in PDAC; however, a new population was also recognized through RNA single-cell sequencing, which is known as antigen-presenting CAFs [36]. It has been reported that some CAFs are inhibitory, while some CAFs promote cancer severity, but most CAFs enhance PDAC progression and minimize overall survival [37]. The myeloid cells of the tumor create an environment that not only halts the function and proliferation of T cells but also encourages the growth of the tumor by promoting angiogenesis, cancer stemness, metastasis, and epithelial to mesenchymal transition (EMT) [38]. Tumor-associated macrophages and MDSCs are the most inspected myeloid cells in pancreatic ductal adenocarcinoma [39]. As primary tumor progression occurs, PDAC cells start producing granulocyte-macrophage colony-stimulating factor, resulting in the enhanced accumulation of MDSCs in the TME; however, hypoxia upregulates hypoxia-inducible factor 1 secretion, which is responsible for the recruitment of MDSCs. MDSCs then directly suppress T lymphocytes in the tumor microenvironment [40, 41].
The debate of the presence or the absence of T lymphocytes in PDAC tumors remains understudy in the previous decades. However, some studies have reported the infiltration of T cell subtypes, including CD4+ and CD8+, in PDAC biopsies, but immunohistochemical (IHC) analysis has proposed that human tumors lack CD8+ T cells. On the other hand, the IHC analysis of human pancreatic ductal carcinoma patients indicated that CD8+ and CD4+ T cells were found in most tumors, but T cells with functional activity were seldom perceived [42]. A deep understanding is a prerequisite for the development of more effective stimulation of the T cell response and TME for the better management of pancreatic cancer.
3 Genetic modification in pancreatic cancer
Genetic mutations play a crucial role in maximizing the risk of initiation and progression of pancreatic cancer [43]. More than ten percent (10%) of pancreatic cancer patients diagnosed with pancreatic cancer disease develop essential regulatory tumor suppressor genes due to alterations or mutations [44]. Multiple mutations in the germline are characterized as having an association with hereditary pancreatic cancer, including ATM, APC, CDKN2A, BRCA1, BRCA2, STK11, MLH1, PRSS1, PMS2, PALB2, MSH2, and MSH6 [45, 46]. Pancreatic cancer diagnoses and further evaluations have proven that it has a secure connection with familial cancer syndromes, particularly Peutz-Jeghers syndrome, Lynch syndrome (aka hereditary nonpolyposis colon cancer), hereditary ovarian and breast cancer syndrome, familial adenomatous polyposis, and familial atypical multiple-mole melanoma syndromes. BRCA2 germline alteration corresponds to the highest frequency of known cases of inherited pancreatic carcinomas and accounts for 5 to 17% of familial or hereditary pancreatic cancers [47,48,49]. Another gene, known as PALB2, is recognized as the susceptibility gene for pancreatic cancer, which localizes to and functions in partnership with a BRCA2 gene [50], and it is estimated that familial pancreatic cancer originating from germline mutation accounts for 3% of all pancreatic patients [51, 52].
Furthermore, germline mutations of PRSS1 and STK11 genes result in the onset of hereditary pancreatitis and Peutz-Jeghers syndrome, respectively, while a mutation in CDKN2A is commonly observed in people with familial atypical multiple-mole melanoma. Many genes are mutated in pancreatic cancer, but in this review, we will summarize four commonly mutated genes, p53 [53], CDKN2A [54], SMAD4 [55], and KRAS [56], which have the highest (more than 50%) mutational evidence in pancreatic cancer (Tables 2 and 3), with current available literature.
4 Oncogenic mutation in pancreatic cancer
4.1 KRAS mutation in pancreatic cancer
K-RAS is an oncogene and a member of the guanosine-triphosphate (GTPase) family, which encodes a small 21 kDa protein. It performs the function of molecular switching by changeover between two different states [65]. The active state is achieved when bound to GTP via guanine nucleotide exchange factors (GEFs), and it deactivates when bound to GDP with the help of GTPase-activating proteins (GAPs). Thus, it becomes a bridge between the receptor of membrane-bound growth factors and intracellular signaling pathways. The RAS family consists of three critical genes (N-RAS, H-RAS, and K-RAS), and mutations in any of these genes play a critical role in the initiation of human tumorigenesis. RAS gene mutations have been observed to occur frequently in multiple human tumors [65, 66]. The RAS protein communicates with and accepts signals from different stimuli, including cell stress signals, growth factors, and contact with extracellular stimuli through integrins, ion channels, or receptor tyrosine kinases (RTKs). This activates different cancer-associated pathways, such as the RAF/MEK/ERK and PI3K/PTEN/AKT signaling pathways [65,66,67] (Fig. 1).
K-RAS mutational mechanism in pancreatic cancer. K-RAS is an oncogene, a member of the guanosine-triphosphate (GTPase) family, that performs the function of molecular switching by the changeover in two different states. RAS is activated when bound to the GTP via guanine nucleotide exchange factors (GEFs) and deactivates when bound to the GDP with the help of GTPase-activating proteins (GAPs). Typically, the RAS protein is in an inactive state but activated upon stress condition or mutation due to SNPs in codons G12, G13, and Q61. These mutations in KRAS protein led to the propagation of signals from RAS protein to one to the tumor/oncogenic pathway leading to PC. The left side of the picture illustrates the normal homeostatic mechanism of RAS protein in tissues. The right side of the picture shows a mutation in KRAS protein results in activation of either RAF/MEK/ERK, PI3K/AKT/mTOR, or RALGDS/RAL/RLIP pathway and cause pancreatic cancer
Oncogenic alteration in the K-RAS gene occurs at approximately 30% in almost all mammalian tumors [68]. The frequency of K-RAS oncogene mutations is markedly elevated in pancreatic cancer, accounting for more than 95% (Tables 2 and 3) of mutations due to point mutations in two highly conserved sequences, codon 12 and codon 61, which are hotspots for the highest mutational frequency [69, 70]. Accumulating literature reports that pancreatic adenocarcinoma is the nastiest prognostic tumor and that K-RAS mutation is considered a driver gene in pancreatic adenocarcinoma. The early events of tumor evaluation and patients with chronic pancreatitis displaying K-RAS mutations are considered risk factors that lead to pancreatic adenocarcinoma [71]. Most of the point mutations in K-RAS occur at codon 12, which affect the specificity of the amino acid by replacing the original amino acid with either valine, aspartic acid, or arginine [72]. A retrospective study was conducted on samples taken from 2003 to 2009. In total, 136 pancreatic adenocarcinoma tissue samples were analyzed for K-Ras mutations at multiple codon locations (codons 12, 13, and 61). Out of 136 PC samples, 71 (52.2%) displayed point mutations in K-Ras, with n = 70 and n = 1 for codons 12 and 61, respectively [73]. A study reported that amino acid replacement, such as glutamine, promotes the progression and proliferation of pancreatic cancer by targeting the metabolic pathway regulated by K-Ras [74]. Mutational differences in amino acids also affect the aggressiveness of cancer. For instance, G12S and G12V mutations are regarded as less severe than K-Ras G12A and G12R mutations, which represent worse survival [75, 76].
The poor prognostic measures of PC and K-Ras mutation appear to have a close relationship and are considered to be the main factors in pancreatic tumorigenesis. A worse prognosis has appeared in tumors that are nonresectable and display a mutation in K-Ras. Even the healthy tissues surrounding the tumor after resection represent a shorter life when detected with mutated Ras [72, 77]. A recent study reported the detection of active chromatin in mutated K-Ras and other cancer-related genes in pancreatic juice after surgical removal [78]. Recently, it was reported that K-Ras mutation affects pancreatic cancer progression by upregulating CD137 via two oncogenic pathways, NF-κB and MAPK, through the stimulus of IL-1α involvement, resulting in a disturbance of cancer immunotherapy and body immune function [79]. Nobuyuki and colleagues investigated whether the association between K-Ras mutations in dissected pancreatic tissue margins might be a suitable prognostic factor for pancreatic adenocarcinoma recurrence [80]. The highest mutational frequency of K-Ras in pancreatic adenocarcinoma renders it the most targeted hotspot for therapy, which exhibits promising effects in pancreatic cancer cell lines and mouse models [81].
Nevertheless, inhibiting K-Ras posttranslational alterations in an enzymatic manner, such as with farnesyltransferase inhibitors in a clinical trial, failed to produce fruitful outcomes [82]. The synergistic effect of a histone deacetylase (MPT0E028) inhibitor and MEK inhibitor triggers cell apoptosis in pancreatic cancer tissue, while neratinib is involved in the downregulation of mutant K-Ras signaling and killing of pancreatic cancer/tumor cells, which offers insight for new therapeutic approaches [83, 84]. However, more exploration of the K-Ras oncogene is a prerequisite in normal and malignant pancreatic tissue for the development of alternative therapeutic strategies to cope with this deadly disease.
4.2 Tumor suppressor genes in pancreatic cancer
4.2.1 P53 in pancreatic cancer
Tumor protein 53 (TP53, p53), or antigen NY-CO-13, is a 53 kDa phosphorylated protein and the most widely characterized and studied tumor suppressor gene in cancers. Due to the protective behavior of p53, the cells are safeguarded from severe DNA damage, inhibiting the initiation of cancers in multiple tissues [85]. Jay et al. discovered that a 53 kDa protein is deficient in cells in the resting state but appears to be upregulated in transformed cells and proposed that the p53 protein might be involved in cell cycle regulation [86]. p53 is activated in response to multiple cellular stresses, such as telomere shortening, oncogene activation, DNA damage, nutrient starvation, virus infection, heat shock, pH change, and hypoxia [87]. These factors result in the activation of p53 via a series of posttranslational alterations, which trigger some molecular cascades and determine the fate of cells, such as cellular senescence, cellular apoptosis, cell death, and cell cycle arrest [88] (Fig. 2). Upon activation, the p53 functions as a sequence-specific transcription factor, which results in the transactivation of a number of its downstream target genes involved in the regulations of cellular processes mentioned earlier [88, 89]. Li and colleagues reported that p53 is directly involved in the regulation of more than 3600 genes, such as p53 arresting the cell cycle at the G1 phase by activating the p21 gene, which restrains CDK2 availability for the cell cycle [90, 91]. In addition to the function of the DNA damage response and cell cycle arrest, p53 initiates the process of apoptosis via the redox pathway or reactive oxygen species (ROS) [92] and halts the multiplication of transformed or damaged cells, which can dispose of cancer development [93].
Mechanism of p53 mutation in pancreatic cancer. The p53 is a tumor suppressor gene frequently mutated in PC. The p53 is activated upon receiving multiple cellular stress signals including telomere erosion, oncogenic stress, hypoxia, ribosomal stress, and DNA damage, as shown in the top of the picture. Upon activation, the p53 encourage multiple gene sets and execute the function of DNA repair, cell cycle arrest, apoptosis, autophagy, and senescence. The MDM2 (mouse double minute 2) acts as a negative regulator of p53 and regulates its function. In PC cells, the mutation in the p53 gene frequently occurs due to mutation on codons 35, 105, 133, 213, 258, and 299 (as shown in the figure). The mutation resulted in blockage of the propagation of the signal from p53 to the sets of genes and failed in performing the tumor suppressor function and the cancer cells proliferate in an uncontrolled fashion. However, a new compound named PRIMA-1 has the ability to restore (shift transformation) the wild-type function of mutated p53 as shown in the figure
P53 is also recognized as a commonly altered gene in pancreatic adenocarcinoma and accounts for 40–75% of mutations [94] (Tables 2 and 3). Mutation in p53 at the germline level leads to Li-Fraumeni syndrome, which is also associated with and elevates the menace of pancreatic adenocarcinomas, such as via p53 inactivation, which leads to pancreatic cancer [95]. Unlike oncogenic K-Ras activation, the mutation of p53 during tumor development characterizes the later stage [96]. Because of the tumor suppressor function of P53, its mutation has been investigated in some preclinical studies. Joseph and colleagues analyzed the formalin-fixed paraffin tissue of pancreatic patients for p53 mutation and reported that 19 (40%) out of 48 samples displayed mutations in p53 and nuclear staining [97]. Other groups have reported that a total of 27 patient samples of pancreatic adenocarcinoma were analyzed, with 19 of 27 (70%) representing point mutations in p53, particularly in the conserved region of CpG dinucleotides [98].
Another study revealed that 16 (47%) samples out of 34 taken from pancreatic cancer patients showed p53 mutations, and the codons that were the most affected and resulted in point mutations were codon 35, codon 105, codon 133, codon 213, codon 258, and codon 299 [99]. p53 mutation has a secure association with pancreatic cancer, which makes it a target gene for chemotherapy and gene therapy. For this purpose, efforts are being made using cell lines and xenograft models to address this deadly dilemma. A study conducted in a cell line reported that PRIMA-1 (which transforms mutant p53 to wild-type p53 via transformation shift) is regarded as an activator of mutant p53, which enhances apoptosis and makes sensitized tumor mass/cells attractive for chemotherapy [100]. Animal models have also been treated with possible success in some drug tests, and reportedly, Nutlin analogs, which are potent activators of wild-type p53 and inhibitors of MDM2, significantly inhibit tumor formation in xenograft models [101]. Stephano et al. discovered that in p53-deficient pancreatic tumors, yes-associated protein (Yap) is activated and assists as a prospective therapeutic target in various p53-mutated cancers [102].
Fucoidans, which are extracted from the Turbinaria conoides marine brown algae, have remarkable antiproliferative effects via p53 activation in pancreatic cancer cells by triggering caspase-dependent apoptosis and NF-κB negative regulation [103]. Recently, Jiongjia and colleagues reported a new molecule and named it compound-1, which potentially suppresses pancreatic cancer invasiveness by activating DNA damage checkpoints and mitochondrial p53, which results in restoration of the apoptotic machinery [104]. Elemene, which is a new compound recently extracted from Zingiberaceae plant roots, upregulates the level of p53 and downregulates the BCL2 protein level depending on dosage concentration both in vivo and in vitro, presenting significant inhibitory and anticancer activities [105]. However, more clinical trials are needed to unveil the p53 reactivation mechanism in pancreatic cancer. Altogether, these works in the literature suggest a strong association between p53 dysfunction and the progression of pancreatic cancer. Previously, researchers mostly focused on chemotherapy before or after surgical resection to inhibit cancer severity and recurrence. However, in the future, reactivation of p53 in pancreatic cancer patients will gain considerable attention to achieve p53-dependent apoptosis in tumor masses. Moreover, using mitochondrial p53 against tumor mass may also help cope with this deadliest malignancy, which is an idea that needs comprehensive investigation.
4.2.2 CDKN2A (p16INK4 and p14ARF) mutation in pancreatic cancer
The cyclin-dependent kinase inhibitor 2A gene (CDKN2A), which is also recognized as p14ARF and p16INK4, is located on human chromosome number 9. p21.3. CDKN2A has unique characteristics that permit the encoding of two different proteins (p14ARF and p16INK4) through alternative splicing or reading frames. Both p16INK4 and p14ARF regulate the cell cycle and act as tumor suppressor genes [106, 107]. p16INK4 constrains cyclin-dependent kinase 6 (CDK6), cyclin-dependent kinase 4 (CDK4), and the cyclin D1 complex, which in turn triggers the activation of retinoblastoma (Rb protein) family proteins, leading to blockage of the crossover from G1 to S phase. p16INK4 interferes with CDK6, CDK4, and retinoblastoma phosphorylation (Rb Protein) mediated by the CyclinD1 complex, resulting in cell cycle arrest [107, 108]. The other protein part of CDKN2A, p14ARF, inhibits the negative regulator of the p53 gene known as mouse double minute homology-2 (MDM-2) and results in control of cell cycle progression [109]. This result indicates that two distinct proteins encoded by CDKN2A, p16INK4 and p14ARF, control the cell cycle via two unique mechanisms (Fig. 3).
Mechanism of CDKN2A (p16INK4a and p14ARF) alteration in pancreatic cancer. CDKN2A encodes two different proteins (p14ARF and p16INK4) through alternative splicing or reading frames. Left side, in stress conditions, the p14ARF part blocks the negative regulator (MDM2) of the p53 tumor suppressor gene and leads to apoptosis, cell cycle arrest, and DNA repair of the cell. Right side, the p16INK4 performs the function to constrain the cyclin-dependent kinase 6 (CDK6), cyclin-dependent kinase 4 (CDK4), and cyclin D1 complex, which in turn trigger the activation of retinoblastoma (Rb protein) family protein leading to blockage of crossover of G1 to S phase. The loss or inactivation of p14 ARF has similar consequences as p53 while the p16INK4 interferes in CDK6, CDK4, and retinoblastoma phosphorylation (Rb Protein) mediated by CyclinD1 complex results in cell cycle arrest. Mutation in the p14ARF or p16INK4a results in divergence of loss of its normal tumor suppressor function. The mutation mostly occurs due to homozygous deletion, aberrant methylation, and point mutation in SNPs including CC, CT, and TT genotypes. These mutations halt the signals and results in uncontrolled proliferation of the cells
Cyclin-dependent kinase 2A (CDKN2A) is widely studied and accepted as a tumor suppressor and has a commonly altered gene in all cancers. The incidence of inactivation or mutation of CDKN2A is the highest in pancreatic adenocarcinomas, which accounts for 98% of cases in the literature [59] (Tables 2 and 3). Inactivation of the tumor suppressor gene CDKN2A/p16 INK4 is reflected to occur in the initial stage of pancreatic cancer progression and accounts for 40% of pancreatic intraepithelial neoplasia (precursor PanIN lesions) [110, 111]. CDKN2A/p16INK4 inactivation is recognized by multiple mechanisms, such as aberrant methylation of the promoter region, homozygous deletion, or mutation in almost 98% of cases [112]. Some clinical studies have been conducted, and CDKN2A has been analyzed as a predictive-prognostic biomarker for pancreatic cancer. In a study of 88 pancreatic adenocarcinoma patients, CDNK2A/p16INK4 was used as a prognostic factor, which illustrated that 69 out of 88 patients showed mutations in the CDKN2A/p16INK4 gene and underwent surgical removal of the tumor, while the remaining 19 patients were not suggested for surgery [113]. The single-nucleotide polymorphisms (SNPs) of both types (surgically resected tumor and surgically unresected tumor) of patients express dissimilar genotypes. In surgical resection, 56 (81%) out of 69 displayed the CC genotype, while 13 (19%) out of 69 represented the CT genotype. In patients in which no resection occurred, 12 (63%) patients out of 13 displayed the CC genotype, 5 (26%) out of 13 showed the CT genotype, and the remaining 2 patients (11%) showed a unique TT genotype [113].
In another study conducted on 25 patients with pancreatic ductal adenocarcinoma, CDKN2A/p16INK4 screening was performed; the data revealed that p16INK4 was mutated or inactivated in more than 80% of pancreatic tumor samples [114]. These mutations were analyzed further and indicated that 52% of cases presented p16INK4 mutation or inactivation due to aberrant methylation at the promoter region, while homozygous deletion and sequence mutation accounted for 12% and 16%, respectively [114]. In vitro analysis of pancreatic cancer cell lines also revealed mutations in p16INK4. Loukopoulos and colleagues identified p16INK4 mutations in 7 out of 10 pancreatic cancer cell lines by performing direct sequencing and qPCR of both exons 1 and 2 [115]. CDKN2A/p16INK4 had a high mutational frequency that rendered it the best diagnostic biomarker in pancreatic ductal adenocarcinoma, as reported by Klump et al. after analyzing a total of 66 samples of pancreatic juice for p16INK4 and p14ARF mutations, which comprised n = 39 pancreatic cancer and n = 16 with chronic pancreatitis, with the remaining n = 6 being typical pancreatic samples. Only among pancreatic cancer samples were 19 (49%) out of 39 identified with aberrant promoter methylation in p16INK4, while no promotor methylation was observed in p14ARK. This suggests that methylation of p16INK4 is a potential diagnostic marker of pancreatic cancer [116]. These facts enlighten the mechanism by which aberrant epigenetic methylation is involved in the silencing of CDKN2A, leading to pancreatic cancer [112].
Because of the frequent mutation observed in the checkpoint of the tumor suppressor gene in PDAC, its targeting and reactivation might be the main direction of future research. For this purpose, a study was executed in pancreatic cancer cell lines after treating them with inhibitors of CDK4, and CDK6 showed significant suppression both in vivo and in vitro [117]. Another group reported previously that the inhibitors of both CDK4/CDK6—PD-0332991—and insulin-like growth factor 1 receptor (IGF1R/IR, crucial for tumorigenesis and cell survival)—BMS-754807—in pancreatic cancer cell lines synergistically represented remarkable outcomes and suggested that the combination of these inhibitors had the potential to halt the proliferation of pancreatic cancer cells both in vivo and in vitro [118]. Multiple drugs were tested to target CDKN2A/p16INK4; however, no satisfying results were achieved. Palbociclib was used on a trial basis in patients with both pancreatic cancer (n = 12) and biliary cancer (n = 10) harboring CDKN2A mutations. The monotherapy of patients with palbociclib drugs did not exhibit any clinical activity in the advanced stage of pancreatic cancer [119]. The previous literature demonstrates that targeting CDKN2A in pancreatic cancer is approached in multiple ways to treat this deadly disease, but still, no drug, inhibitor, or gene therapy has been established that can completely cure or improve the overall survival of pancreatic cancer patients. Therefore, it is also suggested to further investigate the origin and reversal mechanisms of aberrant methylation leading to CDKN2A inactivation for future therapeutic purposes.
4.3 SMAD4 tumor suppressor gene in pancreatic cancer
The mother against decapentaplegic homolog 4 (SMAD4) tumor suppressor gene, which is also known as “deleted in pancreatic carcinoma 4” (DPC4), is positioned on chromosome 18q21.1 [120]. The SMAD4 tumor suppressor gene belongs to the SMAD family. A highly conserved protein encodes a transcription factor involved as a mediator in the transforming growth factor-β (TGF-β) signaling pathway by transducing the signal to the nucleus [121]. Upon activation, TGF-β results in attachment of TGF-β to SMAD2 and SMAD3 receptors, which triggers the phosphorylation of SMAD2/3 and finally merges with SMAD4 to form a SMAD2/3/4 complex capable of repressing or stimulating its target genes [122] (Fig. 4). Investigations have reported that the TGF-β/SMAD4 signaling-dependent pathways have a tumor suppressor function due to its role in apoptosis and cell cycle arrest of epithelial cells [123]. The TGF-β/SMAD4 pathway is involved in controlling multiple cellular processes, such as fibrosis, tumor development, embryo development, wound healing, and immune function [124]. However, due to its apoptosis and cell cycle arrest behavior in pancreatic cancer, it is regarded as a tumor suppressor. Cells proliferate and grow in a typical fashion in multiple steps, such as G1/S/G2 and M phase, upon receiving some growth signals [125]. However, TGF-β can block these growth signals in the cell cycle at any phase by targeting the SMAD4 gene, but this is useful only if a blockage occurs at the G1 phase [126, 127].
Mechanism of action/mutation of SMAD4 in pancreatic cancer. SMAD4 is a tumor suppressor gene involved in DNA repair, cell cycle arrest, and tumor suppression. SMAD4 is a highly conserved protein that encodes a transcription factor involved as a mediator in the transforming growth factor-β (TGF-β) signaling pathway by transducing the signal to the nucleus. Left side: Upon activation of the TGF-β results in attachment of TGF-β to SMAD2 and SMAD3 receptors, which triggered the phosphorylation of SMAD2/3 and finally merged with SMAD4 to form a SMAD2/3/4 complex. The complex enters the nucleus where in combination with other transcription cofactors, transcription factor, and SMAD4 binding elements (SBE) lead to the silencing or stimulating its target genes and execute the function of DNA repair, cell cycle arrest, and inhibit proliferation. Right side: Due to mutation and loss of SMAD4 function, the transformation of the signal is blocked and cells lead to uncontrolled proliferation and result in tumor formation
Inactivation or loss of the SMAD4 gene is evident in multiple cancers, but the highest frequency, which is 50%, has been reported in pancreatic cancer patients, resulting in loss of protein activation [57, 58] (Tables 2 and 3). Almost 30% of mutations in the SMAD4 tumor suppressor gene in pancreatic cancer occur due to homozygous deletion. Therefore, mutation or inactivation of the SMAD4 tumor suppressor gene might be a potential prognostic factor in pancreatic cancer [128]. A previous study investigated SMAD4 mutation or inactivation in 17/90 (19%) pancreatic cancer patients, and gene mutation depicted a significant correlation (P = 0.006) with overall survival [129]. The inactivation of SMAD4 reportedly occurs due to homozygous deletion in 8 out of 25 (32%) and 3 out of 25 (12%) patients, while modification in the MH2 domain accounts for 5 out of 25 (12%) pancreatic cancer patients [130]. Hayashi and colleagues posit that upon applying a targeted deep sequencing procedure in pancreatic cancer patients, 7 out of 100 (7%) show mutations in SMAD4 and suggest that for better overall survival, 2 or 3 mutations are prognostic [131].
Currently, the frequency of SMAD4 mutations in pancreatic cancer is being analyzed, and SMAD4 modification or complete loss is significantly increased in adenocarcinoma compared to noncancerous pancreatic tissues. Moreover, SMAD4 loss is strongly associated with a poor prognosis and overall survival of pancreatic adenocarcinoma patients [132]. Based on all the available literature, evidence suggests that loss or mutation in SMAD4 is a potential biomarker for PADC diagnosis and correlates significantly with the poor prognosis of patients. New therapeutic approaches are prerequisites that can efficiently target and regulate SMAD4 expression. MicroRNA-421 (miRNA 421) is recognized as a regulator of the SMAD4 gene in pancreatic cancer. Samples taken from humans have identified the upregulation of miRNA-421, while SMAD4 has significantly reduced or resulted in loss in pancreatic cancer patient samples. Ectopic expression of miRNA 421 markedly reduces the SMAD4 expression level and promotes colony formation and proliferation in cell lines [133]. Radiation used for therapeutic purposes in SMAD4-mutated pancreatic adenocarcinoma patients elucidates resistance. SMAD4 is overexpressed in mutant SMAD4 cells and is knocked down via siRNA or shRNA. The knockdown cells promote colony formation and proliferation and represent considerable radioresistance compared to overexpressing cells [134].
Research is ongoing to identify any therapeutic approach that can regulate SMAD4 gene expression. The loss of SMAD4 expression in pancreatic cancer is strongly associated with tumor progression and EMT status, and SMAD4 expression can be used as an independent prognostic factor [135]. In addition, it should also be kept in mind that TGF-β is the stimulatory factor of SMAD4. It is also possible that the loss of SMAD4 activation ability may be due to a defect in TGF-β receptors. Therefore, before surgical resection, investigating SMAD4 expression can lead to an effective therapeutic outcome in the future.
5 Metabolism in PDAC cells
Nutritional biomolecules, including amino acids, fatty acids, and carbohydrates, are used to support the supply of energy, biosynthesis of essential materials, and balanced oxidative stress. Aberrant modification of these pathways results in the interruption of metabolic status, as well as changes in the biosynthetic and energy demands of pancreatic cancer cells. It is worth noting that the PDAC microenvironment is surrounded by stellate cells, immune cells, and ECM; therefore, knowledge regarding the metabolic remodeling of the PDAC tumor microenvironment is necessary [136, 137]. Tumor cells exhibit rapid and increased glucose uptake, even in the presence of ample oxygen levels for glycolysis, which is regarded as the Warburg effect [138]. The most predominant genetic modification that presents a potential role in metabolic reprogramming, glycolytic switching, and pancreatic cancer development is KRAS activation [139,140,141,142]. Gene expression analysis revealed that KRAS activation upregulates glucose uptake by increasing the expression of glucose transporter-1 (GLUT1) and glycolytic activity via increased hexokinase 1 and 2 (HK1 and 2) [141, 143]. In addition to the glycolytic pathway, oncogenic KRAS also supports a side pathway of glycolysis known as the hexosamine biosynthetic pathway (HBP), which ensures the availability of precursors for protein glycosylation [143]. Furthermore, oncogenic KRAS also promotes the incorporation of glucose carbon in the pentose phosphate pathway (PPP), and ribose 5 phosphate (R5P) derived through PPP helps in the synthesis of DNA and RNA in proliferating cells. Pentose phosphate pathways have two types, oxidative and nonoxidative; however, pancreatic cancer arising due to oncogenic KRAS activation is mainly dependent on the nonoxidative pentose phosphate pathway [143, 144]. In the majority of normal cells, the synthesis of ribose 5 phosphate occurs via the oxidative pathway, but this inconsistency displays a possible metabolic weakness in KRAS-driven pancreatic cancer [145].
Another predominant genetic mutation that leads to pancreatic cancer is p53 mutation. In contrast to the mutation in KRAS, which is frequently observed in the initial stage, p53 mutations are mostly present in the later stage, which promotes the progression of pancreatic cancer. p53 mutation prevents the nuclear translocation of an important rate-limiting enzyme of the glycolytic pathway, such as glyceraldehyde-3-phosphate dehydrogenase (GAPDH), and enhances its stability inside the cytoplasm, which in turn allows the glycolysis pathway to evade autophagy and apoptosis [146]. Furthermore, a decrease in the generation of intermediates during the tricarboxylic acid cycle (TCA) due to p53 mutation indicates mitochondrial suppression in pancreatic cancer cells [147]. Hypoxia during tumor progression is commonly observed, which encourages hypoxia-inducible factor-1α (HIF-1α) expression and enhances its constancy. In PDAC, the upregulation of HIF-1α was also detected [148]. On the other hand, HIF-1α is also involved in the upregulation of the glucose transporter 1 receptor, as well as the expression of some genes controlling glycolysis for cytosolic ATP generation in PDAC cells [149– 151]. For the continuous uncontrolled proliferation of cancer cells, the generation of multiple cellular components is required. Lipids play a leading role in the cellular structure and membrane architecture. Some lipid-generating enzymes are frequently upregulated in PDAC, including ATP-citrate lyase (ACLY) [152]. By interfering with the activity of the ACLY enzyme, the inhibition of PDAC cell growth was also achieved in some xenograft tumor models [153]. It has also been reported that fatty pancreases are most commonly associated with pancreatic cancer [154]. Based on this evidence and metabolic association with PDAC, it is necessary to focus on cancer metabolism in synergy with other targeting agents to devise a more accurate therapeutic approach helpful for pancreatic cancer patients.
6 Epigenetic signature of pancreatic cancer
Genetic variations are considered the main factors responsible for the onset of pancreatic cancer. The most common types of genetic mutations that occur in pancreatic cancer are p53 [53], CDKN2A [54], SMAD4 [55], and KRAS [56]. Other less frequent mutations also lead to pancreatic cancer, but they rarely occur. Genetic mutation is not the only factor, but aberrant epigenetic modification also leads to pancreatic cancer. Waddington (1942) defined epigenetics in a developmental context as “between genotype and phenotype lies a whole complex of development processes” and called it an “epigenotype” [155]. Advanced research has revealed that the genetic makeup is not affected by epigenetic modification, but it alters the expression of a particular gene [156]. Currently, based on novel research evidence, epigenetics is defined as “an epigenetic trait is a stably heritable phenotype resulting from changes in a chromosome without alteration in the DNA sequence” [157]. To date, multiple epigenetic alterations have been well characterized, such as DNA methylation and histone modification. Other modifications also exist, such as chromatin remodeling, which leads to alterations in the expression of their particular genes. However, its mechanism of direct heritability is still ill investigated. In this review, our main focus is to summarize the DNA methylation status of genes altered in pancreatic cancer concerning the current literature.
7 DNA methylation and demethylation mechanism
DNA methylation is known as the most studied and well-characterized epigenetic modification in mammals. At the fifth carbon position of a cytosine residue, a methyl (CH3) group is covalently attached, leading to the generation of 5-methylcytosine (5-mC). The enzyme DNA methyltransferases, which are also known as DNMTs (DNMT1, DNMT3A, and DNMT3B), are responsible for catalyzed methylation reactions [158]. Parental methylation and successful offspring transformation are catalyzed by the DNMT1 enzyme. DNMTs 3A/3B are known for their de novo methylation [159]. In pancreatic cancer, almost 80% of pancreatic cancer cases show upregulated DNMT1, leading to hypermethylation and paving the way for DNA hypermethylation as the predominant epigenetic alteration in pancreatic cancer [160]. In multicellular organisms, the origins of DNA methylation are not well elucidated, but it might involve the silencing of jumping genes (transposons/repetitive sequences that can change their location) in the maintenance of genomic stability [161].
The DNA methylation frequency is the highest in GC dinucleotide (CpG)–enriched positions called CpG islands, targeting cytosine residues. A large portion of the human gene promotor is composed of CpG dinucleotides and accounts for 70%, which are mostly in the unmethylated state but shift to methylated upon active transcription [162, 163]. The CpG dinucleotide percentage is very succinct outside CpG islands, and the reason might be the 5-methylcytosine transformation into thymine via a spontaneous deamination process [164]. 5-meCpG translation into the TpG (CpG: TpG) mismatch is mostly repaired by methyl-CpG-binding domain protein 4 (MBD4), which is a thymine DNA glycosylase that replaces modified nucleotides with an unmodified cytosine residue [165]. However, some portion of this mismatch is skipped, and instead of replacing the thymine of the TpG mismatch, MBD4 recognizes thymine as a DNA ordinary nucleotide and replaces guanosine with adenine, resulting in mutation and ultimately cancer [166]. Several somatic mutations in the p53 gene occur due to unrepaired deamination and cytosine conversion to thymine [167]. Based on sufficient references, methylated cytosine residues are considered the most mutational hotspot and predisposing factor for multiple cancers, particularly pancreatic cancer.
The removal or reversal of methylation marks can also be achieved by a process known as DNA demethylation. This DNA demethylation can be either active or passive, depending upon the nature of this process. Passive demethylation occurs during DNA replication when maintenance methylation machinery is absent to reduce the methylation content [168], whereas active demethylation requires specific enzymes to execute this process [169]. The most common and well-studied mechanism of demethylation occurs via ten-eleven translocase (TET1, TET2, TET3) enzymes. These enzymes first transform 5-methylcytosine into 5-hydroxymethylcytosine, followed by 5-formylcytosine, and then 5-corboxycytosine and finally replace the residue with an unmodified cytosine via MBD4 [170]. Focusing on pancreatic cancer, we will try to summarize the epigenetic signature, particularly the aberrant DNA hypermethylation status, of some selected genes in the currently available literature.
7.1 Aberrant hypermethylation in pancreatic cancer
Multiple tumor suppressor genes were identified that undergo hypermethylation or hypomethylation of CpG islands in their promoter regions in pancreatic cancer. The mechanism and degree of hypermethylation or hypomethylation vary in different types of cancer. In this review, our primary focus is on aberrant hypermethylation of different genes in pancreatic cancer. Aberrant hypermethylation mostly affects tumor suppressor genes. Some selected tumor suppressor genes are listed in Table 4. Several studies reported that CDKN2A/p16INK4 was recognized as the first tumor suppressor gene inactivated due to aberrant hypermethylation in their promoter region, leading to silencing of the CDKN2a/p16INK4 gene and causing pancreatic cancer [171, 172]. The function of CDKN2A as an inhibitor of cell cycle arrest at the G1 to S phase is well described in the previous section [125,126,127] (Table 4).
CDKN1C/p57KIP2 also belongs to the cyclin-dependent kinase inhibitor family located on chromosome 11 p15.5 and encodes a protein that negatively regulates cellular proliferation at the G1 phase and inhibits cyclin complexes [173]. By gene expression profiling, Sato et al. reported that hypermethylation of CpG islands in the promoter region results in the downregulation of CDKN1C/p51KIP2 in pancreatic adenocarcinoma. Treatment with an inhibitor of DNA methylation, 5-aza-2′-deoxycytidine, leads to restoration of its original DNA status in a pancreatic cancer cell line, confirming its association with pancreatic cancer [174] (Table 4).
The cyclin D2 (CCND2) gene located on chromosome 12 p13 encodes a protein responsible for cell cycle regulation in the G1 to S phase. It ensures the availability of DNA content and other cyclins by activating two crucial cyclin-dependent kinases, 4/6, which phosphorylate retinoblastoma [175]. Despite cyclin D2 involvement in the cell cycle and proliferation, its overexpression has been reported to have a growth inhibitory function due to its ability to prompt a senescence-like effect, which leads to the inhibition of cellular proliferation [176]. Currently, global expression analysis of genes in IPMN of the pancreas suggests that cyclin D2 expression is reduced many-fold in pancreatic adenocarcinoma compared to healthy pancreatic epithelial cells [177]. Matsubayashi et al. reported that the change in the methylation status of the Cyclin D2 promoter occurs with age, but aberrant hypermethylation (86%) is commonly found in pancreatic cancer, which renders it a suitable candidate gene for diagnostic and therapeutic purposes [178] (Table 4).
RAS is an oncogene and a member of the guanosine-triphosphate (GTPase) family located on chromosome # 12 p12.1, encoding a small 21 kDa protein, which performs the function of molecular switching by changeover between two different states [65]. The frequency of K-RAS oncogene mutations is markedly elevated in pancreatic cancer (for a detailed description, refer to the previous section) [69, 70] (Table 4). Epigenetic alteration also results in mutation or mutational activation of the K-RAS gene, particularly via hypermethylation of CpGs in the promoter. Jiao et al. investigated the plasma DNA of pancreatic cancer patients showing K-RAS mutations for methylation status. They reported that 32.5% (33%) of patients had K-RAS mutations due to promoter CpG island hypermethylation. The point mutation of G to A is the predominant mutation at codon 12, and smoking is considered one of the risk factors predisposing patients to codon 12 mutations [179] (Table 4).
Preproenkephalin (PENK) is located on chromosome 8q23–q24 and encodes the neuropeptide precursor protein met-enkephalin, which shows a strong interaction affinity for the receptor of opioid growth factor and causes its inhibition. A previous study conducted by the Zagon group identified that met-enkephalin halts the growth of multiple tumors in humans, particularly pancreatic cancer [180]. Hypermethylation of CpG islands in the PENK promoter significantly reduces its expression, as reported by Comb et al. [181]. Noriyoshi et al. reported in their study on pancreatic ductal adenocarcinoma samples that 14 out of 15 (93%) patients illustrate aberrant hypermethylation in the PENK promoter [182] (Table 4). Hence, aberrant methylation of the PENK promoter is a potential factor that promotes cellular growth and tumor formation.
The suppressor of cytokine-signaling 1 gene (SOCS-1, aka SSI-1 or JAB-1) located on chromosome 16p13.13 encodes a protein known as the JAK binding protein, which is involved in the regulation of Janus kinase signal transducers and activators of transcription (JAK-STAT) signal transduction pathways. The SOCS-1 protein receives signals from multiple cytokines and passages them from the extracellular to the intracellular matrix [183, 184]. Toshiaki and colleagues analyzed pancreatic tumor specimens and reported that 8 out of 14 (57%) display aberrant hypermethylation in the promoter region, resulting in SOCS-1 silencing [185] (Table 4).
Protocadherin 10 (PCDH10) is a tumor suppressor gene located on chromosome 4 q28 that encodes a protein involved in different vital cellular functions. Protocadherin is primarily known for its cell-to-cell adhesion characteristics but also retains some other essential functions, including growth control and signal transduction [186]. Protocadherin is one of the cell adhesion genes that have been studied in pancreatic cancer via transcriptome sequencing, which frequently shows aberrant methylation [187]. Recent work reports that PCDH10 in 14 out of 23 (60.9 = 61%) pancreatic adenocarcinoma patients presents aberrant hypermethylation, leading to the downregulation of PCGH10 expression, which is associated with a poor prognosis in pancreatic cancer [188] (Table 4).
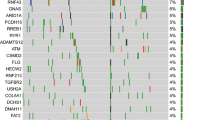
Iroquois homeobox 4 (IRX4), which is a tumor suppressor gene located on chromosome 5p15.33, encodes a protein that plays a role in embryo pattern formation, ventricular differentiation, and heart development [189]. Chakma et al. reported its downregulation in twelve pancreatic cancer cell lines. In resected pancreatic tumor specimens, 15 out of 22 (68%) showed hypermethylation in the promoter region compared to the surrounding healthy tissues [190] (Table 4). Currently, two other tumor suppressor genes, ADAMTS1 “A disinterring and metalloproteinase with thrombospondin motifs 1” and BNC1 “Zinc finger protein basonuclin-1,” are known to be downregulated due to aberrant hypermethylation in pancreatic cancer, as reported by Eissa and colleagues [191] (Table 4).
RPRM (Reprimo, TP53-dependent G2 arrest mediator candidate) is a tumor suppressor gene located on chromosome 2q23.3 that encodes a protein involved in p53-dependent G2/M cell cycle arrest. The downregulation of RPRM due to aberrant hypermethylation of CpG in the promoter has been reported in 20 out of 22 (91%) pancreatic cancer patients [192]. The RARβ “retinoic acid receptor, β” tumor suppressor gene involved in controlling cellular growth is reportedly downregulated in pancreatic cancer via aberrant promoter CpG hypermethylation [193] (Table 4).
Other tumor suppressor genes frequently mutated in pancreatic cancer due to aberrant hypermethylation include ubiquitin carboxyl-terminal esterase L1 (ubiquitin thiolesterase) UCHL1 located on chromosome 4 p14 [194], Forkhead box E1 (thyroid transcription factor 2) FOXE1 located on chromosome 9 q22 [150], survival of motor neuron protein-interacting protein 1 (SIP1) located at chromosome # 14q13–q21 [195], secreted protein, acidic, cysteine-rich (osteonectin) SPARC/ON located at chromosome 5q31.3–q32 [196], and yeast mitosis arrest deficient related (MAD) aka MDF-1 located at chromosome 11 q13 [197] (Table 4). It has also been reported that some microRNAs function as tumor suppressors but mutated in pancreatic cancer due to aberrant hypermethylation. MicroRNA 9-1, or miR9-1, which is located at chromosome 1q22 [197], and microRNA-506 (miR-506), which is located in chromosomal region Xq27.3 [198] (Table 4), were mutated in pancreatic cancer due to aberrant hypermethylation.
Vincent et al. identified through genome-wide analysis that two genes, BMP3 (bone morphogenetic protein 3) located at chromosome 4 q21 and DNMT3A DNA methyltransferases 3 alpha, located at 2 p23.3, were aberrantly hypermethylated in pancreatic cancer [199] (Table 4). CADM1, or cell adhesion molecule 1, located at chromosome 11q23 encodes a protein involved in cell-cell adhesion and is also mutated in pancreatic cancer due to aberrant hypermethylation [200]. All of these available pieces of literature demonstrate very clearly that epigenetic initiation of pancreatic cancer mostly results from hypermethylation of tumor suppressor genes. Other tumor suppressor genes most commonly inactivated in pancreatic cancer, such as SMAD4/DPCA4 and p53, have no relation with the methylation status. All selected genes mutated due to aberrant hypermethylation are listed in Table 4. Hence, it is well elucidated that aberrant hypermethylation is one of the significant factors involved in pancreatic cancer initiation, progression, and metastasis. CpG aberrant methylation in the promoter region might be a hotspot of targeted therapy in the future. Some new drug discoveries are necessary, which can reverse these aberrant methylations and restore the typical functional role of genes.
7.2 Aberrant hypomethylation in pancreatic cancer
The loss of methylation content of DNA in specific cancers has also been observed. The earliest sign of the modified status of DNA methylation observed in cancer cells is the loss or reduction of 5-methylcytosine [201, 202]. Analysis of the whole genome reveals that 5-methylcytosine depletion mostly occurs in repetitive sequences [203, 204]. In addition to aberrant hypermethylation of oncogenes or tumor suppressor genes leading to pancreatic cancer, some genes are also hypomethylated, which downregulates or overexpresses that particular gene and predisposes patients to pancreatic cancer. DNA hypomethylation in pancreatic cancer is mostly observed in the 5’ region of some genes, which results in the upregulation of that particular gene. Hypomethylation can either upregulate or downregulate gene expression and protein levels. Some frequently hypomethylated genes leading to pancreatic cancer will be briefly summarized here (Table 5).
Serpin Family B Member 5 (SERPINB5), which is a tumor suppressor gene located at chromosome 18 q21.3, encodes a protein involved in the regulation of cell motility, apoptosis, autophagy, DNA damage response, and cell death [205]. Sato et al. reported that SERPINB5 is aberrantly hypomethylated in 87% of pancreatic cancer cases [206] (Table 5). Chen and colleagues identified three genes, SULT1E1 (Sulfotransferase Family 1E Member 1, located at 4q13.1), IGF2BP3 (insulin-like growth factor 2 mRNA-binding protein 3, located at chromosome 7p15.3), and MAP4K4 (mitogen-activated protein 4 kinase 4, located at chromosome 2 q11.2), that were mutated due to aberrant hypomethylation in pancreatic cancer. They correlated these three genes with the patient’s overall survival and suggested that mutations in these genes might be prognostically venerable in pancreatic cancer [207] (Table 5).
Mucin 4 (MUC4), a gene located at chromosome 3q29, belongs to the mucin family protein and performs a dual role that depends upon the tissue type. Zhu et al. reported the overexpression of MUC4 due to aberrant hypomethylation in pancreatic cancer tissues [208]. Moreover, the Sato group identified that multiple genes, including MSLN, TFF2, SFN, LCN2, PSCA, S100A4, and S100P, are hypomethylated and predispose individuals to pancreatic cancer (Table 5) [206, 209,210,211]. A recent work identified that in addition to the hypermethylation of miRNA 9-1, hypomethylation also initiates pancreatic cancer [211, 212]. Similarly, Iguchi et al. reported that CDKN1C/p57 and FOXE1 were mutated in pancreatic cancer due to hypomethylation [211, 213] (Table 5). Epigenetic alterations obviously play a significant role in cancer initiation and development. Nevertheless, we are still far from understanding the interplay and origin of epigenetic signatures, which lead to genetic modification and, ultimately, pancreatic cancer. Recognizing the precise origin of these molecular alterations is still a hallmark and leaves a large space for researchers. The characterization of pancreatic cancer genetics by ignoring the epigenetic signature will lead to a dead end. Therefore, an analysis of aberrant epigenetic modification/arrangement will play a crucial role in pancreatic cancer molecular diagnostics in the future.
8 Epigenetic approaches in cancer treatments
The intricacy of cancer can be explained as the interaction between epigenetic and genetic aberrations that mutually help drive the initiation and progression of a specific type of cancer. Genome-wide global DNA methylation analysis reveals that distinctive epigenetic markers have been found in almost all cases of a particular type of cancer, which can be correlated with the tumor type and stage of that cancer [214,215,216]. Based on these characteristics, the researchers appreciate the practice of these epigenetic alterations as potential biomarkers in early screening, detection, treatment, prognosis, and anticipation of a response to therapy [215, 217, 218]. Global histone modification is another epigenetic alteration that takes place during tumorigenesis and results in aberrant expression of genes [219, 220]. The reversible nature of epigenetic alterations and their plasticity make them possible anticancer targets because of the resetting ability of the cancer epigenome. Two epidrugs have been approved by the USA (FDA), including histone deacetylase (iHDAC) inhibitors and DNA methylation (iDNMT) inhibitors, which potentially act on their respective target enzymes, while others are in clinical trials, also showing promising therapeutic approaches [221,222,223,224].
The first approved epidrug (epigenetic drug) designated in the treatment of acute myeloid leukemia was 5-azacitidine, which is a DNA methylation inhibitor. In 2006, 5-aza-2-deoxycytidine, which is a cytosine analog showing the same clinical indication, inhibited DNA methyltransferase at very low dosages in actively replicating cells. This resulted in the loss of methylation marks and reactivation of abnormally silenced tumor suppressor genes and their functionality [225]. It has recently been reported that iDNMTs exhibit antitumoral action in multiple ways, such as through hypomethylation and DNA double-strand break mechanisms [226]. Moreover, the use of a viral defense pathway to activate endogenous retroviral elements by stimulating immune signaling has also been reported [227, 228].
The removal of acetylation marks from histone tails is achieved by HDACs, which are necessary for rendering chromatin in its repressive state. Multiple histone deacetylase inhibitor iHDACs are under development as potential anticancer drugs, expressing a pivotal role in epigenetic regulation, apoptosis, cell death induction, cell mobility inhibition, cell cycle arrest inhibition, and antiangiogenesis in transformed cells [221]. The therapy is mainly mediated via the activation of aberrantly silenced tumor suppressor genes; however, the mechanism is not fully elucidated. Four types of iHDAC drugs have been approved by the US FDA: vorinostat, belinostat, romidepsin, and panobinostat for the treatment of cutaneous T cell lymphoma, peripheral T cell lymphoma, cutaneous and peripheral lymphoma, and drug-resistant multiple myeloma, respectively. All these drugs have the same mode of action exerted by inducing cell cycle arrest, sensitizing cancer cells to therapy, and apoptosis [229, 230].
Although iHDACs and iDNMTs are effective alone, their effectiveness can be enhanced if they are used in combination, especially for solid tumor treatment [231]. It has been reported that low doses of iHDACs and iDNMTs present a robust and long-lasting positive response in patients with NSCLC [232]. However, combination therapy with iDNMTs and iHDACs in acute myeloid leukemia presents conflicting results regarding its efficacy [233]. More work is needed at the clinical and molecular levels to escape undesirable outcomes of the treatment.
9 Future prospects
Pancreatic cancer is estimated to be the second leading cause of cancer-led mortality by 2030 in the USA due to its growing incidence and mortality rate. Researchers have identified multiple factors involved in the PC initiation and progression in thousands of published articles, but PC treatment still lake effectiveness. We think that there are some limitations that need to be appropriately addressed to attain fruitful outcomes. Through this review, we identified that multiple genes are mutated in PC due to homozygous deletions and point mutations, such as single-nucleotide polymorphisms. However, the origin and underlying mechanism involved in this mutation are still unknown. K-RAS is reportedly mutated in PC due to alterations in codons 12, 13, and 61. Nonetheless, it is still unclear what factors depict a targeted affinity for these codons and render them the most mutational hotspot in PC initiation. Similar behavior was observed in p53-mutated PC cases in which frequent point mutations were identified in codon 35, codon 105, codon 133, codon 213, codon 258, and codon 299 [74]. Therefore, more research is a prerequisite to unveil the mechanism underlying these mutations to resolve this unmet medical need. Some current works illustrate that activating the mitochondrial p53 counterpart represents a new direction in cancer therapy.
Moreover, some new drugs should be identified as having the potential to shift transformation of the mutated gene to its wild-type operational activities. If, in the future, researchers succeed in discovering therapeutic drugs that can restore the wild-type activity of the mutated gene, this will lead to a new era of cancer treatment. Aberrant methylation is a widely studied epigenetic modification in DNA that can either upregulate or downregulate a gene. Mostly, tumor suppressor genes are aberrantly hypermethylated in the course of PC initiation and progression. However, the questions that arise here are what is the origin of and what factors are involved in this epigenetic hypermethylation. In addition to hypermethylation, hypomethylation is also observed in gene silencing leading to PC. What factor determines the fate of gene methylation status is still unclear. Many limitations persist in the available literature and need to be further explained appropriately for better understanding. Furthermore, elucidation is required to identify miRNAs with potency in blocking epigenetic alterations or to discover new therapeutic drugs that can potentially restore the wild-type methylation status of a gene and ensure its optimal activity.
10 Conclusion
Pancreatic cancer is a fatal, aggressive, and the leading cause of mortality worldwide, with a poor 5-year survival rate that is less than 9%. Research on targeted therapeutic measures has continued for the last four decades, but PC is also emerging in a parallel manner and is among the top 5 cancers responsible for cancer-led mortality. The incidence ratio is the highest in industrialized countries, and an estimated value suggests that by 2030, PC will be the second leading cause of mortality in the USA. Multiple factors are involved in the initiation and progression of PC, including cigarette smoking [234, 235], alcohol consumption [236], hereditary factors [237], obesity [238, 239], age, nutritional factors [240], genetic mutations [241], and aberrant epigenetic signatures [187]. However, genetic mutations and aberrant epigenetic modifications are the leading factors involved in the course of PC initiation and progression. Multiple genes are involved in the onset of PC, but the highest mutational rate is held by four frequently mutated genes, p53, CDKN2A, SMAD4, and K-RAS. In addition to genetic modifications, epigenetic alterations are also markedly observed in PC. Aberrant hypermethylation of tumor suppressor genes is predominantly involved in gene downregulation leading to PC. Some genes were also observed to be hypomethylated in PC. The prognosis of PC is considered worse because of the lack of symptoms, the lack of detection tools for its early diagnosis, and limitations in therapeutic therapy. Surgical resection is the only possible cure if diagnosed before metastasis to ensure the longevity of patients. Currently, no drug therapy is effective in treating this deadly malignancy. Therefore, some reviewable therapeutic strategies should be applied to overcome the deleterious effect of PC. In addition, the discovery of new therapeutic drugs is strongly necessary to target mutated genes and restore their wild-type genetic and epigenetic status to ensure their effective operational activity.
Abbreviations
- PC:
-
Pancreatic cancer
- PADC:
-
Pancreatic ductal adenocarcinoma
- PanNET:
-
Pancreatic neuroendocrine tumor
- IPMN:
-
Intraductal papillary mucinous neoplasms or tumors
- K-RAS:
-
Kirsten rat sarcoma
- TP53/ p53:
-
Tumor protein 53
- CDKN2A:
-
Cyclin-dependent kinase inhibitor 2 A
- DPC4/ SMAD4:
-
Deleted in pancreatic carcinoma 4/ Mother against decapentaplegic, homologs 4
- BRCA1:
-
Breast cancer 2, early onset
- BRCA2:
-
Breast cancer 2, early onset
- PALB2:
-
Partner and localizer of BRCA2
- SBE:
-
SMAD4 binding protein
- DNMTs:
-
DNA methyltransferases
- ATM:
-
Ataxia telangiectasia mutated
- APC:
-
Adenomatous polyposis coli
- STK11:
-
Serine/threonine kinase 11
- MLH1:
-
MutL homolog
- PRSS1:
-
Serine Protease 1
- PMS2:
-
Postmeiotic Segregation Increased, S. Cerevisiae, 2
- MSH2:
-
MutS protein homolog 2
- MSH6:
-
MutS homolog 6
- GTP:
-
Guanosine triphosphate
- GDP:
-
Guanosine diphosphate
- RTK:
-
Receptor tyrosine kinases
- ERK:
-
Extracellular signal–regulated kinases
- PI3K:
-
Phosphoinositide 3-kinase
- PTEN:
-
Phosphatase and tensin homolog
- AKT/ PKB:
-
Protein kinase B
- NF-κB:
-
Nuclear factor kappa-light-chain-enhancer of activated B cell
- MAPK:
-
Mitogen-activated Protein Kinase
- IL-1 α:
-
Interleukin 1 Alpha
- PRIMA-1:
-
Proline-rich membrane anchor 1
- MDM2:
-
Mouse double minute 2 homolog
- Yap:
-
Yes-associated protein
- BCL2:
-
B-cell lymphoma 2
- Rb:
-
Retinoblastoma
- SNPs:
-
Single nucleotide polymorphism
- qPCR:
-
Quantitative polymerase chain reaction
- IGF1R/IR:
-
Insulin-like growth factor 1 receptor
- TGFβ:
-
Transforming growth factor-β
- TET:
-
Ten-eleven translocase
- MBD4:
-
Methyl-CpG-binding domain protein 4
- CCND2:
-
Cyclin D2
- PENK:
-
Preproenkephalin
- JAK-STAT:
-
Janus kinase signal transducers and activators of transcription
- PCDH10:
-
Protocadherin 10
- SOCS-1:
-
Suppressor of cytokine signaling – 1
- MAD:
-
Mitosis Arrest DeFicient
- MAP4K4:
-
Mitogen-activated protein 4 kinase 4
- SERPINB5:
-
Serpin Family B Member 5
- SULT1E1:
-
Sulfotransferase Family 1E Member 1
- MUC4:
-
Mucin-4
- 5-mC:
-
5- methylcytosine
- 5-hmC:
-
5- hydroxy methylcytosine
References
Siegel, R. L., Miller, K. D., & Jemal, A. (2019). Cancer statistics, 2019. CA: a Cancer Journal for Clinicians, 69, 7–34.2.
Street W. Cancer Facts & Figures 2019. American Cancer Society: Atlanta, GA, USA. 2019. (Accessed on 19-11-2019).
Rahib, L., Smith, B. D., Aizenberg, R., Rosenzweig, A. B., Fleshman, J. M., & Matrisian, L. M. (2014). Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Research, 74(11), 2913–2921.
Parkin, D. M., Bray, F., Ferlay, J., & Pisani, P. (2005). Global cancer statistics, 2002. CA: a Cancer Journal for Clinicians, 55(2), 74–108.
Teague, A., Lim, K. H., & Wang-Gillam, A. (2015). Advanced pancreatic adenocarcinoma: a review of current treatment strategies and developing therapies. Therapeutic Advances in Medical Oncology., 7(2), 68–84.
Niess, H., Kleespies, A., Andrassy, J., Pratschke, S., Angele, M. K., Guba, M., Jauch, K. W., & Bruns, C. J. (2013). Pancreatic cancer in the elderly: guidelines and individualized therapy. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen., 84(4), 291–295.
Oberstein, P. E., & Olive, K. P. (2013). Pancreatic cancer: why is it so hard to treat? Therapeutic Advances in Gastroenterology, 6(4), 321–337.
Neoptolemos, J. P., Stocken, D. D., Friess, H., Bassi, C., Dunn, J. A., Hickey, H., Beger, H., Fernandez-Cruz, L., Dervenis, C., Lacaine, F., & Falconi, M. (2004). A randomized trial of chemoradiotherapy and chemotherapy after resection of pancreatic cancer. The New England Journal of Medicine, 350(12), 1200–1210.
Bosetti, C., Lucenteforte, E., Silverman, D. T., Petersen, G., Bracci, P. M., Ji, B. T., Negri, E., Li, D., Risch, H. A., Olson, S. H., & Gallinger, S. (2011). Cigarette smoking and pancreatic cancer: an analysis from the International Pancreatic Cancer Case-Control Consortium (Panc4). Annals of Oncology, 23(7), 1880–1888.
Klein, A. P., Brune, K. A., Petersen, G. M., Goggins, M., Tersmette, A. C., Offerhaus, G. J., Griffin, C., Cameron, J. L., Yeo, C. J., Kern, S., & Hruban, R. H. (2004). Prospective risk of pancreatic cancer in familial pancreatic cancer kindreds. Cancer Research, 64(7), 2634–2638.
Hidalgo, M., Cascinu, S., Kleeff, J., Labianca, R., Löhr, J. M., Neoptolemos, J., Real, F. X., Van Laethem, J. L., & Heinemann, V. (2015). Addressing the challenges of pancreatic cancer: future directions for improving outcomes. Pancreatology., 15(1), 8–18.
Stewart BW, Wild CP (2019). World cancer report, 2014. Public Health.
De La Cruz, M. S., Young, A. P., & Ruffin, M. T. (2014). Diagnosis and management of pancreatic cancer. American Family Physician, 89(8), 626–632.
Street W. Cancer Facts & Figures 2019. American Cancer Society: Atlanta, GA, USA. 2019. https://www.cancer.org/cancer/pancreatic-cancer/detection-diagnosis-staging/survival-rates.html. (Accessed on Nov 22, 2019).
Rawla, P., Sunkara, T., & Gaduputi, V. (2019). Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World Journal of Oncology., 10(1), 10.
Siegel, R. L., Miller, K. D., & Jemal, A. (2016). Cancer statistics, 2016. CA: a Cancer Journal for Clinicians, 66(1), 7–30.
Mohammed, S., George Van Buren, I. I., & Fisher, W. E. (2014). Pancreatic cancer: advances in treatment. World journal of gastroenterology: WJG, 20(28), 9354.
Haqq, J., Howells, L. M., Garcea, G., Metcalfe, M. S., Steward, W. P., & Dennison, A. R. (2014). Pancreatic stellate cells and pancreas cancer: current perspectives and future strategies. European Journal of Cancer, 50, 2570–2582.
Ikenaga, N., Ohuchida, K., Mizumoto, K., Cui, L., Kayashima, T., Morimatsu, K., et al. (2010). CD10+ pancreatic stellate cells enhance the progression of pancreatic cancer. Gastroenterology, 139, 1041–1051.
Lonardo, E., Frias-Aldeguer, J., Hermann, P. C., & Heeschen, C. (2012). Pancreatic stellate cells form a niche for cancer stem cells and promote their self-renewal and invasiveness. Cell Cycle, 11, 1282–1290.
Jacobetz, M. A., Chan, D. S., Neesse, A., Bapiro, T. E., Cook, N., Frese, K. K., et al. (2013). Hyaluronan impairs vascular function and drug delivery in a mouse model of pancreatic cancer. Gut, 62, 112–120.
Özdemir, B. C., Pentcheva-Hoang, T., Carstens, J. L., Zheng, X., Wu, C. C., Simson, T., et al. (2014). Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with diminished survival. Cancer Cell, 25, 719–734.
Rhim, A. D., Oberstein, P. E., Thomas, D. H., Mirek, E. T., Palermo, C. F., Sastra, S. A., et al. (2014). Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell, 25, 735–747.
Puleo, F., Nicolle, R., Blum, Y., Cros, J., Marisa, L., Demetter, P., et al. (2018). Stratification of pancreatic ductal adenocarcinomas based on tumor and microenvironment features. Gastroenterology, 155, 1999–2013.
Moffitt, R. A., Marayati, R., Flate, E. L., Volmar, K. E., Loeza, S. G., Hoadley, K. A., et al. (2015). Virtual microdissection identifies distinct tumor- and stroma-specific subtypes of pancreatic ductal adenocarcinoma. Nature Genetics, 47, 1168–1178.
Ye, C., Zheng, L., & Yuan, C. H. (2019). Pancreatic ductal adenocarcinoma immune microenvironment and immunotherapy prospects. Zhonghua wai ke za zhi [Chinese Journal of Surgery]., 57(1), 10–15.
Banerjee, K., Kumar, S., Ross, K. A., et al. (2018). Emerging trends in the immunotherapy of pancreatic cancer. Cancer Letters, 417, 35–46.
Yarchoan, M., Hopkins, A., & Jaffee, E. M. (2017). Tumor mutational burden and response rate to PD-1 inhibition. The New England Journal of Medicine, 377, 2500–2501.
Laklai, H., Miroshnikova, Y. A., Pickup, M. W., et al. (2016). Genotype tunes pancreatic ductal adenocarcinoma tissue tension to induce matricellular fibrosis and tumor progression. Nature Medicine, 22, 497.
Feig, C., Gopinathan, A., Neesse, A., Chan, D. S., Cook, N., & Tuveson, D. A. (2012). The pancreas cancer microenvironment. AACR: In.
Ferdek, P. E., & Jakubowska, M. A. (2017). Biology of pancreatic stellate cellsdmore than just pancreatic cancer. Pflügers Archiv - European Journal of Physiology, 469, 1039–1050.
Apte, M., Pirola, R., & Wilson, J. (2012). Pancreatic stellate cells: a starring role in normal and diseased pancreas. Frontiers in Physiology, 3, 344.
Jiang, H., Hegde, S., & DeNardo, D. G. (2017). Tumor-associated fibrosis as a regulator of tumor immunity and response to immunotherapy. Cancer Immunology, Immunotherapy, 66, 1037–1048.
Pothula, S. P., Xu, Z., Goldstein, D., Pirola, R. C., Wilson, J. S., & Apte, M. V. (2016). Key role of pancreatic stellate cells in pancreatic cancer. Cancer Letters, 381, 194–200.
Von Ahrens, D., Bhagat, T. D., Nagrath, D., Maitra, A., & Verma, A. (2017). The role of stromal cancer-associated fibroblasts in pancreatic cancer. Journal of Hematology & Oncology, 10, 76.
Ohlund, D., Handly-Santana, A., Biffi, G., et al. (2017). Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. The Journal of Experimental Medicine, 214, 579–596.
Ozdemir, B. C., Pentcheva-Hoang, T., Carstens, J. L., et al. (2014). Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell, 25, 719–734.
Ugel, S., De Sanctis, F., Mandruzzato, S., & Bronte, V. (2015). Tumor-induced myeloid deviation: when myeloid-derived suppressor cells meet tumor-associated macrophages. Journal of Clinical Investigation, 125, 3365–3376.
Porembka, M. R., Mitchem, J. B., Belt, B. A., et al. (2012). Pancreatic adenocarcinoma induces bone marrow mobilization of myeloidderived suppressor cells which promote primary tumor growth. Cancer Immunology, Immunotherapy, 61, 1373–1385.
Stromnes, I. M., Brockenbrough, J. S., Izeradjene, K., et al. (2014). Targeted depletion of an MDSC subset unmasks pancreatic ductal adenocarcinoma to adaptive immunity. Gut., 63, 1769–1781.
Liu, G., Bi, Y., Shen, B., et al. (2014). SIRT1 limits the function and fate of myeloid-derived suppressor cells in tumors by orchestrating HIF-1aedependent glycolysis. Cancer Research, 74, 727–737.
Stromnes, I. M., Hulbert, A., Pierce, R. H., Greenberg, P. D., & Hingorani, S. R. (2017). T-cell localization, activation, and clonal expansion in human pancreatic ductal adenocarcinoma. Cancer Immunology Research, 5, 978–991.
Ghiorzo, P. (2014). Genetic predisposition to pancreatic cancer. World Journal of Gastroenterology, 20(31), 10778–10789.
Shi, C., Daniels, J. A., & Hruban, R. H. (2008). Molecular characterization of pancreatic neoplasms. Advances in Anatomic Pathology, 15(4), 185–195.
Vincent, A., Herman, J., Schulick, R., Hruban, R. H., & Goggins, M. (2011). Pancreatic cancer. Lancet., 378(9791), 607–620.
Solomon, S., Das, S., Brand, R., & Whitcomb, D. C. (2012). Inherited pancreatic cancer syndromes. Cancer Journal, 18(6), 485491.
Hahn, S. A., Greenhalf, B., Ellis, I., Sina-Frey, M., Rieder, H., Korte, B., Gerdes, B., Kress, R., Ziegler, A., Raeburn, J. A., & Campra, D. (2003). BRCA2 germline mutations in familial pancreatic carcinoma. Journal of the National Cancer Institute, 95(3), 214–221.
Couch, F. J., Johnson, M. R., Rabe, K. G., Brune, K., De Andrade, M., Goggins, M., Rothenmund, H., Gallinger, S., Klein, A., Petersen, G. M., & Hruban, R. H. (2007). The prevalence of BRCA2 mutations in familial pancreatic cancer. Cancer Epidemiology and Prevention Biomarkers., 16(2), 342–346.
Murphy, K. M., Brune, K. A., Griffin, C., Sollenberger, J. E., Petersen, G. M., Bansal, R., Hruban, R. H., & Kern, S. E. (2002). Evaluation of candidate genes MAP2K4, MADH4, ACVR1B, and BRCA2 in familial pancreatic cancer: deleterious BRCA2 mutations in 17%. Cancer Research, 62(13), 3789–3793.
Jones, S., Hruban, R. H., Kamiyama, M., Borges, M., Zhang, X., Parsons, D. W., Lin, J. C., Palmisano, E., Brune, K., Jaffee, E. M., & Iacobuzio-Donahue, C. A. (2009). Exomic sequencing identifies PALB2 as a pancreatic cancer susceptibility gene. Science., 324(5924), 217.
Tischkowitz, M. D., Sabbaghian, N., Hamel, N., Borgida, A., Rosner, C., Taherian, N., Srivastava, A., Holter, S., Rothenmund, H., Ghadirian, P., & Foulkes, W. D. (2009). Analysis of the gene coding for the BRCA2-interacting protein PALB2 in familial and sporadic pancreatic cancer. Gastroenterology., 137(3), 1183–1186.
Slater, E. P., Langer, P., Niemczyk, E., Strauch, K., Butler, J., Habbe, N., Neoptolemos, J. P., Greenhalf, W., & Bartsch, D. K. (2010). PALB2 mutations in European familial pancreatic cancer families. Clinical Genetics, 78(5), 490–494.
Hwang, R. F., Gordon, E. M., Anderson, W. F., & Parekh, D. (1998). Gene therapy for primary and metastatic pancreatic cancer with intraperitoneal retroviral vector bearing the wild-type p53 gene. Surgery, 124, 143–150.
Schutte, M., Hruban, R. H., Geradts, J., Maynard, R., Hilgers, W., Rabindran, S. K., Moskaluk, C. A., Hahn, S. A., Schwarte-Waldhoff, I., Schmiegel, W., et al. (1997). Abrogation of the RB/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas. Cancer Research, 57, 3126–3130.
Blackford, A., Serrano, O. K., Wolfgang, C. L., Parmigiani, G., Jones, S., Zhang, X., Parsons, D. W., Lin, J. C., Leary, R. J., Eshleman, J. R., & Goggins, M. (2009). SMAD4 gene mutations are associated with poor prognosis in pancreatic cancer. Clinical Cancer Research, 15(14), 4674–4679.
Kim, S. T., Lim, D. H., Jang, K. T., Lim, T., Lee, J., Choi, Y. L., Jang, H. L., Yi, J. H., Baek, K. K., Park, S. H., & Park, Y. S. (2011). Impact of KRAS mutations on clinical outcomes in pancreatic cancer patients treated with first-line gemcitabine-based chemotherapy. Molecular Cancer Therapeutics, 10(10), 1993–1999.
De Bosscher, K., Hill, C. S., & Nicolas, F. J. (2004). Molecular and functional consequences of SMAD4 c-terminal missense mutations in colorectal tumour cells. The Biochemical Journal, 379, 209–216.
Blackford, A., Serrano, O. K., Wolfgang, C. L., Parmigiani, G., Jones, S., Zhang, X., Parsons, D. W., Lin, J. C., Leary, R. J., Eshleman, J. R., et al. (2009). SMAD4 gene mutations are associated with poor prognosis in pancreatic cancer. Clinical Cancer Research, 15, 4674–4679.
Schutte, M., Hruban, R. H., Geradts, J., Maynard, R., Hilgers, W., Rabindran, S. K., Moskaluk, C. A., Hahn, S. A., Schwarte-Waldhoff, I., Schmiegel, W., et al. (1997). Abrogation of the RB/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas. Cancer Research, 57, 3126–3130.
Chen, J., Li, D., Killary, A. M., Sen, S., Amos, C. I., Evans, D. B., Abbruzzese, J. L., & Frazier, M. L. (2009). Polymorphisms of p16, p27, p73, and MDM2 modulate response and survival of pancreatic cancer patients treated with preoperative chemoradiation. Annals of Surgical Oncology, 16, 431–439.
Hwang, R. F., Gordon, E. M., Anderson, W. F., & Parekh, D. (1998). Gene therapy for primary and metastatic pancreatic cancer with intraperitoneal retroviral vector bearing the wild-type p53 gene. Surgery, 124, 143–150.
Kern, S. E., Pietenpol, J. A., Thiagalingam, S., Seymour, A., Kinzler, K. W., & Vogelstein, B. (1992). Oncogenic forms of p53 inhibit p53-regulated gene expression. Science, 256, 827–830.
Bamford, S., Dawson, E., Forbes, S., Clements, J., Pettett, R., Dogan, A., Flanagan, A., Teague, J., Futreal, P. A., Stratton, M. R., et al. (2004). Thecosmic (catalogue of somatic mutations in cancer) database and website. British Journal of Cancer, 91, 355–358.
Kim, S. T., Lim, D. H., Jang, K. T., Lim, T., Lee, J., Choi, Y. L., Jang, H. L., Yi, J. H., Baek, K. K., Park, S. H., et al. (2011). Impact of KRAS mutations on clinical outcomes in pancreatic cancer patients treated with first-line gemcitabine-based chemotherapy. Molecular Cancer Therapeutics, 10, 1993–1999.
Fernandez-Medarde, E., & Santos. (2011). Ras in cancer and developmental diseases. Genes & Cancer, 2, 344–358.
Pylayeva-Gupta, Y., Grabocka, E., & Bar-Sagi, D. (2011). RAS oncogenes: weaving a tumorigenic web. Nature Reviews. Cancer, 11, 761–774.
Tites, E. C. S., & Chandran, K. S. R. (2009). A systems perspective of ras signaling in cancer. Clinical Cancer Research, 15, 1510–1513.
Forbes, S. A., Bindal, N., Bamford, S., Cole, C., Kok, C. Y., Beare, D., Jia, M., Shepherd, R., Leung, K., Menzies, A., Teague, J. W., Campbell, P. J., Stratton, M. R., & Futreal, P. A. (2011). COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Research, 39, D945–D950.
Jones, S., Zhang, X., Parsons, D. W., et al. (2008). Core signaling pathways in human pancreatic cancers revealed by global genomic analyses. Science., 321(5897), 1801–1806.
Hruban, R. H., van Mansfeld, A. D., Offerhaus, G. J., et al. (1993). K-ras oncogene activation in adenocarcinoma of the human pancreas: a study of 82 carcinomas using a combination of mutant-enriched polymerase chain reaction analysis and allele-specific oligonucleotide hybridization. The American Journal of Pathology, 143(2), 545–554.
Caldas, S. A., Hahn, R. H., Hruban, M. S., & Redston, C. J. (1994). Detection of K-ras mutations in the stool of patients with pancreatic adenocarcinoma and pancreatic ductal hyperplasia. Cancer Research, 54, 3568–3573.
Kim, J., Reber, H. A., Dry, S. M., Elashoff, D., Chen, S. L., Umetani, N., Kitago, M., Hines, O. J., Kazanjian, K. K., Hiramatsu, S., Bilchik, A. J., Yong, S., Shoup, M., & Hoon, D. S. (2006). Unfavourable prognosis associated with K-ras gene mutation in pancreatic cancer surgical margins. Gut, 55, 1598–1605.
Kawesha, A., Ghaneh, P., Andren-Sandberg, A., Ograed, D., Skar, R., Dawiskiba, S., Evans, J. D., Campbell, F., Lemoine, N., & Neoptolemos, J. P. (2000). K-ras oncogene subtype mutations are associated with survival but not expression of p53 p16(INK4A), p21(WAF-1), cyclin D1, erbB-2 and erbB-3 in resected pancreatic ductal adenocarcinoma. International Journal of Cancer, 89, 469–474.
RM, Ferrone, C. R., Mullarky, E., Shyh-Chang, N., Kang, Y., Fleming, J. B., Bardeesy, N., Asara, J. M., Haigis, M. C., De Pinho, R. A., Cantley, L. C., & Kimmelman, A. C. (2013). Glutamine supports pancreatic cancer growth through a KRAS-regulated metabolic pathway. Nature, 496, 101–105.
Kawesha, A., Ghaneh, P., Andren-Sandberg, A., Ograed, D., Skar, R., Dawiskiba, S., Evans, J. D., Campbell, F., Lemoine, N., & Neoptolemos, J. P. (2000). K-ras oncogene subtype mutations are associated with survival but not expression of p53 p16(INK4A), p21(WAF-1), cyclin D1, erbB-2 and erbB-3 in resected pancreatic ductal adenocarcinoma. International Journal of Cancer, 89, 469–474.
Immervoll, H., Hoem, D., Kugarajh, K., Steine, S. J., & Molven, A. (2006). Molecular analysis of the EGFR-RAS-RAF pathway in pancreatic ductal adenocarcinomas: lack of mutations in the BRAF and EGFR genes. Virchows Archiv, 448, 788–796.
Chen, H., Tu, H., Meng, Z. Q., Chen, Z., Wang, P., & Liu, L. M. (2010). K-ras mutational status predicts poor prognosis in unresectable pancreatic cancer. European Journal of Surgical Oncology, 36, 657–662.
Reza, J., Almodovar, A. J., Srivastava, M., Veldhuis, P. P., Patel, S., Fanaian, N. I., Zhu, X., Litherland, S. A., & Arnoletti, J. P. (2019). K-RAS mutant gene found in pancreatic juice activated chromatin from peri-ampullary adenocarcinomas. Epigenetics Insights., 12, 2516865719828348.
Glorieux, C., & Huang, P. (2019). Regulation of CD137 expression through K-Ras signalling in pancreatic cancer cells. Cancer Communications, 39(1), 41.
Nishizawa, N., Kumamoto, Y., Katoh, H., Ushiku, H., Yokoi, K., Tanaka, T., Ishii, S., Igarashi, K., Tajima, H., Kaizu, T., & Yoshida, T. (2019). Dissected peripancreatic tissue margin is a critical prognostic factor and is associated with a K-ras gene mutation in pancreatic ductal adenocarcinoma. Oncology Letters, 17(2), 2141–2150.
Adjei, A. A. (2001). Blocking oncogenic Ras signaling for cancer therapy. Journal of the National Cancer Institute, 93, 1062–1074.
Martin, N. E., Brunner, T. B., Kiel, K. D., DeLaney, T. F., Regine, W. F., Mohiuddin, M., Rosato, E. F., Haller, D. G., Stevenson, J. P., Smith, D., Pramanik, B., Tepper, J., Tanaka, W. K., Morrison, B., Deutsch, P., Gupta, A. K., Muschel, R. J., McKenna, W. G., Bernhard, E. J., & Hahn, S. M. (2004). A phase I trial of the dual farnesyltransferase and geranylgeranyltransferase inhibitor L-778,123 and radiotherapy for locally advanced pancreatic cancer. Clinical Cancer Research, 10, 5447–5454.
Chao, M. W., Chang, L. H., Tu, H. J., Chang, C. D., Lai, M. J., Chen, Y. Y., Liou, J. P., Teng, C. M., & Pan, S. L. (2019). Combination treatment strategy for pancreatic cancer involving the novel HDAC inhibitor MPT0E028 with a MEK inhibitor beyond K-Ras status. Clinical Epigenetics, 11(1), 85.
Dent, P., Booth, L., Roberts, J. L., Liu, J., Poklepovic, A., Lalani, A. S., Tuveson, D., Martinez, J., & Hancock, J. F. (2019). Neratinib inhibits Hippo/YAP signaling, reduces mutant K-RAS expression, and kills pancreatic and blood cancer cells. Oncogene., 38(30), 5890–5904.
Lane, D. P. (1992). Cancer. p53, guardian of the genome. Nature., 358, 15–16.
Jay, G., Khoury, G., DeLeo, A. B., Dippold, W. G., & Old, L. J. (1981). p53 transformation-related protein: detection of an associated phosphotransferase activity. Proceedings of the National Academy of Sciences, 78(5), 2932–2936.
Oren, M. (2003). Decision making by p53: life, death and cancer. Cell Death and Differentiation, 10(4), 431.
Vogelstein, B., Lane, D., & Levine, A. J. (2000). Surfing the p53 network. Nature., 408(6810), 307.
El-Deiry, W. S., Kern, S. E., Pietenpol, J. A., Kinzler, K. W., & Vogelstein, B. (1992). Definition of a consensus binding site for p53. Nature Genetics, 1(1), 45.
Li, M., He, Y., Dubois, W., Wu, X., Shi, J., & Huang, J. (2012). Distinct regulatory mechanisms and functions for p53-activated and p53-repressed DNA damage response genes in embryonic stem cells. Molecular Cell, 46(1), 30–42.
Waldman, T., Kinzler, K. W., & Vogelstein, B. (1995). p21 is necessary for the p53-mediated G1 arrest in human cancer cells. Cancer Research, 55(22), 5187–5190.
Polyak, K., Xia, Y., Zweier, J. L., Kinzler, K. W., & Vogelstein, B. (1997). A model for p53-induced apoptosis. Nature., 389(6648), 300.
Donehower, L. A., Harvey, M., Slagle, B. L., McArthur, M. J., Montgomery Jr., C. A., Butel, J. S., & Bradley, A. (1992). Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature., 356(6366), 215.
Ruggeri, B., Zhang, S., Caamano, J., et al. (1992). Human pancreatic carcinomas and cell lines reveal frequent and multiple alterations in the p53 and Rb-1 tumor suppressor genes. Oncogene, 7(8), 1503–1511.
Birch, J. M., Alston, R. D., McNally, R., et al. (2001). Relative frequency and morphology of cancers in carriers of germline TP53 mutations. Oncogene, 20(34), 4621–4628.
Casey, G., Yamanaka, Y., Friess, H., et al. (1993). p53 mutations are common in pancreatic cancer and are absent in chronic pancreatitis. Cancer Letters, 69(3), 151–160.
DiGiuseppe, J. A., Hruban, R. H., Goodman, S. N., Polak, M., Van Den Berg, F. M., Allison, D. C., Cameron, J. L., Johan, A., & Offerhaus, G. (1994). Overexpression of p53 protein in adenocarcinoma of the pancreas. American Journal of Clinical Pathology, 101(6), 684–688.
Redston, M. S., Caldas, C., Seymour, A. B., Hruban, R. H., Da Costa, L., Yeo, C. J., & Kern, S. E. (1994). p53 mutations in pancreatic carcinoma and evidence of common involvement of homocopolymer tracts in DNA microdeletions. Cancer Research, 54(11), 3025–3033.
Casey, G., Yamanaka, Y., Friess, H., Kobrin, M. S., Lopez, M. E., Buchler, M., Beger, H. G., & Korc, M. (1993). p53 mutations are common in pancreatic cancer and are absent in chronic pancreatitis. Cancer Letters, 69(3), 151–160.
Izetti, P., Hautefeuille, A., Abujamra, A. L., et al. (2014). PRIMA-1, a mutant p53 reactivator, induces apoptosis and enhances chemotherapeutic cytotoxicity in pancreatic cancer cell lines. Investigational New Drugs, 32(5), 783–794.
Azmi, A. S., Philip, P. A., Wang, Z., et al. (2010). Reactivation of p53 by novel MDM2 inhibitors: implications for pancreatic cancer therapy. Current Cancer Drug Targets, 10(3), 319.
Mello, S. S., Valente, L. J., Raj, N., Seoane, J. A., Flowers, B. M., McClendon, J., Bieging-Rolett, K. T., Lee, J., Ivanochko, D., Kozak, M. M., & Chang, D. T. (2017). A p53 super-tumor suppressor reveals a tumor suppressive p53-Ptpn14-Yap axis in pancreatic cancer. Cancer Cell, 32(4), 460–473.
Delma, C. R., Thirugnanasambandan, S., Srinivasan, G. P., Raviprakash, N., Manna, S. K., Natarajan, M., & Aravindan, N. (2019). Fucoidan from marine brown algae attenuates pancreatic cancer progression by regulating p53–NFκB crosstalk. Phytochemistry., 167, 112078.
Cheng, J., Okolotowicz, K. J., Ryan, D., Mose, E., Lowy, A. M., & Cashman, J. R. (2019). Inhibition of invasive pancreatic cancer: restoring cell apoptosis by activating mitochondrial p53. American Journal of Cancer Research, 9(2), 390.
Long, J., Liu, Z., & Hui, L. (2019). Anti-tumor effect and mechanistic study of elemene on pancreatic carcinoma. BMC Complementary and Alternative Medicine, 19(1), 133.
Stott, F. J., Bates, S., James, M. C., et al. (1998). The alternative product from the human CDKN2a locus, p14 (ARF), participates in a regulatory feedback loop with p53 and MDM2. The EMBO Journal, 17, 5001–5014.
Serrano, M., Hannon, G. J., & Beach, D. (1993). A new regulatory motif in cell-cycle control causing specific inhibition of cyclin D/CDK4. Nature, 366(6456), 704–707.
Liggett Jr., W. H., & Sidransky, D. (1998). Role of the p16 tumor suppressor gene in cancer. Journal of Clinical Oncology, 16(3), 1197–1206.
Stott, F. J., Bates, S., James, M. C., McConnell, B. B., Starborg, M., Brookes, S., Palmero, I., Ryan, K., Hara, E., Vousden, K. H., & Peters, G. (1998). The alternative product from the human CDKN2A locus, p14ARF, participates in a regulatory feedback loop with p53 and MDM2. The EMBO Journal., 17(17), 5001–5014.
Fukushima, N., Sato, N., Ueki, T., Rosty, C., Walter, K. M., Wilentz, R. E., Yeo, C. J., Hruban, R. H., & Goggins, M. (2002). Aberrant methylation of preproenkephalin and p16 genes in pancreatic intraepithelial neoplasia and pancreatic ductal adenocarcinoma. The American Journal of Pathology., 160(5), 1573–1581.
Gerdes, B., Ramaswamy, A., Kersting, M., Ernst, M., Lang, S., Schuermann, M., Wild, A., & Bartsch, D. K. (2001). p16INK4a alterations in chronic pancreatitis—indicator for high-risk lesions for pancreatic cancer. Surgery., 129(4), 490–497.
Schutte, M., Hruban, R. H., Geradts, J., Maynard, R., Hilgers, W., Rabindran, S. K., Moskaluk, C. A., Hahn, S. A., Schwarte-Waldhoff, I., Schmiegel, W., & Baylin, S. B. (1997). Abrogation of the Rb/p16 tumor-suppressive pathway in virtually all pancreatic carcinomas. Cancer Research, 57(15), 3126–3130.
Chen, J., Li, D., Killary, A. M., Sen, S., Amos, C. I., Evans, D. B., Abbruzzese, J. L., & Frazier, M. L. (2009). Polymorphisms of p16, p27, p73, and MDM2 modulate response and survival of pancreatic cancer patients treated with preoperative chemoradiation. Annals of Surgical Oncology, 16(2), 431.
Attri, J., Srinivasan, R., Majumdar, S., Radotra, B. D., & Wig, J. (2005). Alterations of tumor suppressor gene p16 INK4a in pancreatic ductal carcinoma. BMC Gastroenterology, 5(1), 22.
Loukopoulos, P., Kanetaka, K., Takamura, M., Shibata, T., Sakamoto, M., & Hirohashi, S. (2004). Orthotopic transplantation models of pancreatic adenocarcinoma derived from cell lines and primary tumors and displaying varying metastatic activity. Pancreas., 29(3), 193–203.
Klump, B., Hsieh, C. J., Nehls, O., Dette, S., Holzmann, K., Kiesslich, R., Jung, M., Sinn, U., Ortner, M., Porschen, R., & Gregor, M. (2003). Methylation status of p14ARF and p16INK4a as detected in pancreatic secretions. British Journal of Cancer, 88(2), 217.
Heilmann, A. M., Perera, R. M., Ecker, V., Nicolay, B. N., Bardeesy, N., Benes, C. H., & Dyson, N. J. (2014). CDK4/6 and IGF1 receptor inhibitors synergize to suppress the growth of p16INK4A-deficient pancreatic cancers. Cancer Research, 74(14), 3947–3958.
Heilmann, A. M., Perera, R. M., Ecker, V., Nicolay, B. N., Bardeesy, N., Benes, C. H., & Dyson, N. J. (2014). CDK4/6 and IGF1 receptor inhibitors synergize to suppress the growth of p16INK4A-deficient pancreatic cancers. Cancer Research, 74(14), 3947–3958.
Al Baghdadi, T., Halabi, S., Garrett-Mayer, E., Mangat, P. K., Ahn, E. R., Sahai, V., Alvarez, R. H., Kim, E. S., Yost, K. J., Rygiel, A. L., & Antonelli, K. R. (2019). Palbociclib in patients with pancreatic and biliary cancer with CDKN2A alterations: results from the Targeted Agent and Profiling Utilization Registry Study. JCO Precision Oncology, 14.
Hahn, S. A., Schutte, M., Hoque, A. S., Moskaluk, C. A., Da Costa, L. T., Rozenblum, E., Weinstein, C. L., Fischer, A., Yeo, C. J., Hruban, R. H., & Kern, S. E. (1996). DPC4, a candidate tumor suppressor gene at human chromosome 18q21. 1. Science., 271(5247), 350–353.
Massagué, J. (1996). TGFβ signaling: receptors, transducers, and Mad proteins. Cell., 85(7), 947–950.
Saiki, Y., & Horii, A. (2014). Molecular pathology of pancreatic cancer. Pathology International, 64(1), 10–19.
Derynck, R., Akhurst, R. J., & Balmain, A. (2001). TGF-β signaling in tumor suppression and cancer progression. Nature Genetics, 29(2), 117.
Shi, Y., & Massagué, J. (2003). Mechanisms of TGF-β signaling from cell membrane to the nucleus. Cell, 113(6), 685–700.
Evan, G. I., & Vousden, K. H. (2001). Proliferation, cell cycle and apoptosis in cancer. Nature, 411(6835), 342.
Lecanda, J., Ganapathy, V., D’Aquino-Ardalan, C., Evans, B., Cadacio, C., Ayala, A., & Gold, L. I. (2009). TGFβ prevents proteasomal degradation of the cyclin-dependent kinase inhibitor p27kip1 for cell cycle arrest. Cell Cycle, 8(5), 742–756.
Massagué, J., Blain, S. W., & Lo, R. S. (2000). TGFβ signaling in growth control, cancer, and heritable disorders. Cell., 103(2), 295–309.
De Bosscher, K., Hill, C. S., & Nicolás, F. J. (2004). Molecular and functional consequences of Smad4 C-terminal missense mutations in colorectal tumour cells. The Biochemical Journal, 379(1), 209–216.
Blackford, A., Serrano, O. K., Wolfgang, C. L., Parmigiani, G., Jones, S., Zhang, X., Parsons, D. W., Lin, J. C., Leary, R. J., Eshleman, J. R., & Goggins, M. (2009). SMAD4 gene mutations are associated with poor prognosis in pancreatic cancer. Clinical Cancer Research, 15(14), 4674–4679.
Singh, P., Srinivasan, R., & Wig, J. D. (2012). SMAD4 genetic alterations predict a worse prognosis in patients with pancreatic ductal adenocarcinoma. Pancreas., 41(4), 541–546.
Hayashi, H., Kohno, T., Ueno, H., Hiraoka, N., Kondo, S., Saito, M., Shimada, Y., Ichikawa, H., Kato, M., Shibata, T., et al. (2017). Utility of assessing the number of mutated KRAS, CDKN2A, Tp53, and SMAD4 genes using a targeted deep sequencing assay as a prognostic biomarker for pancreatic cancer. Pancreas, 46, 335–340.
Wang, J. D., Jin, K., Chen, X. Y., Lv, J. Q., & Ji, K. W. (2017). Clinicopathological significance of SMAD4 loss in pancreatic ductal adenocarcinomas: a systematic review and meta-analysis. Oncotarget., 8(10), 16704.
Hao, J., Zhang, S., Zhou, Y., Liu, C., Hu, X., & Shao, C. (2011). MicroRNA 421 suppresses DPC4/Smad4 in pancreatic cancer. Biochemical and Biophysical Research Communications, 406(4), 552–557.
Wang, F., Xia, X., Yang, C., Shen, J., Mai, J., Kim, H. C., Kirui, D., Kang, Y. A., Fleming, J. B., Koay, E. J., & Mitra, S. (2018). SMAD4 gene mutation renders pancreatic cancer resistance to radiotherapy through promotion of autophagy. Clinical Cancer Research, 24(13), 3176–3185.
Yamada, S., Fujii, T., Shimoyama, Y., Kanda, M., Nakayama, G., Sugimoto, H., Koike, M., Nomoto, S., Fujiwara, M., Nakao, A., & Kodera, Y. (2015). SMAD4 expression predicts local spread and treatment failure in resected pancreatic cancer. Pancreas., 44(4), 660–664.
Feig, C., Gopinathan, A., Neesse, A., Chan, D. S., Cook, N., & Tuveson, D. A. (2012). The pancreas cancer microenvironment. Clinical Cancer Research, 18(16), 4266–4276.
Bapat, A. A., Hostetter, G., Von Hoff, D. D., & Han, H. (2011). Perineural inva-sion and associated pain in pancreatic cancer. Nature Reviews. Cancer, 11(10), 695–707.
Warburg, O. (1956). Origin of cancer cells. Oncologia, 9(2), 75–83.
Feldmann, G., Beaty, R., Hruban, R. H., & Maitra, A. (2007). Molecular genetics of pancreatic intraepithelial neoplasia. J Hepatobiliary Pan-creat Surg, 14(3), 224–232.
Bryant, K. L., Mancias, J. D., Kimmelman, A. C., & Der, C. J. (2014). KRAS: feed-ing pancreatic cancer proliferation. Trends in Biochemical Sciences, 39(2), 91–100.
Gaglio, D., Metallo, C. M., Gameiro, P. A., Hiller, K., Danna, L. S., Balestrieri, C., Alberghina, L., Stephanopoulos, G., & Chiaradonna, F. (2011). Oncogenic K-Ras decouples glucose and glutamine metabolism to support cancer cell growth. Molecular Systems Biology, 7, 523.
Dell’ Antone, P. (2012). Energy metabolism in cancer cells: how to explain the Warburg and Crabtree effects? Medical Hypotheses, 79(3), 388–392.
Ying, H., Kimmelman, A. C., Lyssiotis, C. A., Hua, S., Chu, G. C., Fletcher-Sananikone, E., Locasale, J. W., Son, J., Zhang, H., Coloff, J. L., Yan, H., Wang, W., Chen, S., Viale, A., Zheng, H., Paik, J. H., Lim, C., Guimaraes, A. R., Martin, E. S., Chang, J., Hezel, A. F., Perry, S. R., Hu, J., Gan, B., Xiao, Y., Asara, J. M., Weissleder, R., Wang, Y. A., Chin, L., Cantley, L. C., et al. (2012). Oncogenic Kras maintains pancreatic tumors through regulation of anabolic glucose metabolism. Cell, 149(3), 656–670.
Ma, Z., Vocadlo, D. J., & Vosseller, K. (2013). Hyper-O-GlcNAcylation is anti-apoptotic and maintains constitutive NF-kappaB activity in pan-creatic cancer cells. The Journal of Biological Chemistry, 288(21), 15121–15130.
Boros, L. G., Puigjaner, J., Cascante, M., Lee, W. N., Brandes, J. L., Bassilian, S., Yusuf, F. I., Williams, R. D., Muscarella, P., Melvin, W. S., & Schirmer, W. J. (1997). Oxythiamine and dehydroepiandrosterone inhibit the nonoxidative synthesis of ribose and tumor cell proliferation. Cancer Research, 57(19), 4242–4248.
Butera, G., Pacchiana, R., Mullappilly, N., Margiotta, M., Bruno, S., Conti, P., Riganti, C., & Donadelli, M. (2018). Mutant p53 prevents GAPDH nuclear translocation in pancreatic cancer cells favoring glycolysis and 2-deoxyglucose sensitivity. Biochimica et Biophysica Acta, Molecular Cell Research, 1865(12), 1914–1923.
Schofield, H. K., Zeller, J., Espinoza, C., Halbrook, C. J., Del Vecchio, A., Magnuson, B., Fabo, T., Daylan, A. E. C., Kovalenko, I., Lee, H. J., Yan, W., Feng, Y., Karim, S. A., Kremer, D. M., Kumar-Sinha, C., Lyssiotis, C. A., Ljungman, M., Mor-ton, J. P., Galban, S., Fearon, E. R., & Pasca di Magliano, M. (2018). Mutant p53R270H drives altered metabolism and increased invasion in pan-creatic ductal adenocarcinoma. JCI Insight, 3(2), 97422.
Guillaumond, F., Leca, J., Olivares, O., Lavaut, M. N., Vidal, N., Berthezene, P., Dusetti, N. J., Loncle, C., Calvo, E., Turrini, O., Iovanna, J. L., Tomasini, R., & Vasseur, S. (2013). Strengthened glycolysis under hypoxia supports tumor symbiosis and hexosamine biosynthesis in pancreatic adeno-carcinoma. Proceedings of the National Academy of Sciences of the United States of America, 110(10), 3919–3924.
Baek, G., Tse, Y. F., Hu, Z., Cox, D., Buboltz, N., McCue, P., Yeo, C. J., White, M. A., DeBerardinis, R. J., Knudsen, E. S., & Witkiewicz, A. K. (2014). MCT4 defines a glycolytic subtype of pancreatic cancer with poor prognosis and unique metabolic dependencies. Cell Reports, 9(6), 2233–2249.
Chaika, N. V., Gebregiworgis, T., Lewallen, M. E., Purohit, V., Radhakrish-nan, P., Liu, X., Zhang, B., Mehla, K., Brown, R. B., Caffrey, T., Yu, F., Johnson, K. R., Powers, R., Hollingsworth, M. A., & Singh, P. K. (2012). MUC1 mucin stabilizes and activates hypoxia-inducible factor 1 alpha to regulate metabolism in pancreatic cancer. Proceedings of the National Academy of Sciences of the United States of America, 109(34), 13787–13792.
Shi, M., Cui, J., Du, J., Wei, D., Jia, Z., Zhang, J., Zhu, Z., Gao, Y., & Xie, K. (2014). A novel KLF4/LDHA signaling pathway regulates aerobic glycolysis in and progression of pancreatic cancer. Clinical Cancer Research, 20(16), 4370–4380.
Swierczynski, J., Hebanowska, A., & Sledzinski, T. (2014). Role of abnor-mal lipid metabolism in development, progression, diagnosis and therapy of pancreatic cancer. World Journal of Gastroenterology, 20(9), 2279–2303.
Hatzivassiliou, G., Zhao, F., Bauer, D. E., Andreadis, C., Shaw, A. N., Dhanak, D., Hingorani, S. R., Tuveson, D. A., & Thompson, C. B. (2005). ATP citrate lyase inhibition can suppress tumor cell growth. Cancer Cell, 8(4), 311–321.
Takahashi, M., Hori, M., Ishigamori, R., Mutoh, M., Imai, T., & Nakagama, H. (2018). Fatty pancreas: a possible risk factor for pancreatic cancer in animals and humans. Cancer Science, 109(10), 3013–3023.
Waddington, C. H. (1942). The epigenotype. Endeavour., 1, 18–20.
Bonasio, R., Tu, S., & Reinberg, D. (2010). Molecular signals of epigenetic states. Science, 330(6004), 612–616.
Berger, S. L., Kouzarides, T., Shiekhattar, R., & Shilatifard, A. (2009). An operational definition of epigenetics. Genes & Development, 23(7), 781–783.
Okano, M., Xie, S., & Li, E. (1998). Cloning and characterization of a family of novel mammalian DNA (cytosine-5) methyltransferases. Nature Genetics, 19(3), 219–220.
Yen, R. W., Vertino, P. M., Nelkin, B. D., et al. (1992). Isolation and characterization of the cDNA encoding human DNA methyltransferase. Nucleic Acids Research, 20(9), 2287–2291.
Li, A., Omura, N., Hong, S. M., & Goggins, M. (2010). Pancreatic cancer DNMT1 expression and sensitivity to DNMT1 inhibitors. Cancer Biology & Therapy, 9(4), 321–329.
Yoder, J. A., Walsh, C. P., & Bestor, T. H. (1997). Cytosine methylation and the ecology of intragenomic parasites. Trends in Genetics, 13(8), 335–340.
McCabe, M. T., Brandes, J. C., & Vertino, P. M. (2009). Cancer DNA methylation: molecular mechanisms and clinical implications. Clinical Cancer Research, 15(12), 3927–3937.
Saxonov, S., Berg, P., & Brutlag, D. L. (2006). A genome-wide analysis of CpG dinucleotides in the human genome distinguishes two distinct classes of promoters. Proceedings of the National Academy of Sciences, 103(5), 1412–1417.
Coulondre, C., Miller, J. H., Farabaugh, P. J., & Gilbert, W. (1978). Molecular basis of base substitution hotspots in Escherichia coli. Nature., 274(5673), 775.
Hendrich, B., Hardeland, U., Ng, H. H., Jiricny, J., & Bird, A. (2000). correction: The thymine glycosylase MBD4 can bind to the product of deamination at methylated CpG sites. Nature, 404(6777), 525.
Walsh, C. P., & Xu, G. L. Cytosine methylation and DNA repair. InDNA Methylation: Basic Mechanisms 2006 (pp. 283-315). Springer, Berlin. Heidelberg.
Coetzee, G. A., Olumi, A. F., Spruck, C. H., & Jones, P. A. (1991). 5-Methylcytosine as an endogenous mutagen in the p53 tumor suppressor gene. InPrincess Takamatsu Symposia, 22, 207–219.
Morgan, H. D., Santos, F., Green, K., Dean, W., & Reik, W. (2005). Epigenetic reprogramming in mammals. Human Molecular Genetics, 14(suppl_1), R47–R58.
Bhutani, N., Burns, D. M., & Blau, H. M. (2011). DNA demethylation dynamics. Cell., 146(6), 866–872.
Ito, S., D’Alessio, A. C., Taranova, O. V., Hong, K., Sowers, L. C., & Zhang, Y. (2010). Role of Tet proteins in 5mC to 5hmC conversion, ES-cell self-renewal and inner cell mass specification. Nature., 466(7310), 1129.
Li, J., Zhu, J., Hassan, M. M., Evans, D. B., Abbruzzese, J. L., & Li, D. (2007). K-ras mutation and p16 and preproenkephalin promoter hypermethylation in plasma DNA of pancreatic cancer patients: in relation to cigarette smoking. Pancreas., 34(1), 55.
Tang, B., Li, Y., Qi, G., Yuan, S., Wang, Z., Yu, S., Li, B., & He, S. (2015). Clinicopathological significance of CDKN2A promoter hypermethylation frequency with pancreatic cancer. Scientific Reports, 5, 13563.
Matsuoka, S., Edwards, M. C., Bai, C., et al. (1995). p57KIP2, a structurally distinct member of the p21CIP1 Cdk inhibitor family, is a candidate tumor suppressor gene. Genes & Development, 9(6), 650–662.
Sato, N., Matsubayashi, H., Abe, T., Fukushima, N., & Goggins, M. (2005). Epigenetic down-regulation of CDKN1C/p57KIP2 in pancreatic ductal neoplasms identified by gene expression profiling. Clinical Cancer Research, 11(13), 4681–4688.
Sherr, C. J. (1995). D-type cyclins. Trends in Biochemical Sciences, 20(5), 187–190.
Meyyappan, M., Wong, H., Hull, C., & Riabowol, K. T. (1998). Increased expression of cyclin D2 during multiple states of growth arrest in primary and established cells. Molecular and Cellular Biology, 18(6), 3163–3172.
Terris, B., Blaveri, E., Crnogorac-Jurcevic, T., Jones, M., Missiaglia, E., Ruszniewski, P., Sauvanet, A., & Lemoine, N. R. (2002). Characterization of gene expression profiles in intraductal papillary-mucinous tumors of the pancreas. The American Journal of Pathology., 160(5), 1745–1754.
Matsubayashi, H., Sato, N., Fukushima, N., Yeo, C. J., Walter, K. M., Brune, K., Sahin, F., Hruban, R. H., & Goggins, M. (2003). Methylation of cyclin D2 is observed frequently in pancreatic cancer but is also an age-related phenomenon in gastrointestinal tissues. Clinical Cancer Research, 9(4), 1446–1452.
Li, J., Zhu, J., Hassan, M. M., Evans, D. B., Abbruzzese, J. L., & Li, D. (2007). K-ras mutation and p16 and preproenkephalin promoter hypermethylation in plasma DNA of pancreatic cancer patients: in relation to cigarette smoking. Pancreas., 34(1), 55.
Zagon, I. S., Roesener, C. D., Verderame, M. F., Ohlsson-Wilhelm, B. M., Levin, R. J., & McLaughlin, P. J. (2000). Opioid growth factor regulates the cell cycle of human neoplasias. International Journal of Oncology, 17(5), 1053–1114.
Comb, M., & Goodman, H. M. (1990). CpG methylation inhibits proenkephalin gene expression and binding of the transcription factor AP-2. Nucleic Acids Research, 18(13), 3975–3982.
Fukushima, N., Sato, N., Ueki, T., Rosty, C., Walter, K. M., Wilentz, R. E., Yeo, C. J., Hruban, R. H., & Goggins, M. (2002). Aberrant methylation of preproenkephalin and p16 genes in pancreatic intraepithelial neoplasia and pancreatic ductal adenocarcinoma. The American Journal of Pathology., 160(5), 1573–1581.
Wen, Z., Zhong, Z., & Darnell Jr., J. E. (1995). Maximal activation of transcription by Statl and Stat3 requires both tyrosine and serine phosphorylation. Cell., 82(2), 241–250.
Naka, T., Narazaki, M., Hirata, M., Matsumoto, T., Minamoto, S., Aono, A., Nishimoto, N., Kajita, T., Taga, T., Yoshizaki, K., & Akira, S. (1997). Structure and function of a new STAT-induced STAT inhibitor. Nature., 387(6636), 924.
Komazaki, T., Nagai, H., Emi, M., Terada, Y., Yabe, A., Jin, E., Kawanami, O., Konishi, N., Moriyama, Y., Naka, T., & Kishimoto, T. (2004). Hypermethylation-associated inactivation of the SOCS-1 gene, a JAK/STAT inhibitor, in human pancreatic cancers. Japanese Journal of Clinical Oncology, 34(4), 191–194.
Mah, K. M., & Weiner, J. A. (2017). Regulation of Wnt signaling by protocadherins. InSeminars in Cell & Developmental Biology, 69, 158–171 Academic Press.
Vincent, A., Omura, N., Hong, S. M., Jaffe, A., Eshleman, J., & Goggins, M. (2011). Genome-wide analysis of promoter methylation associated with gene expression profile in pancreatic adenocarcinoma. Clinical Cancer Research, 17(13), 4341–4354.
Curia, M. C., Fantini, F., Lattanzio, R., Tavano, F., Di Mola, F., Piantelli, M., Battista, P., Di Sebastiano, P., & Cama, A. (2019). High methylation levels of PCDH10 predict poor prognosis in patients with pancreatic ductal adenocarcinoma. BMC Cancer, 19(1), 452.
Christoffels, V. M., Keijser, A. G., Houweling, A. C., Clout, D. E., & Moorman, A. F. (2000). Patterning the embryonic heart: identification of five mouse Iroquois homeobox genes in the developing heart. Developmental Biology, 224(2), 263–274.
Chakma, K., Gu, Z., Motoi, F., Unno, M., Horii, A., & Fukushige, S. (2019). DNA hypermethylation of IRX4 is a frequent event that may confer growth advantage to pancreatic cancer cells., 01, 821–821.
Eissa, M. A., Lerner, L., Abdelfatah, E., Shankar, N., Canner, J. K., Hasan, N. M., Yaghoobi, V., Huang, B., Kerner, Z., Takaesu, F., & Wolfgang, C. (2019). Promoter methylation of ADAMTS1 and BNC1 as potential biomarkers for early detection of pancreatic cancer in blood. Clinical Epigenetics, 11(1), 59.
Sato, N., Fukushima, N., Matsubayashi, H., Iacobuzio-Donahue, C. A., Yeo, C. J., & Goggins, M. (2006). Aberrant methylation of Reprimo correlates with genetic instability and predicts poor prognosis in pancreatic ductal adenocarcinoma. Cancer., 107(2), 251–257.
Ueki, T., Toyota, M., Sohn, T., Yeo, C. J., Issa, J. P., Hruban, R. H., & Goggins, M. (2000). Hypermethylation of multiple genes in pancreatic adenocarcinoma. Cancer Research, 60(7), 1835–1839.
Sato, N., Fukushima, N., Maitra, A., Matsubayashi, H., Yeo, C. J., Cameron, J. L., Hruban, R. H., & Goggins, M. (2003). Discovery of novel targets for aberrant methylation in pancreatic carcinoma using high-throughput microarrays. Cancer Research, 63(13), 3735–3742.
Li, A., Omura, N., Hong, S. M., Vincent, A., Walter, K., Griffith, M., Borges, M., & Goggins, M. (2010). Pancreatic cancers epigenetically silence SIP1 and hypomethylate and overexpress miR-200a/200b in association with elevated circulating miR-200a and miR-200b levels. Cancer Research, 70(13), 5226–5237.
Sato, N., Fukushima, N., Maehara, N., Matsubayashi, H., Koopmann, J., Su, G. H., Hruban, R. H., & Goggins, M. (2003). SPARC/osteonectin is a frequent target for aberrant methylation in pancreatic adenocarcinoma and a mediator of tumor–stromal interactions. Oncogene., 22(32), 5021.
Omura, N., Li, C. P., Li, A., Hong, S. M., Walter, K., Jimeno, A., Hidalgo, M., & Goggins, M. (2008). Genome-wide profiling at methylated promoters in pancreatic adenocarcinoma. Cancer Biology & Therapy, 7(7), 1146–1156.
Li, J., Wu, H., Li, W., Yin, L., Guo, S., Xu, X., Ouyang, Y., Zhao, Z., Liu, S., Tian, Y., & Tian, Z. (2016). Downregulated miR-506 expression facilitates pancreatic cancer progression and chemoresistance via SPHK1/Akt/NF-κB signaling. Oncogene., 35(42), 5501.
Vincent, A., Omura, N., Hong, S. M., Jaffe, A., Eshleman, J., & Goggins, M. (2011). Genome-wide analysis of promoter methylation associated with gene expression profile in pancreatic adenocarcinoma. Clinical Cancer Research, 17(13), 4341–4354.
Thompson, M. J., Rubbi, L., Dawson, D. W., Donahue, T. R., & Pellegrini, M. (2015). Pancreatic cancer patient survival correlates with DNA methylation of pancreas development genes. PLoS One, 10(6), e0128814.
Gama-Sosa, M. A., Slagel, V. A., Trewyn, R. W., et al. (1983). The 5- methylcytosine content of DNA from human tumors. Nucleic Acids Research, 11, 6883–6894.
Feinberg, A. P., Vogelstein, B., et al. (1983). Hypomethylation distinguishes genes of some human cancers from their normal counterparts. Nature., 301, 89–92.
Rauch, T. A., Zhong, X., Wu, X., et al. (2008). High-resolution mapping of DNA hypermethylation and hypomethylation in lung cancer. Proceedings of the National Academy of Sciences of the United States of America, 105, 252–257.
Ehrlich, M. (2002). DNA methylation in cancer: too much, but also too little. Oncogene., 21, 5400–5413.
Ohike, N., Maass, N., Mundhenke, C., et al. (2003). Clinicopathological significance and molecular regulation of maspin expression in ductal adenocarcinoma of the pancreas. Cancer Letters, 199(2), 193–200.
Sato, N., Maitra, A., Fukushima, N., et al. (2003). Frequent hypomethylation of multiple genes overexpressed in pancreatic ductal adenocarcinoma. Cancer Research, 63(14), 4158–4166.
Chen, H., Kong, Y., Yao, Q., Zhang, X., Fu, Y., Li, J., Liu, C., & Wang, Z. (2019). Three hypomethylated genes were associated with poor overall survival in pancreatic cancer patients. Aging (Albany NY), 11(3), 885.
Zhu, Y., Zhang, J. J., Zhu, R., Zhu, Y., Liang, W. B., Gao, W. T., Yu, J. B., Xu, Z. K., & Miao, Y. (2011). The increase in the expression and hypomethylation of MUC4 gene with the progression of pancreatic ductal adenocarcinoma. Medical Oncology, 28(1), 175–184.
Sekine, H., Chen, N., Sato, K., Saiki, Y., Yoshino, Y., Umetsu, Y., Jin, G., Nagase, H., Gu, Z., Fukushige, S., & Sunamura, M. (2012). S100A4, frequently overexpressed in various human cancers, accelerates cell motility in pancreatic cancer cells. Biochemical and Biophysical Research Communications, 429(3-4), 214–219.
Feinberg, A. P., Koldobskiy, M. A., & Göndör, A. (2016). Epigenetic modulators, modifiers and mediators in cancer aetiology and progression. Nature Reviews. Genetics, 17(5), 284.
Abukiwan A, Berger MR. Epigenetics: dissecting gene expression alteration in PDAC. In Advances in DNA Repair 2018 Nov 5. IntechOpen.
Ramassone, A., Pagotto, S., Veronese, A., & Visone, R. (2018). Epigenetics and microRNAs in cancer. International Journal of Molecular Sciences, 19(2), 459.
Iguchi, E., Safgren, S. L., Marks, D. L., Olson, R. L., & Fernandez-Zapico, M. E. (2016). Focus: epigenetics: pancreatic cancer, a mis-interpreter of the epigenetic language. The Yale Journal of Biology and Medicine., 89(4), 575.
Fernandez, A. F., Assenov, Y., Martin-Subero, J. I., Balint, B., Siebert, R., Taniguchi, H., Yamamoto, H., Hidalgo, M., Tan, A. C., Galm, O., et al. (2012). A DNA methylation fingerprint of 1628 human samples. Genome Research, 22(2), 407–419.
Hao, X., Luo, H., Krawczyk, M., Wei, W., Wang, W., Wang, J., Flagg, K., Hou, J., Zhang, H., Yi, S., et al. (2017). DNA methylation markers for diagnosis and prognosis of common cancers. Proceedings of the National Academy of Sciences of the United States of America, 114(28), 7414–7419.
Rodríguez-Rodero, S., Fernández, A. F., Fernández-Morera, J. L., Castro-Santos, P., Bayon, G. F., Ferrero, C., Urdinguio, R. G., Gonzalez-Marquez, R., Suarez, C., Fernández-Vega, I., & Fresno Forcelledo, M. F. (2013). DNA methylation signatures identify biologically distinct thyroid cancer subtypes. The Journal of Clinical Endocrinology & Metabolism., 98(7), 2811–2821.
Baylin, S. B., & Jones, P. A. (2011). A decade of exploring the cancer epigenome – biological and translational implications. Nature Reviews. Cancer, 11(10), 726–734.
Moran, S., Martinez-Cardus, A., Sayols, S., Musulen, E., Balana, C., Estival-Gonzalez, A., Moutinho, C., Heyn, H., Diaz-Lagares, A., de Moura, M. C., et al. (2016). Epigenetic profiling to classify cancer of unknown primary: a multicentre, retrospective analysis. The Lancet Oncology, 17(10), 1386–1395.
Kanwal, R., & Gupta, S. (2012). Epigenetic modifications in cancer. Clinical Genetics, 81(4), 303–311.
Hosseini A, Minucci S (2018). Alterations of histone modifications in cancer. In: Epigenetics in human disease, vol. 6. 2nd ed; p. 141–217.
Baylin, S. B., & Jones, P. A. (2016). Epigenetic determinants of cancer. Cold Spring Harbor Perspectives in Biology, 8, 9.
Berdasco, M., & Esteller, M. (2018). Clinical epigenetics: seizing opportunities for translation. Nature Reviews. Genetics.
Rodriguez-Paredes, M., & Esteller, M. (2011). Cancer epigenetics reaches mainstream oncology. Nature Medicine, 17(3), 330–339.
Allis, C. D., & Jenuwein, T. (2016). The molecular hallmarks of epigenetic control. Nature Reviews. Genetics, 17(8), 487–500.
Herman, J. G., & Baylin, S. B. (2003). Gene silencing in cancer in association with promoter hypermethylation. The New England Journal of Medicine, 349(21), 2042–2054.
Palii, S. S., Van Emburgh, B. O., Sankpal, U. T., Brown, K. D., & Robertson, K. D. (2008). DNA methylation inhibitor 5-Aza-2′-deoxycytidine induces reversible genomewide DNA damage that is distinctly influenced by DNA methyltransferases 1 and 3B. Molecular and Cellular Biology, 28(2), 752–771.
Chiappinelli, K. B., Strissel, P. L., Desrichard, A., Li, H., Henke, C., Akman, B., Hein, A., Rote, N. S., Cope, L. M., Snyder, A., et al. (2015). Inhibiting DNA methylation causes an interferon response in cancer via dsRNA including endogenous retroviruses. Cell., 162(5), 974–986.
Roulois, D., Loo Yau, H., Singhania, R., Wang, Y., Danesh, A., Shen, S. Y., Han, H., Liang, G., Jones, P. A., Pugh, T. J., et al. (2015). DNA-demethylating agents target colorectal cancer cells by inducing viral mimicry by endogenous transcripts. Cell., 162(5), 961–973.
Xue, K., Gu, J. J., Zhang, Q., Mavis, C., Hernandez-Ilizaliturri, F. J., Czuczman, M. S., & Guo, Y. (2016). Vorinostat, a histone deacetylase (HDAC) inhibitor, promotes cell cycle arrest and re-sensitizes rituximab- and chemo-resistant lymphoma cells to chemotherapy agents. Journal of Cancer Research and Clinical Oncology, 142(2), 379–387.
Kronfol, M. M., Dozmorov, M. G., Huang, R., Slattum, P. W., & McClay, J. L. (2017). The role of epigenomics in personalized medicine. Expert Rev Precis Med Drug Dev., 2(1), 33–45.
Cameron, E. E., Bachman, K. E., Myohanen, S., Herman, J. G., & Baylin, S. B. (1999). Synergy of demethylation and histone deacetylase inhibition in the re-expression of genes silenced in cancer. Nature Genetics, 21(1), 103–107.
Juergens, R. A., Wrangle, J., Vendetti, F. P., Murphy, S. C., Zhao, M., Coleman, B., Sebree, R., Rodgers, K., Hooker, C. M., Franco, N., et al. (2011). Combination epigenetic therapy has efficacy in patients with refractory advanced non-small cell lung cancer. Cancer Discovery, 1(7), 598–607.
Jones, P. A., Issa, J. P., & Baylin, S. (2016). Targeting the cancer epigenome for therapy. Nature Reviews. Genetics, 17(10), 630–641.
Ezzati, M., Henley, S. J., Lopez, A. D., & Thun, M. J. (2005). Role of smoking in global and regional cancer epidemiology: current patterns and data needs. International Journal of Cancer, 116(6), 963–971.
Jarosz, M., Sekuła, W., & Rychlik, E. (2012). Influence of diet and tobacco smoking on pancreatic cancer incidence in Poland in 1960–2008. Gastroenterology Research and Practice, 2012.
Wang, Y. T., Gou, Y. W., Jin, W. W., Xiao, M., & Fang, H. Y. (2016). Association between alcohol intake and the risk of pancreatic cancer: a dose–response meta-analysis of cohort studies. BMC Cancer, 16(1), 212.
Jacobs, E. J., Chanock, S. J., Fuchs, C. S., LaCroix, A., McWilliams, R. R., Steplowski, E., Stolzenberg-Solomon, R. Z., Arslan, A. A., Bueno-de-Mesquita, H. B., Gross, M., & Helzlsouer, K. (2010). Family history of cancer and risk of pancreatic cancer: a pooled analysis from the Pancreatic Cancer Cohort Consortium (PanScan). International Journal of Cancer, 127(6), 1421–1428.
Davoodi, S. H., Malek-Shahabi, T., Malekshahi-Moghadam, A., Shahbazi, R., & Esmaeili, S. (2013). Obesity as an important risk factor for certain types of cancer. Iranian Journal of Cancer Prevention., 6(4), 186.
Aune, D., Greenwood, D. C., Chan, D. S., Vieira, R., Vieira, A. R., Navarro Rosenblatt, D. A., Cade, J. E., Burley, V. J., & Norat, T. (2011). Body mass index, abdominal fatness and pancreatic cancer risk: a systematic review and non-linear dose–response meta-analysis of prospective studies. Annals of Oncology, 23(4), 843–852.
Rawla, P., Sunkara, T., & Gaduputi, V. (2019). Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World Journal of Oncology., 10(1), 10.
Ghiorzo, P. (2014). Genetic predisposition to pancreatic cancer. World Journal of Gastroenterology, 20(31), 10778.
Funding
The study was supported by Natural Science Foundation China (Grant # 81702802) and Beijing Municipal Education Commission (Grant# KM201810005032 and Grant# KM201810005005).
Author information
Authors and Affiliations
Contributions
Aamir Ali Khan and Xinhui Liu conceive the idea and write manuscripts of this study. Muhammad Tahir and Xinlong Yan write the abstract and make tables, respectively. Aamir Ali Khan and Sakhawat Ali make the figures. Hua Huang and Xinlong Yan critically revise the manuscript and provide supervision.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participant/animals
No human participant or animal was involved in this study.
Informed consent
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khan, A.A., Liu, X., Yan, X. et al. An overview of genetic mutations and epigenetic signatures in the course of pancreatic cancer progression. Cancer Metastasis Rev 40, 245–272 (2021). https://doi.org/10.1007/s10555-020-09952-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09952-0