Abstract
Colorectal cancer is still a major health problem worldwide. Based on the most recent released data by the World Health Organization GLOBOCAN in 2012, colorectal cancer is the third most prevalent type of cancer in males and the second in females. In 1999, it was published the first report showing evidence of a strong correlation between diet and cancer incidence, being its positive or negative impact intimately linked to dietary patterns. A diet rich in fiber is associated with a low risk of developing colorectal cancer. The fermentation of the dietary fiber by intestinal microflora results in production of butyrate, which plays a plurifunctional role on the colonocytes, and it has also been reported as a chemopreventive agent. However, there are limited studies focusing its anti-cancer potential. Here, we review the recent new insights that focus butyrate and its role in colorectal cancer prevention and treatment, from its synthesis, metabolism, and transport, through its involvement on several cancer-related signaling pathways, to the novel existing approaches for its clinical use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Butyrate: synthesis, metabolism, and transport
Butyrate is a four-carbon naturally occurring short-chain fatty acid (SCFA), obtained by the intake of dietary fiber. This SCFA is produced by bacterial fermentation in the lumen of the colon, being in humans the direct quantification not so easy to determine [1, 2]. In healthy man, SCFA production contributes to the body energy needs, influencing the gastrointestinal function by providing energy-yielding substrates to the colonocytes, increasing or modifying intestinal mucosal growth, increasing colonic blood flow, and promoting sodium and water absorption. Thus, the SCFAs are described as having a key role in gut homeostasis maintenance and its epithelial integrity [2, 3].
The non-digested carbohydrates are exposed to the action of the hydrolytic bacteria which can produce extracellular cellulases, as well as other enzymes that can degrade the polysaccharides into oligosaccharides. Thereafter, the oligosaccharides are used by the hydrolytic bacteria or can be cross-fed to the non-hydrolytic bacteria that can convert the carbohydrate monomers, like pentoses or hexoses, through a variety of intermediates as butyrate, acetate, or propionate [1]. It is known that these fatty acids contribute to about 5–15 % of the total caloric requirements of humans and, under normal physiological conditions, the rate of absorption is in balance with the lumen production rate [4–6]. In fact, SCFA production, which is present at high levels (mM) in the colon lumen, allows the salvage of energy mainly from carbon sources such as the dietary fibers, which escape to digestion in the upper gastrointestinal tract and in the small intestine and reach the colon [5]. Concerning this, it is possible to evaluate SCFA concentration in human feces. However, this possibility is limited due to that more than 95 % of SCFAs are produced and absorbed within the colon [7]. Butyrate-producing bacteria carry out fermentative metabolism. These microorganisms gain energy in the form of ATP by substrate-level phosphorylation during the oxidative substrate breakdown. According with these reactions, the resulting reducing equivalents, NADH, are used for metabolic intermediates, leading to the formation of large amounts of reduced end products, such as butyrate [8]. Butyrate can be synthesized through four pathways (Fig. 1) and can be influenced by different factors, such as the type of limiting substrate and growth rate, tissue oxygen partial pressure, and the type of cell culture. Besides this, the presence of inorganic electron acceptors also promotes anaerobic respiration and aceto-/methanogenesis, which decreases the hydrogen partial pressure enabling more oxidizing fermentation products, such as acetate, and decreasing butyrate production [2].
All the four pathways merge at a central energy-generating step where crotonyl-CoA is transformed to butyryl-CoA, catalyzed by the butyryl-CoA dehydrogenase electron-transferring flavoprotein complex. After, butyryl-CoA is converted in butyrate performed by different butyryl-CoA transferases [2].
Considering butyrate synthesis through lysine, the l-lysine is converted to l-β-lysine (β-lysine), which is then converted to (3S, 5S)-3,5-diaminohexanoate. After, there occurs the deamination to a keto acid and the reaction with acetyl-CoA to form l-3-aminobutyryl-CoA and acetoacetate. l-3-Aminobutyryl-CoA is deaminated to crotonyl-CoA. The use of this pathway to obtain butyrate, as well as glutarate, shows that proteins can also have an important role in butyrate synthesis, demonstrating the adaptation of microbiota to different nutritional conditions and the maintenance of butyrate synthesis. Besides, it is important to refer that there are also other amino acids (like aspartate) that can be converted in butyrate [2].
The acetyl-CoA pathway is present in the majority of butyrate producers. In this case, the acetyl-CoA is converted into acetoacetyl-CoA by thiolase action, and after, through β-hydroxybutyryl-CoA, acetoacetyl-CoA is transformed in 3-hydroxy butanoyl-CoA. Later, this intermediate is converted in crotonyl-CoA by crotonase enzyme [2].
The glutarate pathway includes the transformation of 2-oxoglutarate in 2-hydroxyglutarate by 2-hydroxyglutarate dehydrogenase enzyme. This intermediate is then converted in 2-hydroxy-glutaryl-CoA by glutaconate-CoA transferase enzyme. After, the enzyme 2-hydroxy-glutaryl-CoA dehydrogenase converts the 2-hydroxy-glutaryl-CoA in glutaconyl-CoA which is after converted in crotonyl-CoA, in order to produce butyrate. In this reaction, glutaconyl-CoA decarboxylase is the enzyme responsible for it [2, 3].
The last pathway by which butyrate can be also produced is the 4-aminobutyrate/succinate pathway. In this pathway, succinate semialdehyde is converted in 4-hydroxy butyrate by 4-hydroxybutyrate dehydrogenase enzyme. After, it is possible to obtain 4-hydroxylbutyryl-CoA by hydroxybutyrate-CoA transferase. Vinylacetyl-CoA is then produced after 4-hydroxybutyryl-CoA enzyme action, and finally, through vinylacetyl-CoA enzyme action, crotonyl-CoA is produced in order to generate butyrate [2, 3].
All these four pathways contribute to butyrate production, being the diet the major factor that determines different gut shapes. Therefore, there is data describing that acetyl-CoA pathway is the main pathway of butyrate synthesis in healthy people [2, 3]. The composition of the fecal bacterial flora changes between individuals of different species and strains [9].
Concerning SCFA transport, there is segmental heterogeneity in the colon, possibly related to differences in sodium transport also observed in the colon [3]. However, it was increased when potassium is substituted by sodium in the luminal medium [2, 10–12].
Related to the mechanism for SCFA transport and absorption, there is disagreement among authors reporting some of them that the epithelial transport (Fig. 2) is insignificant [2, 11]. The first approach is the paracellular transport in contrast to the transcellular transport, being this type of transport related with the transference of substances across an epithelium. Therefore, through paracellular transport, the substance passes through the space between cells. This type of transport concerning SCFAs is supported by the fact that pH in the colon is between 6 and 7.5 whereby about 99 % of SCFAs will be dissociated (pKa = 4.8). Besides that, there is a high gradient created by its large luminal concentration above 100 mmol/l comparing with blood concentration, where it is below than 1 mmol/L, and a lumen-negative electrical potential. Both electrical and chemical features will favor net absorption [2, 3].
In contrast with paracellular transport, there is transcellular transport, a passive but selective variable and regulated transport. Transcellular SCFA transport can be demonstrated by the increased sodium absorption in the presence of luminal SCFAs [2, 3]. In the absence of an electrochemical gradient to stimulate SCFAs absorption, these molecules have to interact with the cells of the epithelium. As a consequence of this epithelium interaction, there is a stimulating effect of SCFAs on the ion transport which can be done by different ways. The first includes the stimulation of metabolism by SCFAs, and therefore, there is an increased energy supply to the cells which is not related with the transcellular SCFA transport [3]. The second mechanism is related with the interaction with transport proteins of the cell membrane, which can couple with ion and SCFA transport. Concerning these facts, there are some cellular uptake mechanisms of SCFAs described as the passive diffusion and the facilitated diffusion. In this transport, the passive diffusion is associated with the fact that this type of transport may be influenced by the acid microenvironment, which can be caused by the permeability of the neutral undissociated carboxylic acid of the plasma membrane in higher concentration comparing with the dissociated charged SCFAs, which changes lipid solubility. The facilitated diffusion, a process of spontaneous passive transport, includes the presence of a specialized uptake mechanism in the apical membrane. There are evidences of SCFA-sensitive transporters in colonic tissue such as monocarboxylate transporter 1 (MCT-1), with close correlation with glucose transporter 1 (GLUT1) responsible for glucose uptake which is described as an influence in the colonocytes during the carcinogenic process [3, 13].
2 Butyrate and colon cancer prevention
In 1999, it was published the first report of the World Cancer Research Fund (WCRF) and the American Institute for Cancer Research (AICR) showing evidence of a strong correlation between diet and cancer incidence [14]. It is already known that cancer is caused by internal or environmental/acquired stimuli. Surprisingly, the genetic factors only represent 5 % of all cancers, while lifestyle-related factors (such as diet, tobacco, alcohol consumption, physical activity, etc.) represent 95 % [15, 16].
Scharlau et al. distinguished three phases of the chemoprevention process: (1) primary, wherein the carcinogenesis initiation phase is inhibited, reducing toxification and inducing detoxification; (2) secondary, which is focused in the inhibition of tumor promotion, second step of the carcinogenesis process, by the inhibition of cell growth and increase of apoptosis and differentiation; and (3) therapy, wherein the progression of preneoplastic in neoplastic cells is prevented [17].
Regarding the dietary habits, it is not fully understood how they influence carcinogenesis; however, several epidemiological and experimental studies have demonstrated that diet, namely dietary fiber, plays an important role on cancer prevention. Diet represents 30–35 % of risk factors involved in cancer development [16, 18, 19]. In colorectal cancer, this relation becomes even more important insofar as the diet is linked to 70 % of deaths due to this type of cancer [16]. Currently, the positive or negative impact of the diet as a risk factor for tumor development is no longer restricted to isolated nutrients, but it is broaden to dietary patterns [15]. These dietary patterns are classified according to its characteristics: (1) healthy pattern, which corresponds to a diet rich in fruits, vegetables, poultry, fish, and cereal and reduced dietary intake of fats and it is suggested to have a protective anti-cancer effect; (2) unhealthy pattern, based on a diet rich in red and processed meat, sugar, potatoes, and sweet and a high intake of fats, favoring the occurrence of certain cancers; and (3) drinker pattern, characterized by a high consumption of wines, beers, and liquors [15, 19].
A diet portion that has been related to a lower risk of cancer occurrence, mainly colorectal cancer, is dietary fiber [18]. Epidemiological studies allowed the observation of a reduced incidence of colorectal cancer in African people, whose diet is rich in dietary fiber. These studies suggested that a high consumption of dietary fiber could play a preponderant role in colorectal cancer prevention [18, 20]. There is still a long way to course with respect to the mechanisms by which dietary fiber contributes to the maintenance of a healthy colon and, thus, for the prevention of colorectal cancer. However, it is now recognized that the beneficial effects of a diet rich in dietary fiber are derived from the products of their fermentation by colonic microflora [17]. The presence of dietary fibers in the meal allows the reduction of gastrointestinal transit time, the dilution of colon contents [21], the modulation of nutrients absorption and metabolism [18], the binding and dilution of carcinogens, the modulation of gastrointestinal epithelium proliferation in order to maintain their cellular integrity [20], and the improvement of bacterial anaerobic fermentation, which leads to increased production of SCFA, such as acetate, proprionate, and butyrate [21]. There is broad consensus that this SCFA production is responsible for most of the physiological properties of the gut microbiota, determining the composition and metabolic activity of the same [18].
Although it is a subject whose mechanisms are not yet entirely understood, there is a proposed model which correlates the consumption of dietary fiber and its role in prevention of colorectal cancer. In fact, if, on the one hand, insoluble fibers bulk the luminal content and accelerate transit colon, minimizing colonic epithelium exposure to ingested carcinogens, such as nitrosamines [22], on the other, the fermentation of soluble fibers in SCFA, particularly the butyrate, plays a multifunctional role in intestinal cells at cellular homeostasis level [23]. Despite not only the acetate but also the propionate and the butyrate are metabolized in the colon epithelium to produce energy, acetate and propionate are first transported into the muscle and liver where they perform their function [22]. Thus, the fact that butyrate is selectively absorbed in the colonic epithelium, being further reduced to produce ATP and providing about 70 % of energy to the colonocytes, allied to the fact that it has other functions in the cellular homeostasis of the colon (for example, anti-inflammatory, anti-oxidant, and anti-carcinogenic actions), makes it a good candidate for primary colon cancer chemoprevention [18, 23, 24]. On the other hand, the butyrate anti-cancer effect on tumor cells, inhibiting cell proliferation and inducing apoptosis and cell cycle arrest, conducts to another action of butyrate in a secondary phase of chemoprevention [17].
The role of butyrate in preventing colorectal cancer has generated some controversy over the years, due to that not always the in vitro results are in accordance with the in vivo results. These differences are primarily related to the details of experimental design, such as the butyrate concentrations used, the timing of butyrate administration, the influence of the tumor or colon microenvironment, the butyrate source, among others [5, 25].
Regarding the butyrate ability to act as a chemopreventive agent in a primary phase, and its importance in the colon homeostasis, in activation of drug-metabolizing enzymes, and in the inflammatory process, will be subject of this review.
The physiological functions of butyrate in the maintenance of healthy colonic mucosa are widely known, and they are based on the balance between proliferation, differentiation, and apoptosis of colonocytes [26]. This fact can indeed have a strong correlation with its chemopreventive action. A recently proposed mechanism for butyrate implication on colon cancer progression relies on the downregulation of butyrate transporters in colon cancer tissue, which will compromise the luminal delivery of butyrate in these tissues and reduce its metabolism [5]. Several studies have also shown that this atrophic butyrate metabolism, which includes butyrate oxidation disorders, imbalance between butyrate and glucose oxidation and reactive oxygen species (ROS) production, is related with the pathogenesis of various colon diseases [23]. Scholz described that butyrate administration or production through dietary fiber ingestion reduced the inflammation and clinical symptoms of patients with active ulcerative colitis, one of the major forms of inflammatory bowel disease that is strictly implicated in the development of colorectal cancer [27, 28]. It was also recently described a mechanism of colorectal cancer initiation that is closely related with the loss of function of the intestinal epithelial barrier, which induces the activation of tumor-associated macrophages, responsible for inflammatory cytokine production and, consequently, tumor growth and progression [29]. Peng et al. studied the effect of butyrate on the maintenance of the intestinal barrier and concluded that butyrate facilitates the assembly of tight junctions by the activation of AMP-activated protein kinase (AMPK) [30]. Another colorectal cancer risk factor related with the intestinal barrier is the changed pattern of mucins’ expression, namely the MUC2, being its expression lost in most of colorectal cancers [31]. Hatayama et al. also reported that butyrate decreases cell proliferation and induces an increase of MUC2 production in LS174T cells, a human colon cancer cell line [32]. Long-time decreasing gastrointestinal motility and consequent slow colonic transit have been implicated as risk factors for colorectal cancer development [17, 33]. Besides regulating mucosa colonic homeostasis, butyrate also interferes with enteric nervous system, modulating neuronal excitability and playing an important role in colonic motility-related diseases [34]. In 2010, in vitro and in vivo studies performed by Soret et al. showed that butyrate induces a cholinergic phenotype alteration that resulted in an increase of colonic motility and ex vivo contractile response [35]. In 2014, Hurst et al. used a spatiotemporal mapping technique that allowed them to trace the motility pattern after acetate, propionate, or butyrate injection into the large intestinal lumen. With this study, the authors concluded that butyrate increases the propulsive contraction at the proximal colon, with ascending contraction increment and descending relaxation, enhancing colon contents movement. Interestingly, an opposite effect was seen with propionate and acetate, revealing that the three main SCFAs play different functions regarding colon motility [36].
As above mentioned, butyrate can also have a chemoprotective effect by activating biotransformation enzymes. Several studies have been conducted in order to ascertain how butyrate modulates these enzymes [17, 37]. Glutathione-s-transferases (GST) are a group of enzymes that are known for its capability in detoxifying endogenous and exogenous carcinogens, reducing colonocyte exposure to risk factors, and consequently blocking cancer initiation [37]. These enzymes catalyze the conjugation of the electrophilic intermediates of carcinogens with glutathione (GSH) [38], protecting cells from those carcinogenic compounds [39]. Scharlau et al. exhaustively studied this possible chemopreventive mechanism by different experimental approaches. Although it can be mediated by different mechanisms, butyrate was able to transcriptionally upregulate GST activity, modulating GST-gene expression and enhancing GST protein expression and activity. These experiments were performed in three different cell models of different stages of cancer development. Curiously, butyrate-induced effects differ according to the carcinogenesis stage, since GST induction levels were more pronounced in tumor cells than in adenoma and primary colon cells [17]. The authors also concluded that butyrate modulates the GSH/GST system, enhancing cellular resistance to genotoxic carcinogens, like hydrogen peroxide. However, it is still difficult to assess to what extent this chemoresistance mechanism will not have adverse effects by increasing survival of cancer cells in a more advanced carcinogenic stage. Thus, further studies should be performed in order to clarify the exact role of butyrate in this mechanism of cancer prevention [17, 37].
The relationship between inflammation and cancer promotion and progression has already been postulated [40], with evidences of the involvement of several pro-inflammatory cytokines [like tumor necrosis factor (TNF), interleukins (IL), chemokines], inflammation-inducing enzymes [like cyclooxygenase-2 (COX-2) and matrix metalloproteinase-9 (MMP-9)], adhesion molecules, and transcription factor activation [such as nuclear factor κB (NF-κB) and hypoxia-inducing factor 1α (HIF-1α)] that results in inflammatory gene products [16, 23]. These gene products, essentially controlled by NF-κB, are strictly linked with the carcinogenic process, since they are related with tumor cell survival, anti-apoptotic signaling pathways, proliferation, invasion, and angiogenesis [16]. On the other hand, NF-κB activation was reported in about 40 % of the colorectal cancers [24]. There are various mechanisms by which butyrate plays an anti-inflammatory role; however, one of the most studied is the inhibition of the transcription factor NF-κB [23].
Chronic intestinal inflammation that characterizes patients with inflammatory bowel disease (IBD), namely Crohn’s disease and ulcerative colitis, may be related with colorectal cancer pathogenesis [40]. Butyrate-producing bacteria as well as butyrate concentration in fecal samples were found decreased in patients with ulcerative colitis in comparison with healthy individuals. However, despite that the differences in butyrate concentrations did not have statistical relevance, the authors believed that an impaired butyrate metabolism is intimately associated with ulcerative colitis pathogenesis, with correlation not only with butyrate uptake but also with a reduction in butyrate oxidation [41]. Another recent study revealed that butyrate modulates intestinal macrophage function through the inhibition of histone deacetylases (HDACs). Intestinal macrophages are extremely important in the maintenance of a responsive intestinal immune system and also in the regulation of the intestinal inflammatory response by the secretion of pro- and anti-inflammatory cytokines. The treatment with butyrate induced a decrease in pro-inflammatory mediators (such as nitric oxide, IL-6 and IL-12), as well as in the respective gene expression, however, without altering TNF-α and monocyte chemoattractant protein 1 (MCP-1) levels. The mechanism underlying this butyrate effect was not related to mitogen-activated protein kinases (MAPK) or NF-κB activation. In fact, the authors described that intestinal macrophages reduce the secretion of pro-inflammatory mediators by a butyrate-mediated mechanism that involves HDAC inhibition [42].
A therapeutic approach for Crohn’s disease is the delivery of butyrate in the colonic mucosa, in order to modulate inflammation through the NF-κB inhibition. Russo et al. studied the influence of butyrate on the oxidative stress and mucosal inflammation on 14 patients with Crohn’s disease. They found out that the oxidative stress is responsible for the activation of NF-κB, destruction of the intestinal barrier of epithelial cells, and consequent mucosal inflammation exacerbation. In this study, the authors showed that butyrate was able to restore intestinal epithelial homeostasis by the control of intracellular ROS balance. The modulation of the redox machinery by butyrate involves the reduction of P65 phosphorylation, NF-κB inhibition, and consequent decreased release/expression of pro-inflammatory cytokines (TNF-α and COX-2) [43]. The therapeutic potential of butyrate in an animal model of ulcerative colitis was also evaluated by Vieira et al. The authors concluded that butyrate improves the anti-inflammatory response, since it reduced leukocyte infiltration and improved the inflammatory profile. They also have correlated this improvement of mucosal damage with the increased metabolism or with the absorption of the oral butyrate in the small intestine [44].
The anti-inflammatory effects of butyrate have been reported in several cells and tissues from organs apart from the colon, revealing its anti-inflammatory potential in colon adjacent tissues. In 2012, Liu et al. also demonstrated that butyrate, as well as, acetate and proprionate, decreased pro-inflammatory factor production and increased anti-inflammatory cytokine release in a murine macrophage cell line. They showed that butyrate suppresses the production of TNF-α, pro-inflammatory interleukins (IL-1β and IL-6), and nitric oxide by inhibiting NF-κB pathway, while it also enhances anti-inflammatory IL-10 levels [45]. Ohira et al. used a co-culture cell model to evaluate the effects of butyrate on the inflammatory responses promoted by the interaction of macrophages and adipocytes. Butyrate attenuated pro-inflammatory responses by the decrease of TNF-α, MCP-1, and IL-6 production through the inhibition of NF-κB activity and MAPK phosphorylation [46].
3 Butyrate and colon cancer therapeutics
The biology of the tumors cannot be simply understood as the characteristics of cancer cells as a unit that, itself, generates the effects of tumorigenesis, but rather should include the contributions of each of these individualities in the origin of the tumor microenvironment to tumorigenesis [47].
A fundamental characteristic of cancer cell is its abnormal capacity to proliferate and grow abnormally. One of the principles that distinguish cancerous cells from normal ones is that normal cells are able to carefully control the production and release of growth-promoting signals that regulate the entry or progression through the cell cycle, while cancer cells, by the deregulation of these signals, become able to proliferate wildly. Cancer cells are, by nature, more metabolically active than normal cells, preferring a quick energy source, and primarily undergo aerobic glycolysis instead of oxidative metabolism. The reason why cancer cells act that manner can be clarified by the Warburg effect [48].
Several studies have demonstrated that butyrate is able to inhibit the growth of tumor cells. Among several theories, one seems to have greater impact, relying on its ability to function as an inhibitor of HDAC, which alters the expression of several genes involved in different processes, such as cell proliferation, apoptosis, and cell differentiation [49]. However, butyrate does not inhibit cell growth when it is transported to the normal colonic epithelium or when non-cancerous colonocytes are incubated in vitro with it [25]. These divergent effects of butyrate on growth of normal cells and colon cancer cells have been described as “the butyrate paradox,” which can be explained by the Warburg effect. In other words, butyrate is an energy source for normal colonocytes, and since it is a fatty acid, it is metabolized to acetyl-CoA by β-oxidation followed by tricarboxylic acid cycle. On the other hand, it is also known that butyrate has the ability to inhibit the growth of colon cancer cells because it is not properly metabolized due to the Warburg effect as represented in Fig. 3. As a result, it accumulates in the nucleus acting as a HDAC inhibitor (HDACi) and, consequently, regulates expression of downstream target genes. It is also known that the role of butyrate in histone acetylation is complex, and to function as an inhibitory compound of HDACs, it is necessary the metabolization of butyrate to acetyl-CoA to stimulate the activity of histone acetyltransferases (HAT). Moreover, it is also known that the metabolic state of tumor cells can control the acetyl-CoA levels, and consequently, it modulates the intranuclear butyrate levels and regulates the inhibitory effect of HDACs or the stimulation of HATs, modulating the expression of several target genes [48].
Butyrate metabolism on colon normal cell and colon cancer cell. The basic difference of butyrate metabolism in the normal and cancer colon cells is that, in normal cells, the primary energy source is butyrate, and it metabolizes glucose to obtain pyruvate, followed by oxidation of pyruvate to CO2 through the TCA cycle, producing 36 ATPs for each molecule of glucose, being the O2 necessary as the final acceptor of electrons. In colon cancer cells, the principal energy source is glucose, which is converted to lactate due to the availability of O2 (the Warburg effect), using the glucose metabolites from energy production to accelerate the cell growth and proliferation, producing two ATPs for each molecule of glucose
In colon cancer, the loss of function or mutation of adenomatous polyposis coli (APC) gene, with consequent activation of β-catenin and K-RAS, leads to activation of Wnt/β-catenin/transcription factor 4 (Wnt/β-catenin/TCF4) signaling pathway. Once activated this pathway, the transcription of downstream genes that are involved in tumorigenesis is commonly activated [such as cyclin D1, MYC, vascular endothelial growth factor (VEGF), and MMPs]. In addition, oncogenic mutation of K-RAS results in activation of RAS and their precursors of the signaling cascade. It was seen that the inhibition of inducible nitric oxide synthase (iNOS), COX-2, VEGF, β-catenin, or MMPs can show a protective effect against colon tumor development in different animal models, suggesting that they are crucial targets for mucosa inflammation and colon tumorigenesis [50]. In many ways, directly or indirectly, butyrate can modulate these proteins in a manner that favors the inhibition of tumor growth and aggressiveness.
4 Butyrate in epigenetic and gene expression
The HDACs are important for gene expression, and the levels of these enzymes are increased in tumor cells and differ according to cancer type [51, 52]. For example, HDAC1 is highly expressed in prostate, gastric, lung, esophagus, and breast cancers. High levels of HDAC2 were found in colon, cervical, and gastric cancers. Furthermore, HDAC3 is expressed in breast and colon tumors, while HDAC6 is highly expressed in neuroblastoma cells [53, 54].
The inhibition of HDACs leads to the chromatin relaxation which makes it less condensed and, therefore, more accessible to DNA synthesis or its expression. Some studies have shown that the decrease in HDAC activity is associated with the suppression of tumor cell growth [55, 56]. In a variety of tumors, the change to a greater state of acetylation, as a result of HDAC inhibition, can result in modification of the expression of several genes. These genes can be involved in processes, such as ERK or Wnt signaling pathways, and they can influence the proteasome system, the activity of some kinases (kinase C), and DNA demethylation [57].
Structurally, several HDACi induce cell death by different processes, depending on the different cell targets. These processes include changes in gene expression, histone modifications, and epigenetic postranslational alterations [58]. The ability of butyrate to epigenetically silence genes in cancer cells, by inducing cell cycle arrest and apoptosis, and simultaneously activate these genes in normal cells has important implications in cancer prevention and therapy [59].
Several studies allowed to find that butyrate, as an inhibitor of HDACs, induces cell cycle arrest and apoptosis, decreases HIF-1α expression and angiogenesis, and also attenuates tumor aggressiveness [60]. The modulation of histone acetylation and deacetylation through dietary compounds, like butyrate, can modulate the epigenetic mechanisms to a more specific and effective colon cancer prevention and treatment. Butyrate and phenylbutyrate are HDACi used for non-oncologic purposes for years, with activity at millimolar concentrations [59]. For example, it is known that butyrate influences cell cycle, being capable to promote the expression of CDKN1A, responsible for the encoding of P21 protein [61]. In a variety of tumor cells, inhibition of HDACs causes overexpression of P21 protein, which blocks the formation of “cyclins and cyclin-dependent kinases” dimers. This event leads to cell cycle arrest and cell differentiation inhibition [56]. P21 biosynthesis is modulated by P53 tumor suppressor protein; i.e., in stress conditions, P53 interacts with the Sp1 site of the P21 promoter, competing with HDAC1, which decreases the transcription of P21 gene. When cells are treated with HDACi, HDAC1 protein is released from the Sp1 site, and this process leads to increased expression of P21. In addition, HDAC inhibition results in the increase of acetylated P53 expression with consequent increment of its half-life (hyperacetylation stabilizes P53), which facilitates the interaction with P21 promoter. Moreover, it has been demonstrated that butyrate is able to downregulate Sp1 binding and upregulate Sp3 binding. As the Sp1 and Sp3 transcription factors are responsible for promoting P21, butyrate leads then to an increase of P21 expression and consequently to cell cycle arrest [62].
Apoptosis induced by inhibitors of HDACs, including butyrate, has been shown to be associated with both intrinsic and extrinsic pathways. Studies have found that butyrate could regulate the levels of some protein expression, such as BID and BAX, which act as activators of the intrinsic apoptotic pathway [49, 63]. Another studies have shown that butyrate induces apoptosis not only by cell cycle arrest, but also by increasing BAK expression [64]. Other studies described the ability of butyrate to influence tumor necrosis apoptosis-inducing factor ligand (TRAIL) pathway, insofar as it sensitizes cancer cell lines known to be resistant by TRAIL [65, 66].
On the other hand, butyrate is capable to suppress some genes responsible for tumor growth. It is known that butyrate can suppress the malignant transforming activity of a human N-RAS oncogene [67]. This effect is associated with a more differentiated phenotype, with a decreased tumor growth rate and tumorigenicity. However, the butyrate treatment does not have a measurable effect on the human N-RAS gene in these cells. This evidence can suggest that butyrate does not affect directly the impact of N-RAS gene, and maybe, it can activate a second gene that antagonizes the action of the transforming N-RAS gene [67].
It is known that butyrate is responsible for the downregulation of MYC messenger RNA (mRNA) expression in HT-29 colon cancer cells [59, 68]. Studies performed in SW837 rectal cancer cells showed that butyrate increases the block to transcriptional elongation in the MYC gene. Therefore, butyrate might regulate MYC expression by regulating transcriptional elongation in these cell types [69]. The MYC gene is commonly mutated in colon cancer, and this proto-oncogene is responsible for the encoding of a transcription factor and is involved in DNA replication [70].
5 Butyrate in tumor growth, microenvironment, and invasion
In colon cancer, like in many other cancers, certain proteins are responsible for the tumor growth, the capacity to survive under hypoxia conditions, the angiogenesis, and development of metastasis. Several studies show that butyrate modulates some of these agents, such as HIF-1α, a protein belonging to the family of HIF transcription factors. This family is responsible for the response to the variation of oxygen concentration, more specifically, the reduction or deprivation of oxygen. HIF-1α plays an important role on VEGF synthesis, and consequently, it is implicated in the increase of angiogenesis in hypoxic conditions. Its interaction with different HDAC isoforms increases its transcriptional activity by promoting tumor progression. So, butyrate indirectly interacts with HIF-1α. In other words, as HDAC inhibitor, butyrate decreases the HIF-1α interaction with HDAC, leading to a smaller presence of HIF-1α in the cell nucleus and preventing the synthesis of VEGF [64, 71–73].
In several colon cancers, APC gene is mutated leading to the β-catenin stabilization, which, in turn, leads to tumor growth. In a normal cell, the APC protein forms a complex with axin, glycogen synthase kinase 3 beta (GSK-3β), and β-catenin. This promotes proteasomal degradation of β-catenin and prevents transcription of β-catenin/TCF4 target genes. When APC protein is mutated, the multi-protein complex cannot be formed and β-catenin is not degraded. In this circumstance, β-catenin is rapidly translocated to the nucleus where it binds to TCF4 and activates transcription of various target genes [74]. Several studies also show that butyrate has an effect on Wnt signaling pathway, since tumor cell lines treated with butyrate have shown an increase of cell death by apoptosis, whenever their proliferation depends on the hyperactivity of the canonical Wnt signaling pathway. These conclusions may lead to new approaches for the treatment of tumors that depend on the Wnt signaling pathway activity. Studies reported that structurally different HDAC inhibitors are also capable of modulating the Wnt signaling pathway in colorectal cancer cells [53, 54, 75, 76]. A study showed that one of the possible mechanisms involved in this effect could be the presence of HDAC3. The HDAC3 is overexpressed by tumor cells and plays an important role in the development of colon cancer. Godman et al. found that a greater presence of HDAC3 potentiated the Wnt pathway and stabilized β-catenin in the nucleus. In the absence of HDAC3, the amount of β-catenin in the nucleus was significantly reduced. By treating cells with butyrate, it was found that β-catenin levels were lower in the nucleus and greater in the cytoplasm. Once absent in the nucleus, there is lesser binding of β-catenin with TCF4 and, consequently, minor transcription of various target genes, such as VEGF [53].
In advanced stages of cancer, tumor growth is dependent on certain factors that allow their survival and invasion, such as angiogenesis or metastasis. Tumor growth and metastasis are highly dependent on neoangiogenesis, the initial phase of development of new blood vessels. This process can emerge from preexisting blood vessels, circulating endothelial cells or endothelial precursor cells from the bone marrow [77]. In colorectal cancer, preclinical evidence as well as clinical studies has demonstrated the involvement of the angiogenesis process for tumor growth and metastasis formation. Furthermore, these studies demonstrated that VEGF-A is the main player of angiogenesis besides being one of the key regulators of angiogenesis pathology and physiology. VEGF-A expression is upregulated in many solid tumors including primary and metastatic colorectal carcinoma, being regulated at the transcriptional level, in a complex net of several oncogene mechanisms, tumor suppressors, and hypoxic conditions [71].
Different studies have found that butyrate is able to inhibit the process of angiogenesis in tumor cell lines, through the downregulation of the VEGF-A expression [64, 78].
As mentioned above, the APC gene is a critical mediator of transcriptional response of the Wnt pathway, negatively regulating β-catenin levels. Some studies suggest that the Wnt/β-catenin signaling pathway regulates the development of blood vessels in normal and pathological conditions. One of these studies performed in HeLa cells and in colorectal cell lines reported that VEGF-A gene is a target gene of β-catenin. It was also shown that in human colorectal cancer cells, β-catenin induces the formation of VEGF-A mRNA and its protein synthesis [75]. Moreover, it is known that butyrate regulates the expression of neuropilin 1 and 2 (NRP-1 and NRP-2), non-tyrosine kinase receptors that bind to specific members of the VEGF family. The NRP-1 binds to VEGF165, VEGF-B, VEGF-E, and the placental growth factor 2, and it is expressed in normal colonic epithelium and usually overexpressed in colorectal cancers. This receptor is correlated with tumor invasiveness, metastatic potential, and decreased patient survival [64]. Clinical studies indicate that a tumor with NRP-1 expression has a higher incidence of metastasis, a high proliferation index, and a reduced number of tumor cells in apoptosis compared with a tumor with NRP-1 subexpression, suggesting that the NRP-1 protects tumor from apoptosis. Interestingly, NRP-1 subexpression induced by siRNA showed an increase of the sensitivity of tumor cells to chemotherapy by inducing apoptosis. A study carried out using different colon cancer cell lines as HT29 cells, Caco2, and HCT116 demonstrated that treatment with 5 mM of butyrate induced a subregulation of NRP-1 expression, leading to the reduction of VEGF binding and, thus, to the inhibition of angiogenesis [64].
Many of colorectal cancer aggressive tumors are chemoresistant. Concerning this, certain types of cancer cells have characteristics, such as expression of certain proteins, which confers them the capacity to resist to the chemotherapy by extruding the chemotherapeutic agents. Some studies have demonstrated that butyrate is able to decrease the extruder activity of some proteins responsible for the resistance to chemotherapy, as P-glycoprotein (Pgp), competing with the drug [79–81]. This effect allows the efficient work of the drug inside the cell, turning the tumor cell more sensitive to the chemotherapeutic agent.
Certain components of the plasminogen-plasmin system (PPS) are important intervenients in a range of physiologic and pathologic processes, including tumor growth, invasion, and metastasis, through their effect on angiogenesis and cell migration [82]. It is described that the presence of these components is increased in a wide variety of tumors, and it is also described that its expression not only demonstrates its function, but also reflects a specific prognosis. This means that the increases of PPS component levels in tumor and serum are correlated with a higher degree of invasiveness of tumor cells and, therefore, with a worst prognosis in patients with colon cancer. Certain studies show that butyrate is able to modulate the balance of PPS components in a manner that favors the decrease of plasminogen activity, leading to a lesser-invasive tumor profile [83, 84].
Some conditions are required for tumor survival, like surrounding blood vessels, immune cells, fibroblasts, other cells as cancer stem cells, signaling molecules, extracellular matrix, a specific microenvironment, and a cellular environment that favors the tumor existence. Regarding tumor microenvironment, it is known that, in some malignant tumors, such as leukemia, breast cancer, brain, and gastric tumors, there are evidences that suggest the presence of cancer stem-like cells that express surface markers similar to those expressed by normal stem cells in each tissue [85]. Kato et al. were able to isolate a population of cells with characteristics of self-renewal capacity with low levels of differentiation markers and long-term proliferative capacity and tumorigenicity. This population of cells, designated by RK12V-SP, demonstrated common characteristics to cancer stem cells, like showing resistance to the conventional chemotherapy. In contrast, treatment with sodium butyrate decreased the capacity for self-renewal and completely suppressed the cell colony formation, demonstrating an inhibitory effect on the proliferation of cancer stem cells [86].
Furthermore, butyrate may have an inhibitory effect on tumor cell migration by inhibiting pro-metastatic metalloproteinase activation [87]. The capacity of the human colon cancer to grow and invade surrounding tissues depends on the capacity of tumor cells to proliferate, migrate, and invade the basement membrane. MMP-2 (gelatinase A) and MMP-9 (gelatinase B) are key members of the MMP family of zinc-dependent endopeptidases that have been associated with many pathologic phenotypes, in particular, cancer metastasis [88]. It was documented that the expression of MMP-2 and MMP-9 is high in invasive cells but low in non-invasive cells [89]. Zeng and Briske-Anderson revealed that butyrate can increase the expression of tissue inhibitors of metalloproteinases (TIMP)-1 and TIMP-2 anti-metastatic genes. The effect of these inhibitors increases the inhibition of pro-MMP-2 and pro-MMP-9 activation (proteins responsible for the activation of MMP-2 and MMP-9) and, consequently, leads to a less tumor cell migration and invasion capacity [90].
Butyrate has several effects on many components of the tumor as represented in the Fig. 4. Its influence on gene expression, differentiation, signaling molecules, angiogenesis, and extracellular matrix of the tumor is remarkable, making it a compound that may be taken into account for clinical purposes.
6 Butyrate and its derivate on clinics
Butyrate is a smart compound for anti-cancer therapy because it selectively inhibits tumor growth and it has minimal adverse effects in clinical trials. Nevertheless, the efficiency of butyrate as a chemotherapeutic agent has been limited by its rapid uptake and metabolism by normal cells before reaching tumors [91]. Some alternatives have been considered, one of which consists in the administration of tributyrin, a triglyceride containing, in its structure, three molecules of butyrate esterified to a glycerol. Tributyrin is a more stable molecule that can be hydrolyzed either by acid and neutral aqueous solutions or even by esterases in plasma. In a study with tributyrin administration, it was possible to obtain butyrate concentrations in the blood above 0.45 mM for 4 h, and three daily dose administrations were found to be well tolerated [92]. Another study with animal models of prostate cancer showed a substantial effect induced by administration of butyrate in the form of oral tributyrin [60]. A significant inhibition of tumor growth and a pro-apoptotic activity was observed. These effects seemed to be independent of P53 status, but perhaps dependent on a signaling pathway that involves P21, retinoblastoma protein (Rb), and MYC [60]. Tributyrin was administered orally, with minimal toxicity, allowing several patients to continue therapy for months. It has been shown in several studies that tributyrin oral administration was safe, contrasting with intravenous therapy that is more expensive and less attractive. Despite the efforts, tributyrin still has some disadvantages, considering the short half-life of butyrate in the blood, which consequently causes irregular levels of butyrate for the desired exposure and limits its use in the clinic [93].
So, other alternatives have arisen, including the use of butyrate analogs. One of these studies involved the analysis of the therapeutic potential of 3n-butyrate molecule, a derivative with a long half-life in blood and more effective than butyrate. Preliminary studies of the pharmacokinetics and toxicology of the compound indicated that it was devoid of toxicological effects and persisted for several hours in the blood of mice, being 30 to 40 times more stable than butyrate itself. In this study, they analyzed the combination of this compound with the first-line chemotherapeutic agent for colorectal cancer, 5-fluorouracil (5-FU). The authors were faced with a promising result, where the combination of the two drugs inhibited 16 human colorectal tumors in vivo, while the isolated treatment with 5-FU only inhibited the growth of 3 and the 3n-butyrate molecule alone had no inhibitory effect. Thus, it was demonstrated that there was synergy with the combination of these two molecules [94].
The results obtained in vivo and in patients in several studies may provide a rational strategy. New well-controlled clinical trials are based on the application of these HDACi as genetic regulators for chemoprevention in patients with a high risk of relapse after a specific therapy or its application in combination with other treatment regimens for certain cancers at advanced stage [56]. The oral use of butyrate or its analogs can be a good strategy for alternative treatment or sensitization of tumor cells with a combination of drugs conventionally used in chemotherapeutic regimens.
Another approach is to increase the levels of butyrate (at mM levels) by the natural microbiota, in which, a high-fiber diet can be more effective for chemoprevention. In this case, the main objective is to deliver the desired levels of butyrate into the correct location (colon) before the initiation or in an early stage of cancer development or allowing the modulation by butyrate of some characteristics of tumor growth and invasion at a more advanced stage.
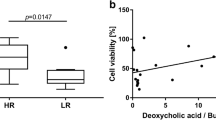
It has been shown, in patients with colorectal cancer, the presence of lower levels of microorganisms responsible for butyrate production compared with healthy individuals. Recent studies have also demonstrated an inverse correlation between the tumor size of colorectal cancer and the fecal levels of butyrate [95].
One recent study has demonstrated, for the first time, that the modulation of the diet, with the final objective of butyrate production optimization, reduces the toxicity induced by irinotecan, a second-line therapeutic agent for colorectal cancer. This result can be exploited to reduce morbidity and improve the irinotecan tolerance administration [96].
Taken together, these findings suggest that human studies should be conducted in order to investigate the combined interaction between dietary fibers or, more specifically, butyrate and gut microbiota in the prevention and treatment of colorectal cancer.
7 Conclusions
Butyrate is a four-carbon naturally occurring short-chain fatty acid (SCFA), obtained by the intake of dietary fiber. SCFAs are described as having a key role in maintaining gut homeostasis and epithelial integrity, being responsible for most of the physiological properties of the gut microbiota and, consequently, for the composition and metabolic activity of the same.
The bioavailability of butyrate has important implications on the maintenance of colon health, as well as, on colon cancer progression, since it can compromise butyrate luminal delivery in the tissues and its metabolism. So, butyrate can be synthesized through four pathways, being diet the major factor that contributes to different gut shape. Regarding its transport, there are two different proposed approaches: paracellular transport in contrast to transcellular transport.
A diet rich in dietary fiber has been related to a lower risk of colorectal cancer occurrence. However, it is now recognized that the beneficial effects of a diet rich in dietary fiber are derived from the products of their fermentation by colonic microflora, namely, the production of butyrate. The fact that butyrate is selectively absorbed in the colonic epithelium, being further reduced to produce ATP and providing about 70 % of energy to the colonocytes, allied to the fact that it has other functions in the cellular homeostasis of the colon (for example, anti-inflammatory, anti-oxidant, and anti-carcinogenic actions), makes it a good candidate for primary colon cancer chemoprevention. The butyrate ability to act as a chemopreventive agent in a primary phase of colorectal cancer progression is based on its importance in the colon homeostasis, in activation of drug-metabolizing enzymes and in its capability to modulate the inflammatory process.
Butyrate is also able to inhibit the growth of tumor cells. Among several theories, one seems to have great impact, relying on its ability to function as an inhibitor of HDAC. Butyrate is an energy source for normal colonocytes; however, in colon cancer cells, it is not properly metabolized due to the Warburg effect. As a result, it accumulates in the nucleus acting as a HDAC inhibitor. Consequently, it regulates the expression of downstream target genes involved in different processes, such as cell proliferation, apoptosis, and cell differentiation.
The butyrate is able to modulate the expression of different proteins responsible for the regulation of cell growth and division, angiogenesis, tumor invasion, and aggressiveness. Since different types of tumor cells have a preference for growth of a specific metabolic and signaling pathway, the fact that this compound is capable of influencing different mechanisms leads to decreased survival of a possible heterogeneous tumor population.
The potential anti-cancer effect of butyrate associated with minimal adverse effects in clinical trials is indisputable; however, its efficiency has been limited by its rapid uptake and metabolism by normal cells before reaching tumors. So, several strategies have emerged, ranging from the development of butyrate derivatives with longer half-lives to the combination with drugs conventionally used in chemotherapeutic regimens or the adoption of high fiber-based diet.
Taking into account all the recent findings here reviewed, the commitment between butyrate and its influence on colorectal cancer prevention and therapy is unmistakable. Thus, the fulfillment of more clinical studies is needed, which includes the delivery of the desired levels of butyrate into the correct location, by the administration of the butyrate or its analogs or by the modulation of the individual diet.
References
Knudsen, B. K. E., Serena, A., Canibe, N., & Juntunen, K. S. (2003). New insight into butyrate metabolism. Proceedings of the Nutrition Society, 62, 81–86.
Vital, M., Howe, A. C., & Tiedje, J. M. (2014). Revealing the bacterial butyrate synthesis pathways by analyzing (meta)genomic data. mBio, 5(2), 1–11. doi:10.1128/mBio.00889-14.
Mortensen, P. B., & Clausen, M. R. (1996). Short-chain fatty acids in the human colon: relation to gastrointestinal health and disease. Scandinavian Journal of Gastroenterology. Supplement, 216, 132–148.
Daly, K., Cuff, M. A., Fung, F., & Shirazi-Beechey, S. P. (2005). The importance of colonic butyrate transport to the regulation of genes associated with colonic tissue homoeostasis. Biochemical Society Transactions, 33, 733–735. doi:10.1042/BST0330733.
Hamer, H. M., Jonkers, D., Venema, K., Vanhoutvin, S., Troost, F. J., & Brummer, R.-J. (2008). Review article: the role of butyrate on colonic function. Alimentary Pharmacology & Therapeutics, 27(2), 104–119. doi:10.1111/j.1365-2036.2007.03562.x.
Ahmad, M. S., Krishnan, S., Ramakrishna, B. S., Mathan, M., Pulimood, A. B., & Murthy, S. N. (2000). Butyrate and glucose metabolism by colonocytes in experimental colitis in mice. Gut, 46(4), 493–499.
Topping, D. L., & Clifton, P. M. (2001). Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiological Reviews, 81(3), 1031–1064. doi:10.1002/(SICI)1096-8644(199706)103:2<157::AID-AJPA2>3.0.CO;2-R.
Louis, P., & Flint, H. J. (2009). Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiology Letters, 294(1), 1–8. doi:10.1111/j.1574-6968.2009.01514.x.
Pryde, S. E., Duncan, S. H., Hold, G. L., Stewart, C. S., & Flint, H. J. (2002). The microbiology of butyrate formation in the human colon. FEMS Microbiology Letters, 217, 133–139. doi:10.1016/S0378-1097(02)01106-0.
Genz, A., Engelhardt, W., & Busche, R. (1999). Maintenance and regulation of the pH microclimate at the luminal surface of the distal colon of guinea-pig. 507–519.
Sehested, J., Diernaes, L., Moller, P. D., & Skadhauge, E. (1996). Transport of sodium across the isolated bovine rumen epithelium: interaction with short-chain fatty acids, chloride and bicarbonate. Experimental Physiology, 81, 79–94.
Gonçalves, P., & Martel, F. (2013). Butyrate and colorectal cancer: the role of butyrate transport. Current Drug Metabolism, 14(9), 994–1008. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/24160296.
Cuff, M. A., & Shirazi-Beechey, S. P. (2004). The importance of butyrate transport to the regulation of gene expression in the colonic epithelium. Biochemical Society Transactions, 32, 1100–1102. doi:10.1042/BST0321100.
Glade, M. J. (1999). Food, nutrition, and the prevention of cancer: a global perspective. Nutrition, 15(6), 523–526.
Baena Ruiz, R., & Salinas Hernández, P. (2014). Diet and cancer: risk factors and epidemiological evidence. Maturitas, 77(3), 202–208. doi:10.1016/j.maturitas.2013.11.010.
Anand, P., Kunnumakkara, A. B., Kunnumakara, A. B., Sundaram, C., Harikumar, K. B., Tharakan, S. T., … & Aggarwal, B. B. (2008). Cancer is a preventable disease that requires major lifestyle changes. Pharmaceutical Research, 25(9), 2097–116. doi:10.1007/s11095-008-9661-9.
Scharlau, D., Borowicki, A., Habermann, N., Hofmann, T., Klenow, S., Miene, C., … & Glei, M. (2009). Mechanisms of primary cancer prevention by butyrate and other products formed during gut flora-mediated fermentation of dietary fibre. Mutation Research, 682(1), 39–53. doi:10.1016/j.mrrev.2009.04.001.
Zeng, H., Lazarova, D. L., & Bordonaro, M. (2014). Mechanisms linking dietary fiber, gut microbiota and colon cancer prevention. World Journal of Gastrointestinal Oncology, 6(2), 41–51. doi:10.4251/wjgo.v6.i2.41.
Irigaray, P., Newby, J. A., Clapp, R., Hardell, L., Howard, V., Montagnier, L., … & Belpomme, D. (2007). Lifestyle-related factors and environmental agents causing cancer: an overview. Biomedicine & pharmacotherapy = Biomédecine & pharmacothérapie, 61(10), 640–58. doi:10.1016/j.biopha.2007.10.006.
Pericleous, M., Mandair, D., & Caplin, M. E. (2013). Diet and supplements and their impact on colorectal cancer. Journal of Gastrointestinal Oncology, 4(4), 409–423. doi:10.3978/j.issn.2078-6891.2013.003.
Durko, L., & Malecka-Panas, E. (2014). Lifestyle modifications and colorectal cancer. Current Colorectal Cancer Reports, 10, 45–54. doi:10.1007/s11888-013-0203-4.
Bultman, S. J. (2014). Molecular pathways: gene-environment interactions regulating dietary fiber induction of proliferation and apoptosis via butyrate for cancer prevention. Clinical Cancer Research: An Official Journal of the American Association for Cancer Research, 20(4), 799–803. doi:10.1158/1078-0432.CCR-13-2483.
Leonel, A. J., & Alvarez-Leite, J. I. (2012). Butyrate: implications for intestinal function. Current Opinion in Clinical Nutrition and Metabolic Care, 15(5), 474–479. doi:10.1097/MCO.0b013e32835665fa.
Fung, K. Y. C., Cosgrove, L., Lockett, T., Head, R., & Topping, D. L. (2012). A review of the potential mechanisms for the lowering of colorectal oncogenesis by butyrate. The British Journal of Nutrition, 108(5), 820–831. doi:10.1017/S0007114512001948.
Lupton, J. R. (2004). Microbial degradation products influence colon cancer risk: the butyrate controversy. The Journal of Nutrition, 134, 479–482.
Klampfer, L., Huang, J., Sasazuki, T., Shirasawa, S., & Augenlicht, L. (2003). Inhibition of interferon; signaling by the short chain fatty acid butyrate. Molecular Cancer Research, 1(September), 855–862.
Scholz, D. (2011). The role of nutrition in the etiology of inflammatory bowel disease. Current Problems in Pediatric and Adolescent Health Care, 41(9), 248–253. doi:10.1016/j.cppeds.2011.04.005.
Rogler, G. (2014). Chronic ulcerative colitis and colorectal cancer. Cancer Letters, 345(2), 235–241. doi:10.1016/j.canlet.2013.07.032.
Wang, K., & Karin, M. (2013). Common flora and intestine: a carcinogenic marriage. Cellular Logistics, 3(1), e24975. doi:10.4161/cl.24975.
Peng, L., Li, Z.-R., Green, R. S., Holzman, I. R., & Lin, J. (2009). Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. The Journal of Nutrition, 139(9), 1619–1625. doi:10.3945/jn.109.104638.
Renaud, F., Vincent, A., Mariette, C., Crépin, M., Stechly, L., Truant, S., … & Buisine, M.-P. (2014). MUC5AC hypomethylation is a predictor of microsatellite instability independently of clinical factors associated with colorectal cancer. International Journal of Cancer. Journal International du Cancer, 00. doi:10.1002/ijc.29342.
Hatayama, H., Iwashita, J., Kuwajima, A., & Abe, T. (2007). The short chain fatty acid, butyrate, stimulates MUC2 mucin production in the human colon cancer cell line, LS174T. Biochemical and Biophysical Research Communications, 356(3), 599–603. doi:10.1016/j.bbrc.2007.03.025.
Blum, H. E. (1995). Colorectal cancer: future population screening for early colorectal cancer. European Journal of Cancer (Oxford, England : 1990), 31A(7-8), 1369–1372.
Canani, R. B., Costanzo, M. D., Leone, L., Pedata, M., Meli, R., & Calignano, A. (2011). Potential beneficial effects of butyrate in intestinal and extraintestinal diseases. World Journal of Gastroenterology: WJG, 17(12), 1519–1528. doi:10.3748/wjg.v17.i12. 1519.
Soret, R., Chevalier, J., De Coppet, P., Poupeau, G., Derkinderen, P., Segain, J. P., & Neunlist, M. (2010). Short-chain fatty acids regulate the enteric neurons and control gastrointestinal motility in rats. Gastroenterology, 138(5), 1772–1782. doi:10.1053/j.gastro.2010.01.053.
Hurst, N. R., Kendig, D. M., Murthy, K. S., & Grider, J. R. (2014). The short chain fatty acids, butyrate and propionate, have differential effects on the motility of the guinea pig colon. Neurogastroenterology and Motility: The Official Journal of the European Gastrointestinal Motility Society, 26(11), 1586–1596. doi:10.1111/nmo.12425.
Kautenburger, T., Beyer-Sehlmeyer, G., Festag, G., Haag, N., Kühler, S., Küchler, A., & … Pool-Zobel, B. L. (2005). The gut fermentation product butyrate, a chemopreventive agent, suppresses glutathione S-transferase theta (hGSTT1) and cell growth more in human colon adenoma (LT97) than tumor (HT29) cells. Journal of Cancer Research and Clinical Oncology, 131(10), 692–700. doi:10.1007/s00432-005-0013-4.
Scharmach, E., Hessel, S., Niemann, B., & Lampen, A. (2009). Glutathione S-transferase expression and isoenzyme composition during cell differentiation of Caco-2 cells. Toxicology, 265(3), 122–126. doi:10.1016/j.tox.2009.09.017.
Sauer, J., Richter, K. K., & Pool-Zobel, B. L. (2007). Products formed during fermentation of the prebiotic inulin with human gut flora enhance expression of biotransformation genes in human primary colon cells. The British Journal of Nutrition, 97(5), 928–937. doi:10.1017/S0007114507666422.
Hofmanová, J., Straková, N., Vaculová, A. H., Tylichová, Z., Safaříková, B., Skender, B., & Kozubík, A. (2014). Interaction of dietary fatty acids with tumour necrosis factor family cytokines during colon inflammation and cancer. Mediators of Inflammation, 2014, 848632. doi:10.1155/2014/848632.
Machiels, K., Joossens, M., Sabino, J., De Preter, V., Arijs, I., Eeckhaut, V., … & Vermeire, S. (2014). A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut, 63(8), 1275–83. doi:10.1136/gutjnl-2013-304833.
Chang, P. V., Hao, L., Offermanns, S., & Medzhitov, R. (2014). The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proceedings of the National Academy of Sciences of the United States of America, 111(6), 2247–2252. doi:10.1073/pnas.1322269111.
Russo, I., Luciani, A., De Cicco, P., Troncone, E., & Ciacci, C. (2012). Butyrate attenuates lipopolysaccharide-induced inflammation in intestinal cells and Crohn’s mucosa through modulation of antioxidant defense machinery. PloS One, 7(3), e32841. doi:10.1371/journal.pone.0032841.
Vieira, E. L. M., Leonel, A. J., Sad, A. P., Beltrão, N. R. M., Costa, T. F., Ferreira, T. M. R., … & Alvarez-Leite, J. I. (2012). Oral administration of sodium butyrate attenuates inflammation and mucosal lesion in experimental acute ulcerative colitis. The Journal of Nutritional Biochemistry, 23(5), 430–6. doi:10.1016/j.jnutbio.2011.01.007.
Liu, T., Li, J., Liu, Y., Xiao, N., Suo, H., Xie, K., … & Wu, C. (2012). Short-chain fatty acids suppress lipopolysaccharide-induced production of nitric oxide and proinflammatory cytokines through inhibition of NF-κB pathway in RAW264.7 cells. Inflammation, 35(5), 1676–84. doi:10.1007/s10753-012-9484-z.
Ohira, H., Fujioka, Y., Katagiri, C., Mamoto, R., Aoyama-Ishikawa, M., Amako, K., … & Ikeda, M. (2013). Butyrate attenuates inflammation and lipolysis generated by the interaction of adipocytes and macrophages. Journal of Atherosclerosis and Thrombosis, 425–442. doi:10.5551/jat.15065.
Hanahan, D., & Weinberg, R. A. (2011). Hallmarks of cancer: the next generation. Cell, 144(5), 646–674. doi:10.1016/j.cell.2011.02.013.
Donohoe, D. R., Collins, L. B., Wali, A., Bigler, R., Sun, W., & Bultman, S. J. (2012). The Warburg effect dictates the mechanism of butyrate-mediated histone acetylation and cell proliferation. Molecular Cell, 48(4), 612–626. doi:10.1016/j.molcel.2012.08.033.
Pajak, B., Orzechowski, A., & Gajkowska, B. (2007). Molecular basis of sodium butyrate-dependent proapoptotic activity in cancer cells. Advances in Medical Sciences, 52, 83–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18217395.
Pan, M.-H., Lai, C.-S., Wu, J.-C., & Ho, C.-T. (2011). Molecular mechanisms for chemoprevention of colorectal cancer by natural dietary compounds. Molecular Nutrition & Food Research, 55(1), 32–45. doi:10.1002/mnfr.201000412.
Stiborová, M., Eckschlager, T., Poljaková, J., Hraběta, J., Adam, V., Kizek, R., & Frei, E. (2012). The synergistic effects of DNA-targeted chemotherapeutics and histone deacetylase inhibitors as therapeutic strategies for cancer treatment. Current Medicinal Chemistry, 19(25), 4218–38. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/22680633.
Witt, O., Deubzer, H. E., Milde, T., & Oehme, I. (2009). HDAC family: what are the cancer relevant targets? Cancer Letters, 277(1), 8–21. doi:10.1016/j.canlet.2008.08.016.
Godman, C. A, Joshi, R., Tierney, B. R., Greenspan, E., Rasmussen, T. P., Wang, H.-W., … & Giardina, C. (2008). HDAC3 impacts multiple oncogenic pathways in colon cancer cells with effects on Wnt and vitamin D signaling. Cancer Biology and Therapy, 7(10), 1570–80. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2614677&tool=pmcentrez&rendertype=abstract.
Li, Y., Zhang, X., Polakiewicz, R. D., Yao, T.-P., & Comb, M. J. (2008). HDAC6 is required for epidermal growth factor-induced beta-catenin nuclear localization. The Journal of Biological Chemistry, 283(19), 12686–12690. doi:10.1074/jbc.C700185200.
Ma, X., Ezzeldin, H. H., & Diasio, R. B. (2009). Histone deacetylase inhibitors: current status and overview of recent clinical trials. Drugs, 69(14), 1911–1934. doi:10.2165/11315680-000000000-00000.
Minucci, S., & Pelicci, P. G. (2006). Histone deacetylase inhibitors and the promise of epigenetic (and more) treatments for cancer. Nature Review. Cancer, 6(1), 38–51. doi:10.1038/nrc1779.
Bordonaro, M., Lazarova, D. L., & Sartorelli, A. C. (2007). The activation of beta-catenin by Wnt signaling mediates the effects of histone deacetylase inhibitors. Experimental Cell Research, 313(8), 1652–1666. doi:10.1016/j.yexcr.2007.02.008.
Federico, M., & Bagella, L. (2011). Histone deacetylase inhibitors in the treatment of hematological malignancies and solid tumors. Journal of Biomedicine and Biotechnology, 2011(Figure 1), 475641. doi:10.1155/2011/475641.
Dashwood, R. H., & Ho, E. (2007). Dietary histone deacetylase inhibitors: from cells to mice to man. Seminars in Cancer Biology, 17(5), 363–369. doi:10.1016/j.semcancer.2007.04.001.
Kuefer, R., Hofer, M. D., Altug, V., Zorn, C., Genze, F., Kunzi-Rapp, K., … & Gschwend, J. E. (2004). Sodium butyrate and tributyrin induce in vivo growth inhibition and apoptosis in human prostate cancer. British Journal of Cancer, 90(2), 535–41. doi:10.1038/sj.bjc.6601510.
Wang, Z., Ehinger, M., & Grant, S. (1999). Induction of apoptosis in U937 human leukemia cells by suberoylanilide hydroxamic acid ( SAHA ) proceeds through pathways that are regulated by, 7016–7025.
Davie, J. R. (2003). Inhibition of histone deacetylase activity by butyrate. The Journal of nutrition, 2485–2493.
Roy, M.-J., Dionne, S., Marx, G., Qureshi, I., Sarma, D., Levy, E., & Seidman, E. G. (2009). In vitro studies on the inhibition of colon cancer by butyrate and carnitine. Nutrition (Burbank, Los Angeles County, California), 25(11-12), 1193–1201. doi:10.1016/j.nut.2009.04.008.
Yu, D. C. W., Waby, J. S., Chirakkal, H., Staton, C. A., & Corfe, B. M. (2010). Butyrate suppresses expression of neuropilin I in colorectal cell lines through inhibition of Sp1 transactivation. Molecular Cancer, 9(1), 276. doi:10.1186/1476-4598-9-276.
Hernandez, A., Thomas, R., Smith, F., Sandberg, J., Kim, S., Chung, D. H., & Evers, B. M. (2001). Butyrate sensitizes human colon cancer cells to TRAIL-mediated apoptosis. Surgery, 130(2), 265–272. doi:10.1067/msy.2001.115897.
Kim, Y.-H., Park, J.-W., Lee, J.-Y., & Kwon, T. K. (2004). Sodium butyrate sensitizes TRAIL-mediated apoptosis by induction of transcription from the DR5 gene promoter through Sp1 sites in colon cancer cells. Carcinogenesis, 25(10), 1813–1820. doi:10.1093/carcin/bgh188.
Niles, R. M. (1989). Sodium butyrate suppresses the transforming activity activated N-ras oncogene in human colon carcinoma cells. Experimental Cell Research, 184, 16–27.
Velázquez, O. C., Lederer, H. M., & Rombeau, J. L. (1996). Butyrate and the colonocyte. Implications for neoplasia. Digestive Diseases and Sciences, 41(4), 727–39. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8674394.
Heruth, D. P., Zirnstein, G. W., Bradley, J. F., & Rothbergs, G. (1993). Sodium butyrate causes an increase in the block to transcriptional elongation in the c-myc gene in SW837 rectal carcinoma cells. The Journal of Biological Chemistry, 268(25), 20466–20472.
Taylora, C. W., & Kimb, Y. S. (1992). Sensitivity of nuclear c-myc levels and induction to agents in human colon tumor cell lines. Cancer Letters, 62(2), 95–105.
Giles, R. H., Lolkema, M. P., Snijckers, C. M., Belderbos, M., van der Groep, P., Mans, D. a, … & Voest, E. E. (2006). Interplay between VHL/HIF1alpha and Wnt/beta-catenin pathways during colorectal tumorigenesis. Oncogene, 25(21), 3065–70. doi:10.1038/sj.onc.1209330.
Furusawa, Y., Obata, Y., Fukuda, S., Endo, T. A., Nakato, G., Takahashi, D., … & Ohno, H. (2013). Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature, 504(7480), 446–50. doi:10.1038/nature12721.
Qian, D. Z., Kachhap, S. K., Collis, S. J., Verheul, H. M. W., Carducci, M. A., Atadja, P., & Pili, R. (2006). Class II histone deacetylases are associated with VHL-independent regulation of hypoxia-inducible factor 1 alpha. Cancer Research, 66(17), 8814–8821. doi:10.1158/0008-5472.CAN-05-4598.
Sancho, E., Batlle, E., & Clevers, H. (2004). Signaling pathways in intestinal development and cancer. Annual Review of Cell and Developmental Biology, 20, 695–723. doi:10.1146/annurev.cellbio.20.010403.092805.
Billin, A. N., Thirlwell, H., & Ayer, D. E. (2000). Beta-catenin-histone deacetylase interactions regulate the transition of LEF1 from a transcriptional repressor to an activator. Molecular and cellular biology, 20(18), 6882–90. Retrieved from http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=88764&tool=pmcentrez&rendertype=abstract.
Yamaguchi, M., Tonou-Fujimori, N., Komori, A., Maeda, R., Nojima, Y., Li, H., … & Masai, I. (2005). Histone deacetylase 1 regulates retinal neurogenesis in zebrafish by suppressing Wnt and Notch signaling pathways. Development (Cambridge, England), 132(13), 3027–43. doi:10.1242/dev.01881.
Luczyńska, E., & Anioł, J. (2013). Neoangiogenesis in prostate cancer. Contemporary Oncology (Poznan, Poland), 17(3), 229–233. doi:10.5114/wo.2013.35272.
Pellizzaro, C., & Coradini, D. (2002). Modulation of angiogenesis-related proteins synthesis by sodium butyrate in colon cancer cell line HT29 sodium butyrate (NaB), a short-chain fatty acid naturally arrest, differentiation and apoptosis in colon cancer cells. Carcinogenesis, 23(5), 735–740.
Bates, S. E., Currier, S. J., Alvarez, M., & Fojo, A. T. (1992). Modulation of P-glycoprotein phosphorylation and drug transport by sodium butyrate. Biochemistry, 31(28), 6366–72. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1352990.
Gonçalves, P., Gregório, I., & Martel, F. (2011). The short-chain fatty acid butyrate is a substrate of breast cancer resistance protein. American Journal of Physiology. Cell Physiology, 301(5), C984–C994. doi:10.1152/ajpcell.00146.2011.
Casalta-Lopes, J. (2011). Efflux pumps modulation in colorectal adenocarcinoma cell lines: the role of nuclear medicine. Journal of Cancer Therapy, 02(03), 408–417. doi:10.4236/jct.2011.23056.
Kwaan, H. C. B., & McMahon, B. (2009). Coagulation in cancer. (P. David Green, MD & H. C. Kwaan, Eds.) (pp. 43–66). Springer New York. Retrieved from http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:No+Title#0.
Gibson, P. R., Birchall, I., Rosella, O., Albert, V., Finch, C. F., Barkla, D. H., & Young, G. P. (1998). Urokinase and the intestinal mucosa: evidence for a role in epithelial cell turnover. Gut, 43, 656–663.
Mortensen, F. V., Jørgensen, B., Christiansen, H. M., Sloth-Nielsen, J., Wolff, B., & Hessov, I. (2000). Short-chain fatty acid enemas stimulate plasminogen activator inhibitor-1 after abdominal aortic graft surgery: a double-blinded, placebo-controlled study. Thrombosis Research, 98(5), 361–366.
Shukla, S., & Meeran, S. M. (2014). Epigenetics of cancer stem cells: pathways and therapeutics. Biochimica et Biophysica Acta (BBA), 1840(12), 3494–3502.
Kato, K., Kuhara, A., Yoneda, T., Inoue, T., Takao, T., Ohgami, T., … & Wake, N. (2011). Sodium butyrate inhibits the self-renewal capacity of endometrial tumor side-population cells by inducing a DNA damage response. Molecular Cancer Therapeutics, 10(8), 1430–9. doi:10.1158/1535-7163.MCT-10-1062.
Rodríguez-Salvador, J., Armas-Pineda, C., Perezpeña-Diazconti, F., Chico-Ponce de León, G., Sosa-Sáinz, P., Lezama, F., … & Arenas-Huertero, F. (2005). Effect of sodium butyrate on pro-matrix metalloproteinase-9 and -2 differential secretion in pediatric tumors and cell lines. Journal of Experimental & Clinical Cancer Research, 24(3), 463–474.
Oukopoulos, P. L., Ungall, B. A. M., Traw, R. C. S., & Hornton, J. R. T. (2003). Matrix metalloproteinase-2 and -9 involvement in canine tumors. Veterinary Pathology, 394, 382–394.
Oba, K., Konno, H., Tanaka, T., Baba, M., Kamiya, K., Ohta, M., … & Nakamura, S. (2002). Prevention of liver metastasis of human colon cancer by selective matrix metalloproteinase inhibitor MMI-166. Cancer Letters, 175, 45–51.
Zeng, H., & Briske-Anderson, M. (2005). Nutrition and cancer prolonged butyrate treatment inhibits the migration and invasion potential of HT1080 tumor cells. The Journal of Nutrition, 291–295.
Pouillart, P. R. (1998). Role of butyric acid and its derivatives in the treatment of colorectal cancer and hemoglobinopathies. Life Sciences, 63(20), 1739–1760.
Egorin, M. J., Yuan, Z. M., Sentz, D. L., Plaisance, K., & Eiseman, J. L. (1999). Plasma pharmacokinetics of butyrate after intravenous administration of sodium butyrate or oral administration of tributyrin or sodium butyrate to mice and rats. Cancer Chemotherapy and Pharmacology, 43(6), 445–53. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10321503.
Marc, D., & Sausville, A. (1998). I study of the in patients orally with administered solid butyrate. 4(March), 629–634.
Bras–Gonçalves, R. A., Pocard, M., Formento‡, J., Poirson–Bichat, F., de Pinieux, G., Pandrea§, I., … & Poupon, M. (2001). Synergistic efficacy of 3n-butyrate and 5-fluorouracil in human colorectal cancer xenografts via modulation of DNA synthesis. Gastroenterology, 120(4), 874–888. doi:10.1053/gast.2001.22440.
Wang, T., Cai, G., Qiu, Y., Fei, N., Zhang, M., Pang, X., … & Zhao, L. (2012). Structural segregation of gut microbiota between colorectal cancer patients and healthy volunteers. The ISME Journal, 6(2), 320–9. doi:10.1038/ismej.2011.109.
Lin, X. B., Farhangfar, A., Valcheva, R., Sawyer, M. B., Dieleman, L., Schieber, A., … & Baracos, V. (2014). The role of intestinal microbiota in development of irinotecan toxicity and in toxicity reduction through dietary fibres in rats. PloS One, 9(1), e83644. doi:10.1371/journal.pone.0083644.
Acknowledgments
Ana Salomé Pires would like to thank the Portuguese Foundation for Science and Technology for the award of PhD scholarship (SFRH/BD/75300/2010).
Support: FCT, Portugal (Strategic Project PEst-C/SAU/UI3282/2013 and UID/NEU/04539/2013), COMPETE-FEDER.
Conflict of interest
The authors declare that they have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Encarnação, J.C., Abrantes, A.M., Pires, A.S. et al. Revisit dietary fiber on colorectal cancer: butyrate and its role on prevention and treatment. Cancer Metastasis Rev 34, 465–478 (2015). https://doi.org/10.1007/s10555-015-9578-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-015-9578-9