Abstract
Hepatocellular carcinoma (HCC), a prototype of hypervascular tumors, is one of the most common malignancies in the world, especially hyperendemic in the Far East where chronic hepatitis B virus (HBV) infection is highly prevalent. It is characterized by the clinical feature of a poor prognosis or a high mortality due to its already far advanced stages at diagnosis. It is so multifactorial that hepatocarcinogenesis cannot be explained by a single molecular mechanism. To date, a number of pathways have been known to contribute to the development, growth, angiogenesis, and even metastasis of HCC. Among the various factors, metastatic tumor antigens (MTAs) or metastasis-associated proteins have been vigorously investigated as an intriguing target in the field of hepatocarcinogenesis. According to recent studies including ours, MTAs are not only involved in the HCC development and growth (molecular carcinogenesis), but also closely associated with the post-operative recurrence and a poor prognosis or a worse response to post-operative anti-cancer therapy (clinical significance). Herein, we review MTAs in light of their essential structure, functions, and molecular mechanism in hepatocarcinogenesis. We will also focus in detail on the interaction between hepatitis B x protein (HBx) of HBV and MTA in order to clarify the HBV-associated HCC development. Finally, we will discuss the prognostic significance and clinical application of MTA in HCC. We believe that this review will help clinicians to understand the meaning and use of the detection of MTA in order to more effectively manage their HCC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Hepatocellular carcinoma (HCC) is a common malignancy that is the fifth most common cancer in the world [1–3]. The prognosis of HCC is generally very poor even in patients who have undergone surgery, due to the frequent vascular invasion and multiple intrahepatic or extrahepatic metastases at the time of diagnosis [4–6]. Furthermore, frequent recurrence after surgery is a major limitation to long-term survival [7–10].
Recently, the metastatic tumor antigens or metastasis-associated proteins of cancers have been studied and isolated. Among them, metastatic tumor antigen 1 (MTA1) is known to increase the migration and invasion of various tumor cells in vitro [11–13]. MTA1 has also been suggested to have a role in angiogenic processes as a stabilizer of hypoxia-inducible factor 1α (HIF-1α) which is a potent angiogenic regulator in a hypoxic state, such as in a solid tumor mass [14–16]. Thus, it has been reported that MTA1 overexpression is closely correlated with an aggressive course in several human cancers, such as breast, prostate, colorectal, gastric, and esophageal cancers [17–24]. Until just a few years ago, few data were available regarding the role of MTA1 in HCC patients [25, 26]. Recently, we have reported the results of several interesting studies regarding the important role of MTA 1 and 2 in tumor invasion and recurrence or survival after surgery in HCC patients [27–31].
In this review, we summarize recent reports regarding the MTA family in HCC patients, especially regarding the molecular structure and expression, the clinicopathological significance, underlying mechanism in cancer development, metastasis, and angiogenesis, the role as a prognostic predictor related to the recurrence and patient survival after surgery, and as an expectedly specific molecular target therapy.
2 Molecular structure and expression of the MTA family
2.1 Structure, localization, and expression of MTA1
MTA1 was originally identified and analyzed as a metastasis-promoting gene that encodes a protein comprising typical DNA-binding motifs and nuclear localization signals. At an initial report, the molecular weight of MTA1 is approximately 80 kDa [32]. Sequence analysis of the primary structure of MTA1 shows multiple DNA-binding domains and a nuclear localization signal [32–37]. MTA1 has a preserved GATA-type zinc finger motif indicating a direct binding to DNA [37]. However, the leucine zipper motif was not observed [32] (Fig. 1).
Amino acid sequence of human MTA1 (NCBI accession No. U35113.1) was analyzed through the National Center for Biotechnology Information (NCBI)-supplied BLAST program. The diagram shows the summarized result from http://www.ncbi.nlm.nih.gov/Structure/cdd/wrpsb.cgi?SEQUENCE=1008544&FULL. BAH (Bromo Adjacent Homology domain, amino acid 3–188); ELM2 (amino acid 167–221); SANT (SWI3, ADA2, N-CoR and TFIIIB, amino acid 286–333); ZnF_GATA (amino acid 388–448)
The MTA1 gene does not have any apparent membrane-associated regions, nor is there an NH2-terminal signal sequence. Moreover, MTA1 protein is quite hydrophilic, thereby suggesting that MTA1 is not a cell-surface protein, nor is it a secreted protein. This protein contains 12 dispersed cysteine residues, thus indicating the formation of intra- and/or intermolecular disulfide bonds [32]. MTA1 also has two src-homology (SH)-binding motifs at its C-terminal residue. This suggests that MTA1 may have a role in the signal transduction involving many kinase and scaffolding proteins [32, 38]. Interestingly, proline-rich sequences in the carboxyl-terminal region completely matched the consensus sequences of the SH3 domain-binding site. The SH3 domain is one of the well-defined protein domains for protein–protein interactions [32, 39] and has an association with the cytoskeletal structure components [40, 41]. The protein motifs of MTA1 also contain two potential phosphorylation sites for tyrosine kinases. MTA1 was phosphorylated after exposure to the vascular endothelial growth factor (VEGF) but not to MTA1 in MCF-7. VEGF-induced phosphorylation of MTA1 occurred in a time-dependent manner. Then, p38 MAP kinase inhibitor abrogated the VEGF-induced phosphorylation of MTA1.
These diverse domain structures clearly show that MTA1 is involved in protein–protein and the regulation for DNA-binding, thus indicating possible functions in signal transduction and transcriptional regulation. The basic structural analysis indicates that MTA1 is mainly located and functions in the nucleus. In cases of distribution of MTA1 expression, the MTA1 mRNA is expressed at low levels in various normal rat organs, including the brain, heart, lung, liver, and kidney, and that the expression level was the highest in the testis [42]. Recent studies have also observed that the localization of MTA1 and MTA1s, a short splice-variant of MTA1, are clearly localized in the cytoplasm [21, 25, 43, 44]. In another recent report, Liu et al. examined both endogenous and exogenous MTA1 and suggested that MTA1 is localized in the nucleus, cytoplasm, and nuclear envelope [45]. They observed the detectable expression level of MTA1 in all cell lines and tissues (normal/cancerous or adult/embryonic), thus suggesting a wide physiological role for MTA1. Even though MTA1 expression is typically low in normal adult tissue, MTA1 is highly expressed during embryonic development, in nerve network organs, such as the brain, eyes, and spinal cord, thus indicating a potentially important role for MTA1 in nerve development. MTA1 is generally localized in the nucleus, but not in pancreatic acinar cells or in the development process [44]. It seems that the location of MTA1 in cytoplasm during embryogenesis might be involved in the inhibition of differentiation by the cytoplasm-positioned MTA1.
In many types of human cancers including breast and HCC, the increased expressions of MTA1 have been continuously reported [24, 35, 36]. In a recent research report, 95 % of HCC specimens (19 of 20) with vascular invasion showed strong MTA1 expression. Also, overexpression of MTA1 correlated with tumor size [25]. And, the immunohistochemical analysis for MTA1 expression in various grades of human ductal breast carcinoma tissue shows that the intensity was not similar in the three different grades, as more intense expression of MTA1 was detected in Grade III tumor [46]. In addition, nuclear localization of MTA1 was increased during high-stage tumor progression [46]. This result indicates that the expression level and location of MTA1 can be used as an axis of the carcinogenesis stage.
2.2 MTA1 and hepatitis B x protein
Hepatitis B Virus (HBV) infection is considered as one of most potent risk factors for HCC [47]. And, HBV integration into the host genome leads to alteration of the host genome, thus leading to changes of cell proliferation, differentiation, and patient survival. The HBV genome is a circular and highly compacted double-stranded DNA that consists of four overlapping open reading frames (ORFs) encoding seven proteins such as a DNA polymerase, HBV core protein, HBV surface protein, and a regulatory x protein, HBx. Among these proteins, the role of HBx has been emphasized because it is highly involved in the development of HCC [48, 49]. HBx enhances the proliferation of liver cells, whereas downregulation of HBx reduces the tumorigenicity of HCC cells [50–52] (Fig. 2a).
The accruing results show that HBV infection results in the HCC development through the complex interaction between the HBx and multiple host factors. Traditionally, HBx does not bind directly to host DNA but causes transcriptional activation of many genes through interaction with nuclear transcription factors and modulation of cytoplasmic signaling pathways, including Ras, Raf, c-JUN, mitogen-activated protein kinases (MAPKs), nuclear factor-kappa B (NF-κB), signal transducer and activator of transcription (STAT), focal adhesion kinase (FAK), protein kinase C (PKC), and MTA1 [53, 54]. Moreover, HBx can regulate the expression of Notch-1, Jagged-1, and Hes-1, suggesting that HBx may promote the progression to HCC by activating the Notch pathway [55]. Notch signaling is deeply involved in the endothelial cell migration and sprouting from pre-existed vessels in the stalk cells during angiogenesis. Moreover, HBx has been implicated in tumor angiogenesis and metastasis during the development of HCC. HBx induces adherens junction disruption and integrin-mediated adhesion to the extracellular matrix [56, 57]. Decreased expression of junction molecules and detachment of mural cell-endothelial cell interaction are the initial processes for tumor-induced angiogenesis. In addition, the expression of matrix metalloproteinases (MMPs) was induced and enhanced the invasive activity of the HCC cells expressing HBx [58–62]. HBx-induced MMPs activation is associated with an induction of cell migration, thereby suggesting that HBx might facilitate tumor invasion by upregulation of MMPs and subsequent disruption of the ECM boundaries. HBx induces the invasion potential by upregulating the expression of miR-143, and thus leading to tumor metastasis [62, 63]. Among many HBx-interacting factors, MTA1 has been considered a metastasis mediator having a deep relationship with HBx. For a long time, abundant downstream targets of the MTA family have been identified; nevertheless, information regarding the upstream regulators of MTA1 is still generally unknown. Only several factors, such as hypoxia, c-Myc [64], and NF-κB signaling are defined as inducers of MTA1 [65]. In a recent report, HBx was seen to stimulate the transcriptional activation of MTA1, but not of MTA2 or MTA3. The MTA1 gene is also a key transcriptional target of HBx protein, which contributes to angiogenesis in liver cancer by activating HIF-1α and VEGF [52]. It was recently shown that HBx recruits p65 to the NF-κB consensus motif on the relaxed MTA1 gene chromatin [65].
HBx can also recruit DNA methyltransferase 3a (DNMT3a) and 3b to the CpG island of the human MTA1 promoter. When HBx was exogenously introduced in Chang liver cells, the DNMT3a expression level was enhanced [66, 67]. The CpGplot program analysis identifies two potential CpG islands at bases −583 to −459 and −212 to +160 in the human MTA1 promoter. ChIP assay showed that both DNMT3a and DNMT3b bound to the CpG island of MTA1 and the binding were increased in the presence of HBx. Interestingly, HBx, itself, bound to the same region of the promoter. Further, DNMT3a and DNMT3b knock down by siRNA reduced the expression levels of MTA1. However, HBx did not affect the methylation status of the CpG island when DNMT3a and DNMT3b were repressed. It also showed increased expressions of MTA1, DNMT3a, and DNMT3b in the liver of HBx-transgenic mice. These results suggest that HBx increases the transcription of the MTA1 gene by an increase of the MTA1 promoter methylation through recruitment of DNMT3a and DNMT3b [68].
Another pathway for HBx-induced MTA1 expression is by suppressing microRNA-661 (miR-661) and subsequently activating inducible nitric-oxide synthase (iNOS) in liver cancer cells [69, 70]. MicroRNAs (miRNAs) have been identified as post-transcriptional modifiers of target gene regulation and control the expression of gene products important in cancer progression. In recent years, miRNAs have gradually assumed an important role in pathological conditions, including cancer [71–73]. In general, miRNAs act at the 3′ untranslated region of target mRNAs with the help of the RNA-induced silencing complex. Binding of miRNAs to target regions leads to the downregulation of the target mRNA by translational inhibition or degradation of mRNA [74]. Recent research suggests that miRNAs can suppress or activate cancer development and metastasis [75–77]. In a previous research report, human miR-661 compromised MTA1 functions, thus leading to substantial reduction in the motility and invasiveness of breast cancer cells. miR-661 inhibits the expression of MTA1 by targeting the 3′ untranslated (UTR) region of MTA1 mRNA. Then, endogenous miR-661 expression level is then upregulated by the CCAAT/enhancer binding protein alpha (c/EBPα) transcription factor, which is strongly downregulated in many cancers. This indicates that when miR-661 and its activator, c/EBPα, are inhibited during cancer development, they in turn sustain the high expression level of MTA1. Taken together, this suggests that HBx widely affects tumor growth and metastasis through the regulation of multiple cellular mechanisms, such as activation of MTA1, microRNA, and many transcriptional factors.
2.3 MTA1 and angiogenesis
To evaluate the role of MTA1 as a secreted protein, Nagaraj et al. collected the serum from ten different breast cancer patients and measured the presence of MTA1 in the serum. Interestingly, the MTA1 protein was detectable in serum and the measured levels of MTA1 were higher by ten-fold (over 500 pg/mL) in cancer patient serum compared to the level in normal serums (around 50 pg/mL) [46]. This result indicates that MTA1 protein can be secreted from the inside of cells during carcinogenesis and could thus be a prognostic indicator.
In addition, in order to determine the direct evidence for the angiogenic activity of MTA1, Nagaraj et al. performed the rat corneal assay and the CAM assay. The results from these two different in vivo assays showed that the strong angiogenic response was induced in the recombinant MTA1-treated group. In an in vitro assay performed to confirm the angiogenic activities of MTA1, cell migration, tube formation, and endothelial cell (human umbilical vein endothelial cells, HUVECs) proliferation were significantly induced after exposure to MTA1 [46]. Moreover, the transfer of conditioned media from 95D cells (human non-small-cell lung cancer) treating small interfering RNA (siRNA) targeting MTA1, could significantly decrease the tube formation of HUVECs compared to that seen in the control group. This inhibitory pathway might be related to the decrease of MMP-9 [78] (Fig. 2a).
The H&E staining analysis clearly indicated that there is an increase in the number of tumor microvessels in MTA1-positive tumors [46]. The phenomenon of the increased microvessels in tumor might be related to the effects of MTA1 on the VEGF signaling pathway. The VEGF and VEGR receptor (VEGFR1, Flt-1) promoter assay showed that the MTA1 can induce VEGF and Flt-1 expression at the transcriptional level in both HEK-293 and MCF-7 (human breast adenocarcinoma cell-line cells) [46]. VEGFR2 (Flk-1) was then phosphorylated by VEGF but not by MTA1. This result indicates that MTA1 may have its own receptor or effect on VEGFR1 activity to mediate MTA1-induced intracellular signaling and angiogenesis. MTA1 also activated c-Jun N-terminal kinases (JNK) and extracellular regulated kinase (ERK) pathways. Both of these signal mediators are well-known factors for tumor-cell proliferation and angiogenesis.
With regard to another molecular mechanism of the angiogenic activity of MTA1, HIF-1α protein was stabilized in MTA1-overexpressed carcinoma cells (MCF-7, human breast adenocarcinoma; H1299, a human non-small cell lung carcinoma cell line; SK-Hep1, adenocarcinoma of the liver) and resulted in the enhancement of VEGF expression, one of the main target genes of HIF-1α. In detail, MTA1 inhibits the acetylation of HIF-1α by recruiting the histone deacetylase 1 (HDAC1) protein, resulting in the stabilization of HIF-1α [14, 15]. Regulation of HIF-1α stability is mediated by the oxygen-dependent degradation (ODD) domain of HIF-1α, through various post-translational modifications [79]. HIF-1α is hydroxylated at proline residues 402 and 564 by the prolyl hydroxylase domain (PHD) proteins [80, 81]. Hydroxylated HIF-1α subsequently interacts with the tumor suppressor von Hippel–Lindau protein (VHL), which targets it for proteasomal degradation [79, 82]. ARD1 might function as another negative regulatory mediator for HIF-1α by acetylating the lysine 532 residue of HIF-1α. Acetylation of HIF-1α can be coordinated with prolyl hydroxylation and ubiquitination, and which leads to the proteasomal degradation of HIF-1α [83]. The direct interaction between MTA1 and the regulatory proteins of HIF-1α stability has not yet been defined.
2.4 Transcriptional regulation by MTA1
ATP-dependent chromatin-remodeling complexes are known to help transcriptional induction by loosening chromatin structures [84–90]. Xue et al. reported a novel human ATP-dependent chromatin-remodeling complex, known as NuRD. NuRD has ATP-dependent nucleosome disruption activity and histone deacetylase activity. It has been reported that NuRD is generally associated with transcriptional repression. In a recent experiment, MTA1 was also isolated as a subunit of NuRD [58] and the experiment established the novel role of MTA1 protein involving the host inflammatory responses to viral/bacterial products and infections, such as HBx core antigen of HBV and lipopolysaccharide (LPS), through the transcriptional regulation of host-immune responsive genes [65, 70, 91–93]. The detail mechanism for this inflammatory response is that MTA1 is mediated for myeloid differentiation primary response gene 88 (MyD88)-dependent stimulation of NF-κB signaling and expression of inflammatory cytokines such as interleukin-1β (IL-1β) and tumor necrosis factor α (TNF-α). MTA1 depletion also resulted in the reduction of NF-κB target genes expression [94]. In addition, the functional activation of NF-κB to induce inflammatory responses might be deeply related to HDAC2 [93].
In the following studies, the MTA1/NuRD complex was reported to be a transcriptional repressor of p21WAF1 and as hypermethylated in cancer 1 (HIC1), as those are direct targets of tumor suppressors p53 [95–98]. A recent study also suggested the possibility that MTA1 develops oncogenesis by induction of CONSTITUTIVELY PHOTOMORPHOGENIC1 (COP1) degradation in an auto-ubiquitination manner. COP1 has tumor suppressor activity. COP1 acts as an E3 ubiquitin-protein ligase and induces ubiquitination of substrates. In addition, COP1 also has a role as a tumor suppressor by negative regulation of the proto-oncogenes ETS variant 1 (ETV1) and c-Jun stability [99–101]. The MTA2-HDAC1 complex has also been reported to repress p53 to stimulate the transcription of genes important in growth and apoptosis [102]. However, MTA family members exist in distinct NuRD complexes, and functional redundancy is not reported between MTA1 and MTA2 protein [36].
For a wide screening of the physiological mechanism of MTA1 in DNA repair, a research group attempted to identify the differences between the MTA1−/− and MTA1−/− mouse embryonic fibroblasts (MEFs). From the initial 5,602 statistically significant probes, the inclusive list of genes totaled 1,124 probes which were screened. Among them, 716 were upregulated and 408 were downregulated in the MTA1−/− MEFs compared with the MTA1−/− controls. This indicates that MTA1 is involved in both gene induction and repression [95]. As discussed above, as the results continue to accumulate regarding MTA1 functions, it seems that the physiologic levels of MTA1 participate in the inflammatory response, although the overexpressed MTA1 is involved in carcinogenesis [36, 103–105].
2.5 MTA1 and epithelial–mesenchymal transition
The idea that epithelial cells can downregulate epithelial characteristics and obtain mesenchymal characteristics was originally observed by Elizabeth Hay [106, 107]. In her original report, she described as it as “epithelial to mesenchymal transformation”, and this process is now called “epithelial–mesenchymal transition (EMT)”. Mesenchymal–epithelial transition (MET) is known as the reverse process of EMT. EMT has been related to the stem-cell potential for development and cancer progression [107]. Similar to epithelial cells, endothelial cells can transform into a mesenchymal phenotype, a process known as endothelial–mesenchymal transition (EndMT) [108, 109]. EndMT also provides a major source of cancer-associated fibroblasts that contribute to oncogenesis [110]. Transforming growth factor-beta1 (TGF-β1) signaling affecting SMADs can induce both EndMT and EMT. TGF-β also activates the SNAILs expression, which is deeply involved in the induction of EMT and EndMT, and represses the expression of VE-cadherin, CD31 (also known as PECAM, endothelial cell marker protein), and claudin-5 [109, 111, 112].
Human epidermal growth factor receptor 2 (HER-2) is an important prognostic protein in breast cancer [113]. Metastasis-related proteins such as c-Met (also known as hepatocyte growth factor (HGF) receptor, HGFR), VEGF, and MTA1 are activated by HER-2 [114]. Moreover, HGF is known as a multifunctional cytokine that enhances the metastatic potential of epithelial tumor cells through the c-Met [115, 116]. Recently, HGF was also identified as an inducer of epithelial to fibroblast-like cells [117]. HGF induces SNAIL1 and SNAIL2 (also known as SLUG) expression leading to EMT [118, 119]. Immunoprecipitation analysis showed an association between c-Met and the cadherin adhesion complex members in these epithelial tumor cells [120], although the role of this interaction in the EMT process has not as yet been clarified. Even though MTA1 and HGF definitely interact to induce tumor metastasis, there is still no clear evidence regarding the relationship between MTA1 and HGF receptor c-Met or HGF ligand during EMT.
A recent study identified TGF-β as a potent inducer of MTA1 transcription and expression, as well as MTA1 as a downstream effector of TGF-β, and which mediates the repression of epithelial-cadherin (E-cadherin) expression [121] (Fig. 2b). E-cadherin has an important role in epithelial cell–cell adhesion and in the maintenance of tissue architecture. Therefore, reduction or E-cadherin promotes EMT and tumor progression [122]. The underlying basis of MTA1-mediated regulation of E-cadherin includes the dual coregulatory nature of MTA1, wherein the MTA1/Pol II coactivator complex stimulates the expression of FosB, which in turn interacts with the MTA1/NuRD corepressor to inhibit the transcription of E-cadherin [121]. Thus, activation of the TGF-β1–MTA1–cadherin axis is emerging as a central feature of EMT and metastasis in epithelial cells. MTA1 also affects the activation of SNAIL1 and SNAIL2 in ovarian cancer cells [123]. Both SNAIL1 and SNAIL2 proteins are direct transcriptional repressors of E-cadherin, and their expression induces EMT [124]. Therefore, it is possible that oncogenic MTA1 exploits multiple signaling pathways to activate EMT programs, directly or indirectly, during cancer invasion and metastasis. Therefore, several recent findings show MTA1 to interject into the HIF-1α, and Wnt1 pathways, and which have been implicated in EMTs through multiple distinct mechanisms [14, 15, 41, 125]. However, it is not yet defined whether MTA1 is involved in the disruption of the cell–cell junction to promote EMT. Furthermore, the possibility that the knockdown of MTA1 expression can lead to the MET should be determined in order to understand the detailed carcinogenesis mechanism.
3 Clinicopathological significance of MTA
3.1 MTA expression in non-cancerous tissue
A recent study reported that MTA1 was expressed in all normal human tissue on immunohistochemical staining, although the expression levels differed greatly, when they used 24 human adult tissues and 8 mouse adult tissues [45]. This study found that a low level of MTA1 was expressed in most normal human tissue, except in the brain, liver, kidney, and cardiac muscle, and thus suggesting that MTA1 may have important physiological roles in these tissues. They also observed that MTA1 localized to both the nucleus and cytoplasm and accumulated in the nucleus. Another study showed that a low level of MTA1 was also present in hepatocytes of background cirrhotic and normal-appearing liver tissue compared with significantly stronger MTA1 expression in HCC. They reported that the MTA1 was overexpressed in 31 of 45 (69 %) HCC specimens compared with non-malignant hepatocytes. The MTA1 expression was also predominantly localized to the nucleus, although in some cells it was localized to the cytoplasm or to both the nucleus and cytoplasm in HCC cells [25]. However, in our previous study, MTA1 was stained in 88 (17 %) of the 506 HCC samples, but none of the surrounding liver tissue was stained. The nuclear staining was also diffuse and there were no other staining patterns such as membranous, nucleolar, or speckled patterns that could be observed in cases of other nuclear proteins [27]. Our other study showed that MTA1 was overexpressed in 34.3 % of HCC tissues, although in none of the surrounding non-tumor tissues [30].
Taken together, MTA1 expression can be noted in normal and cirrhotic liver tissue and is more strongly stained in HCC tissue. There is no MTA1 overexpression in all HCC tissue with different expression levels. The expression is predominantly localized to the nucleus, although in some cells it is localized to the cytoplasm or to both the nucleus and cytoplasm in HCC cells.
3.2 MTA expression in HCC tissue
In our previous study, the level of MTA1 expression was higher in HCC patients with larger tumors (Fig. 3a–f). The MTA1 expression levels of the HCCs greater than 3 cm in diameter was higher than those of the HCCs with less than a 3-cm diameter. In addition, regarding the tumor type, the level of MTA1 expression was lower in the nodular type of HCC than in other types of HCC, such as perinodal, multinodular confluent, pedunculated, and diffuse infiltrative types, in the 434 HCC cases we analyzed. MTA1 expression also differed according to the degree of histologic differentiation of HCC. Increased MTA1 expression levels tended to be associated with worse histologic differentiation of HCC. In addition, the MTA1 expression levels in patients with microvascular emboli on frozen tissues were much greater than in those of patients without microvascular emboli [27].
Different causes of liver disease were associated with differences in MTA1 expression levels [27]. Of the 484 patients, 380 had HBV, 27 had HCV, and 8 had both HBV and HCV. A total of 69 patients had a non-viral hepatitis cause of HCC. Interestingly, MTA1 was expressed in 80 of 380 patients with HBV-associated HCC (21.1 %), but in only one patient (3.4 %) with HCV-associated HCC. None of the HCCs from the patients with HBV and HCV coinfection had MTA1 expression (0 %, 0/8). In HCCs with non-viral causes, 7 % (5/69) had weak MTA1 expression and in 3 % (2/69) the level showed a strong expression of MTA1. The MTA1 overexpression was much more common in HBV-associated HCC compared with HCV-associated or other cause-associated HCC, thus indicating that there might be a relationship between MTA1 and HBx. Yoo et al. supported this data suggesting that HBV x protein induces the expression of MTA1 and HDAC1 which enhances hypoxia signaling via HIF-1α stabilization in HCC cells [52]. There was no association between MTA1 expression levels and age, gender, Child–Turcotte–Pugh (CTP) class of liver disease, decompensation of liver function, or capsule invasion of HCC.
Our other study reported factors predisposing MTA1 overexpression in 303, HBV-associated, HCC patients who underwent surgical resection. In that study, MTA1 overexpression was significantly associated with younger patient age, female gender, a higher serum alpha-fetoprotein (AFP) level, and CTP class A. Portal vein thrombosis, microvascular invasion, capsular invasion, and poor histological differentiation were also associated with the overexpression of MTA1 [30]. In their study, there was no significant relationship between the size of HCC and MTA1 overexpression. They explained that interesting overexpression of MTA1 in patients with CTP class A compared with those patients with CTP class B may be caused by a higher protein synthetic capacity of these patients, who can express biomarkers including MTA1 much higher than those with CTP class B or C. Moon et al. reported that high MTA1 expression levels were correlated with large tumors and vascular invasion based on the analysis of paraffin sections from 45 HCC specimens [25]. Hamatsu et al. showed that high MTA1 mRNA expression levels were more often seen in poorly differentiated HCC than in well- or moderately differentiated HCC; however, they found no association between the MTA1 gene expression levels and cancer invasion to the portal vein or intrahepatic metastasis [26].
4 MTA family as a prognostic factor
4.1 General concepts
The MTA family is reported to be upregulated in various tumors, as mentioned above. Regarding the aspect of prognosis, a wide range of recent studies have clinicopathologically proven the relationship between cancer behaviors and overexpression of MTA family [35]. Recent studies have revealed that MTA1 overexpression may indicate the invasiveness of the malignancies acting through migration and invasion of cancer cells toward surrounding and distant tissues, e.g., a greater amount of lymph node metastasis or early recurrence in breast cancer [17, 82], a deeper invasion of gastrointestinal cancers involving the esophagus, stomach, and colon [20, 22], a larger size of lung cancer [23], and the metastasis of prostate cancer [19]. We have also shown that both MTA1 and MTA2 can function as useful prognostic factors in HCC. In this section, we will discuss in detail the association of the MTA family with the patient prognosis and survival in those with HCC, focused on our previous clinical experience.
4.2 MTA1 as a prognostic factor in patients with HCC
HCC is clinically characterized with the worst patient survival rate and/or the gravest prognosis among all malignancies as it is therapeutically resectable in approximately only 10–20 % of patients. The reasons why most of them are untreatable are its advanced stages with an unresectable size and multiple tumors, the existence of intrahepatic or distant metastases, and vascular invasion as well as poor reserved liver function at presentation [4, 5]. Moreover, the post-operative recurrence rate in 2 years is so high that it reduces the long-term survival even after complete resection of the HCC [9, 10].
Regarding metastasis-associated proteins in cancers, MTA1, a stabilizer of HIF-1α during angiogenesis, is suggested to be closely correlated with the aggressiveness in human cancers [24]. It is hypothesized that the MTA family may have a specific role during the angiogenesis or metastasis of HCC, considering that it is a prototype of hypervascular tumors, and is then identified as a prognostic factor for determining recurrence or patient survival. There are, however, only a limited number of reports demonstrating its role as a prognostic factor in HCC in terms of the tumor burden, invasiveness, recurrence, and patient survival (Table 1). The most important message derived from the previous clinical studies is that the MTA family is overexpressed in HCCs with a larger size, poorly differentiated histology, and microvascular invasion, and thus resulting in a worse survival or more frequent post-operative recurrence [25–29]. We previously performed a large-scale study with a total of 506 patients who underwent curative surgery, in order to investigate the relationship of MTA1 overexpression in HCC with post-operative recurrence after surgical resection and subsequently associated with the patients’ survival rate [27]. As mentioned above, tumor size, worse histologic differentiation, and microvascular invasion, which are the markers for invasiveness and the metastatic potential, were closely correlated with the level of MTA1 expression in HCC. Taken together, MTA1 is thought to be important in tumor-cell migration, invasion, and metastasis at the in vivo level as well as at the in vitro level. Regarding post-operative recurrence or disease-free survival after curative hepatectomy, as mentioned above, MTA1 may affect cell differentiation and intrahepatic metastasis via vigorous angiogenesis. Furthermore, MTA1 overexpression was significantly associated with a higher recurrence and a shorter survival even after curative treatment [25, 26].
One of the remarkable findings in our study [27] is that the majority of the etiologies of HCC consisted of chronic HBV infection (75 %, 380 of 506 HCCs). Interestingly, MTA1 was overexpressed in 21 % of HBV-associated HCCs, whereas in 3.4 % of HCV-associated HCCs. This suggests the probability of MTA1 involvement in hepatitis B virus x protein (HBx)-induced angiogenesis by stabilizing HIF-1α. Actually, HBx, HIF-1α, and VEGF are more strongly detected in dysplastic lesions than in non-neoplastic lesions in HBx-transgenic mice [126]. On the one hand, MTA1 is considered an essential downstream effector of the c-MYC oncoprotein at molecular levels [127]. On the other hand, HBx may potentiate c-MYC-induced hepatocarcinogenesis by inhibiting the ubiquitination and proteasomal degradation of c-MYC [128]. HBx also accelerates metastasis by tumor-cell invasion and destruction of the extracellular matrix by upregulation of MMPs [129]. Accordingly, the analysis of our study’s subgroup composed of HBV-associated HCCs, demonstrates that MTA1 and HBx may interact with each other during oncogenesis. It is clinically meaningful that the levels of MTA1 expression in HCC can predict the overall patient prognosis on the basis that its overexpression is related to tumor size, histologic differentiation, microvascular invasion, post-operative recurrence, and even patient survival, especially in HBV-associated HCCs.
4.3 MTA2 as a prognostic factor in patients with HCC
Although the MTA family is reported to be closely linked to tumor progression and metastasis [17, 18, 20, 22, 23, 25–29, 130], the role of MTA2, compared with that of MTA1, is scarcely known in the fields of hepatocarcinogenesis, HCC progression, and metastasis. Basically, MTA2 interacts with p53 followed by inhibition of p53-mediated cell-growth arrest and apoptosis by deacetylation [102]. It is, therefore, probable that MTA2 also contributes to HCC progression and subsequently to the post-operative recurrence or the patients’ survival. It encouraged us to perform another study to investigate whether MTA2 is related to HCC progression when human HCC samples were used for immunohistochemistry [28]. In the study, the levels of MTA2 expression seen on immunohistochemistry depended on the HCC size and its differentiation, similar to that of MTA1. This may suggest that upregulation of MTA2 has a specific role in HCC progression. According to one study, MTA2 is especially overexpressed in rapidly dividing cells [130]. Herein, MTA2 overexpression was well-matched with tumor size. Of the transcriptional factors, p53 activity can be modulated by interacting with MTA2, and thus resulting in a reduced steady-state level of acetylated p53. MTA2 also inhibits p53-mediated cell-growth arrest and apoptosis [102]. Considering the fact that MTA2 modulates p53-mediated cell growth and apoptosis, deacetylation of p53 by MTA2 contributes to the tumor size or its aggressiveness, as seen in our study. Despite the reasonable speculations as well as its reliable relationship to the HCC size and poorer differentiation, the MTA2 expression level was not statistically associated with portal vein thrombosis, capsule invasion, a satellite nodule, microvascular invasion, or even with metastasis. Consequently, MTA2 overexpression did not predict post-operative recurrence. Taken together, MTA2 seems to be inferior to MTA1 as a prognostic or survival predictor in patients with HCC.
4.4 Single-nucleotide polymorphism of the MTA1 gene as a prognostic factor
Since we have shown the close association of MTA1, a pro-angiogenic factor, with frequent post-operative recurrence and poor survival in patients with HCC, another study was performed to investigate single-nucleotide polymorphisms (SNPs) in angiogenesis-related genes that are associated with MTA1 overexpression in HCC [29]. As is well known, angiogenesis, a new vessel formation from pre-existing vessels, is highly critical for HCC progression and metastasis. Angiogenesis in HCC in detail refers to the reference [131]. Being particular to HCC, besides VEGF, insulin-like growth factor-II (IGF-II), and HIF-1α [132–134], MTA1 can be a good candidate for determining the significance of SNPs in HCC. Briefly, MTA1 stabilizes HIF-1α, thus leading to an increase in the transcriptional activity of HIF-1α. It then enhances angiogenesis through VEGF and IGF-II pathways, which is a target of HIF-1α [14]. However, it remains to be clarified whether MTA1 SNP may affect the clinical course of HCC due to the lack of data.
According to our recent study [29], an A allele at position IVS4-81G/A of the MTA1 gene (P = 0.016) was significantly associated with MTA1 overexpression. Importantly, it was consequently an independent risk factor for post-operative recurrence of HCC, as seen on multivariate analysis. If we can screen and then use specific gene polymorphisms data that diversify the clinical course of HCC or determine the post-operative destiny of HCC patients, we can let the clinicians delicately design the therapeutic strategy before treatment. It will be also valuable to identify new therapeutic targets for HCC in gene therapies. In clinical practice, the results of immunohistochemistry of pre-operative HCC tissues or SNPs may determine the need for post-operative adjuvant therapy. The study was performed only in a specific geographic area (the Far East), with a single ethnic group (Koreans), and with HBV being the main etiology of HCC. It cannot, therefore, be generalized that the polymorphism IVS4-81G/A in MTA1 is associated with MTA1 overexpression in HCC and is an independent prognostic predictor in other populations. The reliability of such findings should be confirmed in a wide range of study subjects worldwide in order to be able to apply them in clinical settings.
4.5 Predisposing factors for MTA1 overexpression in HBV-associated HCC
Thus far, we primarily described the clinical significance of the MTA family as a prognostic or survival factor in HCC patients. All of the studies to date have consistently, more or less demonstrated that the MTA family is overexpressed in invasive or aggressive HCC, and which is suggestive of its pro-angiogenic property. Interestingly, our studies have still underlined the probability of accentuated roles of MTA1 in HBV-associated HCC [27–29]. If MTA1 is clinically useful for predicting the course of HCC post-operatively or of the patients’ survival, are there any clinically predisposing factors for MTA1 overexpression in HCC? A recent study we performed was intended to determine the clinical factors predisposing MTA1 overexpression in HBV-associated HCC (n = 303 patients) [30]. Of the parameters clinically obtained at bedside or in a laboratory, younger age, female gender, a higher serum AFP level, and CTP class A were significantly associated with MTA1 overexpression in HCC. The relationship of MTA1 overexpression with portal vein thrombosis, microvascular invasion, capsular invasion, and poor histological differentiation were the same as those seen in previous studies [27–29]. It is probable that MTA1 may have a critical role in HCC development or progression in unusual conditions of HCC such as younger age, female gender, and good reserved liver function (CTP class A). Collectively, a huge burden of HCC (higher AFP level) in younger female patients and/or good reserved liver function may predict MTA1 overexpression. In those cases, another adjuvant therapy must be post-operatively selected so as to prevent HCC recurrence.
4.6 MTA3 as a prognostic factor
MTA3 also interacts with cell signaling pathways to take part in tumor progression and metastasis. Actually, it is highly upregulated in several cancers, including lung, breast, and esophagus [135–137]. A recent study showed the association of miR-495 with lung cancer and growth [138]. Such information can be expanded to the field of hepatology and will be valuable in the future when anti-cancer target therapy using microRNA is designed. As there are regrettably no commentable data regarding the role of MTA3 in HCC progression or metastasis, we currently do not mention this issue.
5 MTA as a therapeutic target in HCC
5.1 Post-operative adjuvant therapy
As described above, HCC is clinically characterized by its frequent post-operative recurrence which may require adjuvant therapy in selected cases in order to prevent recurrence and prolong the patient survival period. Although a number of options as post-operative, adjuvant therapy have been attempted, to date, there is no universal, single therapy due to the heterogeneity of the HCC features, themselves, or to the baseline characteristics of these patients. As a matter of fact, none of the anti-cancer agents used post-operatively, such as interferon-alpha, interferon-beta, iodine-125 brachytherapy, autologous tumor vaccination, adoptive immunotherapy, acyclic retinoid, vitamin K2 analog, iodine-131-labeled lipiodol, sorafenib, heparanase inhibitor PI-88, or capecitabine, reveal consistently promising benefits in terms of recurrence-free survival or overall survival [139]. Therefore, many recent studies have focused on the molecular targets involved in the diverse pathways of hepatocarcinogenesis in order to complement such limitations of the given adjuvant therapies, e.g., VEGF, epidermal growth factor (EGF), IGF, Ras/Raf/MEK/ERK, PI3K/Akt/mTOR, and Met proto-oncogene (MET). Several drugs targeted at molecular levels have been introduced for clinical use and have been approved for treating specific cancers, including HCC, which are under phase II or II study [140]. However, to our knowledge, there is no study regarding MTA1 as a molecular target, at least in HCC.
5.2 Clinical application of MTA1
Provided that HCC is a prototype of hypervascular tumors and that the most important underlying pathophysiology in HCC development or progression is then angiogenesis [140], it is theoretically reasonable that different antiangiogenic agents can be used as post-operative adjuvant drugs. On the other hand, MTA1 is located in the middle of angiogenic pathways during hepatocarcinogenesis and modulates HIF-1α, thus leading to determining the VEGF expression. Therefore, MTA1 will become another future molecular target of anti-HCC therapy or its expression levels of MTA1 in HCC tissue will be applied to guide the options to be chosen as post-operative adjuvant therapy in order to prevent HCC recurrence. As we suggested, anti-angiogenic chemotherapy may reduce the recurrence rates in selected patients whose HCC shows MTA1 overexpression indicative of hyperactive angiogenesis. Of the proposed agents, interferon is known to have anti-tumorigenic effects in HCC, even in patients with only a partial response in viral eradication, although this is controversial to some degree [141, 142]. In a recent randomized clinical trial, post-operative interferon-alpha treatment was beneficial as it reduced the recurrence rates and improved overall survival rate in patients after curative resection of HBV-related HCC [143].
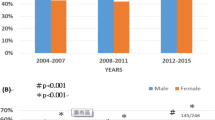
On the basis of our findings [27–29], we hypothesized that post-operative adjuvant therapy using pegylated interferon (Peg-IFN) is effective in the prevention of recurrence after curative resection in MTA1 overexpressed HCCs. The prospective, case–control study showed that the overall cumulative recurrence rates at 1 and 2 years were significantly lower in the Peg-IFN group (n = 31) than in the control group (n = 62) (7 and 14 % vs. 24 and 34 %, respectively; P < 0.05). Undergoing post-operative adjuvant Peg-IFN therapy was one of the favorable independent factors for a lower post-operative recurrence seen in multivariate analysis. Overall survival was also tended to be longer in the Peg-IFN group compared to the control group (100 % vs. 87 % at year two; P < 0.05 in univariate analysis) [31]. It is possibly an anti-cancer mechanism that Peg-IFN may exert an anti-angiogenic activity by downregulation of HIF-1α expression that results in VEGF suppression [144]. Taken together, post-operative adjuvant therapy using Peg-IFN, an anti-angiogenic agent, may be more effective if the candidates are carefully selected, e.g., MTA1-overexpressed, angiogenesis-predominant HCC rather than a MTA1-negative one. Randomized, multi-centered trials enrolling a large number of patients will be warranted in the future.
6 Discussion and conclusions
MTA1, an 80-kDa protein which is a substrate of the transcriptional regulatory complex NuRD, was recently identified as a metastasis-associated protein [27–30, 32, 33, 53]. MTA1 has an important role in the adverse course of various human cancers, including breast, prostate, lung, colorectal, gastric, and esophageal cancers, through migration and invasion of cancer cells toward surrounding and distant tissues [17–24].
In HCC, until a few years ago, only a small number of studies had examined the role of MTA1 in vascular invasion and patient survival after treatment. The MTA1 expression levels in HCC tissue were greater in patients with large tumors, worse histologic differentiation, and microvascular emboli. However, there was no association between the MTA1 expression level and patient age, gender, CTP class of underlying liver cirrhosis, decompensation of liver function or capsule invasion of HCC. These results are in agreement with those of previously published reports [25, 26]. MTA1 overexpression was also significantly related to younger age, female gender, higher serum AFP level, and CTP class A. Larger tumors and tumors with worse histologic differentiation have the potential to invade microvessels and metastasize to distant sites from primary tumors, thereby leading to shorter disease-free survival despite curative surgery. MTA1 is thought to be an important factor for tumor-cell migration, invasion, and metastasis, and the MTA1 expression levels were much higher in HCC patients with large tumors and poor tumor differentiation. The patients with higher MTA1 expression levels showed high recurrence rates and shorter survival times after curative treatment such as surgery. The 1-, 3- and 5-year cumulative recurrence rates after curative hepatectomy were much higher in MTA1-positive HCC. The 1-, 3-, and 5-year cumulative survival rates were also much lower in MTA1-positive HCC.
MTA1 was much more expressed in patients with HBV-associated HCC compared to the other causes associated with HCC. This can be explained by the fact that HBx protein induces the expression of MTA1 and HDAC1, and which enhances hypoxia signaling via HIF-1α stabilization in HCC cells. HBx also induces angiogenesis by stabilizing HIF-1α and HBx increases the transcriptional activity and protein stability of HIF-1α under both normoxic and hypoxic conditions by reducing the binding of von Hippel–Lindau protein to HIF-1α and preventing the ubiquitin-dependent degradation of HIF-1α. MTA1, itself, also induces increased transcriptional activity and the stability of HIF-1α protein through the deacetylation of HIF-1α by increasing the expression level of HDAC1 [26–28]. These findings indicate a close correlation between MTA1-associated metastasis and HIF-1α-induced tumor angiogenesis.
MTA1 is also an essential downstream effector of the c-MYC oncoprotein [137]. HBx not only potentiates c-MYC-induced liver oncogenesis in transgenic mice but also inhibits the ubiquitination and proteasomal degradation of c-MYC. HBx also promotes HCC metastasis by facilitating tumor-cell invasion and subsequent destruction of the extracellular matrix by upregulation of MMPs [27, 138, 139]. Collectively, both MTA1 and HBx induce angiogenesis by stabilizing HIF-1α and increasing the c-MYC oncogene function. HBx also activates the Twist promoter by stimulating STAT3 and induces the EMT process in liver cells. EMT is recently considered as another significant source of liver fibrosis, metastasis, and several other organs. There is also evidence that the inhibition of NF-κB reduces liver fibrosis via inhibition of the EMT process [145, 146]. Moreover, MTA1 activation by TGF-β is involved in the promotion of EMT [121, 123]. However, the co-relationship between HBx and MTAs during the EMT process has not yet been defined.
Although a number of options as a post-operative adjuvant therapy have been attempted in order to prevent recurrence and prolong patient survival, to date there is no universal, single, established treatment. Therefore, many recent studies have focused on the molecular targets involved in the diverse pathways of hepatocarcinogenesis. Several drugs targeted at molecular levels have been introduced into clinical use and approved for specific cancers including HCC, and which are under phase II or III study [140]. However, there is no study focused on MTA1 as a molecular target in HCC patients.
In conclusion, MTA1 expression in HCC is closely associated with larger tumor size, worse histologic differentiation, and microvascular invasion. MTA1 overexpression in HCC tissue can predict frequent post-operative recurrence and poor patient survival, especially in HBV-associated HCCs. Therefore, the expression levels of MTA1 in HCC tissues might be an important prognostic marker after curative surgery. In addition, various molecular-targeted therapies are under development and experimentation in HCC patients. Molecular targeted therapy focused on MTA1 is expected to prevent metastasis and to enhance survival in HCC patients in the future.
References
Bosch, F. X., Ribes, J., Diaz, M., & Cleries, R. (2004). Primary liver cancer: worldwide incidence and trends. Gastroenterology, 127(5 Suppl 1), S5–S16.
Kiyosawa, K., Umemura, T., Ichijo, T., Matsumoto, A., Yoshizawa, K., Gad, A., et al. (2004). Hepatocellular carcinoma: recent trends in Japan. Gastroenterology, 127(5 Suppl 1), S17–S26.
El-serag, H. B. (2004). Hepatocellular carcinoma: recent trends in the United States. Gastroenterology, 127(5 Suppl 1), S27–S34.
Chen, M. F., Hwang, T. L., Jeng, L. B., Jan, Y. Y., Wang, C. S., & Chou, F. F. (1989). Hepatic resection in 120 patients with hepatocellular carcinoma. Archives of Surgery, 124(9), 1025–1028.
Tsuzuki, T., Sugioka, A., Ueda, M., Iida, S., Kanai, T., Yoshii, H., et al. (1990). Hepatic resection for hepatocellular carcinoma. Surgery, 107(5), 511–520.
Nagorney, D. M., van Heerden, J. A., Ilstrup, D. M., & Adson, M. A. (1989). Primary hepatic malignancy: surgical management and determinants of survival. Surgery, 106(4), 740–748.
Llovet, J. M., Fuster, J., & Bruix, J. (1999). Intention-to treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology, 30(6), 1434–1440.
Okada, S., Shimada, K., Yamamoto, J., Takayama, T., Kosuge, T., Yamasaki, S., et al. (1994). Predictive factors for postoperative recurrence of hepatocellular carcinoma. Gastroenterology, 106(6), 1618–1624.
Adachi, E., Maeda, T., Matsumata, T., Shirabe, K., Kinukawa, N., Sugimachi, K., et al. (1995). Risk factors for intrahepatic recurrence in human small hepatocellular carcinoma. Gastroenterology, 108(3), 768–775.
Kumada, T., Nakano, S., Takeda, I., Sugiyama, K., Osada, T., Kiriyama, S., et al. (1997). Patterns of recurrence after initial treatment in patients with small hepatocellular carcinoma. Hepatology, 25(1), 87–92.
Mahoney, M. G., Simpson, A., Jost, M., Noe, M., Kari, C., Pepe, D., et al. (2002). Metastasis-associated protein (MTA) 1 enhances migration, invasion, and anchorage-independent survival of immortalized human keratinocytes. Oncogene, 21(14), 2161–2170.
Hofer, M. D., Menke, A., Genze, F., Gierschik, P., & Giehl, K. (2004). Expression of MTA1 promotes motility and invasiveness of PNAC-1 pancreatic carcinoma cells. British Journal of Cancer, 90(2), 455–462.
Nicolson, G. L., Nawa, A., Toh, Y., Taniguchi, S., Nishimori, K., & Moustafa, A. (2003). Tumor metastasis-associated human MTA1 gene and its MTA1 protein product: role in epithelial cancer invasion, proliferation and nuclear regulation. Clinical and Experimental Metastasis, 20(1), 19–24.
Moon, H. E., Cheon, H., Chun, K. H., Lee, S. K., Kim, Y. S., Jung, B. K., et al. (2006). Metastasis-associated protein 1 enhances angiogenesis by stabilization of HIF-1alpha. Oncology Reports, 16(4), 929–935.
Yoo, Y. G., Kong, G., & Lee, M. O. (2006). Metastasis-associated protein 1 enhances stability of hypoxia-inducible factor-1alpha protein by recruiting histone deacetylase 1. EMBO Journal, 25(6), 1231–1241.
Kim, S. H., Jeong, J. W., Park, J. A., Lee, J. W., Seo, J. H., Jung, B. K., et al. (2007). Regulation of the HIF-1alpha stability by histone deacetylases. Oncology Reports, 17(3), 647–651.
Jang, K. S., Paik, S. S., Chung, H. K., Oh, Y. H., & Kong, G. (2006). MTA1 overexpression correlates significantly with tumor grade and angiogenesis in human breast cancer. Cancer Science, 97(5), 374–379.
Martin, M. D., Hilsenbeck, S. G., Mohsin, S. K., Hopp, T. A., Clark, G. M., Osborne, C. K., et al. (2006). Breast tumors that overexpress nuclear metastasis-associated 1 (MTA1) protein have high recurrence risks but enhanced responses to systemic therapies. Breast Cancer Research and Treatment, 95(1), 7–12.
Hofer, M. D., Kuefer, R., Varambally, S., Li, H., Ma, J., Shapiro, G. I., et al. (2004). The role of metastasis-associated protein 1 in prostate cancer progression. Cancer Research, 64(3), 825–829.
Toh, Y., Ohga, T., Endo, K., Adachi, E., Kusumoto, H., Haraguchi, M., et al. (2004). Expression of the metastasis-associated MTA1 protein and its relationship to deacetylation of the histone H4 in esophageal squamous cell carcinomas. International Journal of Cancer, 110(3), 362–367.
Balasenthil, S., Broaddus, R. R., & Kumar, R. (2006). Expression of metastasis-associated protein 1 (MTA1) in benign endometrium and endometrial adenocarcinomas. Human Pathology, 37(6), 656–661.
Toh, Y., Oki, E., Oda, S., Tokunaga, E., Ohno, S., Maehara, Y., et al. (1997). Overexpression of the MTA1 gene in gastrointestinal carcinomas: correlation with invasion and metastasis. International Journal of Cancer, 74(4), 459–463.
Sasaki, H., Moriyama, S., Nakashima, Y., Kobayashi, Y., Yukiue, H., Kaji, M., et al. (2002). Expression of the MTA1 mRNA in advanced lung cancer. Lung Cancer, 35(2), 149–154.
Kumar, R., Wang, R. A., & Bagheri-Yarmand, R. (2003). Emerging roles of MTA family members in human cancers. Seminars in Oncology, 30(5 suppl 16), 30–37.
Moon, W. S., Chang, K., & Tarnawski, A. S. (2004). Overexpression of metastatic tumor antigen 1 in hepatocellular carcinoma: relationship to vascular invasion and estrogen receptor-α. Human Pathology, 35(4), 424–429.
Hamatsu, T., Rikimaru, T., Yamashita, Y., Aishima, S., Tanaka, S., Shirabe, K., et al. (2003). The role of MTA1 gene expression in human hepatocellular carcinoma. Oncology Reports, 10(3), 599–604.
Ryu, S. H., Chung, Y. H., Lee, H., Kim, J. A., Shin, H. D., Min, H. J., et al. (2008). Metastatic tumor antigen 1 is closely associated with frequent post-operative recurrence and poor survival in patients with hepatocellular carcinoma. Hepatology, 47(3), 929–936.
Lee, H., Ryu, S. H., Hong, S. S., Seo, D. D., Min, H. J., Jang, M. K., et al. (2009). Overexpression of metastasis-associated protein 2 is associated with hepatocellular carcinoma size and differentiation. Journal of Gastroenterology and Hepatology, 24(8), 1445–1450.
Lee, S. H., Chung, Y. H., Kim, J. A., Lee, D., Jin, Y. J., Shim, J. H., et al. (2011). Single nucleotide polymorphisms associated with metastatic tumor antigen 1 overexpression in patients with hepatocellular carcinoma. Liver International, 32(3), 457–466.
Jin, Y. J., Chung, Y. H., Kim, J. A., Park, W. H., Lee, D., Seo, D. D., et al. (2012). Factors predisposing metastatic tumor antigen 1 overexpression in hepatitis B virus associated hepatocellular carcinoma. Digestive Diseases and Sciences, 57(11), 2917–2923.
Lee, D., Chung, Y. H., Kim, J. A., Park, W. H., Jin, Y. J., Shim, J. H., et al. (2013). Safety and efficacy of adjuvant pegylated interferon therapy for metastatic tumor antigen 1-positive hepatocellular carcinoma. Cancer, 119(12), 2239–2246.
Yao, Y. L., & Yang, W. M. (2003). The metastasis-associated proteins 1 and 2 form distinct protein complexes with histone deacetylase activity. Journal of Biological Chemistry, 278(43), 42560–42568.
Toh, Y., Pencil, S. D., & Nicolson, G. L. (1995). Analysis of the complete sequence of the novel metastasis-associated candidate gene, mta1, differentially expressed in mammary adenocarcinoma and breast cancer cell lines. Gene, 159(1), 97–104.
Pencil, S. D., Toh, Y., & Nicolson, G. L. (1993). Candidate metastasis-associated genes of the rat 13762NF mammary adenocarcinoma. Breast Cancer Research and Treatment, 25(2), 165–174.
Toh, Y., & Nicolson, G. L. (2009). The role of the MTA family and their encoded proteins in human cancers: molecular functions and clinical implications. Clinical and Experimental Metastasis, 26(3), 215–227.
Manavathi, B., & Kumar, R. (2007). Metastasis tumor antigens, an emerging family of multifaceted master coregulators. Journal of Biological Chemistry, 282(3), 1529–1533.
Nawa, A., Nishimori, K., Lin, P., Maki, Y., Moue, K., Sawada, H., et al. (2000). Tumor metastasis-associated human MTA1 gene: its deduced protein sequence, localization, and association with breast cancer cell proliferation using antisense phosphorothioate oligonucleotides. Journal of Cellular Biochemistry, 79(2), 202–212.
Singh, R. R., & Kumar, R. (2007). MTA family of transcriptional metaregulators in mammary gland morphogenesis and breast cancer. Journal of Mammary Gland Biology and Neoplasia, 12(2–3), 115–125.
Pawson, T., & Schlessingert, J. (1993). SH2 and SH3 domains. Current Biology, 3(7), 434–442.
Bar-Sagi, D., Rotin, D., Batzer, A., Mandiyan, V., & Schlessinger, J. (1993). SH3 domains direct cellular localization of signaling molecules. Cell, 74(1), 83–91.
Weng, Z., Taylor, J. A., Turner, C. E., Brugge, J. S., & Seidel-Dugan, C. (1993). Detection of Src homology 3-binding proteins, including paxillin, in normal and v-Src-transformed Balb/c 3T3 cells. Journal of Biological Chemistry, 268(20), 14956–14963.
Toh, Y., Pencil, S. D., & Nicolson, G. L. (1994). A novel candidate metastasis-associated gene, mta1, differentially expressed in highly metastatic mammary adenocarcinoma cell lines. cDNA cloning, expression, and protein analyses. Journal of Biological Chemistry, 269(37), 22958–22963.
Kumar, R., Wang, R. A., Mazumdar, A., Talukder, A. H., Mandal, M., Yang, Z., et al. (2002). A naturally occurring MTA1 variant sequesters oestrogen receptor-alpha in the cytoplasm. Nature, 418(6898), 654–657.
Li, W., Ma, L., Zhao, J., Liu, X., Li, Z., & Zhang, Y. (2009). Expression profile of MTA1 in adult mouse tissues. Tissue and Cell, 41(6), 390–399.
Liu, J., Xu, D., Wang, H., Zhang, Y., Chang, Y., Zhang, J., et al. (2014). The subcellular distribution and function of MTA1 in cancer differentiation. Oncotarget, 5(13), 5153–5164.
Nagaraj S. R., Shilpa P., Rachaiah K., Salimath B.P. (2013). Crosstalk between VEGF and MTA1 signaling pathways contribute to aggressiveness of breast carcinoma. Molecular Carcinogenesis, 2013 Nov 22. doi: 10.1002/mc.22104
Neuveut, C., Wei, Y., & Buendia, M. A. (2010). Mechanisms of HBV-related hepatocarcinogenesis. Journal of Hepatology, 52(4), 594–604.
Murakami, S. (2001). Hepatitis B virus X protein: a multifunctional viral regulator. Journal of Gastroenterology, 36(10), 651–660.
Zhang, X., Zhang, H., & Ye, L. (2006). Effects of hepatitis B virus X protein on the development of liver cancer. Journal of Laboratory and Clinical Medicine, 147(2), 58–66.
Yun, C., Um, H. R., Jin, Y. H., Wang, J. H., Lee, M. O., Park, S., et al. (2002). NF-kappaB activation by hepatitis B virus X (HBx) protein shifts the cellular fate toward survival. Cancer Letters, 184(1), 97–104.
Chan, D. W., & Ng, I. O. (2006). Knock-down of hepatitis B virus X protein reduces the tumorigenicity of hepatocellular carcinoma cells. Journal of Pathology, 208(3), 372–380.
Yoo, Y. G., Na, T. Y., Seo, H. W., Seong, J. K., Park, C. K., Shin, Y. K., et al. (2008). Hepatitis B virus X protein induces the expression of MTA1 and HDAC1, which enhances hypoxia signaling in hepatocellular carcinoma cells. Oncogene, 27(24), 3405–3413.
Feitelson, M. A., & Lee, J. (2007). Hepatitis B virus integration, fragile sites, and hepatocarcinogenesis. Cancer Letters, 252(2), 157–170.
Liu, B., Wen, X., Huang, C., & Wei, Y. (2013). Unraveling the complexity of hepatitis B virus: from molecular understanding to therapeutic strategy in 50 years. International Journal of Biochemistry and Cell Biology, 45(9), 1987–1996.
Wang, F., Zhou, H., Yang, Y., Xia, X., Sun, Q., Luo, J., et al. (2012). Hepatitis B virus X protein promotes the growth of hepatocellular carcinoma by modulation of the Notch signaling pathway. Oncology Reports, 27(4), 1170–1176.
Lara-Pezzi, E., Roche, S., Andrisani, O. M., Sánchez-Madrid, F., & López-Cabrera, M. (2001). The hepatitis B virus HBx protein induces adherens junction disruption in a src-dependent manner. Oncogene, 20(26), 3323–3331.
Lara-Pezzi, E., Majano, P. L., Yáñez-Mó, M., Gómez-Gonzalo, M., Carretero, M., Moreno-Otero, R., et al. (2001). Effect of the hepatitis B virus HBx protein on integrin-mediated adhesion to and migration on extracellular matrix. Journal of Hepatology, 34(3), 409–415.
Lara-Pezzi, E., Gómez-Gaviro, M. V., Gálvez, B. G., Mira, E., Iñiguez, M. A., Fresno, M., et al. (2002). The hepatitis B virus X protein promotes tumor cell invasion by inducing membrane-type matrix metalloproteinase-1 and cyclooxygenase-2 expression. Journal of Clinical Investigation, 110(12), 1831–1838.
Chung, T. W., Lee, Y. C., & Kim, C. H. (2004). Hepatitis B viral HBx induces matrix metalloproteinase-9 gene expression through activation of ERK and PI-3K/AKT pathways: involvement of invasive potential. FASEB Journal, 18(10), 1123–1125.
Yu, F. L., Liu, H. J., Lee, J. W., Liao, M. H., & Shih, W. L. (2005). Hepatitis B virus X protein promotes cell migration by inducing matrix metalloproteinase-3. Journal of Hepatology, 42(4), 520–527.
Ou, D. P., Tao, Y. M., Chang, Z. G., Tang, F. Q., & Yang, L. Y. (2006). Hepatocellular carcinoma cells containing hepatitis B virus X protein have enhanced invasive potential conditionally. Digestive and Liver Disease, 38(4), 262–267.
Ou, D. P., Tao, Y. M., Tang, F. Q., & Yang, L. Y. (2007). The hepatitis B virus X protein promotes hepatocellular carcinoma metastasis by upregulation of matrix metalloproteinases. International Journal of Cancer, 120(6), 1208–1214.
Zhang, X., Liu, S., Hu, T., Liu, S., He, Y., & Sun, S. (2009). Up-regulated microRNA-143 transcribed by nuclear factor kappa B enhances hepatocarcinoma metastasis by repressing fibronectin expression. Hepatology, 50(2), 490–499.
Manavathi, B., Singh, K., & Kumar, R. (2007). MTA family of coregulators in nuclear receptor biology and pathology. Nuclear Receptor Signaling, 5, e010.
Bui-Nguyen, T. M., Pakala, S. B., Sirigiri, R. D., Xia, W., Hung, M. C., Sarin, S. K., et al. (2010). NF-kappaB signaling mediates the induction of MTA1 by hepatitis B virus transactivator protein HBx. Oncogene, 29(8), 1179–1189.
Jung, J. K., Park, S. H., & Jang, K. L. (2010). Hepatitis B virus X protein overcomes the growth-inhibitory potential of retinoic acid by downregulating retinoic acid receptor-beta2 expression via DNA methylation. Journal of General Virology, 91(Pt 2), 493–500.
Park, I. Y., Sohn, B. H., Yu, E., Suh, D. J., Chung, Y. H., Lee, J. H., et al. (2007). Aberrant epigenetic modifications in hepatocarcinogenesis induced by hepatitis B virus X protein. Gastroenterology, 132(4), 1476–1494.
Lee, M. H., Na, H., Na, T. Y., Shin, Y. K., Seong, J. K., & Lee, M. O. (2012). Epigenetic control of metastasis-associated protein 1 gene expression by hepatitis B virus X protein during hepatocarcinogenesis. Oncogenesis, 1, e25.
Reddy, S. D., Pakala, S. B., Ohshiro, K., Rayala, S. K., & Kumar, R. (2009). MicroRNA-661, a c/EBPalpha target, inhibits metastatic tumor antigen 1 and regulates its functions. Cancer Research, 69(14), 5639–5642.
Bui-Nguyen, T. M., Pakala, S. B., Sirigiri, D. R., Martin, E., Murad, F., & Kumar, R. (2010). Stimulation of inducible nitric oxide by hepatitis B virus transactivator protein HBx requires MTA1 coregulator. Journal of Biological Chemistry, 285(10), 6980–6986.
Aboobaker, A. A., Tomancak, P., Patel, N., Rubin, G. M., & Lai, E. C. (2005). Drosophila microRNAs exhibit diverse spatial expression patterns during embryonic development. Proceedings of the National Academy of Sciences of the United States of America, 102(50), 18017–18022.
Iorio, M. V., Ferracin, M., Liu, C. G., Veronese, A., Spizzo, R., Sabbioni, S., et al. (2005). MicroRNA gene expression deregulation in human breast cancer. Cancer Research, 65(16), 7065–7070.
Makeyev, E. V., & Maniatis, T. (2008). Multilevel regulation of gene expression by microRNAs. Science, 319(5871), 1789–1790.
Behm-Ansmant, I., Rehwinkel, J., & Izaurralde, E. (2006). MicroRNAs silence gene expression by repressing protein expression and/or by promoting mRNA decay. Cold Spring Harbor Symposia on Quantitative Biology, 71, 523–530.
Ma, L., Teruya-Feldstein, J., & Weinberg, R. A. (2007). Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature, 449(7163), 682–688.
Reddy, S. D., Ohshiro, K., Rayala, S. K., & Kumar, R. (2008). MicroRNA-7, a homeobox D10 target, inhibits p21-activated kinase 1 and regulates its functions. Cancer Research, 68(20), 8195–8200.
Kefas, B., Godlewski, J., Comeau, L., Li, Y., Abounader, R., Hawkinson, M., et al. (2008). microRNA-7 inhibits the epidermal growth factor receptor and the Akt pathway and is down-regulated in glioblastoma. Cancer Research, 68(10), 3566–3572.
Li, S., Tian, H., Yue, W., Li, L., Gao, C., Si, L., et al. (2013). Down-regulation of MTA1 protein leads to the inhibition of migration, invasion, and angiogenesis of non-small-cell lung cancer cell line. Acta Biochimica et Biophysica Sinica, 45(2), 115–122.
Mazure, N. M., Brahimi-Horn, M. C., Berta, M. A., Benizri, E., Bilton, R. L., Dayan, F., et al. (2004). HIF-1: master and commander of the hypoxic world. A pharmacological approach to its regulation by siRNAs. Biochemical Pharmacology, 68(6), 971–980.
Bruick, R. K., & McKnight, S. L. (2001). A conserved family of prolyl-4-hydroxylases that modify HIF. Science, 294(5545), 1337–1340.
Epstein, A. C., Gleadle, J. M., McNeill, L. A., Hewitson, K. S., O’Rourke, J., Mole, D. R., et al. (2001). C. elegans EGL-9 and mammalian homologs define a family of dioxygenases that regulate HIF by prolyl hydroxylation. Cell, 107(1), 43–54.
Semenza, G. L. (2003). Targeting HIF-1 for cancer therapy. Nature Reviews Cancer, 3(10), 721–732.
Jeong, J. W., Bae, M. K., Ahn, M. Y., Kim, S. H., Sohn, T. K., Bae, M. H., et al. (2002). Regulation and destabilization of HIF-1alpha by ARD1-mediated acetylation. Cell, 111(5), 709–720.
Côté, J., Quinn, J., Workman, J. L., & Peterson, C. L. (1994). Stimulation of GAL4 derivative binding to nucleosomal DNA by the yeast SWI/SNF complex. Science, 265(5168), 53–60.
Kwon, H., Imbalzano, A. N., Khavari, P. A., Kingston, R. E., & Green, M. R. (1994). Nucleosome disruption and enhancement of activator binding by a human SW1/SNF complex. Nature, 370(6489), 477–481.
Tsukiyama, T., & Wu, C. (1995). Purification and properties of an ATP-dependent nucleosome remodeling factor. Cell, 83(6), 1011–1020.
Cairns, B. R., Lorch, Y., Li, Y., Zhang, M., Lacomis, L., Erdjument-Bromage, H., et al. (1996). RSC, an essential, abundant chromatin-remodeling complex. Cell, 87(7), 1249–1260.
Wang, W., Chi, T., Xue, Y., Zhou, S., Kuo, A., & Crabtree, G. R. (1998). Architectural DNA binding by a high-mobility-group/kinesin-like subunit in mammalian SWI/SNF-related complexes. Proceedings of the National Academy of Sciences of the United States of America, 95(2), 492–498.
Varga-Weisz, P. D., Wilm, M., Bonte, E., Dumas, K., Mann, M., & Becker, P. B. (1997). Chromatin-remodelling factor CHRAC contains the ATPases ISWI and topoisomerase II. Nature, 388(6642), 598–602.
Xue, Y., Wong, J., Moreno, G. T., Young, M. K., Côté, J., & Wang, W. (1998). NURD, a novel complex with both ATP-dependent chromatin-remodeling and histone deacetylase activities. Molecular Cell, 2(6), 851–861.
Nair, S. S., Bommana, A., Bethony, J. M., Lyon, A. J., Ohshiro, K., Pakala, S. B., et al. (2011). The metastasis-associated protein-1 gene encodes a host permissive factor for schistosomiasis, a leading global cause of inflammation and cancer. Hepatology, 54(1), 285–295.
Ghanta, K. S., Pakala, S. B., Reddy, S. D., Li, D. Q., Nair, S. S., & Kumar, R. (2011). MTA1 coregulation of transglutaminase 2 expression and function during inflammatory response. Journal of Biological Chemistry, 286(9), 7132–7138.
Pakala, S. B., Bui-Nguyen, T. M., Reddy, S. D., Li, D. Q., Peng, S., Rayala, S. K., et al. (2010). Regulation of NF-kappaB circuitry by a component of the nucleosome remodeling and deacetylase complex controls inflammatory response homeostasis. Journal of Biological Chemistry, 285(31), 23590–23597.
Pakala, S. B., Reddy, S. D., Bui-Nguyen, T. M., Rangparia, S. S., Bommana, A., & Kumar, R. (2010). MTA1 coregulator regulates LPS response via MyD88-dependent signaling. Journal of Biological Chemistry, 285(43), 32787–32792.
Li, D. Q., Pakala, S. B., Reddy, S. D., Ohshiro, K., Peng, S. H., Lian, Y., et al. (2010). Revelation of p53-independent function of MTA1 in DNA damage response via modulation of the p21 WAF1-proliferating cell nuclear antigen pathway. Journal of Biological Chemistry, 285(13), 10044–10052.
Van Rechem, C., Boulay, G., Pinte, S., Stankovic-Valentin, N., Guérardel, C., & Leprince, D. (2010). Differential regulation of HIC1 target genes by CtBP and NuRD, via an acetylation/SUMOylation switch, in quiescent versus proliferating cells. Molecular and Cellular Biology, 30(16), 4045–4059.
Wales, M. M., Biel, M. A., el Deiry, W., Nelkin, B. D., Issa, J. P., Cavenee, W. K., et al. (1995). p53 activates expression of HIC-1, a new candidate tumour suppressor gene on 17p13.3. Nature Medicine, 1(6), 570–577.
El-Deiry, W. S., Tokino, T., Velculescu, V. E., Levy, D. B., Parsons, R., Trent, J. M., et al. (1993). WAF1, a potential mediator of p53 tumor suppression. Cell, 75(4), 817–825.
Vitari, A. C., Leong, K. G., Newton, K., Yee, C., O’Rourke, K., Liu, J., et al. (2011). COP1 is a tumour suppressor that causes degradation of ETS transcription factors. Nature, 474(7351), 403–406.
Migliorini, D., Bogaerts, S., Defever, D., Vyas, R., Denecker, G., Radaelli, E., et al. (2011). Cop1 constitutively regulates c-Jun protein stability and functions as a tumor suppressor in mice. Journal of Clinical Investigation, 121(4), 1329–1343.
Li, D. Q., Ohshiro, K., Reddy, S. D., Pakala, S. B., Lee, M. H., Zhang, Y., et al. (2009). E3 ubiquitin ligase COP1 regulates the stability and functions of MTA1. Proceedings of the National Academy of Sciences of the United States of America, 106(41), 17493–17498.
Luo, J., Su, F., Chen, D., Shiloh, A., & Gu, W. (2000). Deacetylation of p53 modulates its effect on cell growth and apoptosis. Nature, 408(6810), 377–381.
Ohshiro, K., Rayala, S. K., Wigerup, C., Pakala, S. B., Natha, R. S., Gururaj, A. E., et al. (2010). Acetylation-dependent oncogenic activity of metastasis-associated protein 1 co-regulator. EMBO Reports, 11(9), 691–697.
Denslow, S. A., & Wade, P. A. (2007). The human Mi-2/NuRD complex and gene regulation. Oncogene, 26(37), 5433–5438.
Mazumdar, A., Wang, R. A., Mishra, S. K., Adam, L., Bagheri-Yarmand, R., Mandal, M., et al. (2001). Transcriptional repression of oestrogen receptor by metastasis-associated protein 1 corepressor. Nature Cell Biology, 3(1), 30–37.
Hay, E. D. (1995). An overview of epithelio-mesenchymal transformation. Acta Anatomica, 154(1), 8–20.
Lamouille, S., Xu, J., & Derynck, R. (2014). Molecular mechanisms of epithelial-mesenchymal transition. Nature Reviews Molecular Cell Biology, 15(3), 178–196.
Medici, D., & Kalluri, R. (2012). Endothelial-mesenchymal transition and its contribution to the emergence of stem cell phenotype. Seminars in Cancer Biology, 22(5–6), 379–384.
van Meeteren, L. A., & ten Dijke, P. (2012). Regulation of endothelial cell plasticity by TGF-β. Cell and Tissue Research, 347(1), 177–186.
Zeisberg, E. M., Potenta, S., Xie, L., Zeisberg, M., & Kalluri, R. (2007). Discovery of endothelial to mesenchymal transition as a source for carcinoma-associated fibroblasts. Cancer Research, 67(21), 10123–10128.
Lee, S. W., Won, J. Y., Kim, W. J., Lee, J., Kim, K. H., Youn, S. W., et al. (2013). Snail as a potential target molecule in cardiac fibrosis: paracrine action of endothelial cells on fibroblasts through snail and CTGF axis. Molecular Therapy, 21(9), 1767–1777.
Medici, D., Shore, E. M., Lounev, V. Y., Kaplan, F. S., Kalluri, R., & Olsen, B. R. (2010). Conversion of vascular endothelial cells into multipotent stem-like cells. Nature Medicine, 16(12), 1400–1406.
Wong, L. L., Chang, C. F., Koay, E. S., & Zhang, D. (2009). Tyrosine phosphorylation of PP2A is regulated by HER-2 signalling and correlates with breast cancer progression. International Journal of Oncology, 34(5), 1291–1301.
Kim, R., Arihiro, K., Emi, M., Tanabe, K., & Osaki, A. (2006). Potential role of HER-2; in primary breast tumor with bone metastasis. Oncology Reports, 15(6), 1477–1484.
Jiang, W. G., Lloyds, D., Puntis, M. C., Nakamura, T., & Hallett, M. B. (1993). Regulation of spreading and growth of colon cancer cells by hepatocyte growth factor. Clinical and Experimental Metastasis, 11(3), 235–242.
Jiang, W., Hiscox, S., Matsumoto, K., & Nakamura, T. (1999). Hepatocyte growth factor/scatter factor, its molecular, cellular and clinical implications in cancer. Critical Reviews in Oncology/Hematology, 29(3), 209–248.
Stoker, M., & Perryman, M. (1985). An epithelial scatter factor released by embryo fibroblasts. Journal of Cell Science, 77, 209–223.
Savagner, P., Yamada, K. M., & Thiery, J. P. (1997). The zinc-finger protein slug causes desmosome dissociation, an initial and necessary step for growth factor-induced epithelial-mesenchymal transition. Journal of Cell Biology, 137(6), 1403–1419.
Grotegut, S., von Schweinitz, D., Christofori, G., & Lehembre, F. (2006). Hepatocyte growth factor induces cell scattering through MAPK/Egr-1-mediated upregulation of Snail. EMBO Journal, 25(15), 3534–3545.
Hiscox, S., & Jiang, W. G. (1999). Association of the HGF/SF receptor, c-met, with the cell-surface adhesion molecule, E-cadherin, and catenins in human tumor cells. Biochemical and Biophysical Research Communications, 261(2), 406–411.
Pakala, S. B., Singh, K., Reddy, S. D., Ohshiro, K., Li, D. Q., Mishra, L., et al. (2011). TGF-β1 signaling targets metastasis-associated protein 1, a new effector in epithelial cells. Oncogene, 30(19), 2230–2241.
Thiery, J. P. (2002). Epithelial-mesenchymal transitions in tumour progression. Nature Reviews Cancer, 2(6), 442–454.
Dannenmann, C., Shabani, N., Friese, K., Jeschke, U., Mylonas, I., & Brüning, A. (2008). The metastasis-associated gene MTA1 is upregulated in advanced ovarian cancer, represses ERbeta, and enhances expression of oncogenic cytokine GRO. Cancer Biology and Therapy, 7(9), 1460–1467.
Batlle, E., Sancho, E., Francí, C., Domínguez, D., Monfar, M., Baulida, J., et al. (2000). The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nature Cell Biology, 2(2), 84–89.
Polyak, K., & Weinberg, R. A. (2009). Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nature Reviews Cancer, 9(4), 265–273.
Moon, E. J., Jeong, C. H., Jeong, J. W., Kim, K. R., Yu, D. Y., Murakami, S., et al. (2004). Hepatitis B virus X protein induces angiogenesis by stabilizing hypoxia-inducible factor-1α. FASEB Journal, 18(2), 382–384.
Zhang, X. Y., DeSalle, L. M., Patel, J. H., Capobianco, A. J., Yu, D., Thomas-Tikhonenko, A., et al. (2005). Metastasis-associated protein I (MTA1) is an essential downstream effector of the c-MYC oncoprotein. Proceedings of the National Academy of Sciences of the United States of America, 102(39), 13968–13973.
Terradillos, O., Billet, O., Renard, C. A., Levy, R., Molina, T., Briand, P., et al. (1997). The hepatitis B virus X gene potentiates c-MYC induced liver oncogenesis in transgenic mice. Oncogene, 14(4), 395–404.
Ou, D. P., Tao, Y. M., Tang, F. Q., & Yang, L. Y. (2007). The hepatitis B virus X protein promotes hepatocellular carcinoma metastasis by upregulation of matrix metalloproteinases. International Journal of Cancer, 120(6), 1208–1214.
Zhang, Y., Ng, H. H., Erdjument-Bromage, H., Tempst, P., Bird, A., & Reinberg, D. (1999). Analysis of the NuRD subunits reveals a histone deacetylase core complex and a connection with DNA methylation. Genes and Development, 13(15), 1924–1935.
Park, N. H., Song, I. H., & Chung, Y. H. (2006). Chronic hepatitis B in hepatocarcinogenesis. Postgraduate Medical Journal, 82(970), 507–51.
Yamaguchi, R., Yano, H., Iemura, A., Ogasawara, S., Haramaki, M., & Kojiro, M. (1998). Expression of vascular endothelial growth factor in human hepatocellular carcinoma. Hepatology, 28(1), 68–77.
Pang, R., & Poon, R. T. (2006). Angiogenesis and antiangiogenic therapy in hepatocellular carcinoma. Cancer Letters, 242(2), 151–167.
Song, B. C., Chung, Y. H., Kim, J. A., Lee, H. C., Yoon, H. K., Sung, K. B., et al. (2001). Association between insulin-like growth factor-2 and metastases after transcatheter arterial chemoembolization in patients with hepatocellular carcinoma: a prospective study. Cancer, 91(12), 2386–2393.
Li, H., Sun, L., Xu, Y., Li, Z., Luo, W., Tang, Z., et al. (2013). Overexpression of MTA3 correlates with tumor progression in non-small cell lung cancer. Plos One, 8(6), 1–8.
Zhang, H., Stephens, L. C., & Kumar, R. (2006). Metastasis tumor antigen family proteins during breast cancer progression and metastasis in a reliable mouse model for human breast cancer. Clinical Cancer Research, 12(5), 1479–1486.
Dong, H., Guo, H., Xie, L., Wang, G., Zhong, X., Khoury, T., et al. (2013). The metastasis-associated gene MTA3, a component of the Mi-2/NuRD transcriptional repression complex, predicts prognosis of gastroesophageal junction adenocarcinoma. PloS One, 8(5), e62986.
Chu, H., Chen, X., Wang, H., Du, Y., Wang, Y., Zang, W., et al. (2014). MiR-495 regulates proliferation and migration in NSCLC by targeting MTA3. Tumour Biology, 35(4), 3487–3494.
Zhong, J. H., Ma, L., & Li, L. Q. (2014). Postoperative therapy options for hepatocellular carcinoma. Scandivian Journal of Gastroenterology, 49(6), 649–661.
Shin, J. W., & Chung, Y. H. (2013). Molecular targeted therapy for hepatocellular carcinoma: current and future. World Journal of Gastroenterology, 19(37), 6144–6155.
Ikeda, K., Saitoh, S., Suzuki, Y., Kobayashi, M., Tsubota, A., Fukuda, M., et al. (1998). Interferon decreases hepatocellular carcinogenesis in patients with cirrhosis caused by the hepatitis B virus: a pilot study. Cancer, 82(5), 827–835.
Yoshida, H., Shiratori, Y., Moriyama, M., Arakawa, Y., Ide, T., Sata, M., et al. (1999). Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group Inhibition of Hepatocarcinogenesis by Interferon Therapy. Annals of Internal Medicine, 131(3), 174–181.
Sun, H. C., Tang, Z. Y., Wang, L., Qin, L. X., Ma, Z. C., Ye, Q. H., et al. (2006). Postoperative interferon alpha treatment postponed recurrence and improved overall survival in patients after curative resection of HBV-related hepatocellular carcinoma: a randomized clinical trial. Journal of Cancer Research and Clinical Oncology, 132(7), 458–465.
Kudo, M. (2008). Impact of interferon therapy after curative treatment of hepatocellular carcinoma. Oncology, 75(suppl 1), 30–41.
Zeisberg, M., Yang, C., Martino, M., Duncan, M. B., Rieder, F., Tanjore, H., et al. (2007). Fibroblasts derive from hepatocytes in liver fibrosis via epithelial to mesenchymal transition. Journal of Biological Chemistry, 282(32), 23337–23347.
Kim, K. H., Lee, W. R., Kang, Y. N., Chang, Y. C., & Park, K. K. (2014). Inhibitory effect of nuclear factor-κB decoy oligodeoxynucleotide on liver fibrosis through regulation of the epithelial-mesenchymal transition. Human Gene Therapy, 25(8), 721–729.
Author information
Authors and Affiliations
Corresponding author
Additional information
Soo Hyung Ryu, Myoung Kuk Jang, and Woo Jean Kim contributed equally to the article.
Rights and permissions
About this article
Cite this article
Ryu, S.H., Jang, M.K., Kim, W.J. et al. Metastatic tumor antigen in hepatocellular carcinoma: golden roads toward personalized medicine. Cancer Metastasis Rev 33, 965–980 (2014). https://doi.org/10.1007/s10555-014-9522-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-014-9522-4