Abstract
Assessment of fetal ventricular function is mostly subjective, and currently, for the objective assessment left ventricular shortening fraction is obtained. However, this by itself is not very reliable. Hence, more tools that can provide an objective assessment are needed to increase the confidence of functional assessment. Speckle tracking imaging can provide one such tool. In this study we sought to establish the normative value of global longitudinal and circumferential strain for our fetal patients and for two major forms of congenital heart diseases, namely atrioventricular canal defects (AVC) and uncorrected dextro-transposition of the great arteries (dTGA) to act as a benchmark. The study was completed via a single center retrospective analysis on 72 fetal echocardiograms (26 normal, 15 dTGA, and 31 AVC). Tomtec Arena™ echocardiography analysis software was used for analysis. In normal fetuses, mean left ventricular (LV) global longitudinal strain (GLS) was − 22.6% (95% CI -24, -21.1) and mean right ventricular (RV) GLS was − 22.1% (95% CI -23.6, -20.6). In AVC patients LV GLS was-26.6% (95% CI -28,-25.3) and mean RV GLS was − 26.5% (95% CI -27.9,-25.2). In dTGA patients LV GLS was − 22.9% (95% CI of -24.8, -21) and RV GLS was − 21.3% (95% CI was − 23.4, -20.8). There was good intra-rater reliability though poor to fair inter-rater reliability. Notwithstanding its current limitations, strain imaging can provide useful information that can increase confidence of cardiac functional assessment in fetal patients. However, to be reliable across the board, further automation and standardization is required.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Assessment of fetal ventricular function is mostly subjective, and very few tools are available for objective evaluation. Currently, for the objective assessment, left ventricular shortening fraction is obtained. However, these methods are not reliable. Hence, more tools that can provide an objective assessment are needed to add to the confidence of functional assessment. Speckle tracking imaging can provide one such tool.
Methods
This was a retrospective, single-center study carried out at the University of Iowa. The study was approved by the University of Iowa Institutional Review Board. The requirement of obtaining informed consent was waived. All studies were performed between 2010 and 2021.
Study population
Inclusion criteria
Fetuses with a normal heart: Consecutive patients with no associated congenital heart disease and normal reported left and right ventricular systolic function with a 4-chamber cine loop recorded between the gestational ages of 20 and 34 weeks were included.
Fetuses with simple uncorrected dextro-transposition of great arteries (dTGA): Consecutive patients between 2010 and 2021 with a diagnosis of dTGA and studies obtained between 20 and 34 weeks containing a 4-chamber cine loop were included in the study. For patients with multiple studies, the last study available was used for measurements.
Fetuses with a simple balanced atrioventricular canal defect (AVC): Consecutive patients between 2010 and 2021 with a diagnosis of AVC and echo containing a 4-chamber cine loop were included in the study. For patients with multiple studies, the last study available was used for measurements.
All fetuses: All patients had to have an echocardiogram that had a 4-chamber cine loop with frame rate of at least 40 Hz or higher and clear visualization of all segments. For patients with multiple studies, the last study available was used for measurements.
Exclusion criteria
Fetuses with a normal heart: Patients with uninterpretable image quality or no 4-chamber cine loop available or gestational age below 20 weeks or above 34 weeks were excluded.
Fetuses with simple uncorrected dTGA: Patients with uninterpretable image quality or no 4-chamber cine loop available or gestational age below 20 weeks or above 34 weeks were excluded. Any patient with a diagnosis of atrial septal restriction or with complex lesions (such as a ventricular septal defect or left ventricular outflow tract obstruction) were excluded.
Fetuses with an AVC: Patients with uninterpretable image quality or no 4-chamber cine loop available or gestational age below 20 weeks or above 34 weeks were excluded. Any patient with a significant atrioventricular valve insufficiency, associated tetralogy of Fallot, other outflow anomalies, diagnosis of heterotaxy or unbalanced AVC were excluded.
All fetuses: Patients without a 4-chamber loop with frame rate of at least 40 Hz or with poor acoustic windows preventing visualization of all segments in 4 chamber view were excluded.
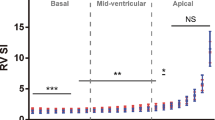
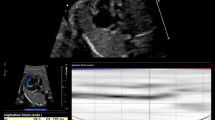
Strain analysis
Strain analysis was performed using Tomtec Arena™ echocardiography analysis software. The entire study was reviewed to confirm that it met inclusion criteria before transferring to the Tomtec software. End diastole was determined by visual inspection to identify the frame just before the atrioventricular valve closing, when the ventricular chamber appeared maximally dilated. This frame was assigned as the end diastolic frame. The R-R interval was defined between two consecutive end diastolic frames. The end systolic frame was assigned to the frame just before the atrioventricular valve opening when the chamber size appeared to be the smallest in the selected R-R interval. Contour points were assigned, and the strain analysis was performed semi automatically by the software. We did not prescribe a region of interest to assess. This was done with the purpose of minimizing the operator related variability in prescribing the region of interest. The right ventricle (RV) and left ventricle (LV) analysis were done separately selecting the appropriate frames to obtain the end-systolic global longitudinal strain (GLS) for RV and LV and end systolic global circumferential strain (GCS) for LV and recorded as percentages (%) (Figs. 1 and 2). Measurements were generated by the software from the 4 chamber images and reliable short axis images were not available consistently to measure GCS.
All the evaluations were performed by an imaging physician with experience of performing strain imaging. Ten normal studies were remeasured in a blinded fashion by the same physician for obtaining data for intra-rater reliability. Ten normal studies were then independently analyzed in a blinded fashion by a fellow physician who had been trained in strain imaging analysis for obtaining data for inter-rater reliability.
Statistical analysis
Continuous variables were presented as mean ± SD, while categorical variables were reported as percentages. Interquartile range was calculated for body mass index. The results for each group for GLS and GCS are presented as mean ± SD.
Type 3 Tests of Fixed Effects were performed to compare GLS among the three groups as well as to determine the effect of obesity. Pairwise comparison was done with Tukey adjusted p-values to compare between the three study groups both for RV and LV GLS and for combined (average) GLS. The effect of mother’s diabetes on GLS was examined by comparing mean GLS between those with and without diabetes. The three study groups were also compared excluding maternal diabetes. The effect of Trisomy 21 was also assessed. Finally, GCS was also compared between the groups.
Comparative evaluation within groups and between groups was performed using intraclass correlation coefficient and Bland-Altman plot to obtain intra-rater and inter-rater reliability.
Results
GLS
A total of 72 patients were analyzed that included 26 structurally and functionally normal hearts, 15 with dTGA and 26 with AVC. The group characteristics are highlighted in Table 1.
First, a mean ± SD was calculated for patients with normal hearts to establish a baseline for our lab. This was − 22.6% (95% CI -24, -21.1) for LV and − 22.1% (95% CI -23.6, -20.6) for RV. Thereafter, mean ± SD were calculated for the AVC and dTGA groups, and the three groups (Normal, dTGA and AVC) were compared. A significant difference was noticed in the mean GLS between the AVC group and the other two groups with fetuses in the AVC group having a significantly higher strain compared to both dTGA and normal patient for both LV and RV measurements (Table 2) (LV p = 0.003, 0.0001, RV p = 0.0001, < 0.0001). However, there was no statistically significant difference between the dTGA and normal group (Table 2) (LV p = 0.96, RV p = 0.8). The differences remained the same after adjusting for gestational age.
Next, the effect of maternal diabetes on GLS was examined by comparing mean GLS between those with (n = 7) and without diabetes (n = 19) in the normal patient group. Fetuses of diabetic mothers were found to have significantly higher strain values compared to fetuses of non-diabetic mothers (p = 0.009). Since diabetes was found to have a significant effect, GLS, groups were then compared, excluding fetuses of diabetic mothers to assess if the maternal diabetic status could have impacted the results. Differences between the groups still persisted after excluding maternal diabetes as a confounder in the results (Table 3).
The effect of maternal obesity on GLS was also examined and showed no significant impact. The average mean difference between obese and non-obese across the groups was 0.7 (95% CI: -0.7, 2.1, p = 0.297).
GCS
In contrast to GLS, the GCS in the AVC and dTGA patients was significantly higher than the normal group. The average strain in the AVC group was higher by 4.3% (95% CI: 7.9, 0.5; p = 0.021) compared to normal group while the average strain was higher by 5.2% (95% CI: 9.7, 0.6; p = 0.022) in the dTGA group compared to normal. No significant difference was seen between the AVC and dTGA (p = 0.87) groups, however (Table 4). Similar results were observed adjusting for effect of gestational age.
The effect of maternal diabetes was also evaluated in the normal group and unlike for GLS, no significant difference was identified between those with and without maternal diabetes (p = 0.31). The effect of maternal obesity on GCS was also examined and showed no significant impact either (p = 0.218).
Given that a significant proportion of AVC patients had Trisomy 21, the effect of Trisomy 21 on strain parameters in that group was assessed and showed no significant difference either in GLS (p = 0.77) or GCS (p = 0.47) between the patients with and without Trisomy 21.
Intra-rater and inter-rater reliability
Finally, the intra-rater and inter-rater reliability were assessed and showed a good intra-rater agreement with an intraclass correlation coefficient of 0.94 (CI of 0.80, 0.99) for RV GLS, 0.98 (CI of 0.92, 0.99) for LV GLS, and 0.99 (CI of 0.98, 0.99) for LV GCS (Fig. 3).
However, the inter-rater agreement was fair to poor with an intraclass correlation coefficient of 0.31 (CI of 0.00, 0.89) for RV GLS, 0.74 (CI of 0.12, 0.92) for LV GLS, and 0.27 (CI of 0.00, 0.72) for LV GCS (Fig. 4).
Discussion
The most commonly and widely used objective method to ascertain cardiac function is to assess for myocardial shortening via estimated shortening fraction on M-mode and ejection fraction on 2D imaging. Strain imaging is a newer tool to assess ventricular function that quantifies regional deformation based on the principles of mechanical engineering. Strain is defined as the deformation of an object, normalized to its original shape. It measures changes in length relative to its initial length and is a dimensionless quantity (expressed as percentage)The speed at which this strain occurs defines strain rate. A local heart coordinate system has been defined to assess the strain and strain rate and involves measuring deformation in longitudinal, circumferential and radial axes [1].
Strain Echocardiography (STE) has several important advantages compared to other modalities that measure deformation. In contrast to cardiovascular magnetic resonance, STE is widely available, cost efficient, can be used at the ‘bedside,’ and has a shorter procedural and post-processing time. In comparison to tissue doppler imaging, STE is relatively insonation angle independent and does not require such high frame rates, is not subjected to the tethering effect, and allows straightforward measurements of radial and circumferential strain in addition to longitudinal strain [2]. . While both strain and left ventricular ejection fraction (LVEF) measure LV function, there is a fundamental difference between the two: strain calculates the contractility of the myocardium, while LVEF is a surrogate parameter that describes myocardial pump function. Even if contractility is reduced, compensatory mechanisms (i.e., ventricular dilatation, geometry changes) can still assure that stroke volume remains normal (at least at rest). Thus, STE is especially suited for the assessment of global and regional systolic function in patients with heart failure with apparently normal ejection fraction. Additionally, exact calculation of LVEF requires good image quality, operator experience, and has a large error of measurement. LVEF is also much more load dependent than strain [2]. Hence, strain can be an important parameter for LV function which can display cardiac dysfunction at an earlier stage of disease [2].
The normative data for adult LV strain have been established [3, 4]. Reference values for RV strain in healthy adults have also been proposed [5]. Speckle tracking strain imaging has found its utility in identifying and following ventricular dysfunction. It has become a mainstay in evaluating and trending cardiac function in disease states such as pulmonary embolism, diabetes, and detection of cardiotoxicity after chemotherapy [6,7,8].
Strain imaging has also been found to be feasible and effective for the assessment of myocardial viability. The clinical availability of strain measurement may offer a solution to the ongoing need for quantification of regional and global cardiac function [9]. Strain and strain rate measurements are helpful in the selection of different therapies and follow-up evaluations of myocardial function after medical and surgical treatments [10]. It has also been used to prognosticate after acute myocardial infarction in adults [11]. With advancements in technology and ease of use, strain imaging has become an important tool in the assessment of cardiac health in adults.
Simultaneously, with its growing popularity in the pediatric and fetal populations, more data and insights are available to provide meaningful information that can impact patient care. Reference values for strain and strain rate in both systole and diastole in healthy children over a large age range have been proposed. Important contributions of heart rate dependence have also been described [12].
RV assessment forms an important aspect of evaluation in various heart diseases in the pediatric population. It is also one of the most difficult chambers to evaluate objectively, especially with echocardiograms. Researchers have tried to use strain to define the RV function both in health [5] and disease states and attempts have been made to assess feasibility in various conditions, for example in premature infants [13] and tetralogy of Fallot [14].
Along those lines, feasibility of performing global longitudinal cardiac strain and strain rate in fetal population were described by Barker as well as Crispi’s groups [15, 16]. Crispi’s group also noted the significant difference in the values of strain obtained using tissue doppler versus speckle tracking method.
Recently, there has been a significant interest to establish normative values for strain and describe changes with various disease states in pediatric and fetal population. An attempt to define global longitudinal reference ranges for fetal myocardial deformation in the second half of pregnancy was evaluated in a group of 120 pregnancies by Lee-Tannock’s group [17]. Maskatia and his coinvestigators have investigated the fetal strain and strain rate at various gestational ages and compared it to left ventricular and right ventricular myocardial performance indices. They hypothesized differences to be related to changes in preload and/or afterload on the fetal heart [18]. In another study, the same group found fetal measurements of diastolic strain rate to have acceptable reproducibility after 24 weeks’ gestation [19]. In another study by Kapusta et al., the investigators noted that the fetal left and right ventricular strain mechanics changed between the second and third trimester during normal pregnancy [20]. However, a recent systemic review of 23 studies by van Oostrum’s group highlighted a significant discrepancy between various studies in measuring speckle tracking, and hence, they could not perform a metanalysis [21, 22]. Their inability to perform the analysis highlights some of the major limitations of current knowledge.
Nevertheless, strain remains a promising parameter, which with further development can add to the tools available to pediatric and fetal cardiologists to assess cardiac function and to assist with medical decision making. This is especially important for fetal cardiac assessment given that there are limited options available to assess cardiac function in this population. Measuring ejection fraction and shortening fraction is error prone and fetal cardiovascular magnetic resonance is still in its nascent stage. Thus, strain can be an additional echocardiographic tool that can be used to increase confidence in assessment of fetal ventricular function, especially in disease states. In the future, it would be reasonable to form normative data tables for various common pathologies to serve as a benchmark against which a more diseased heart can be compared.
In this study we have defined the normal strain values for both RV and LV in our lab including global longitudinal and circumferential strains. We, then, looked at strain values for two common cardiac pathologies namely uncomplicated well-balanced AVC and simple dTGA with the goal of defining the normative parameters for these conditions against which more diseased hearts can be compared to.
In our study the GLS was found to be more robust in AVC patients compared to dTGA and normal, while the RV and LV global circumferential function was found to be more robust in AVC and dTGA patients compared to studies with normal hearts. These differences were interesting, and we do not know the reason why these differences exist but postulate that it could be related to the differences in the loading condition and hemodynamic milieu. This could also be a result of differences in maturity and growth of myocardium as well as its regulatory mechanisms. Additional studies will be required to investigate the underlying mechanisms. However, this data provides a good benchmark against which more complex diseases (for example AVC with significant atrioventricular valve regurgitation or dTGA patient with suspected atrial septal restriction) can be assessed and prognostic information derived.
We also looked at the effect of maternal diabetes, maternal obesity, and impact of Trisomy 21 as these have been known to or can potentially impact fetal cardiac function [22, 23]. These factors, however, were not found to impact or account for the differences in global longitudinal or circumferential strains.
In our study we found a good intra-rater reliability which is reassuring and suggests good reproducibility after a learning curve. However, we also noticed poor to fair inter-rater reliability. We postulate the likely reason for the poor inter-rater reliability to technical variations (for example in assignment of end diastolic and end systolic frames and assignment of contour points). This highlights the importance of learning curve and need for standardization across the labs and finally further automation using artificial intelligence.
Limitations
This study was performed as a single center retrospective study and suffers from the limitations associated with such studies. GCS
Measurements were generated by the software from the 4 chamber images and reliable short axis images were not available consistently to measure GCS and hence short axis images were not used to measure GCS for this study. Another limitation in implementation of our data to other labs is the Inter-Vendor discrepancy, which remains a challenge in Strain imaging. The study may have been underpowered due to small numbers of patients and the data will need to be confirmed through a larger study done in a prospective multi centered fashion.
Conclusions
Notwithstanding its current limitations, strain imaging can provide useful information that can increase confidence of cardiac functional assessment in fetal patients. Based on our data the mean LV GLS was -26.9% (CI 28.3, 25.6) while the mean RV GLS was -26.6% (CI 28.25.3) in AVC patients. In dTGA patients, the mean LV GLS was -22.9% (CI 24.8,20.9) and RV GLS was -21.3% (CI 23.3, 19.4). Meanwhile, the mean LV GCS was -31.7% (CI of 33.8. 29.6) in AVC patients and -32.6% (CI 35.6, 29.6) in dTGA patients. These parameters can provide a benchmark for assessment of dTGA and AVC patients. Further, GLS was found to be more robust in AVC patients compared to dTGA and normal patients while the RV and LV GCS was found to be more robust in AVC and dTGA patients compared to studies with normal heart. The reasons for these differences need to be further explored.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AVC:
-
atrioventricular canal defects
- dTGA:
-
uncorrected transposition of the great arteries
- LV:
-
left ventricle
- GLS:
-
global longitudinal strain
- RV:
-
right ventricle
- GCS:
-
global circumferential strain
- STE:
-
Strain Echocardiography
- LVEF:
-
Left ventricular ejection fraction
References
D’hooge J, Heimdal A, Jamal F et al (2000) Regional strain and strain rate measurements by Cardiac Ultrasound: principles, implementation and limitations. Eur J Echocardiography 1(3):154–170. https://doi.org/10.1053/euje.2000.0031
Blessberger H, Binder T (2010) Two dimensional speckle tracking echocardiography: basic principles. Heart 96(9):716. https://doi.org/10.1136/hrt.2007.141002
Kuznetsova T, Herbots L, Richart T et al (2008) Left ventricular strain and strain rate in a general population. Eur Heart J 29(16):2014–2023. https://doi.org/10.1093/eurheartj/ehn280
Dalen H, Thorstensen A, Aase SA et al (2009) Segmental and global longitudinal strain and strain rate based on echocardiography of 1266 healthy individuals: the HUNT study in Norway. Eur J Echocardiography 11(2):176–183. https://doi.org/10.1093/ejechocard/jep194
Fine NM, Chen L, Bastiansen PM et al (2015) Reference values for right ventricular strain in patients without Cardiopulmonary Disease: a prospective evaluation and Meta-analysis. Echocardiography 32(5):787–796. https://doi.org/10.1111/echo.12806
Kjaergaard J, Sogaard P, Hassager C (2004) Right ventricular strain in pulmonary embolism by Doppler tissue echocardiography. Journal of the American Society of Echocardiography. /11/01/ 2004;17(11):1210–1212. https://doi.org/10.1016/j.echo.2004.06.026
Ng ACT, Delgado V, Bertini M et al (2009) Findings from Left Ventricular Strain and Strain Rate Imaging in Asymptomatic Patients With Type 2 Diabetes Mellitus. The American Journal of Cardiology. /11/15/ 2009;104(10):1398–1401. https://doi.org/10.1016/j.amjcard.2009.06.063
Thavendiranathan P, Poulin F, Lim K-D et al Use of myocardial strain imaging by Echocardiography for the Early Detection of Cardiotoxicity in patients during and after Cancer Chemotherapy. J Am Coll Cardiol. 2014/07/01 2014;63(25_Part_A):2751–2768. https://doi.org/10.1016/j.jacc.2014.01.073
Marwick TH (2006) Measurement of strain and strain rate by Echocardiography. J Am Coll Cardiol 47(7):1313–1327. https://doi.org/10.1016/j.jacc.2005.11.063
Dandel M, Hetzer R (2009) Echocardiographic strain and strain rate imaging — Clinical applications. International Journal of Cardiology. /02/06/ 2009;132(1):11–24. https://doi.org/10.1016/j.ijcard.2008.06.091
Antoni ML, Mollema SA, Delgado V et al (2010) Prognostic importance of strain and strain rate after acute myocardial infarction. Eur Heart J 31(13):1640–1647. https://doi.org/10.1093/eurheartj/ehq105
Boettler P, Hartmann M, Watzl K et al (2005) Heart Rate Effects on Strain and Strain Rate in Healthy Children. Journal of the American Society of Echocardiography. /11/01/ 2005;18(11):1121–1130. https://doi.org/10.1016/j.echo.2005.08.014
Levy PT, Holland MR, Sekarski TJ et al (2013) Feasibility and Reproducibility of Systolic Right Ventricular Strain Measurement by Speckle-Tracking Echocardiography in Premature Infants. Journal of the American Society of Echocardiography. /10/01/ 2013;26(10):1201–1213. https://doi.org/10.1016/j.echo.2013.06.005
Toro KD, Soriano BD, Buddhe S (2016) Right ventricular global longitudinal strain in repaired tetralogy of Fallot. Echocardiography 33(10):1557–1562. https://doi.org/10.1111/echo.13302
Barker PCA, Houle H, Li JS et al (2009) Global longitudinal Cardiac strain and strain rate for Assessment of fetal cardiac function: Novel Experience with Velocity Vector Imaging. Echocardiography 26(1):28–36. https://doi.org/10.1111/j.1540-8175.2008.00761.x
Crispi F, Sepulveda-Swatson E, Cruz-Lemini M et al (2012) Feasibility and reproducibility of a standard protocol for 2D speckle Tracking and tissue doppler-based strain and strain rate analysis of the fetal heart. Fetal Diagn Ther 32(1–2):96–108. https://doi.org/10.1159/000337329
Lee-Tannock A, Hay K, Gooi A et al (2020) Global longitudinal reference ranges for fetal myocardial deformation in the second half of pregnancy. J Clin Ultrasound Sep 48(7):396–404. https://doi.org/10.1002/jcu.22826
Maskatia SA, Pignatelli RH, Ayres NA et al (2016) Longitudinal changes and Interobserver variability of systolic myocardial deformation values in a prospective cohort of healthy fetuses across Gestation and after delivery. J Am Soc Echocardiogr 29(4):341–349 2016/04/01/. https://doi.org/10.1016/j.echo.2015.12.003
Maskatia SA, Pignatelli RH, Ayres NA et al (2016) Fetal and Neonatal Diastolic Myocardial Strain Rate: Normal Reference Ranges and Reproducibility in a Prospective, Longitudinal Cohort of Pregnancies. Journal of the American Society of Echocardiography. /07/01/ 2016;29(7):663–669. https://doi.org/10.1016/j.echo.2016.02.017
Kapusta L, Mainzer G, Weiner Z et al (2013) Changes in Fetal Left and Right Ventricular Strain Mechanics during Normal Pregnancy. Journal of the American Society of Echocardiography. /10/01/ 2013;26(10):1193–1200. https://doi.org/10.1016/j.echo.2013.06.007
van Oostrum NHM, de Vet CM, van der Woude DAA et al (2020) Fetal strain and strain rate during pregnancy measured with speckle tracking echocardiography: a systematic review. Eur J Obstet Gynecol Reproductive Biology 2020/07/01:250:178–187. https://doi.org/10.1016/j.ejogrb.2020.04.002
Depla AL, De Wit L, Steenhuis TJ et al (2021) Effect of maternal diabetes on fetal heart function on echocardiography: systematic review and meta-analysis. Ultrasound Obstet Gynecol Apr 57(4):539–550. https://doi.org/10.1002/uog.22163
Bayoumy S, Habib M, Abdelmageed R (2020) Impact of maternal diabetes and obesity on fetal cardiac functions. Egypt Heart J Jul 31(1):46. https://doi.org/10.1186/s43044-020-00077-x
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
U.G. and K.Y. collected the data.U.G. Wrote the paperH.C. provided chart review and identified the patients for studyM.B.Z. performed statistical analysisB.R. provided input in study design and manuscript review and proof reading.
Corresponding author
Ethics declarations
Competing interests
I am on the editorial board of the Journal.
Disclosures
The authors have no conflict of interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Young, K., Hooton, C., Zimmerman, M.B. et al. Fetal left and right ventricular strain parameters using speckle tracking in congenital heart diseases. Int J Cardiovasc Imaging 40, 1235–1243 (2024). https://doi.org/10.1007/s10554-024-03094-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-024-03094-y