Abstract
Transient alterations in ventricular conduction and synchronized cardiac performance have been reported in experimental models of myocardial ischemia. In post-stress 99mTc-sestamibi-gated-SPECT myocardial perfusion imaging (MPI), the time elapsed between tracer injection and image acquisition could influence the detection of ischemic left ventricular mechanical dyssynchrony (LVMD). We aimed at evaluating whether early vs. delayed post-stress MPI improve ischemic LVMD detection using the phase analysis parameters standard deviation (SD) and histogram bandwidth (HB) and to assess the correlation between stress-induced changes in SD and HB and other functional parameters. We prospectively studied 32 control subjects (Group-1) and 60 ischemic patients (Group-2). Stress-induced changes were calculated as stress minus rest (Δ). LVMD was defined as post-stress increases of either SD or HB. Group-2 showed higher ΔSD and ΔHB in early than in delayed images: early ΔSD: 1.63 (− 0.37 to 4.83) vs. delayed ΔSD: − 0.39 (− 3.82 to 1.74); early ΔHB: 2.50 (− 4 to 12) vs. ΔHB delayed: − 4 (− 15.75 to 4), all p < 0.01. ΔSD and ΔHB correlated linearly with ΔLV-ejection-fraction (EF) and ΔLV-end systolic-volume (ESV) in early images, all p < 0.01. Early images detected LVMD in more patients than delayed scans (78% vs. 38%; p < 0.01) All patients with LVEF drop in early post-stress evaluation had LVMD. Early post-stress images improve ischemic LVMD detection. Ischemic LVEF and LVESV changes correlate with ΔSD and ΔHB.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Myocardial stunning is defined as the delayed recovery of regional myocardial contractile function after reperfusion despite restoration of normal flow and absence of irreversible damage [1]. A transient stunning phenomenon has been also found to occur after treadmill exercise or pharmacologic stress tests [2]. As has been shown in animal models of experimentally-induced ischemia, molecular changes both in Purkinje cells and myocytes transiently alter intraventricular conduction and thereby synchronized functional performance [3]. Left ventricular mechanical dyssynchrony (LVMD) could therefore be an early event that leads to ischemic abnormalities in regional wall motion and left ventricular ejection fraction (LVEF).
Left ventricular (LV) function, one of the most important prognostic variables, can be accurately measured with electrocardiogram-gated single photon emission computed tomography (ECG-gated SPECT) myocardial perfusion imaging (MPI), which provides incremental prognostic information regarding the extent of perfusion abnormalities [4,5,6].
Phase analysis obtained from ECG-gated SPECT MPI has been introduced as an automated method for the evaluation of LVMD with high reproducibility and retrospective evaluation ability [7,8,9].
Beyond predicting the response to resynchronization therapy [10, 11], LV synchrony evaluation has demonstrated additional prognostic information in patients with various comorbidities such as diabetes and terminal stage renal disease [12, 13]. Particularly, in ischemic patients different studies have described LVMD related to large amounts of jeopardized myocardium and to multiple vessel disease [14, 15]. Thus, LV synchrony evaluation could be an additional sensitive tool for acute stunning detection in this population.
Due to the transitory nature of stunning, the timing for post-stress image acquisition may be crucial for the detection of transient ischemic changes in mechanical synchrony [16, 17].
The main objective of this prospective study was to evaluate whether early vs. delayed post-stress images of 99Tc sestamibi ECG-gated SPECT MPI, improve the detection of LVMD produced by myocardial ischemia, compared to control subjects.
An additional objective was to assess the correlation between stress-induced changes in standard deviation (SD) or histogram bandwidth (HB) and other functional parameters.
Materials and methods
Patient selection
This study complies with the Declaration of Helsinki of 1964 and all subsequent revisions and was approved by the Ethics Committee of the Favaloro Foundation University Hospital. Written informed consent was signed by all the patients.
Between March 2018 and March 2020, we prospectively studied 92 consecutive patients referred to our hospital for MPI 99mTc-sestamibi ECG-gated SPECT. We divided them into two groups.
Group-1 (control patients) included patients with (1) low likelihood for coronary artery disease: no typical/atypical angina, no history of myocardial infarction or known coronary artery disease and no diabetes mellitus, peripheral or cerebral vascular disease; (2) normal baseline electrocardiogram and normal exercise or pharmacological stress test (asymptomatic and without pathological ST-segment changes and adequate hemodynamic response to the test), and (3) normal gated perfusion imaging.
Group-2 (ischemic patients) included patients with (1) a positive exercise or pharmacological stress test (typical angina or dyspnea and/or exercise ST-segment depression > 2 mm from baseline or ST elevation > 1 mm in leads in absence of Q waves, and/or drop in systolic blood pressure higher than 10 mmHg from baseline despite an increase in workload, when accompanied by other evidence of ischemia in exercise stress test), and (2) presence of reversible perfusion defects.
Patients with left bundle branch block, history of pacemaker implantation or atrial fibrillation and left ventricular ejection fraction (LVEF) ≤ 35% were excluded from this study.
The demographics, comorbidities, and medications were recorded.
Stress test protocol
Exercise stress modalities included treadmill or bicycle and were carried out according to standardized protocols (Bruce or modified Bruce protocol and Astrand or modified Astrand protocol, respectively).
Pharmacologic stress modalities included: (1) Dipyridamole: After avoiding consumption of any products containing methylxanthines and theophylline for at least 24 h prior to the testing. Dipyridamole was administered at 0.56 mg/kg intravenously over a 4-min period; (2) Dobutamine was infused incrementally starting at a dose of 5 mcg/kg/min, which was increased at 3-min intervals to 10, 20, 30 and 40 mcg/kg/min [18].
SPECT imaging protocol
Patients underwent a 1-day protocol with injections of 300–370 MBq (8–10 mCi) and 740–925 MBq (20–25 mCi) of 99mTc-sestamibi for the low and high dose image, respectively. Patients with body weight > 100 kg, known LV dilation, breast prosthesis or breast perimeter > 100 cm underwent a 2-day protocol with injections of 555 MBq (15 mCi) of 99mTc-sestamibi each day. Prone and/or supine positions were used to avoid breast and diaphragm attenuation artifacts.
Images were obtained with a step and shoot protocol, 180° elliptical orbit with 60 projections. A dual-head detector gamma camera (General Electric Ventri or Discovery NM630) with high resolution, low energy collimator was used. A 15% window was centered on the 140 keV gamma peak and another at 120 keV for scatter correction. A 64 × 64 matrix was used and the gating was done with 8 frames per R-R cycle.
ECG-gated SPECT MPI was obtained at early stress, delayed stress and rest with 99mTc-sestamibi according to ASNC guidelines as previously described [19]. Early stress images were started latest 15 min after tracer injection. Delayed stress images and rest images were started 1 h after tracer injection. All images were reviewed for quality control measures. The overall quality of each study was classified as excellent, good, poor or uninterpretable [20].
Processing of SPECT images
All studies were processed with commercially available Myovation Evolution software (GE Medical Systems, Waukesha, WI, USA) on GE Xeleris nuclear medicine workstation. Non-attenuation correction SPECT emission images were processed. Filtered OSEM with 12 iterations and 10 subsets was used. Motion correction procedure was applied if necessary. After proper alignment, tomography slices (short-axis, vertical and horizontal long-axis) were generated.
Image analysis
Reconstructed SPECT images were reported by nuclear cardiologists using Emory Cardiac Toolbox (ECTbox; Emory University, Atlanta, GA, USA) software.
The American Heart Association 17-segment model was applied for semi-quantitative visual assessment of MPI. Each segment was scored by consensus of two independent expert physicians: normal uptake (score 0); mildly reduced uptake (score 1) moderately reduced uptake (score 2); severely reduced uptake (score 3); and absent uptake (score 4). Semi-quantitative visual scores: summed stress score (SSS), summed rest score, and summed difference score (SDS) were calculated for early and delayed stress and rest images. An SSS = 0 was interpreted as normal perfusion. The ischemic load was defined as mild (SDS: 1–3) moderate (SDS: 4–7) and severe (SDS > 7).
ECG-gated image analysis: left ventricular function and mechanical dyssynchrony
Each study was assessed for gating quality control. Base, apex, radius and center parameters were manually corrected when necessary. Manual check and minor adjustments for misalignment of parameters were done in all cases. In order to avoid errors in imaging processing, we previously developed a training program for high interobserver reproducibility assurance.
LV end diastolic volume, LV end systolic volume (LVESV), transient ischemic dilation ratio and LV ejection fraction (LVEF) were measured from the early and delayed stress and rest ECG-gated images using the software implemented in the ECTbox.
Normal ECG-gated MPI was defined as rest LVEF ≥ 55% and rest LVESV ≤ 70 ml.
The ECTbox was also used for phase analysis to assess LVMD at early stress, delayed stress and rest ECG-gated images [7]. Phase analysis parameters SD and HB were measured from each image in both groups.
Stress-induced changes of SD and HB (ΔSD and ΔHB) were calculated as stress minus rest [21, 22].
Post-stress worsening of phase analysis parameters or LVMD was defined as post-stress increase in either SD or HB [23].
An abnormal post-stress response of LVEF was defined as a ≥ 5% drop with respect to rest, as has been previously reported to indicate post-stress myocardial stunning [16, 23].
Follow-up
A short-term follow-up (3 months) was conducted by reviewing the medical history record or by telephone, in order to know the medical therapy prescribed and the coronary anatomy when assessed.
Statistical analysis
Marrugat’s formula was used to calculate the sample size needed to determine differences in the proportions of LVMD between group-1 and group-2 [24]. Considering the following parameters: (1) 95% 2-tailed confidence level, (2) 80% power, and (3) estimated prevalence of LVMD 0% in group-1 and 40% in group-2, this being the average of 20% in mild ischemic patients and 60% in severe ischemic patients, as previously reported [21], the minimum sample size was 15 patients per group. To determine differences in the proportions of LVMD according to ischemia degree within group-2, the minimum sample size yielded by Marrugat’s formula was 12 patients in each group.
Categorical variables were compared using Pearson Chi-square test or Fisher’s exact test as appropriate and are expressed as number and percentage. Shapiro–Wilk test was applied to check variable normalcy. Continuous data were compared using Student’s t test, Wilcoxon rank sum test or Kruskal–Wallis One-way ANOVA as appropriate, and are expressed as mean ± standard deviation (SD) or median and interquartile range (Q1st–Q3rd) for nonparametric variables. Pearson’s correlation was used to measure the degree of relationship between linearly related variables. All p-values are two-tailed, Values of p < 0.05 indicate statistical significant differences. Statistical analyses were performed using Statistix 7 version 7.1 (Analytical Software, Tallahassee, FL, USA).
Results
Patient characteristics, stress test and LV perfusion results
Group-1 included 32 control subjects and group-2, 60 ischemic patients (18 mild, 19 moderate and 23 severe ischemia). Detailed patient characteristics, stress test and LV perfusion results of both groups are shown in Table 1.
Image quality
MPI quality was graded as excellent in 93.3% of patients for early post-stress and 100% for delayed post-stress, and good in 6.6% and 0%, respectively. For rest studies, image quality was excellent in 93.3% and good in 6.6% of patients. Gated quality control was graded as excellent in all images (Fig. 1).
LV functions and phase analysis results
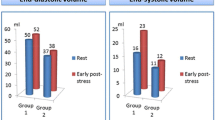
Table 2 shows stress (early and delayed) and rest LV function and phase analysis results in both groups. Early and delayed post-stress phase analysis parameters SD and HB were significantly increased in ischemic patients. Rest images showed no difference in SD and HB in both groups. A representative example of group-1 and group-2 images is shown in Fig. 1.
Inter-group comparisons of early and delayed stress phase analysis parameters
Comparison of early stress, delayed stress and rest phase analysis parameters SD and HB between both groups is shown in Fig. 2.
Left ventricular synchronism behavior in early stress, delayed stress and rest in normal subjects (Group-1) and ischemic patients (Group-2). Both early and delayed standard deviation (SD) and histogram bandwidth (HB) were significantly decreased related to rest in group-1. In contrast, although early SD and HB were increased related to rest images in group-2, no statistical significance was observed. Wilcoxon rank sum tests were applied. p < 0.05 was considered significant. Central box, interquartile range (Q1st–Q3rd); line within box, median. The whiskers extend to the most extreme values within 1.5 IQR. More extreme values are plotted individually
In control subjects, both early and delayed post-stress SD and HB were significantly lower than at rest (all p < 0.01). In group-2, early SD and HB were significantly higher than at delayed post-stress (all p < 0.05), while no change was observed in early SD and HB as compared to rest.
Early and delayed stress-induced changes in synchrony parameters (ΔSD and ΔHB)
In ischemic patients ΔSD and ΔHB were: Early ΔSD: 1.63 (− 0.37 to 4.83) vs. delayed ΔSD: − 0.39 (− 3.82 to 1.74); early ΔHB: 2.50 (− 4 to 12) vs. ΔHB delayed: − 4 (− 15.75 to 4), all p < 0.01.
Early images detected higher ΔSD and ΔHB than delayed ones in all subgroups of ischemic patients (mild, moderate and severe ischemia) as compared to control subjects (Fig. 3).
Early and delayed stress-induced changes in a SD and b HB in group-1; and in different subgroups in ischemic patients according to the amount of ischemia (mild SDS: 1–3; moderate SDS: 4–7 and severe SDS > 7). Early images detect higher ΔSD and ΔHB in ischemic patients in the three subgroups. Δ stress minus rest; SD standard deviation. HB histogram bandwidth; SDS summed difference score. Kruskal Wallis tests were applied. p < 0.05 was considered significant. Central box, interquartile range (Q1st–Q3rd); line within box, median. The whiskers extend to the most extreme values within 1.5 IQR. More extreme values are plotted individually
Early vs. delayed ΔSD and ΔHB according to the amount of myocardial ischemia were: mild ischemia: ΔSD 0.19 (− 0.59 to 3.21) vs. − 0.10 (− 2.69 to 1.42); and ΔHB 2 (− 5 to 9) vs. 0 (− 13 to 3), all p NS; moderate ischemia: ΔSD 2.12 (− 0.28 to 9.56) vs. − 2.60 (− 4.67 to 3.13) and ΔHB 0.5 (− 6 to 15) vs. − 12.5 (− 21.7 to 11) all p < 0.05; and severe ischemia: ΔSD 2.40 (− 0.21 to 5.85) vs. − 0.22 (− 3.48 to 0.99); ΔHB 4 (0–13) vs. − 4 (− 16 to 4), all p < 0.05.
Early and delayed stress-induced changes in SD and HB: correlation between perfusion and functional parameters in ischemic group
Table 3 shows the correlation of early and delayed-stress induced-changes in phase analysis SD and HB with LVEF, LVESV, SDS and transient ischemic dilation ratio (TID).
Significant linear correlation was observed between ΔSD and ΔHB vs. ΔLVEF (inverse) and ΔLVESV (direct) in early images (all p < 0.01) as well as ΔSD and ΔHB vs. ΔLVEF; and ΔSD vs. ΔLVESV in delayed images (all p < 0.05). No significant correlation was found between the stress-induced changes and SDS or TID.
Post-stress worsening of phase analysis indices (LVMD) according to amount of ischemia and to post-stress LVEF response
Forty-seven (78%) patients of group-2 showed LVMD in early stress images vs. 23 (38.3%) patients in delayed stress scans (p < 0.01). No differences were found in LVMD regarding sex, men vs. women: 41 (80.4%) vs. 7 (71.8%), respectively, in early stress images and 20 (39.2%) vs. 3 (33.3%) in delayed ones (both p = NS).
The prevalence of LVMD in early vs. delayed post stress images according to the amount of ischemia was: 83.3% (early) vs. 42% (delayed) in mild ischemia; 72% (early) vs. 39% (delayed) in moderate ischemia; and 82.6% (early) vs.35% (delayed) in severe ischemia, all p < 0.05.
An abnormal response of LVEF was more frequently observed in early post-stress images, 37% of patients (22 out of 60) vs 25% (15 out of 60) in delayed post-stress scans (p NS). Early images showed more LVMD than delayed ones in patients with and without LVEF drop (all p < 0.01). All patients with LVEF drop in early post-stress evaluation had LVMD. Sixty-eight percent of patients (25 out of 38) without LVEF drop had LVMD in early images vs. 35.5% (16 out of 45) in delayed ones, p < 0.01 (Fig. 4b).
Patients with left ventricular mechanical dyssynchrony (LVMD) according to a the extent of coronary artery disease in patients who underwent coronary angiography in the follow up, and to b abnormal response of left ventricular ejection fraction (LVEF) in early and delayed post-stress images. Early post-stress images detect more patients with LVMD than delayed scans regardless of extent of coronary artery disease and LVEF response. p < 0.05 was considered significant
Follow-up
No patient in group-1 underwent coronary artery angiography over the 3-months follow-up period.
Forty-three patients of group-2 (72%) underwent coronary angiography in a median of 23 days (10–52) post MPI. Four patients had angiographically normal coronary arteries and in 39 patients obstructive coronary artery disease was documented (8 patients had single-vessel and 31 had two or three-vessel coronary artery disease). Nineteen were referred to percutaneous transluminal coronary angioplasty, 11 to coronary artery bypass grafting and the rest to adjustments of their medical treatment.
Post-stress worsening of phase analysis indices (LVMD) according to the extent of coronary artery disease
In the 39 patients who had angiographically documented coronary artery disease we analyzed the relationship between LVMD and the extent of coronary artery disease.
Early images detected more LVMD than delayed ones (82% vs.33%), p < 0.01. This was observed in patients with single-vessel disease (75% vs. 0%) and in patients with multiple-vessel disease (83% vs. 42%); all p < 0.01 (Fig. 4a). Of 15 patients with LVMD and no LVEF drop in early images, 13 (87%) had multiple-vessel-disease.
Discussion
To the best of our knowledge, this is the first prospective pilot study evaluating the role of early versus delayed post-stress 99mTc-sestamibi ECG-gated SPECT MPI for the detection of LVMD as a marker of myocardial stunning in ischemic patients. Our results show that early post-stress images allow detecting the impairment of LV synchrony parameters more efficiently than delayed post-stress images without detriment of image quality. Early images detected significantly more stress-induced changes than delayed scans in patients exhibiting moderate and severe ischemia, but not mild ischemia.
Gated MPI can assess myocardial perfusion and LV function in a single study. Conventional MPI protocols using 99mTc tracers are acquired 45–60 min post-stress to avoid liver or gut uptake. Perfusion defects in SPECT MPI reflect the time of radiotracer injection during physical or pharmacological stress; unlike functional transient alterations (LV wall motion abnormalities, LVEF drop and LVMD) which are obtained at the moment when the triggered images are acquired. Therefore, these functional stress-induced changes can be better detected in an early post-stress acquisition.
Our results agree with those of previous retrospective MPI studies using 201Thallium early image acquisition. Singh et al. described LV synchrony parameters worsening in patients with perfusion abnormalities, but these were not related to the type of perfusion abnormality (ischemia, infarct and mixed group) [22].
On the other hand, using early images with 99mTc-sestamibi, as in our case, Peix et al. studied 101 patients (58 ischemic patients; 28 with normal scan and 15 with scar but no ischemia), and reported no difference in SD values between rest and post-stress in ischemic vs. normal groups but higher HB at rest in ischemic patients than in the normal group. They showed this difference to become even larger following stress. However, the selection criteria for the normal groups as well as the clinical features of ischemic patients differed with respect to our study [25]. In agreement with our results, Camilletti et al. found a significant increase of SD and HB in 39 ischemic patients as compared to rest [26].
Using gated positron emission tomography perfusion imaging, Al Jaroudi et al. also reported an association between LVMD and increased ischemic load. However, whereas Al Jaroudi’s patients had ischemic cardiomyopathy with LVEF ≤ 35%, our ischemic population had LVEF > 35% [27].
LVMD related to the ischemic amount was also studied by Peix et al. who observed that when the extension of ischemia and necrosis/fibrosis are considerable (based on the SSS values) post-stress SD and HB significantly increase and are even higher in women with SSS ≥ 4 [14]. It should be noticed that in this study the patients did not have obstructive coronary artery disease.
Importantly, we correlated stress-induced changes in SD and HB with functional parameters that define myocardial stunning. We found a significant linear correlation between stress-induced changes in SD and HB with ΔLVEF and ΔLVESV (inverse and direct, respectively), more evident in early post-stress images than in delayed evaluation. No correlation was found with SDS. This could be explained by balanced ischemia; multiple vessel disease may have normal or low SDS, underestimating the degree of anatomical coronary involvement. In this setting, the non-perfusion variables [28,29,30] like LVMD could add essential information for an accurate interpretation.
In contrast with our results, Chen et al. described a moderate but significant correlation of stress-induced changes in SD and HB with SDS but not with ΔLVEF in 75 patients with ischemia and myocardial necrosis referred for dipyridamole stress/rest 201Thallium ECG-gated SPECT MPI. In the subset of 25 ischemic patients, stress-induced changes in SD and HB did not correlate with either SDS or ΔLVEF [21].
This discrepancy could be explained by different inclusion criteria in ischemic patients groups. Our ischemic patients had stress tests highly suggestive of ischemia plus presence of reversible perfusion defect, while their inclusion criteria was defined by reversible perfusion defects. This could be the cause of a selection bias of patients with balanced ischemia in our population.
To note, the prevalence of LVMD, defined as post-stress increase of either SD or HB like in previous reports [22] was similar among patients with mild, moderate or severe ischemia, and was even higher than that we estimated when designing the study.
In the follow up, 90% of ischemic patients who underwent coronary angiography had obstructive coronary artery disease and 79% of them had multiple-vessel disease. In our cohort of patients with two- and three-vessel disease, LVMD was observed in both early and delayed post-stress images. These results agree with Hida et al. who showed that the addition of exercise-induced LVMD assessment on conventional perfusion analysis allowed better identification of patients with multivessel coronary artery disease [15].
Our study also detected post-stress LVMD in patients with one vessel-disease, and this occurred only in early post-stress evaluation.
Even though myocardial stunning is traditionally expressed as an abnormal post-stress LVEF response [16, 23], ischemic LVMD could be an early step in the cascade of ischemic events, previous to a drop in LVEF.
In summary, our results show that in ischemic patients early post-stress images detect more patients with LVMD than delayed images regardless of post-stress LVEF drop. Furthermore, all patients with post-stress abnormal LVEF response at early evaluation had LVMD. It is worth noting the high prevalence of multiple vessel disease among patients without post-stress LVEF drop but with LVMD in early images. Therefore, LV synchrony evaluation allowed us to recognize multiple-vessel disease patients even in absence of post-stress LVEF abnormal response.
This reinforces the proposed hypothesis of a “myocardial stunning cascade” where post-stress LVMD is an early step in a series of events that culminate with LVEF drop. Thus, LV systolic synchrony evaluation in early post-stress images could be a more sensitive tool for myocardial stunning detection. This parameter, along with other variables of 99mTc-sestamibi ECG-gated SPECT MPI would help improve the stratification of coronary artery disease. Prospective trials on larger patient populations are needed to support this assertion.
We are aware of limitations in this study. First, group-2 included only patients with stress tests highly suggestive of ischemic heart disease and presence of reversible perfusion defects. This strict inclusion criterion resulted in a high rate of multivessel disease, in detriment of other patient subsets in which the results of this study are not necessarily valid. And second, coronary anatomy assessment was not a condition of the present research. This was performed only in patients whose referral physician prescribed it.
Conclusion
Early post-stress 99mTc-sestamibi ECG-gated SPECT MPI improves ischemic LVMD detection compared with delayed evaluation.
Stress-induced dyssynchrony assessed by phase analysis correlates with other functional parameters as a previous step in the “myocardial stunning cascade” and provides additional non-perfusion diagnostic information of coronary artery disease. We propose early post-stress dyssynchrony assessment as a more sensitive tool for detecting myocardial stunning in coronary artery disease. Further investigation on larger patient populations is required.
Data availability
Not applicable.
Code availability
Not applicable.
References
Braunwald E, Kloner RA (1982) The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 66(6):1146–1149. https://doi.org/10.1161/01.cir.66.6.1146
Heiba SI, Santiago J, Mirzaitehrane M, Jana S, Dede F, Abdel-Dayem HM (2002) Transient postischemic stunning evaluation by stress gated Tl-201 SPECT myocardial imaging: effect on systolic left ventricular function. J Nucl Cardiol 9(5):482–490. https://doi.org/10.1067/mnc.2002.123855
Beardslee MA, Lerner DL, Tadros PN, Laing JG, Beyer EC, Yamada KA et al (2000) Dephosphorylation and intracellular redistribution of ventricular connexin43 during electrical uncoupling induced by ischemia. Circ Res 87:656–662. https://doi.org/10.1161/01.res.87.8.656
Sharir T, Germano G, Kavanagh PB, Lai S, Cohen I, Lewin HC et al (1999) Incremental prognostic value of post-stress left ventricular ejection fraction and volume by gated myocardial perfusion single photon emission computed tomography. Circulation 100(10):1035–1042. https://doi.org/10.1161/01.cir.100.10.1035
Carvalho PA, Aguiar PM, Grossman GB, Moraes JF, Baptista IS, Hirakata VN, Ludwig RTF, Ludwig EB (2012) Prognostic implications of the difference between left ventricular ejection fractions after stress and at rest in addition to the quantification of myocardial perfusion abnormalities obtained with gated SPECT. Clin Nucl Med 37(8):748–754. https://doi.org/10.1097/RLU.0b013e31825ae755
Bestetti A, Cuko B, Decarli A, Galli A, Lombardi F (2019) Additional value of systolic wall thickening in myocardial stunning evaluated by stress-rest gated perfusion SPECT. J Nucl Cardiol 26:833–840. https://doi.org/10.1007/s12350-017-1115-5
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL et al (2005) Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 12:687–695. https://doi.org/10.1016/j.nuclcard.2005.06.088
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX et al (2008) Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 4:374–378. https://doi.org/10.1097/MNM.0b013e3282f81380
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P et al (2010) Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol 5:811–816. https://doi.org/10.1007/s12350-010-9238-y
Peix A, Karthikeyan G, Massardo T, Kalaivani M, Patel C, Pabon LM et al (2019) Value of intraventricular dyssynchrony assessment by gated-SPECT myocardial perfusion imaging in the management of heart failure patients undergoing cardiac resynchronization therapy (VISION-CRT). J Nucl Cardiol. https://doi.org/10.1007/s12350-018-01589-5
Song ZZ (2008) Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT preferably predict response to CRT? J Nucl Med 49(4):686. https://doi.org/10.2967/jnumed.107.049601
Malik D, Mittal BR, Sood A, Parmar M, Kaur K, Bahl A (2018) Prognostic value of left ventricular mechanical dyssynchrony indices in long-standing type II diabetes mellitus with normal perfusion and left ventricular systolic functions on SPECT-MPI. J Nucl Cardiol. https://doi.org/10.1007/s12350-018-1436-z
Caobelli F, Popescu CE, Laudicella R, Comis A, Pignata SA, Saea R et al (2018) Predictive and prognostic value of left ventricular mechanical dyssynchrony assessed by myocardial perfusion single photon emission computed tomography in asymptomatic patients under hemodialysis. Nucl Med Commun 39(5):423–429. https://doi.org/10.1097/MNM.0000000000000816
Peix A, Padrón K, Cabrera LO, Pardo L, Sánchez J (2019) Left ventricular mechanical dyssynchrony in patients with chest pain and normal epicardial coronary arteries. J Nucl Cardiol. https://doi.org/10.1007/s12350-019-01804-x
Hida S, Chikamori T, Tanaka H, Igarashi Y, Shiba C, Usui Y et al (2012) Diagnostic value of left ventricular dyssynchrony after exercise and at rest in the detection of multivessel coronary artery disease on single-photon emission computed tomography. Circ J 76:1942–1952. https://doi.org/10.1253/circj.cj-11-1392
Mut F, Giubbini R, Vitola J, Lusa L, Sobic-Saranovic D, Peix A et al (2014) Detection of post-exercise stunning by early gated SPECT myocardial perfusion imaging: results from the IAEA multi-center study. J Nucl Cardiol 21:1168–1176. https://doi.org/10.1007/s12350-014-9983-4
Sobic-Saranovic DP, Bojic L, Petrasinovic Z, Grozdic-Milojevic IT, Pavlovic S, Artiko V, Jaksic E, Obradovic V, Dondi M (2013) Diagnostic and prognostic value of gated SPECT MIBI early post-stress imaging in patients with intermediate Duke Treadmill Score. Clin Nucl Med 38(10):784–789. https://doi.org/10.1097/RLU.0b013e31829f8e5a
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ (2016) ASNC imaging guidelines for SPECT nuclear cardiology procedures: stress, protocols and tracers. J Nucl Cardiol 23(3):606–639. https://doi.org/10.1007/s12350-015-0387-x
Dorbala S, Ananthasubramaniam K, Armstrong IS et al (2018) Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol 25:1784–1846. https://doi.org/10.1007/s12350-018-1283-y
Tilkemeier PL, Bourque J, Doukky R et al (2017) ASNC imaging guidelines for nuclear cardiology procedures. J Nucl Cardiol 24:2064–2128. https://doi.org/10.1007/s12350-017-1057-y
Chen CC, Shen TY, Chang MC, Hung GU, Chen WC, Kao CH et al (2012) Stress-induced myocardial ischemia is associated with early post-stress left ventricular mechanical dyssynchrony as assessed by phase analysis of 201Tl gated SPECT myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 39:1904–1909. https://doi.org/10.1007/s00259-012-2208-7
Singh H, Patel CD, Sharma P, Naik N, Singh S, Narang R (2015) Does perfusion pattern influence stress-induced changes in left ventricular mechanical dyssynchrony on thallium-201-gated SPECT myocardial perfusion imaging? J Nucl Cardiol 22(1):36–43. https://doi.org/10.1007/s12350-014-9979-0
Johnson LL, Verdesca SA, Aude WY, Xavier RC, Nott LT, Campanella MW, Germano G (1997) Postischemic stunning can affect left ventricular ejection fraction and regional wall motion on post-stress gated sestamibi tomograms. J Am Coll Cardiol 30:1641–1648. https://doi.org/10.1016/s0735-1097(97)00388-4
Marrugat J, Vila J, Pavesi M, Sanz F (1998) Estimation of the sample size in clinical and epidemiological investigations. Med Clin 111:267–276
Peix A, Cabrera LO, Padrón K, Rodríguez L, Fernández J, López G et al (2018) Association between non-perfusion parameters and presence of ischemia in gated-SPECT myocardial perfusion imaging studies. J Nucl Cardiol 25(2):609–615. https://doi.org/10.1007/s12350-016-0728-4
Camilletti J, Erriest J, Espinola-Zavaleta N, Hernández-Sandoval S, Redolatti M, Cartasegna L et al (2018) Left ventricular dyssynchrony and abnormalities in wall motion, assessed by gated-SPECT as ischemic auxiliary markers. J Nucl Cardiol. https://doi.org/10.1007/s12350-018-01544-4
AlJaroudi W, Alraies MC, Menon V, Brunken RC, Cerqueira MD, Jaber WA (2012) Predictors and incremental prognostic value of left ventricular mechanical dyssynchrony response during stress-gated positron emission tomography in patients with ischemic cardiomyopathy. J Nucl Cardiol 19(5):958–969. https://doi.org/10.1007/s12350-012-9592-z
Sharir T, Bacher-Stier C, Dhar S, Lewin HC, Miranda R, Friedman JD et al (2000) Identification of severe and extensive coronary artery disease by postexercise regional wall motion abnormalities in Tc-99m sestamibi gated single-photon emission computed tomography. Am J Cardiol 86:1171–1175. https://doi.org/10.1016/s0002-9149(00)01206-6
Lima RS, Watson DD, Goode AR, Siadaty MS, Ragosta M, Beller GA, Habib SH (2003) Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol 42(1):64–70. https://doi.org/10.1016/s0735-1097(03)00562-x
Kapetanopoulos A, Ahlberg AW, Taub CC, Katten DM, Heller GV (2007) Regional wall-motion abnormalities on post-stress electrocardiographic-gated technetium-99m sestamibi single-photon emission computed tomography imaging predict cardiac events. J Nucl Cardiol 14:810–817. https://doi.org/10.1016/j.nuclcard.2007.07.014
Acknowledgements
The authors thank Dr. Roxana Campisi and Dr. Gustavo Giunta for their thoughtful suggestions in the preparation of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study complies with the Declaration of Helsinki of 1964 and all subsequent revisions and was approved by the Ethics Committee of the Favaloro Foundation University Hospital.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cortés, C.M., Aramayo G, E.N., Barboza, P.E. et al. Impact of early post-stress 99mTc sestamibi ECG-gated SPECT myocardial perfusion imaging on the detection of ischemic LV dyssynchrony: an early step in the stunning cascade. Int J Cardiovasc Imaging 37, 1789–1798 (2021). https://doi.org/10.1007/s10554-020-02145-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02145-4