Abstract
Transient ischemic dilation (TID), a marker of severe coronary artery disease (CAD), is the post-stress to rest left ventricular (LV) volume ratio quantified using non ECG gated single photon emission computerized tomography (SPECT). Although prone positioning causes physiological reduction of LV volume in normal subjects, we hypothesize this may not occur in TID with underlying severe CAD as cardiac hemodynamics worsen when prone. We aim to evaluate the utility of the non ECG gated supine to prone LV volume ratio (SPLVr) for identifying severe CAD. Retrospective data analysis from 130 patients with TID ratio ≥ 1.21 and both post-stress supine and prone images. SPLVr had a significant negative correlation with summed stress (r = − 0.221, p = 0.011) and rest (r = − 0.292, p = 0.001) scores. Of the 129 cases with follow-up invasive or computed tomography coronary angiography, 52 (40.3%) had severe CAD (left main ≥ 50% stenosis, 3-vessel with ≥ 70% stenosis or 2-vessel with proximal left anterior descending ≥ 70% stenosis). Mean SPLVr was significantly lower in severe CAD cases (1.05 ± 0.14 vs 1.12 ± 0.17, p = 0.012). SPLVr predicted severe CAD on univariate [OR 0.12 (95% CI 0.00–0.35) p = 0.01] but not in multivariate analysis. SPLVr is a novel marker that negatively correlates with extent of perfusion abnormalities and is lower amongst TID patients with severe CAD. Larger studies are needed to assess if SPLVr can reliably identify underlying severe CAD amongst TID cases
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prone positioning is helpful for identifying inferior wall attenuation artefacts during single photon emission computerized tomography (SPECT) myocardial perfusion imaging (MPI) [1]. ECG gated SPECT studies have demonstrated that prone positioning result in left ventricular (LV) cavity size reduction and worsening cardiac dynamics that may vary according to presence of ischemia and prior myocardial infarction [2, 3]. Transient ischemic dilation (TID) of the LV is a specific marker for severe coronary artery disease (CAD) [4] and can be quantified by the ratio of stress to rest endocardial volumes measured from non ECG gated short axis image sets [5]. The effect of prone positioning on non ECG gated LV volumes is unknown. Given that the apparent LV cavity dilatation in TID is a result of either reduced LV function with consequent elevated end systolic volume or diffuse subendocardial hypoperfusion [6], we hypothesize that patients with TID may be more susceptible to the deleterious hemodynamic effects of prone positioning, such as worsening LV systolic and diastolic function [3]. As such, cases of TID due to severe CAD may not demonstrate the physiological reduction in LV cavity size that is usually seen in normal individuals. In this study, we aim to investigate the effect of prone positioning on non ECG gated LV volumes in cases of TID, as well as to assess the relationship between the non ECG gated supine to prone LV volume ratio (SPLVr) and markers of myocardial ischemia and severe CAD.
Materials and methods
Study population
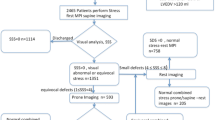
We retrospectively studied all patients who underwent stress/rest technetium-99m (Tc-99m) tetrofosmin SPECT MPI with a software-derived TID ratio ≥ 1.21 (Quantitative Perfusion SPECT, Cedars-Sinai Medical Center, Los Angeles, CA) between 1st January 2014 and 31st December 2015. Only patients with both post stress supine and prone imaging were included. Patients with previous coronary artery bypass surgery were excluded. We gathered data on demographics, medical co-morbidities and subsequent invasive coronary evaluation from electronic medical records. Patients were considered to have severe CAD if they had one of the following seen on either invasive coronary angiography (ICA) or computerized tomography coronary angiography (CTCA) within 90 days after the MPI: left main ≥ 50% stenosis, 3-vessel with ≥ 70% stenosis or 2-vessel with proximal left anterior descending ≥ 70% stenosis. The study was approved by the hospital’s Institutional Review Board.
Imaging procedure
Patients underwent stress testing with either exercise treadmill (according to the Bruce protocol) or pharmacological modalities (intravenous dipyridamole or dobutamine). We used 8 mCi of Tc-99m tetrofosmin for rest imaging and 24 mCi for stress imaging as part of a 1-day rest/stress protocol. Patients undergoing a 2-day study received 20 mCi for each imaging. All patients with body weight exceeding 80 kg underwent 2-day study with 25–30 mCi of Tc-99m tetrofosmin for each imaging depending on actual body weight. Pre-test preparation, cardiac stress testing, image acquisition and processing were performed in accordance to standard published protocols [1, 7]. All patients were scanned using a cadmium zinc telluride-based camera (Discovery NM530c, GE Healthcare). Post stress prone images were routinely acquired immediately after completion of supine imaging for all patients in our institution unless they had physical limitations for prone positioning. Gated images were acquired post stress and rest in only the supine position by dividing the cardiac cycle into eight frames. An average R–R interval of ± 15% was accepted for gating. LV volumes and LV ejection fraction (LVEF) were calculated from the gated images.
Image interpretation
All images were processed and reconstructed on a dedicated workstation (Xeleris, GE Healthcare). Visual interpretation of the images was conducted by an assigned nuclear cardiologist who was blinded to the TID ratio. Using a 20-segment model, the cardiologist scored each segment using a 5-point scoring system (0 = normal, 1 = equivocal, 2 = moderate, 3 = severe, 4 = absence of tracer uptake). Summed stress, rest and difference scores (SSS, SRS, SDS respectively) were also calculated accordingly.
Non ECG gated LV cavity volume and TID measurement
Quantitative Perfusion SPECT (QPS) software automatically generates LV volumes from non ECG gated short axis images. All contours were also manually checked by the same nuclear cardiologist for errors before the values were accepted, with adjustments made whenever necessary. We defined TID as the ratio of the non ECG gated LV cavity volumes at post stress and rest of ≥ 1.21, consistent with a previous landmark study using either exercise or dipyridamole stress and QPS software [8]. The non ECG gated SPLVr was defined as the ratio of the post stress supine to post stress prone LV volume.
Statistical analysis
Numerical variables were presented using mean and standard deviation if the data were normally distributed, or median and interquartile range if the data were skewed. These were compared using the Student’s t-test or the Mann–Whitney U test as appropriate. Categorical variables were presented using frequency and percentage and compared using Pearson Chi-squared tests. Correlation between SDS and SPLVr was assessed with Spearman’s correlation. Logistic regression model was employed to explore the predictors of severe CAD for patients with follow-up ICA or CTCA. Baseline variables showing significant association with the presence of severe CAD upon univariate analysis were entered into the multivariable model. A stepwise backward LR method was subsequently used in the multivariable model. Statistical analysis was performed using IBM SPSS statistics version 19.0, significance tests were 2-sided at the 5% significance level.
Results
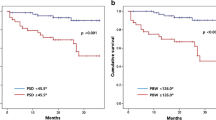
There were 5206 stress/rest SPECT MPI scans performed in the period of which 436 patients had TID ratio ≥ 1.21. Post stress prone imaging was performed in 130 patients and their baseline clinical and imaging characteristics are reported in Table 1. The mean age was 63 years and the majority (62%) were male. Cardiovascular risk factors were common in this cohort (73% hypertension, 82% dyslipidaemia, 48% diabetes mellitus). Dipyridamole stress (56%) and treadmill exercise (39%) were the most common stress modalities employed. Results of the Spearman correlation showed a significant negative correlation between SPLVr and SSS as well as between SPLVr and SDS (Fig. 1). Results of ICA or CTCA performed within 90 days after MPI were available for 129 patients and their clinical characteristics stratified by presence or absence of severe CAD are presented in Table 2. Patients with severe CAD were more likely to have a history of CAD, as well as significantly worse summed scores (SSS, SRS, SDS) and lower LVEF at rest and post stress. In addition, the non ECG gated SPLVr was significantly lower in patients with severe CAD. On univariate binary logistic regression analysis (Table 3), characteristics associated with presence of severe CAD on follow-up ICA or CTCA include SSS, SRS, SDS, both post stress and rest LVEF as well as the non ECG gated SPLVr. After adjustment for all other variables, SRS (aOR 1.13, 95% CI 1.03–1.23) and SDS (aOR 1.34, 95% CI 1.16–1.55) remained significant predictors of severe CAD. Although non ECG gated SPLVr was associated with severe CAD on univariate comparisons, it was no longer independently associated in the multivariable analysis.
Discussion
In this study, we demonstrated that amongst patients with TID, the non ECG gated SPLVr had a significant negative correlation with SPECT perfusion abnormality (SSS, SDS) and was also significantly lower in patients with severe CAD on follow-up ICA or CTCA. To our knowledge, this is the first study assessing the relationship of this novel marker and ischemic heart disease.
TID is reported when the supine post stress LV cavity volume is larger than when in rest. In practice, the post stress prone images may show either a reduction or increase in LV cavity volume (Fig. 2). The effect of prone positioning on cardiac sizes and hemodynamics has been well reported in anaesthesia literature involving otherwise healthy patients undergoing elective spine surgery [9, 10]. Prone decreases the LV volume [9], reduces cardiac index and stroke volume, as well as increases the systemic vascular resistance [10]. The effect of prone positioning for patients with pre-existing cardiac pathology is less understood, although a small study had shown that the negative impact on hemodynamics appear to be more severe in patients with poor baseline cardiac function [3]. Despite this, the indexed end systolic and end diastolic volumes for patients with ischemia in the same study were still significantly lower during prone when compared to supine positioning [3]. In contrast, our data demonstrate a significant negative correlation between the SPLVr and ischemic burden amongst patients with TID, suggesting that the non ECG gated prone LV volume increases with worsening ischemia. This may be because in TID the supine post stress LV cavity is already larger than the supine rest cavity as a result of either LV stunning or diffuse subendocardial ischemia. Since prone positioning worsens cardiovascular hemodynamics, the cavity may become even bigger as the initial pathophysiological mechanism for LV cavity dilatation is further accentuated.
Examples of transient ischemic dilatation and differential response on prone positioning seen on ungated tomographic myocardial perfusion scan images in standard short axis, vertical long axis and horizontal long axis orientations. Within each series, the top row represents post stress supine images, followed sequentially by rest supine and post stress prone images respectively. a Increase in post stress left ventricular cavity volume with prone positioning (supine stress 69 ml, supine rest 58 ml, prone stress 75 ml). b Decrease in post stress left ventricular cavity volume with prone positioning (supine stress 51 ml, supine rest 41 ml, prone stress 46 ml)
Given that TID patients with severe ischemia may have a different LV cavity response in the prone position from those with less ischemia, we proceeded to evaluate the utility of the SPLVr for identifying severe CAD amongst patients with TID on MPI. Prior studies on TID had been inconsistent with the definition of what constitutes extensive CAD [4]. Although TID is a high risk marker that warrants further invasive angiography when seen during the evaluation of suspected coronary disease [11], Class I indications for revascularization are only reserved for left main, 3-vessel or 2-vessel disease with proximal left anterior descending artery disease [12]. Using this definition, we have shown that SPLVr is significantly lower amongst patients with severe CAD, consistent with the findings from the earlier correlation analysis between SPLVr and perfusion abnormality. SPLVr was also a significant predictor of severe CAD on univariate analysis, although only SRS and SDS remain significant after multivariate analysis. There can be several reasons for this. Firstly, the small patient numbers, particularly in the group with severe CAD, makes it more difficult to achieve statistical significance. Secondly, markers of perfusion abnormality are well established and robust markers of severe CAD [6], making it less likely that another variable will be significant when analysed together in a multivariate model.
Another important finding in our study is that more than half of the patients with TID do not have severe CAD on angiography. This may be due to the our more stringent definition of severe CAD limited to coronary anatomy that constitute Class I indications for ICA and revascularisation according to guidelines [11]. Technical or contouring errors, although possible, is less likely given that all images were checked and adjusted by a nuclear cardiologist. Of note, nearly all of the 130 cases of TID required further anatomical evaluation, mostly with ICA. It is possible that many of these additional ICAs and CTCAs could have been avoided if there was a reliable marker to further risk stratify TID cases. TID, when added to perfusion abnormalities alone, is known to increase the sensitivity for diagnosing severe CAD [13]. In our cohort, we demonstrated that markers of ischemia such as the SDS also independently predict underlying severe CAD in the setting of TID. This means that physicians can be more confident that patients with TID and high SDS scores will have severe CAD requiring revascularisation when they are sent for ICA.
Our study has several limitations, the most important being the small number of patients included. In this analysis, we chose a selected group with post stress prone imaging, TID and known follow-up coronary anatomy. We only studied patients with TID for several reasons. Firstly, although TID is reported to be specific for severe CAD [4], ‘false positive’ results occur commonly in clinical practice and is supported by our data. The extent of stress perfusion abnormalities may not always predict the presence underlying severe CAD as high risk CAD can be present even in normal perfusion [14]. On the other hand, MPI is also known for underestimating the extent of CAD [15]. This underscores the need for a new and reliable marker that can identify true severe CAD specifically amongst patients with TID. We chose to study the SPLVr as we hypothesized that in a true case of severe CAD, the same pathophysiological mechanism that caused TID in the first place will be exacerbated by prone positioning, making SPLVr an possible marker for ‘true’ TID. The value of studying non TID patients is also limited as earlier SPECT studies not specifically in TID patients have already shown that cases with myocardial ischemia or infarction also have reduced LV volumes when prone [3]. Secondly, although inclusion of non TID patients may make our results more applicable to the majority of MPI cases encountered clinically, many patients with abnormal MPI but without TID are now treated medically with ICA reserved for refractory symptoms. This practice is consistent with guidelines recommending ICA only when ischemic burden is extensive [11] and supported by studies such as COURAGE [16] and the recent ISCHEMIA trial.
This study is also a retrospective analysis, making it prone to selection bias and highly dependent on the accuracy of medical documentation. The results of our single centre study may not necessarily be generalizable to other patients tested with different stress modalities, tracer or gamma camera technology. The use of an arbitrary software derived TID ratio of ≥ 1.21 may also limit the application of these results, although the TID ratios reported in the literature have varied greatly [4] and there has been no consensus on the optimal ratio to define TID. Finally, ECG gated prone images were not obtained in this study as it is not part of the institution’s usual imaging protocol. Although we are unable to draw conclusions regarding the effects of prone on volumes derived from ECG gated images, previous studies comparing static and ECG gated TID ratios have found similar trends between the two TID measures with respect to severity of coronary disease [17]. A small study also failed to show any significant difference in rest gated LVEF or volumes between supine and prone positioning [18].
Conclusion
A significant proportion of TID cases in our study do not have underlying severe CAD. SPLVr is a novel marker that correlates with extent of SPECT perfusion abnormality and is significantly lower amongst TID patients with proven severe CAD. Further studies involving larger patient numbers are needed to demonstrate if SPLVr can reliably predict severe CAD amongst patients with TID.
References
Dorbala S, Ananthasubramaniam K, Armstrong IS, Chareonthaitawee P, DePuey EG, Einstein AJ, Gropler RJ, Holly TA, Mahmarian JJ, Park M-A, Polk DM, Russell R, Slomka PJ, Thompson RC, Wells RG (2018) Single photon emission computed tomography (SPECT) myocardial perfusion imaging guidelines: instrumentation, acquisition, processing, and interpretation. J Nucl Cardiol 25:1784–1846. https://doi.org/10.1007/s12350-018-1283-y
Schaefer WM, Lipke CSA, Kühl HP, Koch K-C, Kaiser H-J, Reinartz P, Nowak B, Buell U (2004) Prone versus supine patient positioning during gated 99mTc-sestamibi SPECT: effect on left ventricular volumes, ejection fraction, and heart rate. J Nucl Med 45:2016–2020
Shimizu M, Fujii H, Yamawake N, Nishizaki M (2015) Cardiac function changes with switching from the supine to prone position: analysis by quantitative semiconductor gated single-photon emission computed tomography. J Nucl Cardiol 22:301–307. https://doi.org/10.1007/s12350-014-0058-3
Alama M, Labos C, Emery H, Iwanochko RM, Freeman M, Husain M, Lee DS (2018) Diagnostic and prognostic significance of transient ischemic dilation (TID) in myocardial perfusion imaging: a systematic review and meta-analysis. J Nucl Cardiol 25:724–737. https://doi.org/10.1007/s12350-017-1040-7
Mazzanti M, Germano G, Kiat H, Kavanagh PB, Alexanderson E, Friedman JD, Hachamovitch R, Van Train KF, Berman DS (1996) Identification of severe and extensive coronary artery disease by automatic measurement of transient ischemic dilation of the left ventricle in dual-isotope myocardial perfusion SPECT. J Am Coll Cardiol 27:1612–1620. https://doi.org/10.1016/0735-1097(96)00052-6
Bourque JM (2015) Contemporary relevance of TID: based on the company it keeps. J Nucl Cardiol 22:535–538. https://doi.org/10.1007/s12350-015-0122-7
Henzlova MJ, Duvall WL, Einstein AJ, Travin MI, Verberne HJ (2016) ASNC imaging guidelines for SPECT nuclear cardiology procedures: stress, protocols, and tracers. J Nucl Cardiol 23:606–639. https://doi.org/10.1007/s12350-015-0387-x
Abidov A, Bax JJ, Hayes SW, Hachamovitch R, Cohen I, Gerlach J, Kang X, Friedman JD, Germano G, Berman DS (2003) Transient ischemic dilation ratio of the left ventricle is a significant predictor of future cardiac events in patients with otherwise normal myocardial perfusion SPECT. J Am Coll Cardiol 42:1818–1825
Toyota S, Amaki Y (1998) Hemodynamic evaluation of the prone position by transesophageal echocardiography. J Clin Anesth 10:32–35. https://doi.org/10.1016/s0952-8180(97)00216-x
Edgcombe H, Carter K, Yarrow S (2008) Anaesthesia in the prone position. Br J Anaesth 100:165–183. https://doi.org/10.1093/bja/aem380
Fihn SD, Gardin JM, Abrams J, Berra K, Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC, Hinderliter AL, King SB, Kligfield PD, Krumholz HM, Kwong RYK, Lim MJ, Linderbaum JA, Mack MJ, Munger MA, Prager RL, Sabik JF, Shaw LJ, Sikkema JD, Smith CR, Smith SC, Spertus JA, Williams SV (2012) 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. J Am Coll Cardiol 60:e44–e164. https://doi.org/10.1016/j.jacc.2012.07.013
CRW Group, Patel MR, Calhoon JH, Dehmer GJ, Grantham JA, Maddox TM, Maron DJ, Smith PK (2017) ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2017.02.001
Xu Y, Fish M, Hyun M, Germano G, Berman D, Slomka P (2011) Diagnostic value of transient ischemic dilation for coronary artery disease in sestamibi myocardial perfusion SPECT. J Nucl Med 52:2040–2040
Nakanishi R, Gransar H, Slomka P, Arsanjani R, Shalev A, Otaki Y, Friedman JD, Hayes SW, Thomson LEB, Fish M, Germano G, Abidov A, Shaw L, Rozanski A, Berman DS (2016) Predictors of high-risk coronary artery disease in subjects with normal SPECT myocardial perfusion imaging. J Nucl Cardiol 23:530–541. https://doi.org/10.1007/s12350-015-0150-3
Beller GA (2008) Underestimation of coronary artery disease with SPECT perfusion imaging. J Nucl Cardiol 15:151–153. https://doi.org/10.1016/j.nuclcard.2008.01.012
Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL, Chaitman BR, Shaw L, Gosselin G, Nawaz S, Title LM, Gau G, Blaustein AS, Booth DC, Bates ER, Spertus JA, Berman DS, Mancini GBJ, Weintraub WS (2007) Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 356:1503–1516. https://doi.org/10.1056/NEJMoa070829
Xu Y, Arsanjani R, Clond M, Hyun M, Lemley M, Fish M, Germano G, Berman DS, Slomka PJ (2012) Transient ischemic dilation for coronary artery disease in quantitative analysis of same-day sestamibi myocardial perfusion SPECT. J Nucl Cardiol 19:465–473. https://doi.org/10.1007/s12350-012-9527-8
Yap K, Campbell P, Cherk M, McGrath C, Kalff V (2012) Effect of prone versus supine positioning on left ventricular ejection fraction (LVEF) and heart rate using ECG gated Tl-201 myocardial perfusion scans and gated cardiac blood pool scans. J Med Imaging Radiat Oncol 56:525–531. https://doi.org/10.1111/j.1754-9485.2012.02438.x
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MSY, WSJO and SJJO. The first draft of the manuscript was written by MSY and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
This study was not funded and the authors declare that they have no conflict of interest to disclose.
Ethical approval
The approval for this study had been granted by the National Healthcare Group Institutional Review Board prior to its conduct. The study therefore had been performed in accordance with the Ethical Standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yew, M.S., Ong, W.S.J. & Ong, S.J.J. Non ECG gated supine to prone left ventricular volume ratio: a novel marker for myocardial ischemia. Int J Cardiovasc Imaging 36, 1377–1384 (2020). https://doi.org/10.1007/s10554-020-01836-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01836-2