Abstract
The purpose of this work was to evaluate CMR T1 and T2 mapping sequences in patients with intracardiac thrombi and masses in order to assess T1 and T2 relaxometry usefulness and to allow better etiological diagnosis. This observational study of patients scheduled for routine CMR was performed from September 2014 to August 2015. All patients referred to our department for a 1.5 T CMR were screened to participate. T1 mapping were acquired before and after Gadolinium injection; T2 mapping images were obtained before injection. 41 patients were included. 22 presented with cardiac thrombi and 19 with cardiac masses. The native T1 of thrombi was 1037 ± 152 ms (vs 1032 ± 39 ms for myocardium, p = 0.88; vs 1565 ± 88 ms for blood pool, p < 0.0001). T2 were 74 ± 13 ms (vs 51 ± 3 ms for myocardium, p < 0.0001; vs 170 ± 32 ms for blood pool, p < 0.0001). Recent thrombi had a native T1 shorter than old thrombi (911 ± 177 vs 1169 ± 107 ms, p = 0.01). The masses having a shorter T1 than the myocardium were lipomas (278 ± 29 ms), calcifications (621 ± 218 ms), and melanoma (736 ms). All other masses showed T1 values higher than myocardial T1, with T2 consistently >70 ms. T1 and T2 mapping CMR sequences can be useful and represent a new approach for the evaluation of cardiac thrombi and masses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cardiac tumors are a relatively rare condition, with a reported prevalence of less than 1% in autopsy series [1]. Pseudo-tumors, among which cardiac thrombi, are much more frequent [2]. They are often detected by echocardiography, but cardiac magnetic resonance (CMR) imaging has now emerged as the method of choice for their evaluation, allowing unlimited imaging planes, a large field of view and an interesting contrast with relevant tissue characterization to discriminate between the different components of these structures. Their content in fat and in water can be appreciated by T1- and T2-weighted sequences with distinctive signal features. Post-gadolinium late-enhancement imaging provides complementary tissular characterization, in regard to potential vascularization or fibrosis [3].
New CMR sequences called T1 and T2 mapping provided an important breakthrough by offering simple and effective diagnostic possibilities [4]. With these easily implemented sequences, the intensity of each pixel corresponds precisely to the value of the T1 or T2 relaxation times [5]. In contrast, usual CMR sequences are adjusted to provide a degree of “weighting” of these parameters, but do not provide the absolute value of T1 or T2. T1 or T2 mapping are based on sets of precisely known T1 or T2 weighting images. After correction for misregistration and exponential fitting, pixel wise T1 or T2 parametric images are obtained. Measurements can be performed before or after injection of contrast agent (gadolinium). Access to a true absolute quantification rather than a simple weighting of the image contrast can be considered a true revolution in CMR. If T1 and T2 mapping sequences have been already extensively described in the setting of cardiomyopathies, only seldom studies have focused on T1 or T2 mapping in cardiac masses [6–8].
The main objective of this work was to evaluate T1 and T2 mapping in patients with intracardiac thrombi or cardiac masses in order to assess if T1 and T2 relaxometry might be useful for the etiological diagnosis of these cardiac masses.
Materials and methods
This observational study of patients scheduled for routine cardiac MRI, was performed in accordance with the ethics rules of our institution and was approved by our institutional review board. An informed consent was obtained from all patients.
Population study
From September 2014 to August 2015, all patients referred to our department for a 1.5 T CMR were screened to participate in the study (n = 598). Patients referred for MR characterization of cardiac mass or thrombus, as well as those for which a mass or thrombus was discovered at the time of the examination were enrolled. Exclusion criteria were, in addition to the classical contraindications to MRI, subjects younger than 18 years old, pregnancy, inability to give informed consent, or severe agitation or any other condition that could interfere with the patient’s ability to comply with the examination. 41 patients were included. 22 presented with cardiac thrombi and 19 presented with cardiac masses. The diagnosis of cardiac thrombus was based on the clinical context and on the regression of the mass during anticoagulant therapy. Based on the clinical context, thrombi were classified according to their age into recent (<1 week), old (>1 month) or of undetermined age. Among patients with tumoral masses, histological results were available in cases of myxoma, rhabdomyoma, lymphoma, renal carcinoma metastasis, melanoma metastasis, and papillary fibroelastoma. The diagnosis of other masses was based on the clinical context (known calcifications, history of cancer,…), and results of other imaging tests (echocardiography, CT-scan, PET-scan).
MR imaging
MRI examination was performed on a 1.5 T imaging system (Aera XQ MRI, Siemens, Erlangen, Germany) equipped with a dedicated 6-channel cardiac coil. The CMR imaging protocol included was standardized with the following sequences acquired at least in the long axis, short axis and four-chamber orientations: Half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequences, T2-weighted sequences with Short Tau-inversion recovery (STIR) and fat suppression technique, steady-state free precession (SSFP) cine sequences, post-injection (Gadovist at a dose of 0.1 mmol/kg, Bayer Healthcare, Leverkusen, Germany) sequences including perfusion sequences (early after bolus injection) and delayed enhancement up to 10 min after injection (inversion-recovery sequences and phase-sensitive inversion recovery sequences). Concerning the dedicated T1 mapping sequences, the native T1 modified Look-Locker inversion-recovery sequence (MOLLI, 3(3)3(3)5) and T2 mapping images were obtained by the Siemens Tx-mapping WIP780 (VD13A) package just before injection of Gadolinium. Post-contrast T1 Mapping sequences were performed 10 min after injection.
The reported values of relaxation times were measured in regions of interest (ROI) drawn in cardiac masses, myocardial wall and blood pool, taking care to exclude proximity cardiac structures (e.g. excluding the blood pool and epicardial fat when ROI placed in the myocardium). All measurements were performed on at least two imaging planes, by two operators and then averaged. The planimetry of the cardiac mass or thrombus was obtained on the plane where it was the bigger using a freehand drawn ROI. The image analysis and post-treatment were performed using OsiriX software version 3.9.2 (Pixmeo SARL, Geneva, Switzerland).
Statistical analysis
Statistical analyses were performed using SPSS software version 18 (SPSS Inc., Chicago, Illinois, USA). Continuous variables are expressed as mean ± standard deviation. Categorical variables are presented as numbers (percentages). A Student’s t test (continuous variables) was performed to determine differences between the two groups after passing a preliminary Shapiro–Wilk test for normality. p values (two-tailed test) <0.05 were considered statistically significant.
Results
Thrombi
Patient characteristics
25 patients with intracardiac thrombi were included. 22 patients (16 men, mean age 64 ± 15 years) with thrombi were finally analyzed by T1 and T2 mapping sequences because 3 patients were excluded owing to image planes that did not encompass the thrombus. 126 different image planes were acquired (average of 5.7 per patient). The location of the thrombus was preferentially in the left ventricle (16, including 13 in a context of ischemic cardiomyopathy and three in a context of non-ischemic dilated cardiomyopathy). Three thrombi were located in the right atrium (including one case of cardiac amyloidosis) and three in the left atrium. The thrombus size was an average of 1.7 ± 1.3 cm2.
MRI findings
The native (before injection of gadolinium) T1 relaxation time of thrombi was 1037 ± 152 vs 1032 ± 39 ms for myocardium (p = 0.88). Blood pool T1 was 1565 ± 88 ms. The post-gadolinium T1 relaxation time of thrombi was significantly longer than T1 of myocardium (731 ± 208 vs 339 ± 67 ms, p < 0.0001) as well as compared with T1 of blood pool (222 ± 52 ms, p < 0.0001). Post contrast T1 decrease were respectively 29.5% (thrombus), 67.2% (myocardium) and 85.8% (blood pool). The native T2 relaxation time of thrombi was significantly longer as compared to myocardium (74 ± 13 vs 51 ± 3 ms < 0.0001), and significantly shorter than blood pool T2 (170 ± 32 ms, p < 0.0001).
Based on the clinical context, thrombi were classified according to their age into recent (<1 week), old (>1 month) or of undetermined age. Recent thrombi (n = 6) had a native T1 shorter than old thrombi (n = 11): (911 ± 177 vs 1169 ± 107 ms, p = 0.01). The decrease of T1 after gadolinium injection was not significantly different between recent and old thrombi (−26.0 ± 13 vs −32.3 ± 18%, respectively, p = 0.55). T2 did not allow to differentiate between recent and old thrombi (73.8 ± 7.3 vs 71.9 ± 10.9 ms, p = 0.72).
Cardiac masses
Patient characteristics
19 patients (8 men, mean age 65 ± 16 years) with cardiac masses were analyzed by T1 and T2 mapping sequences on 124 different image planes (an average of 6.5 per patient). Their location was very variable in the heart: intra or para-left ventricular (n = 5), in the left atrioventricular groove (n = 2), the right atrium (n = 3), the left atrium (n = 2), the right ventricle (n = 1), the inter-atrial septum (n = 1), the mitral valve or annulus (n = 4) and the tricuspid valve (n = 1). The types of masses were as follow: two myxomas, two papillary fibroelastomas, one hemangioma, one rhabdomyoma, four lipomas, five calcified masses, one lymphoma, three metastases (renal adenocarcinoma, melanoma, unknown origin). The masses size was 8 ± 12 cm2.
MRI findings
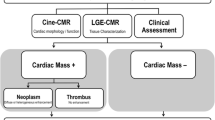
Overall results are summarized in Table 1 and in Fig. 1.
Three kinds of masses presented with native T1 shorter than the myocardium: lipomas (278 ± 29 ms), calcifications (621 ± 218 ms), and melanoma metastasis (736 ms). These masses with a short T1 could be distinguished by:
-
i.
the post-gadolinium T1, which did not decrease significantly for lipomas and calcifications (−1.5%) as compared to the melanoma (−59%)
-
ii.
the value of T2: short for calcifications (42 ± 7 ms), intermediate for the melanoma (58 ms) and very long for lipomas (111 ± 12 ms).
All other masses showed native T1 values longer than myocardial T1 values, with T2 values always increased over 70 ms. In particular, the long values of both T1 (1926 ms) and T2 (180 ms) of the two papillary fibroelastomas should be stressed.
Discussion
In this observational study including 41 patients with cardiac thrombi (n = 22) or masses (n = 19), we were able to assess the values of T1 and T2 relaxation times with T1 and T2 mapping CMR sequences.
Thrombi
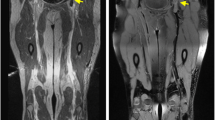
Thrombi generally showed T1 values similar to that of normal myocardium (Fig. 2), with a significant difference between recent (shorter T1) and old (longer T1) thrombi. T2 relaxation times of thrombi were consistently longer than myocardial T2, regardless of their age. Post-contrast T1 values of thrombi decreased about 30% as compared with pre-contrast T1. This could be explained by either some degree of gadolinium soaking inside the thrombus and/or by partial volume effect in small thrombi (owing to inclusion of some blood in the image slice).
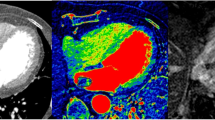
Thrombus: Chronic (>1 year-old) apical thrombus in a 36-year old patient with anterior myocardial infarction. Slightly longer T1 (a) and T2 (b) values are measured in the thrombus as compared with normal myocardium. Despite lack of visible gadolinium uptake on late enhacement imaging (d), a 33% drop in T1 value is observed 10 min after gadolinium injection (c)
The analysis of intracardiac tumors and masses with T1 and T2 mapping disclosed important differences among the different subtypes, generating multiple T1 / T2 profiles according to the etiology: short T1/short T2 (as compared with myocardium) for calcifications (Fig. 3), short T1/long T2 for melanoma or lipomas, long T1/long T2 for most tumors, whether benign or malignant (Fig. 4), with different degrees in particular for the T1 (close to the myocardium for rhabdomyoma, long or very long for myxomas and fibroelastomas (Fig. 5)).
Calcification: 25 mm large calcified rounded mass with regular contours embedded in the basal part of the hypertrophied interventricular septum in a 71 year-old patient with mild aortic stenosis. The shortest T1 values of all cardiac masses (a) are observed in case of calcifications (demonstrated by CT in b). T2 was 39 ms. T1 value decreases (−21%) after gadolinium injection (c) and a thin annular rim of hyperenhacement is seen (d) around the calcification (as well as an apical transmural infarct scar)
Renal cell carcinoma metastasis: Huge right ventricular metastasis of a renal cell carcinoma (histologically proven after biopsy) in a 83 year-old male with history of nephrectomy 18 months before. Most of the right ventricle is obstructed by the mass, showing elevated T1 (a) and T2 (b) values. Marked tumoral vascularization is demonstrated by the 72% post-gadolinium T1 drop (c) related to multiple tumoral septa separated by necrotic area (d)
Papillary fibroelastoma (surgically proven) in a 70-year old female. An elongated small mobile mass was discovered by echocardiography on the atrial side of the anterior tricuspid leaflet. Very long T1 and T2 values are observed in case of fibroelastoma (longest values of all cardiac masses). On these short axis MR views, T1 is 2053 ms (a) and T2 is 183 ms (b). Strong gadolinium uptake is seen on late (>10 min) post-contrast imaging (c, d) with marked T1 drop (111 ms)
Our results seem to be consistent with previous reports from the literature in terms of signal intensity on T1- and T2-weighted sequences. Indeed, it is known that MRI thrombi properties depend on their age and content [9]. Most of the literature reviews [3] that focus on the signal of cardiac thrombi classify them according to their age as acute, subacute or chronic. At the very acute phase of their formation, thrombi are usually T1- and T2-hyperintense (short T1 and long T2) because hemoglobin is still oxygenated. In a subacute thrombus, hemoglobin is metabolized into methemoglobin. The paramagnetic effect of methemoglobin (shortening of the relaxation times) is responsible for a high T1 signal (shortening of T1). The T2 signal is generally increased (longer T2) because of water content due to red cells lysis. After a longer period of time, the thrombus is depleted of water and cell debris containing methemoglobin are replaced by fibrous tissue, responsible for a decrease in signal on T1-weighted images (longer T1) and a decrease of signal on T2-weighted images (shortening of T2). The terminology differentiating acute and subacute thrombi, mostly derived from neuroradiology studies [10] and experimental works involving animal models [11], seems relatively inappropriate for cardiac thrombi. Indeed, it is quite uncommon to obtain CMR images of a thrombus at the very acute phase (1st day). We did not observe in our cohort thrombi at such early stage of formation. However, we were able to differentiate between recent (<1 week), and old (> 1 month) thrombi for some of them. T1 mapping allowed us to highlight the difference between recent and old thrombi, as recent thrombi had a significantly shorter T1. However, this difference was not found on T2 mapping sequences. The T2 was long as compared to the myocardium, regardless of the age or location of the thrombus. In this study, thrombus was probably not diagnosed in the very early phase and that might explain why the T2 times were not found to change between acute and chronic thrombus. Also, thrombus in this setting may not be accompanied by the injury seen in other tissues such as the brain and hence the degree of associated edema may be less with intracardiac thrombus.
Cardiac masses
Furthermore, there are only very few cases reported in the literature for cardiac masses analyzed by T1 and/or T2 mapping. Except for two cases of myxomas [6, 7], one case of a calcified mitral pseudocyst and a lipomatous hypertrophy of the interatrial septum [8], this study is the first series of cases on the subject including various etiologies of intracardiac masses and tumors. The Table 2 illustrates the most frequent types of cardiac masses, with a comparison of T1- and T2- weighted signal intensity data and our T1- and T2-mapping results. Our data is in line with previously described data in the literature except for the T2 of old thrombi (long values vs non-increased values usually described).
Limitations
There are several limitations in this study among which, its limited number of patients. This preliminary data would benefit from the performance of a pluricentric work on a larger scale, including several cases for each tumor subtype to corroborate our results, as well as the few tumor etiologies missing in our work (sarcoma, fibroma, etc.). However, intracardiac masses are relatively rare, and access to CMR Tx mapping sequences is still limited. Moreover, the anatomopathological diagnosis could not be obtained for all patients (hemangioma, one metastasis from unknown origin). However the clinical context and the contribution of multimodality imaging allowed a relative certainty of diagnosis for virtually all the patients included. Finally, Tx mapping methods are vendor specific with variable accuracy and precision of relaxation times values between systems and sequences. Therefore these data should be interpreted with caution as they might not be applicable to all systems and sequences.
Clinical perspectives
To be able to quantify T1 and T2 values of cardiac masses seems to be very interesting in the seek for incremental discriminative diagnostic performance of CMR. Usual T1 and T2-weighted sequences often remain insufficient with similar signal intensity characteristics for several tumor etiologies. Thus, being able to get absolute relaxometry values might help to differentiate between the most common masses. Our results highlight the particular appeal of such sequences for the diagnosis of melanoma metastases and for papillary fibroelastomas, in which T1 and T2 relaxation times are quite singular (Fig. 1). For the latter, these new CMR tools might be of help when the Gadolinium injection is contra-indicated, in so far as the native sequences seem to be highly informative. Thus, T1 and T2 mapping might become the new indispensable tool for the noninvasive diagnosis of papillary fibroelastomas, just as it is for cardiac amyloidosis [18]. Another interesting clinical perspective might be the potential contribution of these sequences for the follow-up of malignant tumors (e.g. lymphomas) during and after cancer chemotherapy.
In contrast, for cardiac thrombi, the incremental value of T1 and T2 mapping sequences in terms of diagnostic capability seems poor, and late-gadolinium enhancement (LGE) sequences must still be regarded as the gold-standard. However, the assessment of thrombi T1 might help to evaluate the age of thrombi and thus help to guide the antithrombotic treatment.
Conclusion
This small observational study showed that T1 and T2 mapping CMR sequences could be useful and represent a new approach for the evaluation of cardiac tumors and masses. This work demonstrates, how the integration of new cardiac imaging techniques can contribute to the exploration of a cardiac mass, and ultimately help the etiological diagnosis, providing complementary information to that of the echocardiography, CT-scan and usual CMR sequences. T1 and T2 mapping CMR sequences allow a significant improvement in the approach of tissue characterization. Despite the small size of the present study, our results could give the foundations for a more comprehensive analysis of the different types of cardiac masses. For cardiac thrombi, these CMR sequences could assist in the differential diagnosis of an intracardiac mass, although the post-Gadolinium sequences (with 3D acquisition) remain the gold standard. Nevertheless, when a patient has a gadolinium injection contra-indication, these sequences could be used to provide additional support to confirm the diagnosis. Moreover, the estimation of native T1 could also help to know the age of a thrombus.
Abbreviations
- CMR:
-
Cardiac magnetic resonance
- HASTE:
-
Half-Fourier acquisition single-shot turbo spin-echo
- LGE:
-
Late gadolinium enhancement
- MRI:
-
Magnetic resonance imaging
- MOLLI:
-
Modified Look-Locker inversion-recovery
- ROI:
-
Region of interest
- SSFP:
-
Steady-state free precession
- STIR:
-
Short Tau-inversion recovery
- Tx mapping:
-
T1 and T2 mapping software
References
Sütsch G, Jenni R, von Segesser L, Schneider J (1991) Heart tumors: incidence, distribution, diagnosis—exemplified by 20,305 echocardiographies. Schweiz Med Wochenschr 121:621–629
Mollet NR, Dymarkowski S, Volders W et al (2002) Visualization of ventricular thrombi with contrast-enhanced magnetic resonance imaging in patients with ischemic heart disease. Circulation 106:2873–2876
Motwani M, Kidambi A, Herzog BA, Uddin A, Greenwood JP, Plein S (2013) MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology 268:26–43
Salerno M, Kramer CM (2013) Advances in parametric mapping with CMR imaging. J Am Coll Cardiovasc Imaging 6:806–822
Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP (2004) Modified look-locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 52:141–146
Germain P, El Ghannudi S, Jeung M-Y et al (2014) Native T1 mapping of the heart—a pictorial review. Clin Med Insights Cardiol 8:1–11
Kübler D, Gräfe M, Schnackenburg B (2013) T1 and T2 mapping for tissue characterization of cardiac myxoma. Int J Cardiol 169:e17–e20
Ferreira VM, Holloway CJ, Piechnik SK, Karamitsos TD, Neubauer S (2013) Is it really fat? Ask a T1-map. Eur Heart J Cardiovasc Imaging 14:1060
Blackmore CC, Francis CW, Bryant RG, Brenner B, Marder VJ (1990) Magnetic resonance imaging of blood and clots in vitro. Invest Radiol 25:1316–1324
Schellinger PD, Chalela JA, Kang DW, Latour LL, Warach S (2005) Diagnostic and prognostic value of early MR imaging vessel signs in hyperacute stroke patients imaged <3 h and treated with recombinant tissue plasminogen activator. Am J Neuroradiol 26:618–624
Corti R, Osende JI, Fayad ZA et al (2002) In vivo noninvasive detection and age definition of arterial thrombus by MRI. J Am Coll Cardiol 39:1366–1373
Esposito A, De Cobelli F, Ironi G (2014) CMR in assessment of cardiac masses: primary benign tumors. J Am Coll Cardiol Imaging 7:733–736
Braggion-Santos MF, Koenigkam-Santos M, Teixeira SR, Volpe GJ, Trad HS, Schmidt A (2013) Magnetic resonance imaging evaluation of cardiac masses. Arq Bras Cardiol 101(3):263–272
Altbach MI, Squire SW, Kudithipudi V, Castellano L, Sorrell VL (2007) Cardiac MRI is complementary to echocardiography in the assessment of cardiac masses. Echocardiography 24:286–300
Vallurupalli S, Hayes K, Bhatti S (2014) Ventricular papillary fibroelastoma. J Am Coll Cardiol 63:2170
Srivatsa SV, Adhikari P, Chaudhry P, Srivatsa SS (2013) Multimodality imaging of right-sided (tricuspid valve) papillary fibroelastoma: recognition of a surgically remediable disease. Case Rep Oncol 6:485–489
Kiaffas MG, Powell AJ, Geva T (2002) Magnetic resonance imaging evaluation of cardiac tumor characteristics in infants and children. Am J Cardiol 89:1229–1233
Karamitsos TD, Piechnik SK, Banypersad SM (2013) Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. J Am Coll Cardiol Imaging 6:488–497
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caspar, T., El Ghannudi, S., Ohana, M. et al. Magnetic resonance evaluation of cardiac thrombi and masses by T1 and T2 mapping: an observational study. Int J Cardiovasc Imaging 33, 551–559 (2017). https://doi.org/10.1007/s10554-016-1034-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-1034-6