Abstract
To assess right ventricular functions by echocardiography in patients with proximal right coronary artery (RCA) CTO and correlating it with clinical and angiographic variables. We studied 60 consecutive patients with CTO of the proximal RCA and no other significant lesions in the left coronary system. Echocardiography was performed in order to measure left ventricular (LV) dimensions, LVEF, RV end diastolic area (RVEDA), RV end systolic area (RVESA), RV fractional area change (RVFAC), tricuspid annular plane systolic excursion (TAPSE), Doppler myocardial performance index (MPI), trans-tricuspid E and A waves, E/A ratio, S′, e′ and a′. Grades of coronary collaterals was assessed. Doppler MPI showed negative correlation with TAPSE (r = −0.8997, p < 0.0001) and RVFAC (r = −0.928, p < 0.0001). Positive correlation with trans-tricuspid E/A ratio (r = 0.893, p < 0.0001) and E/e′ ratio (r = 0.783, p < 0.0001). Patients with no evidence of MI had more well-developed (grade 3) coronary collaterals (83.8 vs. 17.4 %). Patients with evidence of MI had lower RVFAC 38.13 ± 5.39 versus 45.08 ± 4.99 % (p < 0.0001), lower TAPSE 20.17 ± 3.85 versus 25.35 ± 3.46 mm (p < 0.0001), higher MPI 0.4 ± 0.08 versus 0.31 ± 0.05 (p < 0.0001), higher trans-tricuspid E/A ratio 1.79 ± 0.38 versus 1.13 ± 0.36 (p < 0.0001) and E/e′ ratio 5.23 ± 1.02 versus 3.61 ± 0.88 (p < 0.0001). Patients with poorly developed collaterals had lower TAPSE and RVFAC and a higher MPI (p < 0.0001 for each). Patients with proximal RCA CTOs and evidence of inferior wall MI have significant impairment of RV functions in addition to poorly developed coronary collaterals. Those with proximal RCA CTOs and well-developed coronary collaterals have better RV functions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Echocardiographic assessment of right ventricular (RV) functions has been gaining importance in recent years after being fairly neglected in the past. Several quantitative methods for assessment of the RV have been validated after mainly depending on qualitative assessment in the past and are now recommended as standard by both the American Society of Echocardiography (ASE) and the European Association of Cardiovascular Imaging (EACVI) [1, 2].
RV functions have been shown to have an effect of long term outcomes of patients especially in the setting of myocardial infarction (MI) [3], pulmonary hypertension and pulmonary embolism [4].
Chronic total occlusions (CTO) have been reported to have a prevalence of about 20 % in large registries among patients with known or suspected coronary artery disease. The clinical benefit of opening CTOs is still a topic of debate with increasing evidence from several registries and retrospective studies supporting the clinical benefit from revascularization of occluded vessels by percutaneous coronary intervention (PCI) [5, 6].
The aim of this study was to assess right ventricular functions by echocardiography in patients with proximal right coronary artery (RCA) CTO and correlating it with clinical and angiographic variables.
Methods
Study design
We studied 60 consecutive patients presenting to our catheterization laboratory for elective, clinically-indicated coronary angiography found to have CTO of the proximal RCA with no other significant lesions in the left coronary system in the period between December 2013 and August 2015.
Chronic total occlusion was defined as complete interruption of coronary blood flow [Thrombolysis in Myocardial Infarction (TIMI) flow grade 0] with estimated duration of the occlusion ≥3 months [7, 8]. Proximal RCA was defined as the segment from the ostium of the RCA to one half the distance to the acute margin of the heart according to the SYNTAX scoring system [9].
Approval of institutional ethical committee was obtained. Informed consents were required from all subjects. Patients were excluded from the study if they had one or more significant lesions in the left coronary system (defined as luminal stenosis ≥50 % in the left main coronary or proximal left anterior descending arteries or ≥70 % luminal stenosis in any other segment of the left coronary system), recent (<3 months) MI or acute coronary syndrome, patients with obstruction in the mid or distal RCA, history of previous PCI or coronary artery bypass grafting (CABG), significant valvular stenosis or more than mild tricuspid regurgitation, left ventricular ejection fraction (LVEF) <50 %, any cardiomyopathy, rhythm other than sinus, pulmonary hypertension, chronic obstructive pulmonary disease, history of pulmonary hypertension of any etiology or history of pulmonary embolism.
Clinical history and electrocardiogram (ECG)
Detailed patient history was taken specially to assess the presence of history of ischemic symptoms consistent with developing an old inferior wall MI (defined in this study as history of MI ≥ 3 months in addition to pathological Q waves in ≥2 of the inferior leads on 12-lead ECG according to the third universal definition of MI [10]). We considered history and ECG together as ECG alone can underestimate the presence of MI in patients with CTO [5, 11].
Angina was graded at presentation using the Canadian Cardiovascular Society (CCS) classification [12].
Trans-thoracic echocardiography
Standard trans-thoracic echocardiography with machine-integrated ECG recording was performed for all patients using a Vivid S5 machine with an M3S matrix sector array probe with a frequency range from 1.7 to 3.2 MHz (GE Vingmed, Horten, Norway). A standard study following standardized protocols [2] was performed for all subjects by an echocardiographer accredited by the EACVI in order to obtain the following measurements: left ventricular (LV) dimensions measured by M-mode from the parasternal short axis view at the level of the papillary muscles, LVEF measured by Simpson’s method of discs [2].
Assessment of RV areas
From an RV-focused apical four chamber view, manual tracing of the RV endocardial border was performed starting from the lateral tricuspid annulus along the free wall to the apex and back to the medial tricuspid annulus along the interventricular septum at end-diastole and at end-systole to measure RV end diastolic area (RVEDA) and RV end systolic area (RVESA) respectively (trabeculations, papillary muscles and moderator band were included in the cavity area).
We assumed a normal reference range of 10–25 cm2 for RVEDA and 4–14 cm2 for RVESA [1, 2].
Estimation of RV systolic function
RV fractional area change (RVFAC)
RVFAC was defined as (RVEDA–RVESA)/RVEDA X 100. We assumed the normal value of RVFAC to be ≥35 % [1, 2].
Tricuspid annular plane systolic excursion (TAPSE)
From the apical four chamber view, TAPSE was measured by M-mode echocardiography as the distance of systolic excursion of the lateral RV annular segment of the tricuspid valve along its longitudinal plane. Total displacement was measured by the leading edge to leading edge convention and expressed in millimeters. We assumed the normal value of TAPSE to be ≥16 mm [1, 2].
Doppler myocardial performance index (MPI)
From the apical four chamber view, pulsed wave Doppler was acquired by placing the sample volume between the leaflet tips of the tricuspid valve with the Doppler beam aligned with RV inflow and measurements taken at end expiration for trans-tricuspid early diastolic velocity (E) wave, late diastolic velocity (A) wave, and E/A ratio. In addition, tricuspid valve closure-opening time (TCO) was measured as the time from tricuspid valve closure (marked at the end of A wave) to tricuspid valve opening (marked at the beginning of E wave) in the next cardiac cycle.
Pulsed wave Doppler of the RV outflow was acquired by placing the sample volume in RV outflow tract. Ejection time (ET) was calculated as time from onset to cessation of flow across the pulmonary valve.
MPI was calculated as (TCO–ET)/ET. We assumed the normal value of MPI to be <0.4 [1, 2].
Pulsed wave tissue Doppler imaging (TDI)
Pulsed wave TDI images were acquired by placing the region of interest in the RV free wall at the level of tricuspid annulus. Gains were optimized and low wall filter settings were selected in addition to a Doppler velocity range of −20 to +20 cm/s with a sweep speed of 50 mm/s. Having proper alignment with ultrasound beam was considered mandatory. Peak velocities of the following waves were measured: (S′) which is the major positive (systolic) wave, (e′) which is the first negative (diastolic) wave and (a′) which is the second negative wave.
We assumed the normal value of S′ velocity to be ≥9.5 cm/s, of e′ to be ≥7.8 cm/s of e′/a′ to be ≥0.52 [1, 2].
RV wall motion abnormality
The presence or absence of RV wall motion abnormality was assessed qualitatively from the parasternal short axis view at the level of the aortic valve and from the apical four chamber view.
Estimation of RV diastolic function
Trans-tricuspid E/A ratio, e′/a′ ratio, e′ velocity and E/e′ ratio were taken as measurements of RV diastolic function.
We assumed the normal E/A ratio to be 0.8–2.1, E/e′ ratio to be ≤6, e′/a′ to be 0.5–1.9, e′ to be 8–20 cm/s [1, 2].
Coronary angiography
Coronary angiography was performed using standard techniques with assessment of the left and right coronary arteries in several orthogonal views. RCA CTO was assessed to confirm site of occlusion and the grades of coronary collaterals which were classified according to Rentrop as Grade 0 for no collaterals; Grade 1 for filling of side branches of the artery to be perfused via collateral vessels without visualization of the epicardial segment; Grade 2 for partial filling of the epicardial segment via collateral vessels; and Grade 3 for complete filling of the epicardial segment via collateral vessels [13]. The presence of well-developed coronary collaterals was defined as Rentrop grade 3 while poorly developed collaterals was defined as Rentrop class <3.
Statistics
Data were statistically analyzed using IBM SPSS Statistics version 23 (IBM corporation, Armonk, NY, USA). Categorical variables were expressed as number and percentage and analyzed using Fisher’s exact test. Continuous variables were expressed as mean ± SD and analyzed using student’s t test and one-way ANOVA test for variables that passed normality tests while Mann–Whitney U-test and non-parametric ANOVA test were used for those that did not pass normality. Correlations were analyzed using Pearson’s correlation coefficient (r). A probability value p < 0.05 was considered statistically significant and a p value <0.0001 was considered highly significant.
Results
Baseline characteristics
The baseline clinical characteristics are detailed in Table 1. Angiographic assessment of collaterals found Rentrop grade 1 in 15 (25 %) patients, Rentrop grade 2 in 10 (16.7 %) patients and Rentrop grade 3 in 35 (58.3 %) patients.
Echocardiographic measurements are detailed in Table 2. Measurements of RV systolic function showed that MPI was abnormal in 19 (31.7 %) patients, RVFAC was abnormal in 9 (15 %) patients while TAPSE was normal in all patients. Regarding measures of RV diastolic function, E/A ratio was abnormal in 6 (10 %) patients and E/e′ ratio in 3 (5 %) patients, all other measures of diastolic function were normal. There was no evidence of RV wall motion abnormalities in all patients.
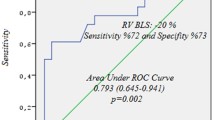
Correlating MPI to echocardiographic measurements of the RV
Doppler MPI showed a strong negative correlation with each of TAPSE (r = −0.8997, p < 0.0001) and RVFAC (r = −0.928, p < 0.0001). However, it showed a strong positive correlation with both trans-tricuspid E/A ratio (r = 0.893, p < 0.0001) and E/e′ ratio (r = 0.783, p < 0.0001). Correlations were also found with trans-tricuspid E and A wave velocities, in addition to, all tissue Doppler velocities of the tricuspid annulus at the RV free wall (Table 3).
Comparing patients according to the presence of old inferior wall MI
We classified patients into 2 subgroups according to the presence (n = 23) or absence (n = 37) of an old inferior wall MI (defined as a history of MI ≥ 3 months in addition to pathological Q waves in the inferior leads on ECG).
Patient characteristics
Patients with evidence of old inferior wall MI had a larger body mass index (BMI) 35.04 ± 7.07 versus 30.78 ± 6.38 kg/m2 (p = 0.019). On the other hand, there was a slightly larger number of hypertensives in the group with no evidence of old inferior wall MI 26 (70.3 %) versus 10 (43.5 %) but this did not reach statistical significance (p = 0.058). There was no difference between both groups regarding age, gender, and presence of diabetes mellitus (Table 4). They also had comparable CCS angina at presentation (p = 0.545).
Angiographic findings
The group with no evidence of old inferior wall MI had a larger number of patients with well-developed (grade 3) coronary collaterals (83.8 vs. 17.4 %) while those in the group with evidence of old inferior wall MI had a larger number with poorly developed (grade 1 and 2) collaterals (82.6 % vs. 16.2 %, p < 0.0001).
Echocardiographic measurements
There was no difference between both groups regarding LV dimensions and LVEF (Table 5).
Patients with evidence of old inferior wall MI had a larger RVESA 10.41 ± 1.08 versus 9.47 ± 0.85 cm2 (p = 0.0004) and accordingly had a lower RVFAC 38.13 ± 5.39 versus 45.08 ± 4.99 % (p < 0.0001). TAPSE was also lower in that group 20.17 ± 3.85 versus 25.35 ± 3.46 mm (p < 0.0001), while Doppler MPI was higher in that group 0.4 ± 0.08 versus 0.31 ± 0.05 in the group with no evidence of old inferior wall MI (p < 0.0001).
Regarding measurements of RV diastolic function, the group with evidence of old inferior wall MI had a larger trans-tricuspid E wave velocity and a lower A wave velocity (p < 0.0001 for both) and accordingly had a higher trans-tricuspid E/A ratio of 1.79 ± 0.38 versus 1.13 ± 0.36 (p < 0.0001). All tissue Doppler velocities (e′ and a′) from the tricuspid annulus at the RV free wall were lower in the group with evidence of old inferior wall MI (p < 0.0001 for each), in addition, tricuspid E/e′ ratio was higher in that group 5.23 ± 1.02 versus 3.61 ± 0.88 (p < 0.0001). However, there was no difference regarding e′/a′ ratio (p = 0.978).
Comparing patients according to coronary collateral grade
Patients were also classified according to coronary collateral grade into 3 subgroups grade 1 (n = 15), grade 2 (n = 10) and grade 3 (n = 35).
Patient characteristics
There was a significantly lower number of patients with history of an old inferior wall MI in grade 3 patients 4 (11.43 %) in comparison to grades 1 and 2 (86.67 and 60 % respectively) (p < 0.0001). There was no difference between the three groups regarding age, gender, smoking status, presence of diabetes mellitus or hypertension, and BMI (Table 6).
Echocardiographic measurements
Patients with grade 1 collaterals had significantly lower TAPSE and RVFAC and a higher MPI (p < 0.0001 for each) (Table 7).
Regarding measurements of RV diastolic function, patients with poorly developed coronary collateral grades had larger trans-tricuspid E wave velocities, lower A wave velocities and accordingly had a higher trans-tricuspid E/A ratio (p < 0.0001 for each). In addition, they had lower tissue Doppler velocities (e′ and a′) from the tricuspid annulus at the RV free wall (p < 0.0001 for each), however, there was no difference regarding e′/a′ ratio (p = 0.203). E/e′ ratio was highest in patients with grade 1 collaterals 5.85 ± 0.57 versus 4.81 ± 0.73 and 3.37 ± 0.53 in grades 2 and 3 respectively (p < 0.0001).
Discussion
Echocardiographic assessment of the right side of the heart is gaining importance in current clinical practice and research with guidelines recently published specifically to address this purpose [1]. This is because of growing evidence of its effects on clinical outcome, morbidity and mortality of several cardiac conditions [14, 15]. CTO-PCI has been gaining momentum in recent years with success rates in experienced centers reaching up to 85 %, without an increased risk of complications compared with non-CTO-PCI. Evidence from observational studies suggests that the beneficial effects of CTO-PCI will finally be extended by evidence from adequately powered, randomized, controlled trials which are currently ongoing [5, 6].
This study aimed to assess RV functions in patients with CTO of the proximal RCA (who may or may not have developed an inferior wall MI > 3 months prior to presentation) and correlating them with angiographic coronary collateral grades and clinical findings.
The main findings of this study were that patients with evidence suggestive of old inferior wall MI had significant impairment of RV systolic function (manifested by reduction of TAPSE, RVFAC and increased Doppler MPI) in comparison to those with no evidence of old inferior wall MI. There was also evidence suggestive of RV diastolic dysfunction manifested by elevated trans-tricuspid E/A and E/e′ ratios with reduced tricuspid annular e′ and a′ velocities. It was also shown that poorly developed coronary collaterals (namely grade 1) were associated with impaired RV systolic function and RV diastolic dysfunction. To the best of our knowledge no study previously assessed RV functions in patients with proximal RCA CTO according to coronary collateral grade.
In the current study, well-developed collaterals (Rentrop grade 3) were more common in patients considered to have no history of old inferior wall MI (n = 31, 83.8 % vs. n = 4, 17.4 %). Similar findings were reported in a study to assess frequency of myocardial infarction and its relationship to angiographic collateral flow in 170 patients with CTO. In that study, 18.8 % had multiple CTO lesions, with 66.5 % having more than one-vessel disease and RCA CTO was present in 40 % of patients. It was stated that the frequency of pathological Q waves on ECG was significantly lower in patients with well-developed collaterals in comparison with patients with poorly developed collaterals [16].
In the current study, patients with a history of old inferior wall MI had more impaired RV systolic functions this is similar to findings of a study done on 71 patients with old MI in comparison to 45 healthy controls that showed TAPSE and Doppler MPI of the RV to be significantly reduced in the old MI group in comparison to controls [17]. Similar results were demonstrated in an experimental study on mice, where acute MI involving the LV and sparing the RV induced a significant acute decline in RV systolic function after 1 week in the absence of pulmonary hypertension (manifested by significantly reduced RVFAC and TAPSE) [18].
Interestingly previous studies have shown that RVFAC and TAPSE show no improvement after successful PCI of single-vessel RCA CTO [19] or PCI of a collateral supplying left coronary artery in patients with RCA CTO [20].
Regarding the value of good coronary collaterals, a myocardial perfusion SPECT study on 56 patients with a single vessel CTO having a mixed coronary anatomy (with RCA CTO present in 42.8 %) has shown that in the setting of single vessel CTO and no prior MI, coronary collaterals appear to protect against resting perfusion defects and that excellent angiographic collaterals may prevent resting regional wall motion abnormalities but do not appear to protect against stress-induced perfusion defects [21]. In addition, myocardial segments supplied by CTO with well-developed collaterals are less prone to inducible ischemia, have better systolic function, and are less likely to undergo myocardial infarction, in comparison to those supplied by CTO with poor collateral circulation as assessed by cardiac magnetic resonance imaging [22]. It has also been shown that the frequency of myocardial infarction in territories supplied by CTO is significantly higher than generally recognized and that the degree of myocardial injury downstream CTO is inversely correlated with the degree of angiographic collaterals [16].
In the current study, Doppler MPI showed a strong negative correlation with other measures of RV systolic function (namely TAPSE, RVFAC, and tricuspid annular S′). Previous studies have shown good correlations between RVEF measured by thermodilution and each of TAPSE (r = 0.62, p < 0.0001) and RVFAC (r = 0.69, p < 0.0001) [23].
Study limitations
Limitations of the current study are that it comes from a single medical center with a relatively small number of patients, however, we argue that such selected patients are hard to come by. Follow-up of the patients after attempted revascularization of the RCA was not performed which is especially necessary in the group with poorly developed coronary collaterals who had more impairment of RV functions in order to identify possible improvement of RV functions which would help direct the management strategy for such patients (conservative versus invasive). Furthermore, applying emerging echocardiographic techniques to the RV such as strain of the RV free wall and global longitudinal strain of the RV should be considered in future studies to add more insight into changes affecting RV function.
Conclusions
Patients with proximal RCA CTOs and evidence of old inferior wall MI have significant impairment of RV systolic and diastolic functions in addition to poorly developed coronary collaterals in comparison to those with no evidence of old inferior wall MI. In general, patients with proximal RCA CTOs and well-developed coronary collaterals have better RV functions.
References
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39
Zornoff LA, Skali H, Pfeffer MA, St John SM, Rouleau JL, Lamas GA et al (2002) Right ventricular dysfunction and risk of heart failure and mortality after myocardial infarction. J Am Coll Cardiol 39:1450–1455
Ferlinz J (1982) Right ventricular function in adult cardiovascular disease. Prog Cardiovasc Dis 25:225–267
Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S et al (2012) Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol 59:991–997
Hoebers LP, Claessen BE, Dangas GD, Råmunddal T, Mehran R, Henriques JP (2014) Contemporary overview and clinical perspectives of chronic total occlusions. Nat Rev Cardiol 11:458–469
Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S et al (2005) Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: Part I. Circulation 112:2364–2372
Hoye A (2012) Management of chronic total occlusion by percutaneous coronary intervention. Heart 98:822–828
Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K et al (2005) The SYNTAX score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1:219–227
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD et al (2012) Joint ESC/ACCF/AHA/WHF task force for the universal definition of myocardial infarction. Third universal definition of myocardial infarction. Circulation 126:2020–2035
Kwong RY, Sattar H, Wu H, Vorobiof G, Gandla V, Steel K et al (2008) Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation 118:1011–1020
Campeau L (1976) Grading of angina pectoris. Circulation 54:522–523
Rentrop KP, Cohen M, Blanke H, Phillips R (1985) Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J Am Coll Cardiol 5:587–592
de Groote P, Millaire A, Foucher-Hossein C, Nugue O, Marchandise X, Ducloux G et al (1998) Right ventricular ejection fraction is an independent predictor of survival in patients with moderate heart failure. J Am Coll Cardiol 32:948–954
Bleeker GB, Steendijk P, Holman ER, Yu CM, Breithardt OA, Kaandorp TA et al (2006) Assessing right ventricular function: the role of echocardiography and complementary technologies. Heart 92:19–26
Choi JH, Chang SA, Choi JO, Song YB, Hahn JY, Choi SH et al (2013) Frequency of myocardial infarction and its relationship to angiographic collateral flow in territories supplied by chronically occluded coronary arteries. Circulation 127:703–709
Konishi K, Dohi K, Tanimura M, Sato Y, Watanabe K, Sugiurae E et al (2013) Quantifying longitudinal right ventricular dysfunction in patients with old myocardial infarction by using speckle-tracking strain echocardiography. Cardiovasc Ultrasound 11:23
Toldo S, Bogaard HJ, Van Tassell BW, Mezzaroma E, Seropian I, Robati R et al (2011) Right ventricular dysfunction following acute myocardial infarction in the absence of pulmonary hypertension in the mouse. PLoS One 6:e18102
Ozkan B, Urumdas Y, Alici G, Acar G, Alizade E, Kalkan ME et al (2013) Echocardiographic evaluation of right ventricular functions after successful percutaneous recanalization of right coronary artery chronic total occlusions. Eur Rev Med Pharmacol Sci 17:917–922
Acar G, Aksakal A, Ozkan B, Alici G, Alizade E, Bulut M et al (2012) Early effect of left coronary system revascularization on right ventricular mechanics in patients with right coronary artery chronic total occlusion. Acta Cardiol 67:707–712
Aboul-Enein F, Kar S, Hayes SW, Sciammarella M, Abidov A, Makkar R et al (2004) Influence of angiographic collateral circulation on myocardial perfusion in patients with chronic total occlusion of a single coronary artery and no prior myocardial infarction. J Nucl Med 45:950–955
Małek ŁA, Śpiewak M, Kłopotowski M, Marczak M, Witkowski A (2015) Combined analysis of myocardial function, viability, and stress perfusion in patients with chronic total occlusion in relation to collateral flow. Kardiol Pol 73:909–915
Ghio S, Recusani F, Klersy C, Sebastiani R, Laudisa ML, Campana C et al (2000) Prognostic usefulness of the tricuspid annular plane systolic excursion in patients with congestive heart failure secondary to idiopathic or ischemic dilated cardiomyopathy. Am J Cardiol 85:837–842
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Missiri, A.M.E., Guindy, R.R. Echocardiographic assessment of right ventricular functions in patients with proximal right coronary artery chronic total occlusion. Int J Cardiovasc Imaging 32, 895–903 (2016). https://doi.org/10.1007/s10554-016-0850-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-016-0850-z