Abstract
Regional right ventricular (RV) dysfunction (RRVD) is an echocardiographic feature in acute pulmonary embolism (PE), primarily reported in patients with moderate-to-severe RV dysfunction. This study investigated the clinical importance of RRVD by assessing its relationship with clot burden and biomarkers. We identified consecutive patients admitted to the emergency department between 1999 and 2014 who underwent computed tomographic angiography, echocardiography, and biomarker testing (troponin and NT-proBNP) for suspected acute PE. RRVD was defined as normal excursion of the apex contrasting with hypokinesis of the mid-free wall segment. RV assessment included measurements of ventricular dimensions, fractional area change, free-wall longitudinal strain and tricuspid annular plane systolic excursion. Clot burden was assessed using the modified Miller score. Of 82 patients identified, 51 had acute PE (mean age 66 ± 17 years, 43 % male). No patient had RV myocardial infarction. RRVD was present in 41 % of PEs and absent in all patients without PE. Among patients with PE, 86 % of patients with RRVD had central or multi-lobar PE. Patients with RRVD had higher prevalence of moderate-to-severe RV dilation (81 vs. 30 %, p < 0.01) and dysfunction (86 vs. 23 %, p < 0.01). There was a strong trend for higher troponin level in PE patients with RRVD (38 vs. 13 % in PE patients without RRVD, p = 0.08), while there was no significant difference for NT-proBNP (67 vs. 73 %, p = 0.88). RRVD showed good concordance between readers (87 %). RRVD is associated with an increased clot burden in acute PE and is more prevalent among patients with moderate-to-severe RV enlargement and dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A regional pattern of right ventricular (RV) dysfunction (RRVD) is a recognized echocardiographic finding in patients with acute pulmonary embolism (PE), first described in 1996 [1] and later termed “McConnell sign” by Goldhaber [2]. This finding, characterized by normal excursion of the apex contrasting with hypokinesis of the mid-free wall segment, was shown to display high specificity for PE diagnosis in a population of patients with moderate-to-severe RV systolic dysfunction [1]. Several hypotheses have been proposed for the RRVD in acute PE, including tethering of the RV apex to a normal or hypercontractile left ventricle (LV), spherical change in RV shape in order to equalize regional wall stress in response to the acute increase in afterload, and localized ischemia of the RV free wall secondary to increased wall stress [1, 3, 4].
Although RRVD in acute PE was described almost two decades ago, several questions remain unanswered. For example, it is unknown whether RRVD is observed in patients with low embolic burden or mild RV dysfunction. In addition, the relationship between RRVD in acute PE and the degree of troponin elevation is not fully defined. Establishing this relationship can help guide the evaluation of the RV in acute PE. Lastly, the inter-reader agreement for qualitative evaluation of RRVD is not well known.
In this retrospective study, we addressed these questions by analyzing echocardiograms of consecutive patients admitted to the Stanford Hospital within the past 15 years, with a suspicion of acute PE and who had undergone both computed tomography angiography (CTA) and echocardiography within 48 h of each other, as well as cardiac biomarkers (troponin and NT-proBNP). The overall objective of the study was to clarify the functional and clinical implications of RRVD in the setting of acute PE.
Methods
Study population
After acceptance by the Stanford University Institutional Review Board, we screened the Stanford Translational Research Integrated Database Environment (STRIDE) for all consecutive patients (aged ≥18 years) evaluated in the Emergency Department of Stanford University Medical Center (CA, USA) between 1999 and 2014, in whom a computed tomographic angiography (CTA) for suspicion of PE was obtained. In addition, patients had to have an echocardiogram performed within 2 days of CTA, as well as biomarkers (troponin Ic and NT-proBNP), due to clinical suspicion for acute PE (Fig. 1). We excluded patients in whom echocardiographic image quality precluded RV assessment. Because we were interested in clarifying RRVD relation to RV dilation and dysfunction severity, we also chose to exclude patients with previously known pulmonary hypertension (PH), congenital heart disease (CHD) or systolic dysfunction (defined by a left ventricular ejection fraction LVEF lower than 45 %), which could all be confounders.
To understand the prevalence of RRVD in other patient groups, we also studied a cohort of patients with idiopathic pulmonary arterial hypertension (PAH), advanced lung diseases (ALD, such as GOLD 3 or 4 stages of chronic obstructive pulmonary disease COPD or interstitial lung disease) and non-ischemic dilated cardiomyopathy (DCM). Patients were randomly selected from the respective Stanford Pulmonary Hypertension, Advanced Lung Disease and Heart Failure Clinics. Presence of RRVD was determined in these three additional patient groups.
This study was conducted in agreement with the Helsinki-II declaration; all subjects gave their informed consent prior to their inclusion in the study.
Computed-tomographic angiography
CTAs for PE diagnosis were performed on either a LightSpeed VCT 64 Slice (GE Healthcare, Waukesha, WI, USA) or a Somaton 128 Slice Dual Source (Siemens, Erlangen, Germany) CT scanner, using 80–100 mL intravenous injection of Isovue-370 or Omnipaque-300 contrast. Radiation exposure ranged from 7 to 10 mSv, with a dose-length product of 300–550 mGy/cm. Up to 5 mm contiguous axial images were reconstructed and reviewed using a picture archiving and communication system workstation (Centricity, GE Healthcare, Waukesha, WI, USA). Pulmonary embolism was defined by the presence of partial or complete filling defects in the arterial pulmonary vessels. The embolic burden was classified based on the most proximal pulmonary artery branch in which a thrombus was visualized as follows: central, lobar, segmental or sub-segmental. Multi-lobar PE was defined as ≥2 lobes involved. Clot burden was then semi-quantified according to the modified Miller score (ranging from 0 to 16 the highest burden) assessing the presence of obstruction or filling defect in the pulmonary arterial vessels. A pre-defined score of ≥10 was used as the threshold for high clot burden, as previously validated by Bankier et al. [5].
Echocardiography
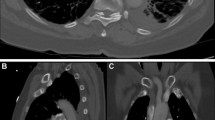
Resting trans-thoracic echocardiograms were performed using a Philips 7500 or iE33 ultrasound system (Philips Medical Systems, Andover, MA, USA) with 5 MHz transducers. End-diastolic measurements were performed in the frame coinciding with the peak of the QRS while end-systole was defined as the smallest visualized RV volume [6]. RRVD was defined as “present” in the case of clear visualization of a normal or increased contraction of the apex contrasting with hypokinesis or akinesis of the mid RV free-wall (Fig. 2a). RV size was measured as the RV maximal transverse diameter relative to the LV diameter in end-diastole. The following functional parameters were measured according to the American Society of Echocardiography recommendations [7]: RV fractional area change (RVFAC), tricuspid annular plane systolic excursion (TAPSE), and RV free-wall (or lateral) longitudinal strain (RVLS). The RVLS was traced as the difference in the length of the RV free wall between end-systole (L1) and end-diastole (L0) divided by L0 [8], as shown in Fig. 2b. For classification purposes, we used the following predefined thresholds [7, 9]: (1) RV size was classified as normal if RV/LV diameter ratio was <0.67, mildly dilated if between 0.67 and <1.0, moderately dilated if between 1.0 and <1.5 and severely dilated if ≥1.5, (2) RVLS was classified as normal if the absolute value was ≥25 %, mildly reduced if 24–20 %, moderately reduced if 19–17 % and severely reduced if <17 %, (3) RVFAC was classified as normal if ≥35 %, mildly reduced if 25–34 %, moderately if 15–24 % and severely reduced if <15 %, (4) normal TAPSE was ≥1.6 cm, and defined as moderately-to-severely altered if <1.2 cm. RVLS threshold was defined as ≤−25 % according to previous guidelines current at the beginning of our study and based on our center’s normative values for manual strain. The latest guidelines propose a threshold of −20 %, acknowledging however that automatic strain assessment is vendor-dependent and so are normative values [9]. RV systolic pressure (RVSP) was estimated from the maximal RV-to-right atrial pressure gradient added to the right atrial pressure (RAP) estimated from the inferior vena cava size and collapsibility following a quick inspiration [7].
End-diastolic and end-systolic apical four-chamber views of regional RV dysfunction in a patient with acute PE (a) and the manual tracing technique for quantifying mid-free-wall RV longitudinal Lagrangian strain (b). a The regional RV dysfunction (asterisk and arrow) is characterized by a normal excursion of the RV apex contrasting with the decreased excursion of the mid-free and basal segments of the RV lateral wall. b L0 (blue line) represents the RV lateral length in end-diastole and L1 (blue line) in end-systole. The tricuspid annular plane is represented by the white dashed line. PE pulmonary embolism, RV right ventricle
Cardiac biomarkers
Troponin and NT-proBNP are the two routinely used biomarkers to assess right heart consequences of PE, as recommended in the latest guidelines [10]. Blood samples were drawn from a peripheral vein. Serum N-terminal pro-brain natriuretic peptide (NT-proBNP, Roche Diagnostics, Mannheim, Germany) and troponin Ic (Siemens, Erlangen, Germany) were collected in lithium heparinized tubes. As there is no consensus on which Troponin or NT-proBNP threshold to use in PE, we chose the following laboratory normative values, which did not change during the study period (1999–2014): Troponin Ic level ≥0.3 ng/mL and NT-proBNP level ≥300 pg/mL.
Statistical analyses
Continuous data are presented as mean ± SD or median and interquartile range; qualitative variables as number and percentage. Differences were assessed using a Student’s t test if normally distributed or Mann–Whitney test otherwise, while differences between two distributions were made using a Chi square (χ2) test. Relationship between echocardiographic parameters and high clot burden (score ≥10/16) was assessed using logistic regression, and expressed as area under the ROC curve (AUC). In order to assess inter-observer reproducibility, all four-chamber views were read by two readers (one cardiologist expert in RV assessment and one board-certified cardiologist) blinded to each other and to the CTA results. Inter-observer variability for continuous variables (RVFAC and RVLS) was estimated using two-way mixed single-measure intra-class correlation coefficients (ICC), while for discrete variables (presence of a RRVD, moderate-to-severe RV dysfunction defined by RVFAC, RVLS and TAPSE) by the percentage of concordance. p values <0.05 were considered statistically significant. Statistical analyses were performed using SPSS® (version 14.0, SPSS, Inc., Chicago, IL, USA) and all the figures were made using Adobe Illustrator (version CC 2014, Adobe Systems, San Jose, CA, USA).
Results
Study population
Using STRIDE, we identified 124 patients who underwent CTA, echocardiogram and cardiac biomarkers within 2 days of each other for possible PE during the study period of 15 years, of whom 42 were excluded (main reasons being poor image quality in acute setting and low LVEF, Fig. 1).
Of the 82 patients, 51 had PE and 31 did not (controls). The groups were well-matched in terms of baseline clinical and electrocardiographic characteristics (Table 1). Although nine patients from the non-PE group had a history of deep venous thrombosis, they did not have a history of PE or significant differences compared to the other non-PE patients (p > 0.05). Mean age of the included population (n = 82) was 66 ± 17 years, and 43 % were male. Thirteen patients (16 %) were hypotensive on presentation of symptoms (systolic blood pressure <100 mmHg), of whom 5 patients (all with PE) received vasopressor support. PE patients had the following clot burden distribution: 18 (35 %) central, 8 (16 %) multi-lobar, 5 (10 %) single lobar, 5 (10 %) multiple segmental, 7 (14 %) single segmental, 4 (8 %) multiple sub-segmental, and 4 (8 %) single sub-segmental. Median modified Miller score was 9 [interquartile range 2–15]. No patient was diagnosed with right ventricular myocardial infarction (RVMI) in our population of patients investigated for suspected PE. Because of inappropriately timed lab draws, two patients in the control group were retrospectively excluded from the biomarker analysis.
Concordance between different metrics of RV dysfunction
Using TAPSE (<1.2 cm), RVFAC (<25 %) or RVLS (>−20 %), moderate-to-severe RV dysfunction was observed in 8.5, 12.2 or 43.9 % of the total population (n = 82), respectively. All patients with moderate-to-severe dysfunction by RVFAC had moderate-to-severe RVLS alteration as well.
RRVD relationship with clot burden, RV metrics and biomarkers
RRVD was observed in 21 patients (41 %), all of whom had confirmed PE on CTA. The majority of patients with RRVD (86 %) had central or multi-lobar PE, with only 3 patients having either single lobar, multiple segmental or single segmental PE. The modified Miller score was higher (15 [9–16]) in PE patients with RRVD than in PE patients without RRVD (4 [1–13]), p = 0.002.
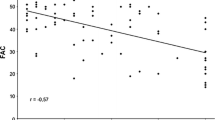
RV enlargement and overall dysfunction were common in patients with RRVD and those with greater PE clot burden (Figs. 3, 4). In patients with PE, RVLS was the only functional parameter significantly associated with a high clot burden (defined by a modified Miller score of ≥9/16): AUC = 0.69 [0.55–0.81], p = 0.03. AUCs for RVFAC and TAPSE were 0.62 [0.47–0.75], p = 0.19 and 0.64 [0.49–0.77], p = 0.11 respectively. In our non-PE control group, RV functional parameters and size metrics were also often altered (Fig. 3).
Right ventricular size and function according to presence of pulmonary embolism and regional right ventricular dysfunction. RV size was classified as normal if RV/LV diameter ratio was <0.67, mildly dilated if between 0.67 and <1.0, moderately dilated if between 1.0 and <1.5 and severely dilated if ≥1.5. RV function was assessed integrating RVFAC and TAPSE, and was classified as: normal if both RVFAC and TASPE were within the normal range; severe if both severe; and mild to moderate otherwise. RV right ventricle, RVFAC right ventricle fractional area change, TAPSE tricuspid annular plane systolic excursion. Comparisons were made using Chi square test. *All p values are <0.001
Presence of regional RV dysfunction (a) and other RV parameters (b–d) according to PE clot burden. Mod moderate, Neg negative/absent, PE pulmonary embolism, Pos positive/present, RRVD regional right ventricular dysfunction, RV right ventricle, RVFAC right ventricle fractional area change, RVLS right ventricle lateral longitudinal strain. Comparisons were made using Chi square test. *all p values are < 0.001
Although not statistically significant, troponin levels were more frequently positive in PEs with RRVD (38 %) than in PEs with no RRVD (13 %), p = 0.08; and similarly in patients with central or multi-lobar PEs (31 %) than in other PEs (16 %), p = 0.35 (Fig. 5). Median troponin level (ng/mL) was 0.1 [0.0–0.4] in PEs with RRVD versus 0.0 [0.0–0.2] in PEs with no RRVD (p = 0.09), whereas it was significantly higher in central or multi-lobar PEs (0.2 [0.0–0.7]) than in other PEs (0.0 [0.0–0.2]), p = 0.03. This trend was not observed for NT-proBNP levels (67 % versus 73 %, p = 0.88 and 65 % versus 76 %, p = 0.58 respectively). After logarithmic transformation, NT-proBNP levels (pg/mL) were not different between PEs with RRVD (3.3 [2.2–3.7]), than in PEs with no RRVD (3.1 [2.5–3.4]), p = 0.72.
Biomarker profiles according to PE clot burden and presence of regional RV dysfunction. a and b respectively display troponin and NT-proBNP levels according to presence of RRVD and PE (no patient without PE had RRVD). c and d display biomarkers levels according to clot burden. The p values displayed are for comparison between two groups using Student test and all *p values are <0.01 for Chi square tests. NT-proBNP N-terminal pro-brain natriuretic peptide, PE pulmonary embolism, RRVD regional right ventricular dysfunction, RV right ventricle
RRVD in PAH, ALD, and DCM
We randomly selected three groups of patients with DCM (n = 82, with mean LV end diastole diameter of 61.8 ± 17.5 mm), ALD (n = 82, including 62 % secondary to interstitial lung disease and 38 % to COPD, half of them having PH) and PAH (n = 82) in order to assess presence of RRVD in those conditions. Characteristics are presented in Table 2. None of the patients in the three comparison groups had evidence of RRVD on echocardiography.
Inter-observer agreement
The concordance of RRVD assessment between two readers was good (87 %), as shown in Supplemental Figure S1, with two patients in the non-PE group misclassified by the less expert reader as having RRVD. Among the other RV parameters, inter-observer variability between readers was ICC = 0.81 for RVLS and ICC = 0.64 for RVFAC. Concordance was 84 % for classifying moderate-to-severe dysfunction according to RVLS and 87 % according to RVFAC.
Discussion
The main finding of our study is that, in the clinical setting of patients investigated for suspicion of acute PE (by CTA, echocardiography and biomarkers), RRVD is mainly observed in patients with high embolic burden, enlarged right ventricles and evidence of systolic dysfunction. Moreover, there was good agreement for the visual assessment of RRVD.
RRVD was originally described in 1996 as a regional dysfunctional pattern in patients with moderate-to-severe RV systolic dysfunction [1]. After defining the sign using a “training” cohort of patients with either PE or PAH and pre-defined RV dysfunction, as well as healthy controls, McConnell and colleagues then determined a 94 % specificity of RRVD for PE using a validation cohort of patients with significant RV dysfunction from multiple causes, with normal or mild RV dysfunction being an exclusion criteria. Since then, several studies have confirmed the high specificity (ranging from 96 to 100 %) in cohorts without RVMI [11–13]. The overall sensitivity of RRVD for PE is low (<20 %), although several attempts have recently been made to increase sensitivity by combining RRVD presence with signs of RV overload pressure or disturbed RV ejection pattern [11].
In the present study, we did not aim to re-assess the diagnostic performance of RRVD (in terms of sensitivity or specificity) but instead assess its relationship with clot burden, right heart function and biomarkers. We included all consecutive patients regardless of their RV parameters, in order to be more representative of clinical practice. The non-PE control group had well-matched baseline characteristics and included patients undergoing the same investigation for clinical suspicion for PE. Consistent with prior studies, we showed that RRVD was not observed in these patients without PE. RRVD was also not found in the three additional cohorts of patients studied (PAH, ALD and DCM).
In addition, our study showed that RRVD is strongly related to clot burden and RV enlargement or dysfunction. We found that presence of RRVD is suggestive of central or multi-lobar PE, which is clinically relevant as higher embolic burden PEs are associated with increased risk for clinical deterioration and mortality [15]. The positive correlation between presence of RRVD and higher degree of clot burden found in our cohort contrasts with Lodato et al.’s results showing no clear correlation between the location of PE and the prevalence of RRVD [14]. However, in their study of 67 patients who also underwent CTA and echocardiogram within two days of each other for suspected PE, the PE subset was defined based on the location of the most proximal thrombus, without accounting for the number of lobes affected. This may underestimate clot burden, as a multi-lobar PE could be as deleterious as a central PE, and it could explain the discordance with our results. Lastly, RRVD was mainly observed in patients with moderate-to-severe RV dysfunction, which is consistent with the original paper [1].
Several studies have shown that positive biomarkers in acute PE are useful for risk stratification as they suggest RV dysfunction and worse prognosis [16, 17]. A recent review of cardiac biomarkers utility in acute PE recommended obtaining an echocardiogram only for patients with both normal blood pressure and positive biomarkers, as patients with normal biomarkers will usually have normal RV function [18]. In our study, there was a trend of more positive troponin levels in presence of RRVD and more severe PE burden, although not statistically significant probably due to the limited number of patients in each group. Moreover, we confirmed troponin levels were only mildly elevated in our population, which contrasts with elevated troponin levels expected in RVMI.
RVMI has previously been described as an etiology of RRVD [19]. In fact, Casazza et al. [20] estimated the specificity of RRVD for PE to be very low (33 %) when including RVMI patients. Although our study selection of patients referred for the three investigations (CTA, echocardiography and biomarkers) precludes a more general estimation of RRVD specificity, our 15-year study period shows that a diagnostic dilemma between acute RVMI and PE is rare, as no patient was found to have RVMI. Moreover, in our clinical experience, RVMI is typically associated with extension of the mid free-wall hypokinesis to involve the RV base, while acute PE has more preserved wall motion at the RV base compared to the mid free wall, as was found in our initial quantitative and qualitative analyses [1].
Assessment and quantification of RV size and dysfunction can be challenging, particularly in the acute setting. Recent guidelines define sub-massive PE and consequently allow fibrinolysis therapy in patients with moderate-to-severe RV dysfunction [10, 21]. However, the metrics and thresholds used to define RV dysfunction differ greatly between studies. While TAPSE appears to be the easiest parameter to measure, it can be falsely low in patients who have undergone cardiac surgery [22]. RVFAC is a commonly used visual metric, but it can be challenging to obtain in the acute setting. Recently, RVLS has emerged as a useful metric in acute PE. Indeed, two studies used myocardial deformation imaging by speckle tracking in patients with RRVD related to PE in order to understand better the regional pattern of RRVD. One report showed RV strain was altered at the free-wall level, mid- and basal septum levels compared to healthy controls [12] while another quantified those reversible regional alterations [23]. López-Candales et al. [13] further showed that the RV apex function is actually not spared in RRVD and the apical hyperkinesis is thus thought to be the consequence of RV apex tethering by the LV. Overall, our study highlights that specifying which of the above criteria is used has important consequences since concordance between them is not perfect. It is important to recognize that choosing different parameters to define RV dysfunction can have clinically meaningful implications, such as allowing fibrinolysis in sub-massive PE. Further investigations are needed in order to better define which RV functional parameters should be used in PE patients.
Limitations
The main limitation of our study comes from the patient selection. As our aim was to provide a multi-modal evaluation of RRVD, we only selected patients who underwent all investigations within 48 h of each other. Because of this specific selection, we cannot draw broader conclusions about the diagnostic performance of echocardiography in acute PE. However, although highly selected, our population displayed a wide range of clot burden, RV size and function. Moreover, the PE group and the non-PE group were found to be well-matched.
Conclusion
RRVD is a visually simple, reproducible echocardiographic parameter that is associated with increased clot burden and right ventricular dysfunction in patients with acute PE.
References
McConnell MV, Solomon SD, Rayan ME, Come PC, Goldhaber SZ, Lee RT (1996) Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol 78:469–473
Goldhaber SZ (1998) Pulmonary embolism. N Engl J Med 339:93–104
Sosland RP, Gupta K (2008) Images in cardiovascular medicine: McConnell’s Sign. Circulation 118:e517–e518
Torrent Guasp F (2001) Agonist-antagonist mechanics of the descendent and ascendent segments of the ventricular myocardial band. Rev Esp Cardiol 54:1091–1102
Bankier AA, Janata K, Fleischmann D, Kreuzer S, Mallek R, Frossard M et al (1997) Severity assessment of acute pulmonary embolism with spiral CT: evaluation of two modified angiographic scores and comparison with clinical data. J Thorac Imaging 12:150–158
Voigt J-U, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F et al (2010) Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 23:351–369
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39
Konstantinides SV, Torbicki A, Agnelli G, Danchin N, Fitzmaurice D, Galiè N et al (2014) 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J 35:3033–3069
Kurzyna M, Torbicki A, Pruszczyk P, Burakowska B, Fijałkowska A, Kober J et al (2002) Disturbed right ventricular ejection pattern as a new Doppler echocardiographic sign of acute pulmonary embolism. Am J Cardiol 90:507–511
Platz E, Hassanein AH, Shah A, Goldhaber SZ, Solomon SD (2012) Regional right ventricular strain pattern in patients with acute pulmonary embolism. Echocardiography 29:464–470
López-Candales A, Edelman K, Candales MD (2010) Right ventricular apical contractility in acute pulmonary embolism: the McConnell sign revisited. Echocardiography 27:614–620
Lodato JA, Ward RP, Lang R (2008) Echocardiographic predictors of pulmonary embolism in patients referred for helical CT. Echocardiography 25:584–590
Vedovati M, Becattini C, Agnelli G, Kamphuisen P, Masotti L, Pruszczyk P et al (2012) Multidetector CT scan for acute pulmonary embolism: embolic burden and clinical outcome. Chest 142:1417–1424
Pruszczyk P, Kostrubiec M, Bochowicz A, Styczyński G, Szulc M, Kurzyna M et al (2003) N-terminal pro-brain natriuretic peptide in patients with acute pulmonary embolism. Eur Respir J 22:649–653
Becattini C, Vedovati MC, Agnelli G (2007) Prognostic value of troponins in acute pulmonary embolism: a meta-analysis. Circulation 116:427–433
Kucher N, Goldhaber SZ (2003) Cardiac biomarkers for risk stratification of patients with acute pulmonary embolism. Circulation 108:2191–2194
Shah P, Schleifer JW, Mookadam F, Chandrasekaran K (2015) Right ventricular myocardial infarction: an underrecognized aetiology of McConnell’s sign. Eur Heart J Cardiovasc Imaging 16:225
Casazza F, Bongarzoni A, Capozi A, Agostoni O (2005) Regional right ventricular dysfunction in acute pulmonary embolism and right ventricular infarction. Eur J Echocardiogr 6:11–14
Jaff MR, McMurtry MS, Archer SL, Cushman M, Goldenberg N, Goldhaber SZ et al (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation 123:1788–1830
Raina A, Vaidya A, Gertz ZM, Chambers S, Forfia PR (2013) Marked changes in right ventricular contractile pattern after cardiothoracic surgery: implications for post-surgical assessment of right ventricular function. J Heart Lung Transplant 32:777–783
Sugiura E, Dohi K, Onishi K, Takamura T, Tsuji A, Ota S et al (2009) Reversible right ventricular regional non-uniformity quantified by speckle-tracking strain imaging in patients with acute pulmonary thromboembolism. J Am Soc Echocardiogr 22:1353–1359
Acknowledgments
M.A. received a research fellowship from the Fédération Française de Cardiologie. M.V.M. receives MRI research support from GE Healthcare. None of the other authors have any conflicts of interest relative to the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This research involves human participants. All participants gave their informed consent before inclusion.
Conflict of interest
None of the authors have any conflicts of interest.
Additional information
Mirela Tuzovic, Sasikanth Adigopula and Myriam Amsallem have contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure S1:
Inter-observer agreement of the regional RV dysfunction between level 3 and level 2 readers. (+): Regional RV dysfunction (RRVD) classified as present/(−): RRVD classified as absent. L2 represents level 2 reader and L3 level 3. (TIFF 968 kb)
Rights and permissions
About this article
Cite this article
Tuzovic, M., Adigopula, S., Amsallem, M. et al. Regional right ventricular dysfunction in acute pulmonary embolism: relationship with clot burden and biomarker profile. Int J Cardiovasc Imaging 32, 389–398 (2016). https://doi.org/10.1007/s10554-015-0780-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0780-1