Abstract
N-terminal pro-B-type natriuretic peptide (NT-proBNP) and cardiac troponins (cTns) measured with sensitive assays provide strong prognostic information in patients with stable coronary artery disease. However, the relationship between these biomarkers and myocardial contractile function, as well as infarct size, in this patient group, remains to be defined. The study population consisted of 160 patients referred to a follow-up echocardiography scheduled 1 year after coronary revascularization. Concentrations of NT-proBNP, high-sensitive cTnT (hs-cTnT) and sensitive cTnI assays were assessed. Left ventricular function was measured as global peak systolic longitudinal strain by speckle tracking echocardiography and infarct size was assessed by late-enhancement MRI. NT-proBNP and sensitive cTnI levels were significantly associated with left ventricular function by peak systolic strain (R-values 0.243 and 0.228, p = 0.002 and 0.004) as well as infarct size (R-values 0.343 and 0.366, p = 0.014 and p = 0.008). In contrast, hs-cTnT did not correlate with left ventricular function (R = 0.095, p = 0.231) and only marginally with infarct size (R = 0.237, p = 0.094). NT-proBNP and sensitive cTnI levels correlate with left ventricular function and infarct size in patients with stable coronary artery disease after revascularization. As opposed to hs-cTnT, NT-proBNP and cTnI seem to be indicators of incipient myocardial dysfunction and the extent of myocardial necrosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary artery disease (CAD) represents the most common chronic, life-threatening disease in developed countries [1]. Stable CAD may progress to an acute coronary syndrome and, despite recent therapeutic advances, potentially lead to heart failure or death. Serious efforts have been made to search for molecules that may contribute to better identify patients at risk for CAD and few biomarkers have already been identified as reliable and useful tools in medical decision making, such as cardiac troponin (cTn) [2] and N-terminal pro-B-type natriuretic peptide (NT-proBNP) [3]. cTns have traditionally been considered diagnostic markers of myocardial necrosis [4] and indicators of the risk of early recurrent ischemic events [5], but observations that very low levels of cTn are found circulating in patients with stable CAD [6, 7] and even in the general population [8], have challenged this paradigm. However, the development of high-sensitivity troponin (hs-cTn) assays allows accurate measurement over the lower range of cTn concentrations, and levels well below the limit of detection of previous assays have shown to be significantly associated with the incidence of cardiovascular death in patients with stable CAD. Furthermore, NT-proBNP is a strong and independent prognostic marker in patients with stable CAD and is particularly closely related to incidence of death and heart failure [3, 9–11].
NT-proBNP is known to be associated with the degree of left ventricular (LV) dysfunction [9], while chronic low-grade cTnT elevation has been linked to the risk of heart failure development [6]. However, the relationship between these biomarkers and LV function as assessed by speckle tracking echocardiography (2D-STE) in patients with stable CAD has not been evaluated. 2D-STE is established as an accurate method for assessing LV function [12, 13] and has demonstrated to be superior to LV ejection fraction (LVEF) as a means for detecting subclinical myocardial dysfunction [14]. Recent studies have documented the prognostic value of global longitudinal systolic strain by 2D-STE [15–17].
In the present study, we hypothesised that both NT-proBNP and cTns, determined by sensitive assays, are associated with LV function as measured by 2D-STE and with MRI-determined infarct size in patients with stable CAD.
Materials and methods
Patients
This study was conducted in a single tertiary coronary care centre, using a prospective design. The study population consisted of 160 patients referred to a follow-up echocardiography scheduled 1 year after coronary revascularization. Significant CAD was defined as ≥50 % diameter stenosis in any coronary artery. Exclusion criteria were valvular disease, atrial fibrillation, left bundle branch block with QRS > 120 ms, and recurrent angina or cardiovascular (CV) events after the coronary revascularization.
The study complies with the Declaration of Helsinki and was approved by the Regional Committee for Medical Research (REK South, Oslo, Norway). All subjects gave written informed consent.
Biochemical analyses
Venous blood was collected at the same day as the echocardiographic recordings, approximately 1 year after revascularization. After centrifugation, serum aliquots were frozen and stored at −70 °C until determination of two cTn assays and NT-proBNP. The analytical characteristics of the assays were supplied by the manufacturers. The Siemens cTnI Ultra assay was analyzed with the use of the ADVIA Centaur immunoassay system (Siemens®, Germany), with a detection limit of 6 ng/L, a 99th-percentile cutoff of 40 ng/L, and a coefficient of variation of <10 % at 30 ng/L. The Roche hs-cTnT and NT-proBNP assays were both performed on a Modular E170 platform, using the Elecsys reagents (Roche Diagnostics, Basel, Switzerland). Hs-cTnT had a detection limit of 2 ng/L, a 99th-percentile cutoff of 14 ng/L, and a coefficient of variation of <10 % at 13 ng/L. NT-proBNP had a detection limit of 5 ng/L, and a 97.5th-percentile cutoff of 263 ng/L for those of age 55–64. The interassay coefficient of variation was 4.5 % at a concentration of 21 ng/L and 2.2 % at a concentration of 9.12 ng/L. The median values and the number of patients at or above the limit of detection and at or above the 99th percentile for apparently healthy subjects of the respective biomarkers are shown in Table 1. Levels below the limit of detection were considered as zero.
Kits for determination of high-sensitive cTnT and NT-proBNP and Siemens cTnI Ultra assay kit were donated by Roche Diagnostics and Siemens Healthcare Diagnostics, respectively. The companies played no role in the study conception or design, the analysis of the data, or the preparation of the manuscript.
Echocardiographic analysis
A Vivid 7 ultrasound scanner (GE Vingmed Ultrasound, Horten, Norway) was used to record two-dimensional grey-scale images and strain by STE. Recordings were done in the three standard apical planes (4-chamber, 2-chamber and long-axis). Loops were digitally stored and later analyzed off-line using EchoPac version 7 (GE Vingmed, Horten, Norway).
LV volumes were traced manually at end-diastole and end-systole at apical 4- and 2-chamber views, and LVEF was derived from modified biplane Simpson’s method.
Strain analyses
Longitudinal strain was measured by 2D-STE using a 16 LV-segment model [18]. In each of the LV apical planes, the endocardial border was marked manually and tracking of deformation was automatically performed by the software. The average frame rate was 69 ± 12 frames/s. For each segment, the peak negative systolic strain value, representing maximum segmental systolic contraction, was recorded. Values for all analyzed segments were then averaged to obtain global strain. An example of the technique is shown in Fig. 1. End-systole was defined by aortic valve closure in the apical long-axis view. No patients were excluded due to suboptimal image quality on echocardiography. Myocardial strain could be assessed in 94 % of the myocardial segments. All echocardiographic analyses, including strain analyses, were performed separately and blinded to all other patient data.
Left ventricular longitudinal strain measured by speckle tracking echocardiography from a 4-chamber view and delayed contrast-enhanced MRI in the left ventricular short axis projection from a patient with a previous history of myocardial infarction 1 year after revascularisation. The arrows point towards hyperenhanced regions, appearing white on MRI. Strain is reduced compared with healthy individuals, while the levels of N-terminal pro-B-type natriuretic peptide and cardiac troponin I are increased
Cardiac magnetic resonance imaging
Gadolinium contrast-enhanced cardiac MRI (CE-MRI) was performed in 51 patients referred to Oslo University Hospital, Rikshospitalet 1 year earlier with a clinical diagnosis of MI confirmed by ECG and elevated troponin I or troponin T above the 99 % percentile. The CE-MRI was done immediately after the echocardiography, using either a 1.5-T (Magnetom Sonata, Siemens, Erlangen, Germany) or a 3-T (Philips Medical Systems, Best, The Netherlands). Breath-hold cine images were acquired in short and long axis views. Late enhancement images were obtained 10–20 min after intravenous injection of 0.2 mmol/kg gadopentetate dimeglumine (Magnevist, Schering, Berlin, Germany) in multiple short-axis slices covering the entire LV (Fig. 1). On each short-axis image, total myocardial area as well as area of infarcted myocardium was manually drawn (PACS, Sectra, Sweden). Infarct size was calculated as infarct volume as a percentage of total myocardial volume. Transmurality was calculated in a 16 LV-segment model as infarct volume divided by myocardial volume per segment, and segments with ≥50 % contrast-enhancement were judged to have transmural infarction [19].
Coronary angiography and revascularization
Coronary angiography was performed on clinical indication by standard (Judkins) technique 1 year before the echocardiographic examinations. 117 of the patients had a clinical diagnosis of acute coronary syndrome and underwent planned coronary angiography within 3 days of index admission. The remaining patients were referred to elective diagnostic coronary angiography because of stable chest pain. Percutaneus coronary intervention (PCI) was performed at the discretion of the operator. Single-vessel disease was found in 82 (51 %) of the patients, whereas 78 (49 %) had coronary disease in ≥2 vessels. Coronary occlusion was found in 34 (21 %) of the patients. PCI was performed in 126 (79 %) of the patients, whereas 114 patients (21 %) underwent coronary artery bypass grafting.
Statistical analysis
Continuous variables with a normal distribution are expressed as means with standard deviation (SD). Variables with a skewed distribution are given as medians with inter-quartile range (IQR), and categorical variables as numbers and percentages. Differences in continuous variables between quartiles of biomarker levels were tested using Kruskal–Wallis and Mann–Whitney test with Bonferroni correction. The correlations between biomarker levels and LV function/infarct size were estimated by Spearman correlation.
All p values are 2-tailed, and a significance level of 0.05 was used. All statistical analyses were performed on SPSS version 16.0 (SPSS Inc. Chicago, IL).
Results
Clinical data of the 160 patients are presented in Table 2. There were 42 females and 118 males. All patients had stable CAD. Most of the patients were on beta-blockers, lipid-lowering drugs, and aspirin or other antiplatelet medication.
Table 1 shows the median values and the number of patients at or above the limit of detection and at or above the 99th percentile for apparently healthy subjects of the respective biomarkers. LV function was reduced, with a mean peak systolic strain of −17.6 ± 2.4 % [14].
Infarct size and transmurality by CE-MRI
Mean infarct size was 8.0 ± 8.6 % of the total LV myocardial volume. Mean LVEF, as determined by MRI, was 63 ± 9 %. Evidence of myocardial infarction was seen in 40 (78 %) of the patients undergoing CE-MRI. Of these, 20 (50 %) demonstrated transmural infarction.
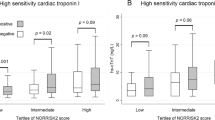
Biomarkers and left ventricular function
Calculation of 25th, 50th, and 75th percentiles was done to divide data into quartiles. The medians of peak systolic strain were significantly different across the quartiles of NT-proBNP (p = 0.007) and sensitive cTnI (p = 0.013) (Table 3). Correspondingly, patients in the highest quartile had significantly reduced contractile function compared to subjects in the two lowest quartiles of both NT-proBNP and sensitive cTnI (p < 0.001 and p = 0.012). However, there were no differences between the medians of peak systolic strain across the quartiles of hs-cTnT (p = 0.494) (Table 3).
Both NT-proBNP and sensitive cTnI correlated significantly with peak systolic strain (Table 4), while there was no significant association between strain and hs-cTnT (Table 4). There were no correlations between the respective biomarkers and LVEF (Table 4).
Biomarkers and infarct size
Both NT-proBNP and sensitive cTnI levels were significantly associated with infarct size (Table 4), whereas hs-cTnT did not correlate with the extent of myocardial necrosis as assessed by CE-MRI (Table 4).
Discussion
The results of the present study extend currently available information about the value of NT-proBNP and cTns measured by contemporary, sensitive assays in patients with stable CAD. The main findings can be summarized as follows: (1) both NT-proBNP and sensitive cTnI are independently related to myocardial systolic function; (2) levels of NT-proBNP and sensitive cTnI are associated with the extent of myocardial necrosis as assessed by CE-MRI; (3) hs-cTnT did not correlate neither with systolic function nor with the extent of myocardial necrosis.
Biomarkers and left ventricular function
Both NT-proBNP and sensitive cTnI were significant indicators of myocardial contractile function. We used global longitudinal strain to estimate LV systolic function. Global peak systolic longitudinal strain has been validated as a measure of LV systolic function [20], and has proven superiority to LVEF for prediction of all cause mortality [21, 22]. Global longitudinal strain has also been shown to be superior to LVEF for prediction of infarct size in chronic ischaemic heart disease [23] and for prediction of ventricular arrhythmias in patients after myocardial infarction [24]. The relationship between the different biomarkers and myocardial strain was statistically significant, but weak. However, this findings suggest that a single blood test may aid identify threshold concentrations of biomarkers that indicate reduced myocardial systolic function in patients with stable CAD. 92 % of the patients in our study appeared to have normal systolic function, as assessed by LVEF. Consequently, the elevated biomarker levels in this study seems to reflect unrecognized LV remodelling that is detectable only by more sensitive and accurate methods, such as 2D-STE, and may be useful for long-term risk assessment of the patients with stable CAD. The present study could not show significant correlations between the different biomarkers and LVEF.
Biomarkers and infarct size
The levels of sensitive cTnI and NT-proBNP in patients with stable CAD were significantly related to infarct size, as assessed by CE-MRI. These findings on NT-proBNP are in keeping with a recent report [25]. They found that NT-proBNP levels 3 months after ST-segment-elevation myocardial infarction were strongly associated with infarct size. However, this is the first study relating sensitive cTnI to infarct size in patients with stable CAD. The levels of hs-cTnT were not significantly related to infarct size.
Discrepancy among the cTn assays
Our data suggest that measurements of sensitive cTnI are better indicators of LV function compared with hs-cTnT. Previous studies, investigating the role of the sensitive cTn assays in patients with stable CAD, have concentrated mainly on hs-cTnT [6, 26]. However, in a recent study assessing the prognostic value of cTnI levels in patients with stable CAD, the concentrations of cTnI and and cTnT were correlated only moderately [27]. Possible explanations for these differences remain speculative and experimental studies are needed, but different biological behaviour and analytical characteristics of cTnT and cTnI might affect the diagnostic and prognostic performance [28, 29]. The molecular weight of the two troponins are different; 24 kDa for cTnI and 38 kDa for cTnT. The physiological mechanisms responsible for the clearance of cTn from the circulation are poorly characterized, although the reticuloendothelial system has been implicated [30]. It is well known that circulating cTn can be modified by various enzymes. Such processing appears to occur more frequently with cTnI than cTnT and may affect assay results.
Clinical perspectives
Sensitive and hs-cTn assays provide a new non-invasive window to cardiac diseases [31]. However, despite the wealth of information documenting the strong prognostic merit of both NT-proBNP and hs-cTnT, most clinicians have moved slowly to incorporate NT-proBNP and sensitive cTn testing into the routine management of patients with stable CAD.
The present observations may have important implications for the clinical use of the respective biomarkers. The current study demonstrates that in patients with stable CAD, NT-proBNP and sensitive cTnI provide information of myocardial systolic function. Clearly, biomarkers cannot replace echocardiography as a method for assessment of LV function. However, identification of threshold concentrations of biomarkers that indicate reduced myocardial systolic function in clinically stable patients would be helpful for the clinician. In the future we will hopefully witness a much clearer delineation of the clinical indications for NT-proBNP and sensitive cTn measurements in patients with stable CAD.
Study limitations
The results of our study are limited to patients with stable CAD. Findings and results in patients with acute coronary syndrome may be different. Our patient group consists of a mixture of patients with first time angina, but also patients with old myocardial infarcts. We therefore believe that our patient group reflects common clinical practice in an outpatient clinic.
The echocardiographic examination and the blood tests were performed 1 year after coronary revascularization. Consequently, the results of this study can only be valid for patients with CAD after revascularization. Even though none of the patients reported recurrent angina, a progression of CAD might be a confounder, but a follow-up angiography was not performed for clinical reasons. Moreover, we measured NT-proBNP and sensitive cTn only once and without correction for potential variability in concentrations.
The CE-MRI study was only performed in those with earlier MI. Consequently, conclusions regarding the relationship between infarct size and biomarkers are limited to post-MI patients.
We cannot rule out the possibility that part of the observed differences may be due to analytical differences between the two assays. In this study only 35 % of the patients had Siemens cTnI values above the detection limit, while 100 % of the patients had hs-cTnT values above the detection limit. Along the same line of argument, our results cannot be extrapolated to other cTnI assays.
The number of patients included was modest compared to other studies investigating the value of cardiac biomarkers [3, 6, 9]. However, the present study is not small in number of patients compared with previous studies with echocardiography and MRI [32–34], and, most importantly, the findings in the present study were significant despite the apparent limited number of patients included. Nevertheless, a larger study is needed to determine more definitively the relationship between levels of sensitive cTn and NT-proBNP and myocardial contractile function, as well as infarct size.
2D-STE measurements have the advantage of being relatively angle independent, but are, like all echocardiographic methods, dependent on image quality.
Conclusion
In conclusion, this study demonstrates that the circulating levels of sensitive cTnI and NT-proBNP are related to LV function and infarct size in patients with stable CAD after revascularization. Our data suggest that elevated NT-proBNP and sensitive cTnI partly reflect LV remodelling that is detectable only by more sensitive and accurate imaging methods, such as 2D-STE.
References
Hemingway H, McCallum A, Shipley M, Manderbacka K, Martikainen P, Keskimaki I (2006) Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 295:1404–1411
Eggers KM, Al-Shakarchi J, Berglund L, Lindahl B, Siegbahn A, Wallentin L, Zethelius B (2013) High-sensitive cardiac troponin T and its relations to cardiovascular risk factors, morbidity, and mortality in elderly men. Am Heart J 166:541–548
Bibbins-Domingo K, Gupta R, Na B, Wu AH, Schiller NB, Whooley MA (2007) N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA 297:169–176
Hallen J (2012) Troponin for the estimation of infarct size: what have we learned? Cardiology 121:204–212
Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, Fischer GA, Fung AY, Thompson C, Wybenga D, Braunwald E (1996) Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 335:1342–1349
Omland T, de Lemos JA, Sabatine MS, Christophi CA, Rice MM, Jablonski KA, Tjora S, Domanski MJ, Gersh BJ, Rouleau JL, Pfeffer MA, Braunwald E (2009) A sensitive cardiac troponin T assay in stable coronary artery disease. N Engl J Med 361:2538–2547
Ndrepepa G, Braun S, Mehilli J, Birkmeier KA, Byrne RA, Ott I, Hosl K, Schulz S, Fusaro M, Pache J, Hausleiter J, Laugwitz KL, Massberg S, Seyfarth M, Schomig A, Kastrati A (2011) Prognostic value of sensitive troponin T in patients with stable and unstable angina and undetectable conventional troponin. Am Heart J 161:68–75
de Lemos JA, Drazner MH, Omland T, Ayers CR, Khera A, Rohatgi A, Hashim I, Berry JD, Das SR, Morrow DA, McGuire DK (2010) Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 304:2503–2512
Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R (2005) N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med 352:666–675
Ndrepepa G, Braun S, Niemoller K, Mehilli J, von Beckerath N, von Beckerath O, Vogt W, Schomig A, Kastrati A (2005) Prognostic value of N-terminal pro-brain natriuretic peptide in patients with chronic stable angina. Circulation 112:2102–2107
Gravning J, Smedsrud MK, Omland T, Eek C, Skulstad H, Aaberge L, Bendz B, Kjekshus J, Morkrid L, Edvardsen T (2013) Sensitive troponin assays and N-terminal pro-B-type natriuretic peptide in acute coronary syndrome: prediction of significant coronary lesions and long-term prognosis. Am Heart J 165:716–724
Montgomery DE, Puthumana JJ, Fox JM, Ogunyankin KO (2012) Global longitudinal strain aids the detection of non-obstructive coronary artery disease in the resting echocardiogram. Eur Heart J Cardiovasc Imaging 13:579–587
Smedsrud MK, Sarvari S, Haugaa KH, Gjesdal O, Orn S, Aaberge L, Smiseth OA, Edvardsen T (2012) Duration of myocardial early systolic lengthening predicts the presence of significant coronary artery disease. J Am Coll Cardiol 60:1086–1093
Smedsrud MK, Pettersen E, Gjesdal O, Svennevig JL, Andersen K, Ihlen H, Edvardsen T (2011) Detection of left ventricular dysfunction by global longitudinal systolic strain in patients with chronic aortic regurgitation. J Am Soc Echocardiogr 24:1253–1259
Woo JS, Kim WS, Yu TK, Ha SJ, Kim SY, Bae JH, Kim KS (2011) Prognostic value of serial global longitudinal strain measured by two-dimensional speckle tracking echocardiography in patients with ST-segment elevation myocardial infarction. Am J Cardiol 108:340–347
Sarvari SI, Gjesdal O, Gude E, Arora S, Andreassen AK, Gullestad L, Geiran O, Edvardsen T (2012) Early postoperative left ventricular function by echocardiographic strain is a predictor of 1-year mortality in heart transplant recipients. J Am Soc Echocardiogr 25:1007–1014
D’Andrea A, Cocchia R, Caso P, Riegler L, Scarafile R, Salerno G, Golia E, Di SG, Calabro P, Bigazzi MC, Liccardo B, Esposito N, Cuomo S, Bossone E, Russo MG, Calabro R (2011) Global longitudinal speckle-tracking strain is predictive of left ventricular remodeling after coronary angioplasty in patients with recent non-ST elevation myocardial infarction. Int J Cardiol 153:185–191
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542
Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM (2000) The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 343:1445–1453
Reisner SA, Lysyansky P, Agmon Y, Mutlak D, Lessick J, Friedman Z (2004) Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr 17:630–633
Stanton T, Leano R, Marwick TH (2009) Prediction of all-cause mortality from global longitudinal speckle strain: comparison with ejection fraction and wall motion scoring. Circ Cardiovasc Imaging 2:356–364
Kearney LG, Lu K, Ord M, Patel SK, Profitis K, Matalanis G, Burrell LM, Srivastava PM (2012) Global longitudinal strain is a strong independent predictor of all-cause mortality in patients with aortic stenosis. Eur Heart J Cardiovasc Imaging 13:827–833
Gjesdal O, Hopp E, Vartdal T, Lunde K, Helle-Valle T, Aakhus S, Smith HJ, Ihlen H, Edvardsen T (2007) Global longitudinal strain measured by two-dimensional speckle tracking echocardiography is closely related to myocardial infarct size in chronic ischaemic heart disease. Clin Sci (Lond) 113:287–296
Haugaa KH, Smedsrud MK, Steen T, Kongsgaard E, Loennechen JP, Skjaerpe T, Voigt JU, Willems R, Smith G, Smiseth OA, Amlie JP, Edvardsen T (2010) Mechanical dispersion assessed by myocardial strain in patients after myocardial infarction for risk prediction of ventricular arrhythmia. JACC Cardiovasc Imaging 3:247–256
Mistry N, Abdelnoor M, Seljeflot I, Hoffmann P, Bohmer E, Bjornerheim R, Kjeldsen SE, Halvorsen S (2011) Amino-terminal pro-B-type natriuretic peptide (NT-proBNP) levels 3 months after myocardial infarction are more strongly associated with magnetic resonance-determined ejection fraction than NTproBNP levels in the acute phase. J Card Fail 17:479–486
Ndrepepa G, Braun S, Schulz S, Fusaro M, Keta D, Pache J, Seyfarth M, Mehilli J, Schomig A, Kastrati A (2011) Sensitive troponin and N-terminal probrain natriuretic peptide in stable angina. Eur J Clin Investig 41:1054–1062
Omland T, Pfeffer MA, Solomon SD, de Lemos JA, Rosjo H, Saltyte BJ, Maggioni A, Domanski MJ, Rouleau JL, Sabatine MS, Braunwald E (2013) Prognostic value of cardiac troponin I measured with a highly sensitive assay in patients with stable coronary artery disease. J Am Coll Cardiol 61:1240–1249
Giannitsis E, Katus HA (2004) Comparison of cardiac troponin T and troponin I assays–implications of analytical and biochemical differences on clinical performance. Clin Lab 50:521–528
Lyck HM, Saaby L, Nybo M, Rasmussen LM, Thygesen K, Mickley H, Svenstrup PT (2012) Discordant diagnoses of acute myocardial infarction due to the different use of assays and cut-off points of cardiac troponins. Cardiology 122:225–229
Mohammed AA, Januzzi JL Jr (2010) Clinical applications of highly sensitive troponin assays. Cardiol Rev 18:12–19
Twerenbold R, Jaffe A, Reichlin T, Reiter M, Mueller C (2012) High-sensitive troponin T measurements: what do we gain and what are the challenges? Eur Heart J 33:579–586
Bruder O, Jensen C, Jochims M, Farazandeh M, Barkhausen J, Schlosser T, Sabin GV, Hunold P (2010) Relation of B-type natriuretic peptide (BNP) and infarct size as assessed by contrast-enhanced MRI. Int J Cardiol 144:53–58
Ingkanisorn WP, Rhoads KL, Aletras AH, Kellman P, Arai AE (2004) Gadolinium delayed enhancement cardiovascular magnetic resonance correlates with clinical measures of myocardial infarction. J Am Coll Cardiol 43:2253–2259
Sjoli B, Orn S, Grenne B, Ihlen H, Edvardsen T, Brunvand H (2009) Diagnostic capability and reproducibility of strain by Doppler and by speckle tracking in patients with acute myocardial infarction. JACC Cardiovasc Imaging 2:24–33
Conflict of interest
Jørgen Gravning has received lecture fees from Siemens. Torbjørn Omland has received speaker honoraria and research support from Roche Diagnostics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smedsrud, M.K., Gravning, J., Omland, T. et al. Sensitive cardiac troponins and N-terminal pro-B-type natriuretic peptide in stable coronary artery disease: correlation with left ventricular function as assessed by myocardial strain. Int J Cardiovasc Imaging 31, 967–973 (2015). https://doi.org/10.1007/s10554-015-0646-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0646-6