Abstract
To evaluate whether the extracellular volume fraction (ECV) measured using cardiac magnetic resonance (CMR) imaging can detect myocardial tissue changes in dilated cardiomyopathy (DCM) without late gadolinium enhancement (LGE). Forty-one DCM patients and 10 healthy volunteers underwent pre- and post-T1 mapping using a modified Look-Locker Inversion recovery sequence, LGE, and cine MRI on a 3-T CMR system. LGE-MR findings were used to divide DCM patients into two groups: Group A had no apparent LGE, and Group B had LGE apparent in at least one segment. The ECV of the left ventricle (LV) myocardium (16 segments) was calculated in the short-axis view as follows: ECV = [(ΔR1 of myocardium/ΔR1 of LV blood pool)] × (1 − hematocrit), where R1 = 1/T1, ΔR1 = post-contrast R1 − pre-contrast R1. The LV ejection fraction (LVEF) was obtained from cine MRI images. The mean myocardial ECV in LGE (−) segments in Group A + B was compared to that of controls. The mean myocardial ECV in Group A was compared to that of LGE (−) segments in Group B. The correlation between LV systolic function and the mean myocardial ECV of the whole myocardium was evaluated in all groups. Among the 41 DCM patients, 22 were in Group A, and 19 were in Group B. The mean ECV of DCM patents (n = 41, 568 segments, 30.7 % ± 5.9) was significantly higher (P < 0.001) than that of the control group (n = 10, 157 segments, 25.6 % ± 3.2). The ECV was inversely related to LVEF in Group A (r = −0.551, P = 0.008), Group B (r = −0.525, P = 0.021), and Group A + B (r = −0.550, P < 0.001). The ECV measured by MRI could be a useful parameter in evaluating diffuse myocardial changes in DCM patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dilated cardiomyopathy (DCM) is a disease characterized by systolic and diastolic dysfunction with ventricular chamber enlargement that leads to progressive heart failure [1, 2]. Although there are several established causes of DCM (e.g., ischemic, nonischemic, genetic, myocarditis, cardiac toxins), the etiology is not apparent in many cases [2–4]. In DCM, diffuse myocardial fibrosis is a prominent factor during cardiac remodeling [1, 5], as increasing degrees of myocardial fibrosis are associated with progression of cardiac dysfunction [6, 7]. Late gadolinium enhancement (LGE) is a powerful imaging tool that can detect patterns of fibrosis [8]. Approximately 30 % of DCM patients show mid-wall LGE in areas that do not correspond to a coronary artery territory, which is a finding known to be related to cardiac events and prognosis in DCM [9, 10]. However, LGE often fails to detect diffuse myocardial fibrosis [5, 9]. An endomyocardial biopsy (EMB) can be performed to evaluate possible myocardial fibrosis; however, it is invasive with considerable risk in native hearts [11, 12]. Moreover, fibrosis may be patchy, and therefore the yield of EMB is reduced. Thus, a non-invasive method for quantitating ECV is desirable. Quantification of the myocardial extracellular volume fraction (ECV) using the CMR T1 mapping technique is a noninvasive method for detecting diffuse changes in the myocardium [13]. In non-ischemic DCM, variably elevated ECV were reported [14, 15]; however, there are no prior reports on the quantification of the ECV in patients without obvious LGE. The purpose of the current study was thus to evaluate the utility of the ECV in the detection of diffuse myocardial changes in DCM without obvious LGE.
Materials and methods
Patient selection
From March 2010 through November 2013, 123 patients who were suspected to have cardiomyopathy were referred to our hospital. The inclusion criteria for the patient group were as follows: (1) left-ventricular chamber dilatation and LV end diastolic diameter (LVEDD) on short-axis view ≥6 cm and (2) systolic dysfunction with or without right ventricle (RV) dysfunction and LV ejection fraction (LVEF) ≤40 %. Sixty-three patients fit the inclusion criteria. The exclusion criteria were (1) ischemic cardiomyopathy (n = 21) and (2) restrictive cardiomyopathy (n = 1). In total, 41 patients were enrolled in this study. Ten healthy volunteers who had no history or risk factors associated with heart disease were also enrolled. The hematocrit values of the patients and volunteers were acquired by venous sampling on the day of CMR acquisition. This single-center, prospective study was approved by our Institutional Review Board (IRB), and informed consent was obtained from all patients.
CMR protocol
CMR imaging was performed using a 3.0T MR scanner (Magnetom Trio Tim, Siemens AG Healthcare Sector, Erlangen, Germany) with a six-element body matrix coil and a spine matrix coil array. Localization of the heart was performed with TrueFISP localizers under electrocardiographic (ECG) gating. Cine, LGE, and pre- and post-contrast T1 mapping images were acquired. For cardiac functional analysis, cine images were acquired using a TrueFISP sequence in a short-axis plane orientation using the following parameters: TR = 3.3 ms, TE = 1.44 ms, flip angle = 50°, 25 phases, slice thickness = 8 mm, slice gap = 8 mm, acquisition matrix = 216 × 256, and a field of view = 337 × 400 mm2. T1 mapping was performed using a non-product modified Look-Locker Inversion-recovery (MOLLI) sequence in end expiration at three short-axis planes (i.e., basal, mid, apical left-ventricular level). For imaging, the nonselective inversion pulse, a TrueFISP single-shot readout sequence in mid-diastolic phase, was employed using the following parameters: field of view = 308 × 380 mm, acquisition matrix = 126 × 192, slice thickness = 8 mm, TR = 2.43 ms, TE = 1.01 ms, minimum inversion time = 100 ms, inversion time increment = 80 ms, flip angle = 35°, parallel acquisition technique factor = 2, number of inversions = 3, three images acquired after the first inversion, pause three heart beats, three images acquired after the second inversion, pause three heart beats, and five images acquired after the third inversion (“3,3,5” sequence). Fully-automated, non-rigid motion correction was applied to register the individual TI images before inline T1 fitting was performed using a mono-exponential 3-parameter fit. Pre-T1 mapping images were acquired before the injection of contrast. Post-contrast T1 mapping images were acquired 15 min after injection of a 0.2 mmol/kg intravenous dose of gadolinium contrast agent (Gadovist, Bayer Schering PharmaAG, Berlin, Germany). Between pre- and post-contrast T1 mapping sequences, LGE MR imaging was obtained 10 min after the injection of the contrast agent using a magnitude- and phase-sensitive inversion recovery (PSIR) prepared TrueFISP sequence, with the inversion time adjusted to null, representing the normal myocardium. LGE images were obtained along the same axis plane and with the same slice thickness as that used for the T1 mapping images (TR = 5.83 ms, TE = 3.24 ms, FOV 380 × 380 mm2, thickness 8 mm, matrix = 320 × 320, non-selective inversion recovery, flip angle = 20º, BW 460 Hz/pixel, number of trigger pulses = 2). The appropriate inversion time prior to LGE MR imaging was determined using a FLASH sequence with varying inversion times from 150 to 650 ms to null, representing the signal from the normal myocardium.
MR image analysis
Functional analysis
All MR images were transferred to a picture archiving and communication system (PACS; Centricity 1.0; GE Medical Systems, Mt Prospect, IL, USA) for image analysis. Two radiologists (Y.J.H and C.H.P) with 9 years of experience in cardiovascular image interpretation, who were blinded to the clinical data, independently analyzed all MRI images. The two observers assessed the function of the left ventricle (LV) on the short-axis cine MRI images using commercially-available software (Argus; Siemens AG Healthcare Sector, Erlangen, Germany). LVEDD was assessed at the mid ventricle where papillary muscles are visible on the short-axis view (Fig. 1). The endocardial and epicardial borders of the LV wall were delineated semi-automatically on the end-diastolic and end-systolic images. The papillary muscles and trabeculations were excluded from the LV myocardium. LV end-diastolic volume (LVEDV) and LV end-systolic volume (LVESV) were automatically measured. LVEF (%) was calculated as follows:
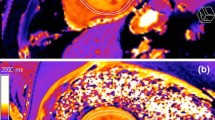
Measurement of pre-and post-contrast T1 values and ECV (%)
For regional analysis of the LV myocardium, pre-and post-contrast T1 mapping images obtained in three short-axis planes (i.e., basal, mid, apical LV level) were divided into 16 segments based on the AHA recommendation for the regional analysis of LV myocardium [18], excluding the apical segment (six segments for basal, mid LV, and four segments for apical level). For measurement of the T1 myocardial value, the region of interest covering each segment was drawn as large as possible while avoiding the partial volume averaging artifact [19, 20] (Fig. 2). For a measurement of the T1 value of blood, a circular region of interest larger than 200 mm2 was drawn in the LV cavity avoiding the papillary muscle. The ECV of the myocardium was calculated from the equation using hematocrit and pre-and post-contrast T1 values of the LV myocardium and blood cavity as follows:
Image analyses
Two investigators systematically recorded the presence of LGE in each segment: LGE (+) or LGE (−), and DCM patients were divided into two groups according to the LGE-MR findings. Group A included patients with no obvious LGE in all segments, and Group B included patients with the presence of obvious LGE in at least one segment. To evaluate the myocardium without obvious LGE, the mean myocardial ECV of LGE (−) segments in DCM patients (all segments in Group A and LGE (−) segments in Group B) was compared to that of the myocardium in healthy volunteers. Among DCM patients, the mean myocardial ECV in Group A was compared to that of LGE (−) segments in Group B. The correlation between the systolic function of LV and the mean ECV of the whole LV myocardium, including LGE (−) and LGE (+) segments, was evaluated in Group A, Group B, and healthy volunteers.
Statistical analyses
All continuous data were expressed as means ± standard deviations (SD), and categorical variables were presented as numbers or percentages. An independent t test was used to compare means of the pre-T1, EF, LVEDV, LVESV, LVEDD, and ECV from DCM patients and the control group. Analysis of variance (ANOVA) with post hoc analysis using the Bonferroni method was used to compare the pre-T1, EF, LVEDV, LVESV, LVEDD, and ECV in the control group, Group A, and Group B. A Pearson analysis was used to evaluate the correlation between ECV and EF in each group. An intraclass correlation coefficient (ICC) was used to determine the inter-observer reliability of T1 values and ECV measurements. P values less than 0.05 were considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Science (SPSS) software (ver. 20, SPSS Inc., Chicago, IL, USA).
Results
A total of 41 DCM patients (26 men, 15 women; mean age 52.8 ± 16.4 years, range 17–84 years), and 10 healthy subjects (7 men, 3 women; mean age 53.5 ± 4.0 years, range 48–60 years) were included in the current study. The clinical characteristics of the three groups and the etiologies of DCM are summarized in Table 1. Among the 41 DCM patients, 22 patients did not exhibit delayed enhancement (Group A, n = 22; 349 LGE [-] segments, three segments were excluded due to the presence of an artifact), and 19 patients displayed delayed enhancement on the LGE sequence (Group B, n = 19; 219 LGE [−] segments, 85 LGE [+] segments). The patterns of delayed enhancement are shown in Table 2.
The mean myocardial ECV of LGE (−) segments in DCM patients (30.7 % ± 5.9), (Group A + B, n = 41; 568 segments) was significantly higher (P < 0.001) than that of the control group (25.6 % ± 3.2, n = 10; 157 segments, three segments excluded due to the presence of an artifact; Table 3; Fig. 3). The mean myocardial ECV in Group A (31.2 % ± 5.6, 349 segments,) was significantly higher (P < 0.001) than the mean myocardial ECV in the control group (25.6 % ± 3.2); it was also significantly higher (P = 0.019) than that of LGE (−) segments in Group B (29.9 % ± 6.2, 219 segments) (Table 3; Fig. 4). The mean EF was 25.3 ± 8.8 % in Group A and 23.9 ± 7.0 % in Group B. The EF of the control group was 64.9 ± 6.4 % (Table 3). When the ECV of the whole myocardium, including LGE (−) and LGE (+) segments, was correlated with LVEF analyzed by cine MRI, there was no relationship between EF and ECV in the control group (P = 0.553; Fig. 5a). In Group A and B, the ECV was negatively correlated with EF (Group A: r = −0.551, P = 0.008; Group B: r = −0.525, P = 0.021; and Group A + B: r = −0.550, P < 0.001) (Fig. 5b–d). The pre-contrast T1 myocardial values in Group A (1,255.6 ± 75.8 ms) were not significantly different from the T1 myocardial values in Group B (1,238.2 ± 55.2 ms) or the control group (1,205.4 ± 37.4 ms). The mean LVEDD was 71.8 ± 7.6 mm in Group A, 69.0 ± 6.7 mm in Group B, and 51.9 ± 3.2 mm in the control group (Table 3). The interobserver reliability between the two readers was very high (ICC = 0.998 in T1, 0.986 in ECV, P < 0.001).
Discussion
The objective of the current study was to evaluate the feasibility of using cardiac MRI to quantify the ECV in DCM patients without overt LGE. The results of our study showed that quantification of the ECV using CMR was an effective method for detecting myocardial changes in DCM patients, even in cases where LGE was not apparent in the myocardium. The mean myocardial ECV in DCM patients without overt LGE was significantly higher than the average myocardial ECV in control subjects, and was negatively correlated with the ejection fraction. Recently, there have been numerous reports on the usefulness of the ECV as a parameter for detecting various cardiomyopathies other than myocardial infarction [15, 21, 22]. In non-ischemic cardiomyopathy, variably elevated ECV were noted [15, 22]; however, there have been no prior reports on the clinical significance of the ECV in patients without apparent LGE. Wu et al. [21] reported that adverse cardiac outcomes were significantly higher in non-ischemic cardiomyopathy patients with LGE than without LGE. However, the absence of LGE did not ensure the absence of adverse cardiac events, including malignant ventricular arrhythmias [21]. We focused on DCM patients without overt LGE and demonstrated that ECV is correlated to systolic dysfunction and is a reliable value for characterizing diffuse myocardial changes.
Although LGE could not detect myocardial abnormalities in patients with diffuse myocardial changes, it has been regarded as the gold standard for the evaluation of myocardial fibrosis. Several studies have reported on the prognostic value of LGE in cardiomyopathy, and thus the utility of LGE for detecting myocardial fibrosis has been well established [9, 21, 23]. In non-ischemic cardiomyopathy, LGE has also proven to be a useful tool for diagnosis and prognosis. Assomull et al. [9] reported that the LGE pattern of focal mid-wall fibrosis sparing the endocardium was a finding characteristic of DCM, and they showed a hazard ratio of 3.1 (95 % CI 1.1–8.5, P = 0.03) for the combined outcomes of all-cause mortalities and hospitalizations for any type of cardiovascular event. Further, Wu et al. [21] reported that the presence of LGE, regardless of segmental pattern, is associated with an adverse cardiac prognosis in non-ischemic cardiomyopathy.
Still, the use of LGE for the evaluation of diffuse myocardial fibrosis remains limited because it can only detect focal myocardial fibrosis. In diffuse or subtle myocardial disease, the accurate nulling of normal myocardium is difficult owing to the lack of a normal myocardial Ref. [5]. Among the 41 DCM patients included in our study, more than 50 % of the patients displayed delayed enhancement or no overt delayed enhancement in the myocardium. However, on ECV analysis, almost all of the DCM patients without apparent LGE exhibited elevated ECV in the myocardium. Additionally, the myocardial segment without overt LGE also displayed an elevated ECV even in DCM patients with an obvious LGE segment, which suggests that the myocardium without LGE had already changed to diffuse fibrosis. Without the T1 mapping sequence, any myocardial changes in these patients could not be detected using cardiac MRI.
T1 mapping has emerged as a promising quantitative method for detecting diffuse myocardial fibrosis. However, T1 values are known to be affected by confounding variables such as field strength, dose of gadolinium contrast agent, scan time, and renal function [24]. In contrast, ECV is known to be a more constant value rarely affected by these variables. Recently, the evaluation of ECV using equilibrium contrast CMR (EQ-CMR) was shown to be a robust and accurate method to quantify diffuse myocardial fibrosis. Measurement of ECV in EQ-CMR is based on the hypothesis that in an equilibrium state, concentrations of gadolinium contrast are equal in the blood and myocardial interstitium [25, 26]. Ugander et al. [13] showed that ECV measured by pre- and post-contrast T1 mapping could quantitatively characterize myocardial infarction, atypical diffuse fibrosis, and subtle myocardial abnormalities not clinically apparent on LGE images. Mongeon et al. [22] quantified ECV in patients with various infiltrative heart diseases and showed that ECV was strongly correlated to segmental LGE and LV mass index and reflected the severity of myocardial infiltration. Sado et al. [15] also demonstrated that ECV was a potentially useful biomarker for various cardiomyopathies. The results of the present study are in accordance with earlier studies that validated the use of CMR to assess the ECV and demonstrated that assessment of ECV was highly correlated with disease severity and deterioration of cardiac function [22, 27].
There are several limitations in our study. First, the sample size was small, which prevents generalization of the data. Second, follow-up data or pathological confirmation was not possible. Further studies will be required to evaluate whether or not elevation of ECV on a CMR study is independently associated with an adverse cardiac prognosis. Third, the amount of delayed hyperenhancement was not measured quantitatively. Fourth, in measuring ECV values, although pre-T1 and post-T1 maps were created with the same parameters including slice thickness and slice position, the location of measurement on the pre-T1 and post-T1 map images may be not exactly the same because they were scanned at different time points. Finally, the wide range of ages in the patient group might introduce bias; however, the age distribution followed a nominal distribution, and the mean value was not different from that of the control group.
Conclusion
In conclusion, almost all of the DCM patients without apparent LGE exhibited elevated myocardial ECV. In addition, the ECV was negatively correlated with LV systolic function. Therefore, ECV measurements using a T1 mapping technique could be a useful non-invasive tool to detect diffuse myocardial changes in DCM patients.
Abbreviations
- CMR:
-
Cardiac magnetic resonance
- DCM:
-
Dilated cardiomyopathy
- ECV:
-
Extracellular volume fraction
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- LVEDD:
-
Left-ventricular end-diastolic diameter
- LVEF:
-
Left-ventricular ejection fraction
- MOLLI:
-
Modified Look-Locker Inversion recovery
- PSIR:
-
Phase-sensitive inversion recovery
- RV:
-
Right ventricle
References
Iles L, Pfluger H, Phrommintikul A, Cherayath J, Aksit P, Gupta SN, Kaye DM, Taylor AJ (2008) Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J Am Coll Cardiol 52(19):1574–1580
Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB, American Heart A, Council on Clinical Cardiology HF, Transplantation C, Quality of C, Outcomes R, Functional G, Translational Biology Interdisciplinary Working G, Council on E, Prevention (2006) Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 113(14):1807–1816
Harris SR, Glockner J, Misselt AJ, Syed IS, Araoz PA (2008) Cardiac MR imaging of nonischemic cardiomyopathies. Magn Reson Imaging Clin N Am 16(2):165–183
O’Donnell DH, Abbara S, Chaithiraphan V, Yared K, Killeen RP, Martos R, Keane D, Cury RC, Dodd JD (2012) Cardiac MR imaging of nonischemic cardiomyopathies: imaging protocols and spectra of appearances. Radiology 262(2):403–422
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57(8):891–903
Maisch B (1996) Ventricular remodeling. Cardiology 87(Suppl 1):2–10
Sun Y, Weber KT (1998) Cardiac remodelling by fibrous tissue: role of local factors and circulating hormones. Ann Med 30(Suppl 1):3–8
McCrohon JA, Moon JC, Prasad SK, McKenna WJ, Lorenz CH, Coats AJ, Pennell DJ (2003) Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation 108(1):54–59
Assomull RG, Prasad SK, Lyne J, Smith G, Burman ED, Khan M, Sheppard MN, Poole-Wilson PA, Pennell DJ (2006) Cardiovascular magnetic resonance, fibrosis, and prognosis in dilated cardiomyopathy. J Am Coll Cardiol 48(10):1977–1985
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S, Morarji K, Brown TD, Ismail NA, Dweck MR, Di Pietro E, Roughton M, Wage R, Daryani Y, O’Hanlon R, Sheppard MN, Alpendurada F, Lyon AR, Cook SA, Cowie MR, Assomull RG, Pennell DJ, Prasad SK (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309(9):896–908
Deckers JW, Hare JM, Baughman KL (1992) Complications of transvenous right ventricular endomyocardial biopsy in adult patients with cardiomyopathy: a seven-year survey of 546 consecutive diagnostic procedures in a tertiary referral center. J Am Coll Cardiol 19(1):43–47
From AM, Maleszewski JJ, Rihal CS (2011) Current status of endomyocardial biopsy. Mayo Clin Proc 86(11):1095–1102
Ugander M, Oki AJ, Hsu LY, Kellman P, Greiser A, Aletras AH, Sibley CT, Chen MY, Bandettini WP, Arai AE (2012) Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J 33(10):1268–1278
Kellman P, Wilson JR, Xue H, Bandettini WP, Shanbhag SM, Druey KM, Ugander M, Arai AE (2012) Extracellular volume fraction mapping in the myocardium, part 2: initial clinical experience. J Cardiovasc Magn Reson 14:64
Sado DM, Flett AS, Banypersad SM, White SK, Maestrini V, Quarta G, Lachmann RH, Murphy E, Mehta A, Hughes DA, McKenna WJ, Taylor AM, Hausenloy DJ, Hawkins PN, Elliott PM, Moon JC (2012) Cardiovascular magnetic resonance measurement of myocardial extracellular volume in health and disease. Heart 98(19):1436–1441
Lalande A, Salve N, Comte A, Jaulent MC, Legrand L, Walker PM, Cottin Y, Wolf JE, Brunotte F (2004) Left ventricular ejection fraction calculation from automatically selected and processed diastolic and systolic frames in short-axis cine-MRI. J Cardiovasc Magn Reson 6(4):817–827
Baldy C, Douek P, Croisille P, Magnin IE, Revel D, Amiel M (1994) Automated myocardial edge detection from breath-hold cine-MR images: evaluation of left ventricular volumes and mass. Magn Reson Imaging 12(4):589–598
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS, American Heart Association Writing Group on Myocardial S, Registration for Cardiac I (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105(4):539–542
Moon JC, Messroghli DR, Kellman P, Piechnik SK, Robson MD, Ugander M, Gatehouse PD, Arai AE, Friedrich MG, Neubauer S, Schulz-Menger J, Schelbert EB, Society for Cardiovascular Magnetic Resonance I, Cardiovascular Magnetic Resonance Working Group of the European Society of C (2013) Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson 15:92
Piechnik SK, Ferreira VM, Lewandowski AJ, Ntusi NA, Banerjee R, Holloway C, Hofman MB, Sado DM, Maestrini V, White SK, Lazdam M, Karamitsos T, Moon JC, Neubauer S, Leeson P, Robson MD (2013) Normal variation of magnetic resonance T1 relaxation times in the human population at 1.5 T using ShMOLLI. J Cardiovasc Magn Reson 15:13
Wu KC, Weiss RG, Thiemann DR, Kitagawa K, Schmidt A, Dalal D, Lai S, Bluemke DA, Gerstenblith G, Marban E, Tomaselli GF, Lima JA (2008) Late gadolinium enhancement by cardiovascular magnetic resonance heralds an adverse prognosis in nonischemic cardiomyopathy. J Am Coll Cardiol 51(25):2414–2421
Mongeon FP, Jerosch-Herold M, Coelho-Filho OR, Blankstein R, Falk RH, Kwong RY (2012) Quantification of extracellular matrix expansion by CMR in infiltrative heart disease. JACC Cardiovasc Imaging 5(9):897–907
Green JJ, Berger JS, Kramer CM, Salerno M (2012) Prognostic value of late gadolinium enhancement in clinical outcomes for hypertrophic cardiomyopathy. JACC Cardiovasc Imaging 5(4):370–377
Lee JJ, Liu S, Nacif MS, Ugander M, Han J, Kawel N, Sibley CT, Kellman P, Arai AE, Bluemke DA (2011) Myocardial T1 and extracellular volume fraction mapping at 3 tesla. J Cardiovasc Magn Reson 13:75
Flett AS, Hayward MP, Ashworth MT, Hansen MS, Taylor AM, Elliott PM, McGregor C, Moon JC (2010) Equilibrium contrast cardiovascular magnetic resonance for the measurement of diffuse myocardial fibrosis: preliminary validation in humans. Circulation 122(2):138–144
Klein C, Nekolla SG, Balbach T, Schnackenburg B, Nagel E, Fleck E, Schwaiger M (2004) The influence of myocardial blood flow and volume of distribution on late Gd-DTPA kinetics in ischemic heart failure. J Magn Reson Imaging 20(4):588–593
Miller CA, Naish JH, Bishop P, Coutts G, Clark D, Zhao S, Ray SG, Yonan N, Williams SG, Flett AS, Moon JC, Greiser A, Parker GJ, Schmitt M (2013) Comprehensive validation of cardiovascular magnetic resonance techniques for the assessment of myocardial extracellular volume. Circ Cardiovasc Imaging 6(3):373–383
Acknowledgments
This work was supported by a faculty research grant of Yonsei University College of Medicine for 2011 (6-2011-0190).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hong, Y.J., Park, C.H., Kim, Y.J. et al. Extracellular volume fraction in dilated cardiomyopathy patients without obvious late gadolinium enhancement: comparison with healthy control subjects. Int J Cardiovasc Imaging 31 (Suppl 1), 115–122 (2015). https://doi.org/10.1007/s10554-015-0595-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0595-0