Abstract
Purpose
There is increasing evidence that coffee consumption is related to reduced risks for some cancers, but the evidence for renal cancer is inconclusive. Therefore, we conducted a meta-analysis to summarize the cohort evidence of this relationship.
Methods
A literature search was performed in PubMed and Embase through February 2021. Meta-analyses using a random effects model were conducted for reported relative risk estimates (RRs) relating coffee intake and renal cancer incidence or mortality. We also performed a two-stage random effects exposure–response meta-analysis. Between-study heterogeneity was assessed.
Results
In a meta-analysis of the ten identified cohort studies, we found a summary RR of 0.88 [95% confidence interval (CI) 0.78–0.99] relating the highest vs. the lowest category of coffee intake and renal cancer, with no significant between-study heterogeneity observed (I2 = 35%, p = 0.13). This inverse association remained among studies of incident cancers (RR 0.85, 95% CI 0.76–0.96) and studies adjusting for smoking and body mass index (RR 0.87, 95% CI 0.77–0.99).
Conclusions
Our findings from this meta-analysis of the published cohort evidence are suggestive of an inverse association between coffee consumption and renal cancer risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cancer is estimated to have accounted for 2.4% of all estimated worldwide cancer cases in 2018 [1] and was the sixth and tenth most commonly diagnosed cancer among US men and women, respectively [2]. The US incidence rate of cancers of the kidney and renal pelvis in 2017 (15.6 per 100,000) has increased 24% since 2000 (12.5 per 100,000) and 120% since 1975 (7.8 per 100,000) [3], partly because of incidental detection of asymptomatic tumors using medical imaging [4]. Modifiable risk factors of renal cancer established to date include excess body weight [5, 6], hypertension [7] and tobacco smoking [8]. There is also accumulating evidence supporting an inverse association with alcohol consumption [9].
Coffee, one of most popular beverages worldwide, contains antioxidants and anticarcinogenic compounds [10, 11] and has been associated with reduced risks of some malignancies such as cancers of the liver, colon/rectum, and endometrium [12, 13]. The epidemiologic evidence relating coffee intake to renal cancer risk, however, has been inconclusive. A previous meta-analysis [14] including 16 case–control and six cohort studies found no significant association between coffee intake and renal cancer risk. However, a weak inverse relationship was observed in an analysis restricted to cohort studies, which are less susceptible to bias than case–control studies [15]. Since the publication of that meta-analysis [14] several large cohort analyses investigating coffee consumption and renal cancer risk have been published [16,17,18,19]. To better understand the cohort evidence of this relationship, we conducted a new meta-analysis focusing on evidence from this study design.
Methods
Search strategy
We performed a literature search in PubMed, Embase, and The Cochrane Library for studies published through February 2021, using the Medical Subject Headings (MeSH) terms or key words “cancer”, “tumor”, “carcinoma”, “malignant neoplasm”, “renal cancer”, “kidney cancer”, “renal cell carcinoma”, “kidney neoplasm”, “coffee”, “caffeine” and “beverages” (Supplementary File 1). Additionally, the reference lists of all retrieved articles, including previous relevant meta-analysis and review articles, were checked to identify additional studies. We followed the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines throughout the design, conduct, analysis, and reporting of this meta-analysis [20].
Study selection, data extraction, and quality assessment
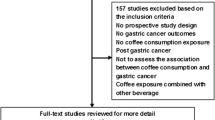
We included cohort studies which reported relative risks (RRs) with corresponding 95% confidence intervals (CIs) estimating the association between coffee intake (any kind) and renal cancer. The studies reporting RRs and 95% CIs for more than three categories of coffee intake as well as category-specific number of participants and number of renal cancers were further eligible for exposure–response meta-analysis. We excluded review articles, abstracts, editorial letters, non-English articles, and relevant studies of coffee and cancer risk that did not include renal cancer specifically (Fig. 1).
From each selected study we extracted the following information: authors, publication year, study geographic region, number of years of follow-up, type of endpoint (incident cases, deaths), renal cancer definition, number of participants, number of cases, scales of coffee intake (categorical and/or continuous number of drinks per day), most fully adjusted RRs and corresponding 95% CIs, and adjusted variables in the multivariable models. For the exposure–response meta-analysis, we extracted category-specific ranges of coffee intake, its most fully adjusted RRs and corresponding 95% CIs. All extracted data were cross-checked by the authors.
We performed quality assessments using the Newcastle–Ottawa scale [21] for cohort studies which addresses subject selection, study comparability, and the assessment of outcome.
Statistical analysis
Meta-analyses for RRs contrasting the highest vs. lowest level of coffee intake per day were performed using a random effects model. We additionally performed a two-stage random effects exposure–response meta-analysis to examine linear and potential non-linear relationships between coffee intake and risk of renal cancer using the Greenland and Longnecker method [22, 23] for covariance approximation and the multivariate DerSimonian and Laird method [24, 25] to estimate summary RRs. For the analysis of a linear relationship, we calculated the median value of coffee intakes in each exposure category and matched it to the category-specific RR. For categories with undefined upper boundary (e.g., ≥ 4 cups/day), we calculated the median value assuming the range of the category to be the same as other defined intervals. For a non-linear exposure–response meta-analysis, we used a restricted cubic spline model with 3 knots at fixed percentiles of the distribution (25%, median, 75%) [26]. We excluded studies that did not report the number of participants or renal cancer cases for each category of coffee intake [18, 27, 28] from our analysis of linear/non-linear relationships to avoid biases in the estimates for the variances of the log RRs [29]. We used a Wald-type test to calculate a P value for non-linearity testing that null hypothesis that the coefficient of the second spline was equal to zero [29].
As a sensitivity analysis, we restricted meta-analyses to study findings having non-drinkers as a reference group [18, 19, 27] instead of the least coffee drinkers (e.g., < 1 cup/day or ≤ 2 cups/day) [16, 17, 28, 30,31,32,33]. We also examined the summary risk of renal cancer excluding a study for which we manually calculated the effect estimates [30], a study having a different scale for coffee intake other than cup/day (e.g., occasions per day [31]), and a study which did not adjust for additional confounders other than age and sex [27]. Similarly, we conducted influence analyses, repeating our meta-analysis after excluding each study one at a time.
Potential publication bias was evaluated by the asymmetrical shape of a funnel plot and by the p-value from Egger’s test [34]. Between-study heterogeneity was assessed using Cochran Q-statistic and quantified by Higgins I2 statistic and associated 95% CIs [35]. Sources of heterogeneity were explored by performing meta-regression and subgroup analyses by sex (women, men), study region (US/Canada, other regions), outcome definition (kidney cancer, renal cell carcinoma), type of outcome (incidence, mortality), smoking status (never smokers, ever smokers), BMI (study-specific BMI cutpoints splitting participants into categories of healthy weight and overweight/obesity; see Table 1 footnote) and adjustment for established risk factors for renal cancer (smoking [8], BMI [5, 6], alcohol consumption [9]).
All statistical analyses were conducted with the metaphor [36] and dosresmeta [37] packages in R (R Foundation for Statistical Computing, Vienna, Austria) [38]. P values less than 0.05 were considered statistically significant.
Results
The results of our systematic review of the published literature are summarized in Fig. 1. From our collection of screened articles (n = 7,584) we excluded irrelevant topic articles (n = 7,469), systematic reviews (n = 48), editorial letter (n = 1), abstracts (n = 5), and non-English articles (n = 2). Among 59 full-text articles assessed for eligibility, we further excluded relevant articles not reporting measures of association (n = 9), relevant articles including only non-renal cancer outcomes (n = 13), and case–control studies (n = 27). Following these exclusions, ten cohort studies remained. These remaining studies had estimated Newcastle–Ottawa total quality scores of 9 (n = 9) or 8 (n = 1) (Supplementary Table 1).
In a meta-analysis of the ten identified studies [16,17,18,19, 27, 28, 30,31,32,33], which collectively included 8,399 renal cancer cases, we found a summary RR of 0.88 (95% CI 0.78–0.99) relating the highest study category of coffee intake (vs. the lowest category or non-drinkers) and renal cancer risk (Fig. 2), with no significant between-study heterogeneity observed (I2 = 35%, 95% CI 0–69.1%, p = 0.13). In the influence analyses, we observed the summary RRs ranged from 0.86 (95% CI 0.76–0.97, excluding Allen et al. [32], lowest RR; Fig. 3) to 0.91 (95% CI 0.80–1.03, excluding Rhee et al. [19], highest RR). Visual inspection of the funnel plot suggested that the studies were nearly symmetrically distributed around the log of the summary estimate (Fig. 4), and Egger’s tests presented that there was no significant evidence of publication bias (p = 0.78).
In the exposure–response meta-analysis, which included seven studies [16, 17, 19, 30,31,32,33], the test for non-linear effects was not statistically significant (p for non-linearity = 0.13, Supplementary Fig. 1). In computing a linear exposure–response relationship, we estimated that one additional cup of coffee per day was associated with a 3.0% decrease in the risk of renal cancer (summary RR 0.97, 95% CI 0.94–1.00).
The meta-regression tests showed that none of the evaluated study characteristics (sex, study region, outcome definition, type of outcome, smoking status, BMI, adjustment of renal cancer risk factors) significantly modified the summary RR of coffee intake on the risk of renal cancer (Table 1). The summary RR of comparing the highest vs. lowest coffee intake and risk of renal cancer was comparable for men and women (0.89, 95% CI 0.69–1.15 and 0.85, 95% CI 0.72–1.02, respectively; p for interaction = 0.90). There was no difference in the association by outcome definition (p = 0.40) as more than 90% of kidney cancers are renal cell carcinoma [39]. In meta-analyses of results stratified by smoking status, a stronger inverse association was observed among never smokers (RR 0.79, 95% CI 0.59–1.08) than ever smokers (RR 0.96, 95% CI 0.87–1.06), although a test of interaction was not statistically significant (p = 0.15). The inverse association remained when restricted to studies of incident renal cancer [17, 19, 28, 30,31,32,33] (RR 0.85, 95% CI 0.76–0.96) and those which adjusted for both smoking and BMI [16,17,18,19, 28, 31, 32] (RR 0.87, 95% CI 0.77–0.99) as well as studies with additional adjustment for alcohol consumption [16,17,18,19, 28] (RR 0.85, 95% CI 0.78–0.94).
In sensitivity analyses, we found that the summary RRs of the highest vs. lowest meta-analysis were similar after excluding a study with manually calculated RR [30] (summary RR 0.88, 95% CI 0.78–1.00), a study with a different scale for coffee intake [31] (RR 0.88, 95% CI 0.80–0.97), and a study only adjusting for age and sex [27] (RR 0.87, 95% CI 0.78–0.96). We observed a similar association when we restricted studies to those having non-drinkers as a reference group [18, 19, 27] (summary RR of highest vs. lowest 0.90, 95% CI 0.64–1.27).
Discussion
In this meta-analysis of ten cohort studies, we found a 22% lower risk of renal cancer in the highest coffee intake group compared to the lowest category with no significant between-study heterogeneity. The inverse associations remained when we restricted to studies with incident renal cancer as the outcome and those adjusting for smoking, BMI and alcohol intake. The linear exposure–response analysis of seven studies estimated a 3% lower risk of renal cancer for one additional cup of coffee per day. There was no evidence of publication bias in our study.
Our findings suggest that the cohort evidence for an inverse association between coffee intake and renal cancer is stronger than that observed in the previous meta-analysis [14] (summary RR 0.88, 95% CI 0.70–1.10). We additionally conducted a linear exposure–response analysis and found a 3% lower RR of renal cancer for one additional cup of coffee a day. It is notable that two studies [18, 28] which could not be included in the exposure–response analysis due to missing information on case frequencies across exposure categories reported similar RRs per cup per day (0.97, 95% CI 0.93–1.01 [28]; 0.95, 95% CI 0.90–1.01 [18], respectively). Interestingly, an identical magnitude of association was observed in previous meta-analyses of coffee in relation to total cancer [40] and endometrial cancer [13] (RR 0.97 per one cup of coffee/day, 95% CI 0.96–0.98 in each meta-analysis).
We observed a non-significantly stronger inverse association among never smokers (RR 0.79, 95% CI 0.59–1.08) compared to coffee RRs among smokers (RR 0.96, 95% CI 0.87–1.06) for the four studies [16, 17, 19, 28] that presented RRs stratified by smoking status. We further observed an inverse association among seven studies that presented smoking-adjusted RRs (summary RR 0.87, 95% CI 0.77–0.99) [16,17,18,19, 28, 31, 32], but no association among three studies that provided RRs without adjustment of smoking (RR 1.12, 95% CI 0.59, 2.14) [27, 30, 33]. The potential for residual confounding towards the null from smoking may at least partially account for the null association among ever smokers, as coffee consumption is more common among smokers than non-smokers [41]. We found a low level of between-study heterogeneity overall, although we observed a slightly stronger inverse association after excluding Allen et al. [32] (which reported substantially higher coffee intakes than other studies; Supplementary Table 1) and a slightly weaker, non-significant association after excluding Rhee et al. [19]. None of the study characteristics appeared to materially affect the summary effect estimates.
Our findings are compatible with the hypothesis that coffee intake may be associated with a lower renal cancer risk. There are several biologic mechanisms that potentially play a role in mediating such an effect from coffee. Cafestol and kahweol, natural diterpenes extracted from coffee beans, have been shown to have a role in anti-carcinogenic activity [11]. Particularly, it has been found that cafestol modulates multiple proteins in apoptotic response of Caki-1 human renal cancer cell lines in an in vivo study [42]. Coffee intake has been associated with lower risks of chronic kidney disease (CKD) [43,44,45] and lower estimated glomerular filtration rate, which are themselves risk factors for renal cancer [46]. Additionally, coffee intake has been related to higher insulin sensitivity and lower risk of type 2 diabetes [47], another renal cancer risk factor. Finally, coffee intake may dilute the concentration of carcinogens in renal epithelial cells by increasing urine volume [28].
There are several strengths to this meta-analysis. We substantially updated the cohort evidence in the recent meta-analysis [14] by including four additional studies involving over 5,600 incident renal cancer cases [16,17,18,19, 30]. Our restriction to cohort-based evidence helped avoid summarizing potentially biased risk estimates due to recall or selection bias in case–control studies. Unlike with the previous meta-analysis, we performed exposure–response meta-analyses and assessed the robustness of our findings through several sensitivity and subgroup analyses. We observed consistent findings in the influence test and found no evidence of publication bias.
Our study has some limitations to be noted. First, variation in the definition of cup size could lead to misclassification of coffee consumption. Poole et al. [48] found that when standardized by volume (227 mL), 84% of study participants had correctly classified reported intakes, 8% underestimated, and 8% overestimated, compared to reported cups. Second, we were not able to evaluate potential differences in renal cancer risk by coffee type (caffeinated vs. decaffeinated) or brewing method (boiled vs. filtered) due to the limited number of studies providing such results. Among studies providing evidence, it is unclear whether coffee type or brewing method modifies the association. Nilsson et al. [31] reported a stronger inverse association for filtered coffee intake (hazard ratio (HR) 0.46, 95% CI 0.17–1.24 for coffee intake ≥ 4 occasions/day vs. < 1 occasion/day) than boiled coffee (0.90, 95% CI 0.28–2.97). However, Lukic et al. [17] found similar associations for both brewing methods. Both Gapstur et al. [16] and Rhee et al. [19] did not find significant differences in renal cancer risk for caffeinated and decaffeinated coffee. Third, selected studies mainly included studies conducted in North America and Europe; it is unclear whether the observed findings are generalizable to Asian or African populations.
In conclusion, in this meta-analysis of ten cohort studies, we observed an inverse association between higher coffee consumption and lower renal cancer risk. Additional large prospective investigations of coffee consumption and renal cancer risk in diverse populations are needed to clarify this relationship, as well as experimental and molecular studies to elucidate possible anti-neoplastic mechanisms related to coffee consumption.
Data availability
All data reported in this manuscript are found in the literature as cited in the text.
Code availability
Researchers who are interested in R codes for the analyses may contact the authors.
Abbreviations
- MeSH:
-
Medical subject headings
- MOOSE:
-
Meta-analysis of observational studies in epidemiology
- RR:
-
Relative risk
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- BMI:
-
Body mass index
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30
Howlader N, Noone AM, Krapcho M et al (2020) SEER cancer statistics review, 1975–2017. National Cancer Institute, Bethesda, MD
Chow W-H, Devesa SS, Warren JL, Fraumeni JF Jr (1999) Rising incidence of renal cell cancer in the United States. JAMA 281:1628–1631
Bergström A, Hsieh C, Lindblad P, Lu C, Cook N, Wolk A (2001) Obesity and renal cell cancer–a quantitative review. Br J Cancer 85:984–990
Bjørge T, Tretli S, Engeland A (2004) Relation of height and body mass index to renal cell carcinoma in two million Norwegian men and women. Am J Epidemiol 160:1168–1176
Hidayat K, Du X, Zou S-Y, Shi B-M (2017) Blood pressure and kidney cancer risk: meta-analysis of prospective studies. J Hypertens 35:1333–1344
Cumberbatch MG, Rota M, Catto JW, La Vecchia C (2016) The role of tobacco smoke in bladder and kidney carcinogenesis: a comparison of exposures and meta-analysis of incidence and mortality risks. Eur Urol 70:458–466
Song DY, Song S, Song Y, Lee JE (2012) Alcohol intake and renal cell cancer risk: a meta-analysis. Br J Cancer 106:1881–1890
Gómez-Ruiz JÁ, Leake DS, Ames JM (2007) In vitro antioxidant activity of coffee compounds and their metabolites. J Agric Food Chem 55:6962–6969
Cavin C, Holzhaeuser D, Scharf G, Constable A, Huber W, Schilter B (2002) Cafestol and kahweol, two coffee specific diterpenes with anticarcinogenic activity. Food Chem Toxicol 40:1155–1163
Poole R, Kennedy OJ, Roderick P, Fallowfield JA, Hayes PC, Parkes J (2017) Coffee consumption and health: umbrella review of meta-analyses of multiple health outcomes. BMJ 359:J5024
Lukic M, Guha N, Licaj I et al (2018) Coffee drinking and the risk of endometrial cancer: an updated meta-analysis of observational studies. Nutr Cancer 70:513–528
Wijarnpreecha K, Thongprayoon C, Thamcharoen N, Panjawatanan P, Cheungpasitporn W (2017) Association between coffee consumption and risk of renal cell carcinoma: a meta-analysis. Intern Med J 47:1422–1432
Gibson TM, Ferrucci LM, Tangrea JA, Schatzkin A (2010) Epidemiological and clinical studies of nutrition. Semin Oncol 37:282–296
Gapstur SM, Anderson RL, Campbell PT et al (2017) Associations of coffee drinking and cancer mortality in the cancer prevention study-II. Cancer Epidemiol Biomarkers Prev 26:1477–1486
Lukic M, Nilsson LM, Skeie G, Lindahl B, Braaten T (2018) Coffee consumption and risk of rare cancers in Scandinavian countries. Eur J Epidemiol 33:287–302
Park S-Y, Freedman ND, Haiman CA, Le Marchand L, Wilkens LR, Setiawan VW (2018) Prospective study of coffee consumption and cancer incidence in non-white populations. Cancer Epidemiol Biomarkers Prev 27:928–935
Rhee J, Loftfield E, Freedman ND, Liao LM, Sinha R, Purdue MP (2021) Coffee consumption and risk of renal cell carcinoma in the NIH-AARP Diet and Health Study. Int J Epidemiol. https://doi.org/10.1093/ije/dyab011
Stroup DF, Berlin JA, Morton SC et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 283:2008–2012
Wells GA, Tugwell P, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 15 April, 2021
Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135:1301–1309
Orsini N, Bellocco R, Greenland S (2006) Generalized least squares for trend estimation of summarized dose–response data. Stata J 6:40–57
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Jackson D, White IR, Thompson SG (2010) Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med 29:1282–1297
Crippa A, Discacciati A, Larsson SC, Wolk A, Orsini N (2014) Coffee consumption and mortality from all causes, cardiovascular disease, and cancer: a dose-response meta-analysis. Am J Epidemiol 180:763–775
Washio M, Mori M, Sakauchi F et al (2005) Risk factors for kidney cancer in a Japanese population: findings from the JACC Study. J Epidemiol 15:S203–S211
Lee JE, Hunter DJ, Spiegelman D et al (2007) Intakes of coffee, tea, milk, soda and juice and renal cell cancer in a pooled analysis of 13 prospective studies. Int J Cancer 121:2246–2253
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175:66–73
Stensvold I, Jacobsen BK (1994) Coffee and cancer: a prospective study of 43,000 Norwegian men and women. Cancer Causes Control 5:401–408
Nilsson LM, Johansson I, Lenner P, Lindahl B, Van Guelpen B (2010) Consumption of filtered and boiled coffee and the risk of incident cancer: a prospective cohort study. Cancer Causes Control 21:1533–1544
Allen N, Balkwill A, Beral V, Green J, Reeves G (2011) Fluid intake and incidence of renal cell carcinoma in UK women. Br J Cancer 104:1487–1492
Hashibe M, Galeone C, Buys SS et al (2015) Coffee, tea, caffeine intake, and the risk of cancer in the PLCO cohort. Br J Cancer 113:809
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48
Crippa A, Orsini N (2016) Multivariate dose-response meta-analysis: the dosresmeta R package. J Stat Softw 72:1–15
Team RC (2013) R: A language and environment for statistical computing. Austria, Vienna
Hsieh JJ, Purdue MP, Signoretti S et al (2017) Renal cell carcinoma. Nat Rev Dis Primers 3:17009
Yu X, Bao Z, Zou J, Dong J (2011) Coffee consumption and risk of cancers: a meta-analysis of cohort studies. BMC Cancer 11:1–11
Swanson JA, Lee JW, Hopp JW (1994) Caffeine and nicotine: a review of their joint use and possible interactive effects in tobacco withdrawal. Addict Behav 19:229–256
Choi MJ, Park EJ, Oh JH et al (2011) Cafestol, a coffee-specific diterpene, induces apoptosis in renal carcinoma Caki cells through down-regulation of anti-apoptotic proteins and Akt phosphorylation. Chem Biol Interact 190:102–108
Jhee JH, Nam KH, An SY et al (2018) Effects of coffee intake on incident chronic kidney disease: a community-based prospective cohort study. Am J Med 131:1482–1490
Hu EA, Selvin E, Grams ME, Steffen LM, Coresh J, Rebholz CM (2018) Coffee consumption and incident kidney disease: results from the Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis 72:214–222
Bigotte Vieira M, Magriço R, Viegas Dias C, Leitão L, Neves JS (2019) Caffeine consumption and mortality in chronic kidney disease: a nationally representative analysis. Nephrol Dial Transplant 34:974–980
Herber-Gast G-CM, Hv E, Verschuren WM et al (2016) Coffee and tea consumption in relation to estimated glomerular filtration rate: results from the population-based longitudinal Doetinchem Cohort Study. Am J Clin Nutr 103:1370–1377
Van Dam RM, Feskens EJ (2002) Coffee consumption and risk of type 2 diabetes mellitus. Lancet 360:1477–1478
Poole R, Ewings S, Parkes J, Fallowfield JA, Roderick P (2019) Misclassification of coffee consumption data and the development of a standardised coffee unit measure. BMJ Nutr Prev Health. https://doi.org/10.1136/bmjnph-2018-000013
Funding
This research was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, Division of Cancer Epidemiology & Genetics.
Author information
Authors and Affiliations
Contributions
JR: designed study, extracted data, conducted analyses, and wrote the manuscript. RKL contributed to literature searches, literature review, data retrieval and provided feedback to the manuscript. MPP critically reviewed the manuscript and supervised the project.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and consent to participate
The systematic review and meta-analysis do not require ethical approval or consent to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rhee, J., Lim, R.K. & Purdue, M.P. Coffee consumption and risk of renal cancer: a meta-analysis of cohort evidence. Cancer Causes Control 33, 101–108 (2022). https://doi.org/10.1007/s10552-021-01506-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01506-1