Abstract
Purpose
Despite an increasing understanding of the pathology and genetics of non-Hodgkin lymphoma (NHL), global reports on variations in the incidence of NHL remain limited in their number and scope.
Methods
To provide a situation analysis, national incidence estimates for NHL in 185 countries for the year 2018 were obtained from the GLOBOCAN database. We also used recorded incidence data from Cancer Incidence in Five Continents (CI5) plus for years of diagnosis 1980–2012 to examine temporal trends.
Results
NHL ranked as the 5th to 9th most common cancer in most countries worldwide, with almost 510,000 new cases estimated in 2018. Observed incidence rates of NHL 2008–2012 varied markedly by world region: among males, rates were highest among Israel Jews [age-standardized (world) rate of 17.6 per 100,000), Australia (15.3), US whites (14.5), Canada (13.7), and Portugal (13.3)]. Where data were available, most populations exhibited stable or slightly increasing incidence rates; in North America, parts of Europe, and Oceania the rising incidence rates were generally observed until the 1990s, with a stabilization seen thereafter.
Conclusion
Marked variations in NHL incidence rates remain in populations in each world region. Special attention should be given to further etiological research on the role of endemic infections and environmental exposures, particularly in Africa, Asia, and Latin America. To permit internationally comparable statistics, an equal focus on addressing the quality of hematological information in population-based registries is also warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-Hodgkin lymphoma (NHL) ranks as the tenth and twelfth most frequent cancer in males and females worldwide, respectively, with an estimated 509,590 new cases and 248,724 deaths in 2018 [1]. These malignancies arise from the malignant transformation of mature and immature cells of immune system, affecting either B lymphocytes (B cells, representing around 86% of all NHL), and a smaller proportion of T- and natural killer (NK) cells (14% in developing regions) [2]. The classification of NHL is complex; knowledge of both clinical features and genetic abnormalities is essential to distinguish entities and provide accurate diagnoses [3]. A large proportion of NHL diagnoses (e.g., 35% in the UK) occur at older ages, with a peak incidence rate at ages at 75 or older [4]; the frequency of NHL subtypes varies by country [5]. Five-year survival estimates of 80% are observed in high-income settings but vary according to subtype and age; survival is markedly lower in low- and middle-income countries (LMIC) [6].
The incidence of NHL is associated with considerable geographic and temporal variability worldwide, although this inherent aetiological heterogeneity has helped uncover few risk factors. Genetic determinants, including a family history of NHL, have been implicated as a cause of NHL, as have certain lifestyle and environmental factors, including obesity and certain occupational exposures [7]. It has been established that infections, particularly those associated with Hepatitis C virus (HCV), Epstein–Barr virus (EBV), and Helicobacter pylori (H. pylori) can increase or modulate the risk of NHL [8]. While the risk of NHL is higher among HIV-infected persons as a result of immunosuppression [9], declines in the elevated risk have been reported from some high-income settings in the post-antiretroviral therapy (ART) era [10].
Even with an increasing understanding of the pathology and genetics of NHL, global reports on the patterns and trends of NHL remain rather limited in number and scope. In part, this may reflect the underlying complexity of evolving classification and diagnostic criteria that cancer registries are tasked to comply with. This global overview seeks to identify distinct patterns of incidence that may serve to generate hypotheses for further investigation, as well as inform cancer control. We focus on geographical and temporal variations in NHL according to country, sex, and age using the recorded data from population-based cancer registries (PBCR), alongside national estimates compiled at the International Agency for Research on Cancer (IARC).
Methods
Data sources and population
Estimates of NHL incidence for 185 countries in the year 2018 were extracted from IARC’s GLOBOCAN database [1]. The methods of estimation are based on the most reliable sources of cancer incidence and mortality data available at national or subnational level. A detailed account of the methods is provided by Ferlay and colleagues elsewhere [11]. We examined the age profile of NHL according to the Human Development Index (HDI) based on the predefined cut-points: low (HDI < 0.5), medium (0.5 ≤ HDI < 0.8), high (0.8 ≤ HDI < 0.9), and very high (HDI ≥ 0.9) [12].
The prevalence of HIV among adults aged 15 to 49 in 128 countries for the year 2010 was extracted from the WHO Global Health Observatory [13], representing the percentage of the national population aged 15–49 years and living with HIV. These are visually correlated with age-standardized NHL incidence rates as estimated in GLOBOCAN for the year 2018 [11].
New cases of NHL and population-at-risk data were extracted from successive volumes of Cancer Incidence in Five Continents (CI5), a compendium of high-quality data from population-based cancer registries (PBCR) worldwide [14]. We extracted recorded incidence and population data as reported in the latest volume of CI5 (volume XI) for 343 cancer registries in 62 countries worldwide, predominantly for the years of diagnosis 2008–2012. We examined temporal patterns of NHL in selected countries using the longstanding high-quality cancer registries that were included in the last six volumes of CI5 covering the period from 1980 to 2012, based on the data provided by population-based cancer registries (PBCR) worldwide [15]. In the absence of national coverage, an existing subnational registry or a pool of such registries represented the relevant country (http://ci5.iarc.fr/CI5-XI/Pages/registry_summary.aspx).
To ensure comparability in the incidence between registry populations in CI5, morphological groups of the International Classification of Diseases for Oncology (ICD-O, 2000) were converted to the 10th revision of the International Classification of Diseases (ICD-10) and coded to C82-86, C96 [16] as shown in Appendix I in supplementary file. In order to ensure consistency in the included tumor types between the successive volumes of CI5 malignant lymphoma, small B lymphocytic, NOS (9,670) was included in our grouping of NHL, whereas NHL B-cell chronic lymphocytic leukemia/small lymphocytic lymphoma (9,823) was excluded.
Statistical analyses
Age-specific incidence rates per 100,000 person-years were estimated by country and sex and presented according to HDI levels. Age-standardized rates (ASR) were weighted using the World Standard population [17] and presented in tabular form with corresponding 95% confidence intervals [18]. The ASR for 2018 and its ranking in relation to other cancer types were depicted in global maps. Time trends in the ASR are presented by calendar year and sex. Analyses were undertaken using R software 3.3.3 [19].
Results
Estimated incidence 2018
Figure 1a illustrates the global variation in NHL incidence rates in 2018 for both sexes combined; the corresponding ASR by world region and sex are shown in Table 1. Overall, rates were consistently higher among males compared with females, with sex ratios varying from 1.1 to 1.8 by region. Among men, the highest incidence rates were observed in Australia and New Zealand (16.4 per 100,000), Northern America (14.8 per 100,000), and in Northern Europe (13.5 per 100,000), while the lowest rates were seen in Middle Africa (3.2 per 100,000) and Central America (4.60 per 100,000). A similar geographical pattern was observed in females, with the highest rates observed in Northern America (10.4 per 100,000) and the lowest in Middle Africa (2.8 per 100,000). Figure 1b shows the ranking of NHL by frequency of new cases relative to other major cancers. Marked differences were seen between and within regions worldwide, with NHL ranking as the 4th leading cause of cancer occurrence in Oman, Egypt, Bahrain, Qatar, and Sudan. In a further 87 countries, NHL was the fifth to ninth most common cancer.
Observed incidence circa 2008–2012
Figure 2 shows the recorded national or subnational NHL incidence rates circa 2008–2012 by country according to HDI level. The number of cases and corresponding populations covered by the registries are tabulated in Table 2. Incidence rates of NHL varied tenfold, with NHL rates among males highest in Israel Jews (17.6 per 100,000), Australia (15.3 per 100,000), US whites (14.5 per 100,000), Canada (13.7 per 100,000), and Portugal (13.3 per 100,000). Among females, similar patterns were observed with elevated rates in Israel Jews (13.0 per 100,000) and Australia (12.3 per 100,000), followed by US whites (10.3 per 100,000) and Canada (10.0 per 100,000). In males, incidence rates were lowest in South Africa (1.6 per 100,000), Vietnam, and India (3.5 and 3.6 per 100,000, respectively), with an analogous profile observed among females, but with the lowest rates ranging between 1 and 2 per 100,000.
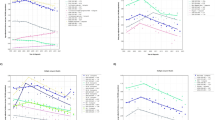
Temporal patterns 1980–2012
Time trends in the NHL incidence rates by sex in selected countries circa 1980–2012 are shown in Fig. 3. In the majority of countries, trends in incidence rates were either stable or decreases among both males and females. The United States, Canada, Australia, and New Zealand all exhibited a rising incidence trend until the 1990s, followed by a stabilization thereafter. Similar temporal patterns were observed in Europe (e.g., in Austria, Croatia, Germany, Italy, France, Spain, and Switzerland) and Asia (e.g., in Japan, Korea, India, Philippines, and Thailand).
HIV prevalence, Human Development Index, and NHL incidence
Figure 4a presents a graphic representation of HIV prevalence in 2010 and the estimated incidence of NHL in 2018, both sexes combined. Figure 4b shows the estimated incidence of NHL in 2018, and the Human Development Index, both sexes combined. Higher rates of NHL were common in countries classified as very high HDI, while many countries classified as low and medium HDI presented lower incidence rates. The linear relation between the magnitude of the NHL incidence rates and level of HDI appears confined to very high HDI countries.
a Prevalence of HIV among adults aged 15–49 years old in 2010 (log scale) and age-standardized incidence rates 2018 by Human Development Index; b age-standardized incidence rates and Human Development Index (natural scale) by the prevalence of HIV among adults aged 15–49 years. The diameter of the circles is relative to the magnitude of the HIV prevalence and their color represents HDI level
Discussion
In this population-based study, we provide a comprehensive review of NHL incidence using national estimates in 185 countries for the year 2018, complemented by a more detailed exposition of geographical and temporal variations based on either national or subnational high-quality data from population-based cancer registries included in the Cancer Incidence in Five Continents series. We report distinct geographic patterns in NHL incidence by world region, HDI level, sex, and age, with rates consistently higher among males than females. As a disease entity, NHL ranks as the fourth leading cause of cancer occurrence in Oman, Egypt, Bahrain, Qatar, and Sudan, and as the fifth to ninth most common cancer in a further 87 countries of the world. The incidence trends were stable or increasing in most countries where data were available; in the populations representing North America, Europe, and Oceania, a pattern of rising incidence until the 1990s, followed by a stabilization, was commonly observed.
NHL comprises a wide range of cancers of the immune system ranging from indolent to aggressive types [3] for which the extent of clinical resources are a major factor in assuring accurate diagnoses. The observed heterogeneity of NHL incidence rates by human development level seen in this study can thus be postulated to be driven by disparities in health system infrastructure and the delivery of cancer services, and consequently, the availability of diagnostic and treatment facilities for cancer [20]. Diagnostic precision of NHL requires excisional biopsy, followed by a pathologist examination and the final classification, based on morphology, immunophenotype, genetic, and clinical features [21, 22]. Such a process may be unattainable at present in some LMIC, where advanced diagnostic techniques are not available. The reported NHL incidence may thus also be subject to some misclassification and under-reporting in these settings.
The heterogeneity of NHL incidence rates and trends is also related to the prevalence and distribution of the underlying known and putative risk factors [20]. In Africa, parts of South America, and Asia, the estimated incidence rates could in part reflect the infectious origin of NHL. There is accumulating evidence that EBV is linked to the etiology of NHL [23]. EBV-positive diffuse large B-cell lymphoma (DLBCL) is a category of NHL subtype included in the WHO Blue Books since 2008 and represents between 5 and 15% of all DLBCLs worldwide [24]. These cases are more common in the elderly, as they relate to the process of aging that causes alterations in the immune system and the protracted latency of EBV infection [25]. Several other T-cell and NK-cell NHL are classified as EBV-positive; these are rarer types, that have been reported to occur more commonly in less-resourced settings in Asia and among indigenous populations in Latin America [26].
Assessments of the causal association between HIV and NHL at the global level through ecologic analyses are subject to well-known biases and any interpretation should be undertaken with caution. The observation that countries with a low prevalence of HIV in 2010 had quite variable NHL incidence rates may relate to the poorer survival of HIV-infected patients in LMIC, and the possibility that many patients die before they would have developed NHL. HIV infection plays an important role in the etiology of NHL, and it has been estimated that around 5–10% of HIV-infected patients develop lymphomas [27], and thus countries with a high prevalence of HIV, such as Uganda (7%, data not shown), and Zimbabwe (15.5%, data not shown), the incidence of NHL is expected to be elevated, even in the presence of some misclassification. As NHL is an AIDS-defining cancer, incidence rates may have declined upon the introduction of the antiretroviral treatment, notably in these Sub-Saharan Africa countries that have been among the most impacted by the HIV epidemic [28, 29].
Globally, we observed some disparities in the temporal patterns of NHL incidence in different countries. An explanation for the slight increases in incidence in certain Asian countries including the Republic of Korea, and Japan is not clear but may be partially linked to better diagnosis and complete registration, as well as environmental exposures and lifestyle factors [30]. HBV has been linked to NHL incidence in Korea [31] and an increasing incidence of NHL observed at older ages, while HBV prevalence is decreasing at younger ages [32]. A high proportion (50–60%) of adult T-cell leukemia/lymphoma among NHL in Japan [33] illustrates the importance of HTLV-I infection on NHL incidence. The high prevalence of HTLV-1 recorded in Japan, and certain populations in Africa, South America, and Caribbean [34] may contribute to the observed elevated incidence rates of NHL, that are likely modulated by other factors. Perry et al. [35] found marked differences in the frequencies of NHL subtypes in developed and developing regions; for instance, a lower frequency of B-cell NHL and higher frequency of T- and NK-cell NHL were seen in developing regions, while a higher frequency of Burkitt lymphoma was observed in parts of Central and South America and Africa.
Our common observation of a rising incidence in North America, parts of Europe, and Oceania until the 1990s with a stabilization thereafter is confirmed by other reports. van Leeuwen et al. [36] reported NHL incidence increasing during the period 1982–1996, with stable trends seen from 1997 to 2006. In Spain, Marcos-Gragera et al. [37] found an attenuation in NHL incidence after 1996, that was hypotheses as partly explained by the decrease in incidence of AIDS-related lymphomas among young adults and other factors. Adamson et al. [38] described the trends in incidence of 13 European countries until 2000, observing an increase in the number of NHL registration in all countries of the study [38].
While a higher incidence of NHL has been consistently reported In North America and other developed countries and one that has been linked to the HIV epidemic [37, 39], the temporal patterns of NHL, must be interpreted with caution. The improvements in cancer registration, as well as the changing classification may have impacted on the observed patterns over time. The Revised European-American Classification of lymphoid Neoplasms (REAL) became the basis for the WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue when originally published in 2001, and represented a global consensus on hematopoietic classification that likely coincides with some of the period-related changes in the trends observed in this study.
There are also a number of limitations in our study. The robustness of the national estimates in GLOBOCAN varies by country depending on the availability of high-quality incidence and mortality data. International comparisons based on the observed data from PBCR may be subject to varying coding practices between the registries included in the CI5 series and within each institution over time. It is also important to note that incidence data are derived from subnational cancer registries in many countries, and some will be more representative of the national profile and time trends than others. While the registries included in CI5 are deemed of high quality by an appointed editorial board, there remains the need to improve the accuracy of information on hematological malignancies as defined in the pathology reports abstracted at the PBCR. Not all cancer registries provide specific morphological diagnosis for a sufficiently large proportion of cases as to be included in analyses by histological subgroup. Although such analyses may help interpreting the results in the areas with high-quality pathology services, the definition of subtypes may be subjected to regional variation.
An important strength of our study is the global coverage assembled via successive volumes of CI5 spanning 30 years, alongside national estimates for all world areas for the year 2018 from the GLOBOCAN database that can be inspected at IARC’s Global Cancer Observatory (http://gco.iarc.fr). In countries with longstanding cancer registries of high quality, an age-period-cohort analysis is warranted to determine more explicitly the role of period effects (linked mainly to artifact, such as changes in practices affecting all studied age groups at a given time or time period) versus birth cohort effects (linked mainly to changes in population-level risk and the prevalence of the underlying determinants among successive generations).
Conclusion
The marked differences in contemporary NHL incidence rates by country and region may be partly linked to contrasting levels of access to care and the availability of diagnostic services. In addition, endemic infections and environmental exposures in regions in Africa, Asia, and Latin America likely contribute to these differences. Changes in classification of NHL have been applied at different time points in the contributing registries, and these may have partially affected the observed patterns and time trends. All of these factors need to be taken into account to gain further insight into this complex set of diseases.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries: global cancer statistics 2018. CA Cancer J Clin. https://doi.org/10.3322/caac.21492
Weltgesundheitsorganisation (2017). WHO classification of tumours of haematopoietic and lymphoid tissues, Revised 4th edn. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H et al (eds) World Health Organization classification of tumours. International Agency for Research on Cancer, Lyon, p 585
Armitage JO, Gascoyne RD, Lunning MA, Cavalli F (2017) Non-Hodgkin lymphoma. Lancet 390(10091):298–310
CRUK (2018) Non-Hodgkin’s lymphoma statistics. 2012. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-hodgkin-lymphoma. Accessed 21 Jan 2019
Boffetta P (2011) I. Epidemiology of adult non-Hodgkin lymphoma. Ann Oncol 22(Supplement 4):iv27–iv31
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M et al (2018) Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 391(10125):1023–1075
Morton LM, Slager SL, Cerhan JR, Wang SS, Vajdic CM, Skibola CF et al (2014) Etiologic heterogeneity among non-Hodgkin lymphoma subtypes: the InterLymph Non-Hodgkin lymphoma subtypes project. J Natl Cancer Inst Monogr 2014(48):130–144
Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S (2016) Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob Health 4(9):e609–e616
Shiels MS, Engels EA (2017) Evolving epidemiology of HIV-associated malignancies. Curr Opin HIV AIDS 12(1):6–11
Gibson TM, Morton LM, Shiels MS, Clarke CA, Engels EA (2014) Risk of non-Hodgkin lymphoma subtypes in HIV-infected people during the HAART era: a population-based study. AIDS 28(15):2313–2318
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M et al (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012: Globocan 2012. Int J Cancer 136(5):E359–E386
United Nations Development Programme (2017) Human development programme index (HDI). Available from: http://hdr.undp.org/en/content/human-development-index-hdi. Accessed 21 Sept 2018
WHO Global Health Observatory. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/tobacco. Accessed 16 Sep 2018
Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Ferlay J (eds) (2017) Cancer incidence in five continents, Vol. XI (electronic version). International Agency for Research on Cancer, Lyon. Available from: http://ci5.iarc.fr. Accessed 20 Aug 2018
Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Ferlay J (eds) (2017) Cancer incidence in five continents plus, (time trends) (electronic version). International Agency for Research on Cancer, Lyon. http://ci5.iarc.fr/CI5plus/Default.aspx. Accessed 22 Sep 2018
WHO. World Health Organization (1995) International statistical classification of diseases and health-related problems - 10th Revision, 2nd edn [Internet]. Available from: http://apps.who.int/classifications/icd10/browse/2010/en. Accessed 17 May 2017
Segi M (1960) Cancer mortality for selected sites in 24 countries (1950–1957). Tohoku University School of Medicine, Sendai
Jensen OM, International Agency for Research on Cancer, World Health Organization, International Association of Cancer Registries (eds) (1991) Cancer registration: principles and methods, IARC scientific publications. International Agency for Research on Cancer, Lyon, p 288
R Development Core Team. R Development Core Team (2014) R: a language and environment for statistical computing (computer programme). R Foundation for Statistical Computing, Vienna
Østgård LSG, Nørgaard M, Nørgaard JM, Severinsen MT, Sengeløv H, Friis LS et al (2013) Data quality in the Danish national acute leukemia registry: a hematological data resource. Clin Epidemiol 5:335
McKay P, Fielding P, Gallop-Evans E, Hall GW, Lambert J, Leach M et al (2016) Guidelines for the investigation and management of nodular lymphocyte predominant Hodgkin lymphoma. Br J Haematol 172(1):32–43
Eichenauer DA, Thielen I, Haverkamp H, Franklin J, Behringer K, Halbsguth T et al (2014) Therapy-related acute myeloid leukemia and myelodysplastic syndromes in patients with Hodgkin lymphoma: a report from the German Hodgkin study group. Blood 123(11):1658–1664
IARC. IARC (1997) Epstein–Barr virus and Kaposi’s sarcoma herpesvirus/human herpesvirus 8. World Health Organization, Lyon. Available from: https://monographs.iarc.fr/iarc-monographs-volume-100b-epstein-barr-virus/. Accessed 10 Jan 2019
Weltgesundheitsorganisation, Swerdlow SH, International Agency for Research on Cancer (eds) (2008) WHO classification of tumours of haematopoietic and lymphoid tissues: [… reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25–27, 2007, World Health Organization classification of tumours, 4 edn. International Agency for Research on Cancer, Lyon. p 439
Castillo JJ, Beltran BE, Miranda RN, Young KH, Chavez JC, Sotomayor EM (2016) EBV-positive diffuse large B-cell lymphoma of the elderly: 2016 update on diagnosis, risk-stratification, and management: EBV+ DLBCL 2016 update. Am J Hematol 91(5):529–537
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R et al (2016) The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 127(20):2375–2390
Silverberg MJ, Lau B, Achenbach CJ, Jing Y, Althoff KN, D’Souza G et al (2015) Cumulative incidence of cancer among persons with HIV in North America: a cohort study. Ann Intern Med 163(7):507–518
Chaabna K, Bray F, Wabinga HR, Chokunonga E, Borok M, Vanhems P et al (2013) Kaposi sarcoma trends in Uganda and Zimbabwe: a sustained decline in incidence?: trends of KS incidence in Zimbabwe and Uganda. Int J Cancer 133(5):1197–1203
Parkin DM, Garcia-Giannoli H, Raphael M, Martin A, Katangole-Mbidde E, Wabinga H et al (2000) Non-Hodgkin lymphoma in Uganda: a case–control study. AIDS 14(18):2929–2936(
Chihara D, Ito H, Matsuda T, Shibata A, Katsumi A, Nakamura S et al (2014) Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol 164(4):536–545
Engels EA, Cho ER, Jee SH (2010) Hepatitis B virus infection and risk of non-Hodgkin lymphoma in South Korea: a cohort study. Lancet Oncol 11(9):827–834
Kim H, Shin AR, Chung HH, Kim MK, Lee JS, Shim J-J et al (2013) Recent trends in hepatitis B virus infection in the general Korean population. Korean J Intern Med 28(4):413–419
Arisawa K, Soda M, Endo S, Kurokawa K, Katamine S, Shimokawa I et al (2000) Evaluation of adult T-cell leukemia/lymphoma incidence and its impact on non-Hodgkin lymphoma incidence in southwestern Japan. Int J Cancer 85(3):319–324
Proietti FA, Carneiro-Proietti ABF, Catalan-Soares BC, Murphy EL (2005) Global epidemiology of HTLV-I infection and associated diseases. Oncogene 24(39):6058–6068
Perry AM, Diebold J, Nathwani BN, MacLennan KA, Müller-Hermelink HK, Bast M et al (2016) Non-Hodgkin lymphoma in the developing world: review of 4539 cases from the international non-Hodgkin lymphoma classification project. Haematologica 101(10):1244–1250
van Leeuwen MT, Turner JJ, Joske DJ, Falster MO, Srasuebkul P, Meagher NS et al (2014) Lymphoid neoplasm incidence by WHO subtype in Australia 1982–2006: lymphoid neoplasms in Australia 1982–2006. Int J Cancer 135(9):2146–2156
Marcos-Gragera R, Pollán M, Chirlaque MD, Gumà J, Sanchez MJ, Garau I et al (2010) Attenuation of the epidemic increase in non-Hodgkin’s lymphomas in Spain. Ann Oncol 21(Suppl 3):iii90–iii96
Adamson P, Bray F, Costantini AS, Tao M-H, Weiderpass E, Roman E (2007) Time trends in the registration of Hodgkin and non-Hodgkin lymphomas in Europe. Eur J Cancer 43(2):391–401
Clarke CA, Glaser SL (2002) Changing incidence of non-Hodgkin lymphomas in the United States. Cancer 94(7):2015–2023
Acknowledgments
The work reported here was undertaken by Dr. Miranda-Filho during the tenure of an IARC Postdoctoral Fellowship, partially supported by the European Commission FP7 Marie Curie—Actions—People—co-funding regional, national, and international programmes (COFUND). We would like to thank the Directors and staff of the population-based cancer registries worldwide who compiled and submitted their data for the CI5 and GLOBOCAN projects used in this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Miranda-Filho, A., Piñeros, M., Znaor, A. et al. Global patterns and trends in the incidence of non-Hodgkin lymphoma. Cancer Causes Control 30, 489–499 (2019). https://doi.org/10.1007/s10552-019-01155-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01155-5