Abstract
Purpose
California Cancer Registry data were used to explore the impact of hepatocellular carcinoma (HCC) surveillance on patient outcomes. The purpose of this analysis was to determine the trend in diagnosis of early-stage HCC in California from 1988 to 2010.
Methods
Patients 20+ years old, diagnosed with early HCC during 1988–2010 in California, were included. Stratified proportions of early HCC were evaluated to estimate any trends and significant disparities. The primary endpoint was the average annual percent change (AAPC) of the proportion of early-stage HCC; 2- and 5-year survival trends were calculated for age, sex, race, SES, and stage.
Results
A total of 13,855 patients were diagnosed with early HCC. The proportion of patients diagnosed early increased from 19.2 to 49.2 % between 1988 and 2010, at an AAPC of 4.3 %. The proportion of cases diagnosed with early HCC increased in all demographic groups. Both the 2- and 5-year cause-specific survival analyses showed that survival among HCC patients has been increasing since 1988.
Conclusion
The proportion of HCC cases diagnosed early, and the 2- and 5-year survival trends of all HCC patients have increased in California since 1988. It is not entirely clear whether better diagnostic imaging or better surveillance has led to these findings and whether earlier diagnosis has led to improved patient survival. This increase in survival among patients with HCC may be correlated with the innovation of new treatments and most importantly that patients are being diagnosed earlier to receive such treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Hepatocellular carcinoma (HCC) is the third leading cause of mortality among all cancers worldwide [1, 2] and is the most common type of liver cancer [3]. The incidence of HCC in the USA has tripled since the 1980s [4], and HCC is predicted to become the third leading cause of cancer-related death in the USA by the year 2030 [5]. California was ranked as one of the five states with the highest mortality rates in 2010 [6].
From 2001 through 2010, incidence rates of liver cancer among California men and women increased significantly (by 44 and 28 %, respectively). This increase in liver cancer incidence was detected among all racial and ethnic groups except Asian/Pacific Islanders, for whom rates fluctuated during this time period, but still remained the highest among all race groups. Mortality rates for liver cancer also increased in men and women of all racial and ethnic groups during this time period (by 31 and 14 %, respectively) except among Asian/Pacific Islander men, in whom mortality rates have declined significantly (by 16 %) since 1996 [7].
While the prognosis of HCC is generally dismal with a 5-year survival of 12 % or less, early detection allows treatment by radiofrequency ablation, partial hepatectomy, and liver transplantation which are associated with 5-year survival of 50–70 % [8]. Thus, early detection and treatment of HCC are paramount to improved patient survival [9].
In the 1980s, surveillance efforts shifted from the use of alpha-fetoprotein (AFP) screening in average risk individuals to periodic surveillance with AFP and abdominal ultrasound in increased risk individuals. At the time of the shift, some clinical evidence had become available which suggested that this combined screening method improved diagnosis rates of earlier-stage, asymptomatic cancer compared to AFP screening alone [10]. The purpose of this study was to determine trends in the detection of early HCC in California and survival trends since the implementation of abdominal ultrasound-based HCC surveillance.
Methods
Patients with HCC were identified through the California Cancer Registry (CCR). The CCR is a population-based database that contains data on all California residents diagnosed with any reportable cancer since 1988. Treatment facilities, hospitals, and health professionals are required to report all cancer. Reports include demographics, diagnosis, treatment information, and tumor characteristics. To ensure current follow-up for vital status and cause of death, the CCR database is linked annually to death certificates, hospital discharge data, Medicare files, the Department of Motor Vehicles, Social Security, and other administrative databases. Linkage to the National Death Index ensures capture of deaths occurring outside California as well as cause of death, and the follow-up is over 96 % for patients diagnosed since 2000. The CCR is a participant in both the Centers for Disease Control National Program of Cancer Registries and the National Cancer Institute Surveillance Epidemiology and End Results (SEER) program, which requires the highest standards of data quality, as judged by completeness, accuracy, and timeliness.
Patients included in this study were males and females, aged 20 years and older, diagnosed with HCC during 1988–2010 according to ICD-O-3 histology codes 8170–8175, and resided in California at the time of their diagnosis. Age was categorized into three groups: 20–49 years, 50–64 years, and 65+ years. Race and ethnicity were collected from medical records and categorized into four mutually exclusive racial/ethnic groups: non-Hispanic White, Hispanic, non-Hispanic Black, and non-Hispanic Asian/Pacific Islander. An additional analysis included the following Asian subgroups: Chinese, Japanese, Filipino, Korean, South Asian (Asian Indian/Pakistani), Vietnamese, Cambodian, Thai, and Laotian/Hmong. Socioeconomic status (SES) was determined using the summary Yost index which utilizes US Census characteristics [11] and categorized as low, middle-low, middle, middle-high, and high. Stage at diagnosis was defined based on SEER summary staging categorized as follows: localized, regional, distant, and unknown, and in this analysis, early HCC was defined as localized.
All data were analyzed using SEER*Stat version 8.1.15 and Joinpoint Regression Program version 4.1.0, and a p value of <0.05 was considered statistically significant. Joinpoint regression is a program of SEER that defines trends during a defined time period. The primary endpoint in this analysis was the average annual percent change (AAPC) of the proportion of early-stage HCC. The AAPC was calculated for age, race, sex, and SES to determine any trends during this time period.
Lastly, a 2- and 5-year cause-specific survival analysis was performed with follow-up through 2011. Estimates were calculated using the Kaplan–Meier method and the standard life table approach. Only individuals with one primary cancer and with the cause of death being liver cancer were used in this analysis. Survival trends were calculated for age, sex, race, SES, and stage.
Results
During the years 1988–2010, 35,190 patients were diagnosed with HCC. Of these cases, 13,855 (39 %) were localized cancers or early HCC. The proportion of early HCC was 42.6 % in women and 38.3 % in men. The proportion of early HCC was 35.7 % in 20–49 year olds, 40.4 % in 50–65 year olds, and 39.5 % in patients 65 years and older. There were slight differences among the proportion of early HCC in the racial/ethnic groups: non-Hispanic Whites (39.3 %), non-Hispanic Blacks (35.0 %), Hispanics (40.8 %), and non-Hispanic Asian/Pacific Islanders (39.5 %).
In Asian subgroups, the proportion of early HCC was 43.1 % in Vietnamese, Japanese (39.4 %), Chinese (39.0 %), Filipino (37.9 %), Korean (37.6 %), Cambodian (37.4 %), South Asian (37.0 %), Thai (33.0 %), and Laotian/Hmong (29.4 %) (Table 1).
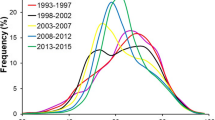
The proportion of cases diagnosed with early HCC increased in all age, race, sex, and SES groups between 1988 and 2010. The overall proportion of patients diagnosed with early HCC increased from 19.2 to 49.2 % during this period, with an AAPC of 4.3 %. The increase in proportion diagnosed early was seen in all age groups: 20–49 years (4.5 %), 50–64 years (4.6 %), and 65+ years (4.6 %). Women had an AAPC of 5.1 % and men 4.3 %. The increase was greatest among non-Hispanic Asian/Pacific Islander patients and among patients residing in low and middle-low SES neighborhoods (Table 2).
Both the 2- and 5-year cause-specific survival analyses showed that survival among HCC patients has been increasing since 1988 across all categories; 2-year survival for all HCC cases increased from 14.5 % for patients diagnosed in 1998 to 45.9 % for those diagnosed in 2010 with an AAPC of 5.4 %, and 5-year survival increased from 8.0 to 31.9 % for patients diagnosed in 1988–2007 with an AAPC of 7.9 %. In all categories, the increase in 5-year survival was greater than the increase in 2-year survival. The overall and stratified trends were statistically significant at a p value <0.05 except for patients diagnosed with tumors diagnosed at distant summary stage. Younger patients generally had higher survival, but patients 65 years and older had the highest AAPC in both the 2- and 5-year cause-specific survival trends (5.9 and 8.0 %, respectively). The 20–49 years old and 50–64 years old age groups had similar AAPCs in both 2- and 5-year survival trends. Non-Hispanic Blacks had the lowest survival, but the greatest increase in 5-year survival with an AAPC of 20.4 %. Non-Hispanic Asian/Pacific Islanders had the highest survival starting in about 1994 and the second greatest increase in 5-year survival with an AAPC of 8.1 %. Females had overall better survival than males, but the two groups had similar AAPCs. Although survival was generally lower in the lowest SES group and higher in the highest group, all groups had a similar increase in survival over time (Table 3).
Discussion
The proportion of HCC cases diagnosed early, as well as the proportion of patients surviving 2 and 5 years, have increased in California since 1988 over all and across all demographic groups. These findings may be influenced by improvements in screening and surveillance of patients with known risk factors for HCC as well as advances in curative therapies [4, 12, 13].
Our study, as well as other studies, has seen the proportion of early-stage HCC increasing steadily. Altekruse et al. [9] suggested that there is more awareness to HCC now increasing the number of patients diagnosed at an early stage. In a summary of HCC diagnosis and treatment, El-Serag et al. indicated that the screening of HCC has manifested recently with the combination of screenings such as serum alpha-fetoprotein testing, abdominal ultrasound, and diagnostic testing [9, 14–16]. More so, special attention to high-risk groups has increased the number of patients diagnosed at an early stage [9, 15, 16]. Although not drastically different, in our study non-Hispanic Asian/Pacific Islanders, known to be a high-risk group, had the highest increase in the proportion of early HCC diagnosis [2, 15].
While all age, sex, race, and SES groups demonstrated increasing survival trends, notable disparities were apparent among certain racial, SES, and age groups. Although not statistically comparable, overall, non-Hispanic Blacks and non-Hispanic Asian/Pacific Islanders had the highest 2 and 5 years average annual percent increase in survival between 1988 and 2010. Non-Hispanic Blacks consistently had the lowest 2-year survival across all racial groups during the entire period examined and generally the lowest 5-year survival. However, this group had the greatest increase in survival. In previous studies, low income, education, employment, and lack of access to health care among non-Hispanic Blacks have been linked to this racial disparity in survival [17–20]. It is possible that the dramatic increase in survival for non-Hispanic Blacks reflects that this disparity gap is decreasing. The survival advantage among non-Hispanic Asian/Pacific Islanders, especially after surgical resection, may be related to a lower prevalence of cirrhosis in hepatitis B-associated HCC and better hepatic reserve after treatment as compared to cases of hepatitis C-associated HCC cases [21]. In addition, practitioners are advised to perform more stringent HCC surveillance in high-risk groups.
Although patients residing in higher SES neighborhoods had better survival overall, no dramatic differences in regard to the average annual percent changes in the 2- and 5-year survival trends were seen among the SES groups. Presumably, patients with more economic resources have better access to healthcare as well as improved healthcare literacy. Although there may still be disparities among socioeconomic status, the similar AAPCs indicate that survival is increasing in all groups at a similar rate despite historical disparities. Lastly, it appears patients 65 years and older had poorer 2- and 5-year survival outcomes than other age groups. This may be due to increased concomitant co-morbidities at later stages in life as well as more advanced fibrosis in an older population. However, survival appears to be increasing at a greater rate in this age group, indicating that treatment of co-morbidities may be improving.
Altekruse et al. [9] found similar results in which the survival has been increasing which can be attributed to the increase in diagnosis at such an early-stage and more advanced treatments, such as transplantation and tumor resection. Although increase in survival has been seen by utilizing transplants, there is controversy on how long patients should wait on the transplant list before trying other forms of treatment [16]. Nathan et al. [22] found a fivefold increase in surgical treatment of HCC, which may be attributable to the increase in diagnosis and proportion of early HCC.
Having access to data since 1988 from the largest cancer registry in the USA gave our study tremendous power allowing trends and interpretations to be made. The population in this study represented the diverse population of California which allowed analysis of diagnosis and survival by race/ethnicity, SES, and age. Limitations of the study include lack of information about infection with hepatitis B and C, and lack of information on screening, and limited information on treatment.
Our study found that despite the increasing incidence of HCC, the proportion of patients diagnosed early is continuing to climb, and the overall survival of HCC is improving across all demographics. This increase in survival among patients with HCC may be correlated with the innovation of new treatments and most importantly that patients are being diagnosed at an earlier stage to receive such treatments. Future studies looking at these individual treatments to see which may be having the most impact on survival could help translate the findings in this study. It may be a combination of treatment and diagnosis that are having the most impact on overall survival of patients with HCC. With continued surveillance and improved primary prevention of HCC, we can expect to observe declining incidence and mortality in future years.
References
Hepatocellular Carcinoma (Humana Press, 2010). http://springerlink.bibliotecabuap.elogim.com/10.1007/978-1-60327-376-3
Naugler W, Schwartz J (2008) Hepatocellular carcinoma. Liver Dis 54:432–444
American Cancer Society. Liver Cancer (2015). http://www.cancer.org/cancer/livercancer/detailedguide/liver-cancer-what-is-liver-cancer
El-Serag HB (2011) Hepatocellular carcinoma. N Engl J Med 365:1118–1127
Rahib L et al (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. doi:10.1158/0008-5472.CAN-14-0155
Monsour HP Jr et al (2013) Hepatocellular carcinoma: the rising tide from east to west—a review of epidemiology, screening and tumor markers. Transl Cancer Res 2:492–506
Cook S et al (2014) Annual report on the status of cancer in California, 1988–2010. http://www.ccrcal.org/pdf/Reports/AnnualReport2014_9-15-14.pdf
Crissien AM, Frenette C (2014) Current management of hepatocellular carcinoma. Gastroenterol Hepatol 10:153–161
Altekruse SF, McGlynn KA, Reichman ME (2009) Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol 27:1485–1491
Shanghai Coordinating Group for Research on Liver Cancer (1979) Diagnosis and treatment of primary hepatocellular carcinoma in early stage: report of 134 cases. Chin Med J (Engl) 92:801–806
Yost K, Perkins C, Cohen R et al (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control CCC 12:703–711
Schwarz RE, Smith DD (2008) Trends in local therapy for hepatocellular carcinoma and survival outcomes in the US population. Am J Surg 195:829–836
Yang JD et al (2011) Factors that affect risk for hepatocellular carcinoma and effects of surveillance. Clin Gastroenterol Hepatol 9:617–623
El-Serag HB, Marrero JA, Rudolph L, Reddy KR (2008) Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology 134:1752–1763
Song DS, Bae SH (2012) Changes of guidelines diagnosing hepatocellular carcinoma during the last ten-year period. Clin Mol Hepatol 18:258–267
Llovet JM, Bruix J (2000) Early diagnosis and treatment of hepatocellular carcinoma. Best Pract Res Clin Gastroenterol 14:991–1008
Artinyan A et al (2010) Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer 116:1367–1377
Chen J-D et al (2010) Carriers of inactive hepatitis B virus are still at risk for hepatocellular carcinoma and liver-related death. Gastroenterology 138:1747–1754
Yuen M-F et al (2008) Independent risk factors and predictive score for the development of hepatocellular carcinoma in chronic hepatitis B. J Hepatol 50:80–88
Yu L, Sloane DA, Guo C et al (2006) Risk factors for primary hepatocellular carcinoma in Black and White Americans in 2000. Clin Gastroenterol Hepatol 4:355–360
Kao W-Y et al (2011) A comparison of prognosis between patients with hepatitis B and C virus-related hepatocellular carcinoma undergoing resection surgery. World J Surg 35:858–867
Nathan H et al (2012) National trends in surgical procedures for hepatocellular carcinoma: 1998–2008. Cancer 118:1838–1844
Acknowledgments
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement U58DP003862-01 awarded to the California Department of Public Health. The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Funding
This work was supported by the NCI Comprehensive Cancer Center Support Grant (P30CA93373).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Rodriguez, D.N., Torruellas, C. & Cress, R.D. Trends in early-stage hepatocellular carcinoma, California 1988–2010. Cancer Causes Control 27, 325–331 (2016). https://doi.org/10.1007/s10552-015-0705-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-015-0705-2